Today is Holy Saturday, the day when Jesus joined the dead; a day of sorrow as we await Easter and rebirth. Tonight, at the Easter Vigil mass at St Paul’s Church in Harvard Square, Shou-Ching will be baptized and received into the Roman Catholic Church.
[1] Interesting posts this week: Bix at Fanatic Cook finds another study showing that calcium supplements increase risk of heart attack and stroke. Ned Kock discusses why older Inuit had lower bone mineral density. Stan the Heretic links to a study showing that if you have heart disease and want to eat a BIG meal, you should make it fatty. Jimmy Moore discusses the rising cost of coconut oil. Jimmy recounts his 7 day fast here. Jamie Scott provides background on the epigenetics of obesity, and a recipe for shrinking pig brains. Mark Sisson explains how to breathe. CarbSane finds that exercise is highly under-rated for fat (not weight) loss. Earlier, CarbSane engaged her critics on insulin. From Kit Perkins, a correspondent of Richard Nikoley, comes a good line indicating the link between hunger and fat regulation: “for me and a lot of others, we felt the most hungry when gaining fat and the most satiated while losing fat.”
The New York Times “Think Like a Doctor” series is getting to be like an episode of House. Test your analytical skills: The puzzle. The solution.
Finally, Don Matesz gives us more evidence from the China Study. Rice, fish, meat, and green vegetables are good. Wheat, other grains including corn, legumes, and light-colored vegetables are bad.
[2] Aw Maa!:
Via Yves Smith.
[3] Autism and Diet: “Best of Emily” continues at Psychology Today with two posts on the links between opioid peptides, leaky gut, and autism, and evidence in support of two possible fixes: a gluten-free casein-free diet and low dose naltrexone.
LDN enhances bacterial and viral immunity, and there are links between autism and viral infection, so we consider LDN as a highly plausible frontline therapy for autism.
Emily has a third post that mentions evidence that maternal malnutrition contributes to autism. In it she links to a free review of maternal nutrition and birth outcomes.
[4] 10 Years of Weight Loss: My favorite post this week was from Seth Roberts, reporting 10 years of weight measurements from one of his readers:
Low-carb dieting worked great for a time – Alex lost 50 pounds in his first year on low-carb – but over the second year his weight bottomed at 200 pounds and went back up to 220, at which point he gave up on low-carb.
Alex went to the opposite extreme, vegetarian and vegan dieting, but gained more weight.
Then he began walking. As with the low-carb diet, he lost weight rapidly for a time and then regained some of it.
Finally, on Seth’s Shangri-La Diet he lost weight rapidly for a time, then plateaued in the 190s.
A long data series like this is instructive on the difficulties of returning to slenderness; and the tendency for weight – yes, even on low-carb low-insulin diets – to reach a plateau and then rebound.
[5] Fraud revisited: Last week (#13) I mentioned the arrest of a leading autism researcher for stealing research funds, and problems with research fraud.
This week John Hawks hints at another fraud problem in biomedical science: dishonest grant applications. This is a problem two ways: (1) Only 15% of grants are funded, so even if a small fraction of the proposals are fraudulent, frauds may get most of the money if the “best” (read: too good to be true) proposals are funded. (2) Reviewers defend against fraud by awarding money only to people they know – their friends and the “big name” groups. So the field becomes inbred and un-innovative.
The best solution, I argued last week, would be to decentralize funding to patients and taxpayers. An Amazon-like system letting people rate researcher performance and review public records of proposals and results would be enough, I think, to guide funds to productive groups and institutions such as hospitals and universities, while enabling innovators and outsiders to get a share of funds.
[6] Preserving the Serengeti: JS Stanton has an appeal to protect migration ways of Serengeti wildlife by stopping construction of a highway through the park. (Depressing and covering the highway would be another solution.)
He provides some video as well as photos from a Guardian picture gallery:
[7] Do you know your bug type?: The New York Times reports that humans have four blood types, but only three “enterotypes” – gut microbial ecosystems. The story is based on this Nature article.
[8] Dr Steve Parker unearths a good line:
Diet has always generated passion, and passion in science is an infallible marker of lack of evidence.
That sentence is from a review of diabetic diet cycles over the last 150 years, published in Diabetologia (2009, vol. 52, pages 1-7).
[9] The key to healthy shoulders: The Boston Globe reports that the leading cause of shoulder injuries may be misaligned shoulder blades.
This doesn’t surprise me, as the two things that most helped my shoulders were:
- Strengthening exercises, such as push-ups and the reverse fly, that promote shoulder blade retraction.
- Mobility exercises for the shoulder which retract the scapula. I like the following, which someone dubbed “shoulder dislocations”:
[10] REMOVED DUE TO DISGUST BY CO-AUTHOR. Do not watch the video linked by Stabby here.
[11] I hate when that happens: A bank in India opened a vault to find termites had eaten through millions of rupees.
[12] Beth Mazur is giddy: Beth points out a new way high-carb, high-vegetable-oil diets may promote obesity.
It turns out that insulin upregulates an enzyme that turns omega-6 fatty acids into an appetite stimulating hormone called anandamide, “which is a chemical that affects the same receptor in the brain that THC does … you know THC, it’s the active ingredient in pot. And when people smoke pot they often get … the munchies.”
Beth goes on to give a reason why American food works better than pot at causing obesity.
[13] Pesticides impact IQ: The most pesticides in the mother, the lower the IQ of the child, says The Scientist reporting on new research in Environmental Health Perspectives.
[14] Mozart: Two guys, one guitar:
[15] Another upright blogger: Emily Deans has a fancy new (hardwood!) standing desk.
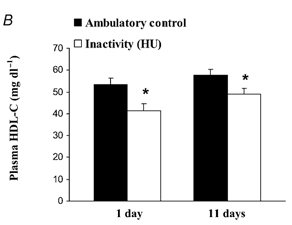
[16] Ooh! Ooh! Can I have one?: If Jamie Scott’s walking desk doesn’t raise your HDL enough, consider a Dutch HDL-raising closet:
[17] Weekly video: Director Krzysztof Kie?lowski produced for Polish television a magnificent, dark but moving and inspirational, series called The Decalogue , consisting of 10 hour-long dramas each dealing with one of the Ten Commandments. The videos are on Youtube with English subtitles.
For those who have an hour to spare, in honor of Passion Week, here is Dekalog I part I:
The remainder of Dekalog I: Part 2, Part 3, Part 4, Part 5, and Part 6.




























Recent Comments