Jan Kwasniewski developed his Optimal Diet something like 40 years ago and it has become extremely popular in Poland.
Kwasniewski recommended that adults should eat in the ratio
(Source).
In terms of calories this is roughly 240 calories protein / 1640 calories fat / 120 calories carbohydrate on a 2000 calorie diet.
The Perfect Health Diet proportions are more like 300 calories protein / 1300 calories fat / 400 calories carbohydrate. So the diets would be similar if about 300 calories, or 15% of energy, were moved from fat to carbohydrate in the form of glucose/starch (not fructose/sugar!).
Note that we recommend obtaining at least 600 calories per day from protein and carbs combined. This ensures adequate protein for manufacture of glucose and ketones in the liver. But the Optimal Diet prescribes only 360 calories total (less in women), suggesting that gluconeogenesis cannot, over any long-term period, fully make up for the dietary glucose deficiency.
In the book, we note that a healthy body typically utilizes and needs about 600 glucose calories per day. On the Bellevue All-Meat Trial in 1928 Vilhjalmur Stefansson ate 550 protein calories per day, which is probably a good estimate for the minimum intake needed to prevent lean tissue loss on a zero-carb diet.
With only 360 carb plus protein calories per day, the Optimal Diet forces ketosis if lean tissue is to be preserved. Since at most 200 to 300 calories per day of the glucose requirement can be displaced by ketones, the Optimal Diet is living right on the margin of glucose deficiency.
Gastrointestinal Cancers in Optimal Dieters
I learned over on Peter’s blog that Optimal Dieters have been dying of gastrointestinal cancers at a disturbing rate. Recently Adam Jany, president of the OSBO (the Polish Optimal Dieters’ association), died of stomach cancer at 64 after 17 years on the Optimal Diet. Earlier Karol Braniek, another leader of the OSBO, died at 68 from duodenal cancer.
A Polish former Optimal Dieter who has now switched to something closer to the Perfect Health Diet noted that gastrointestinal cancers seem to be common among Optimal Dieters:
The impression we get is that there’s rather high occurrence of gut cancer, including stomach, duodenum, colon … [source]
I want to talk about why I think that is, since the danger that the Optimal Dieters are discovering was one of the key factors leading us to formulate and publish the Perfect Health Diet.
Zero-Carb Diets Can Induce Mucus Deficiency
I ate a high-vegetable but extremely low-carb diet from December 2005 to January 2008. At the time I thought I was getting about 300 carb calories a day, but I now consider this to have been a zero-carb diet, since I don’t believe carb calories are available from most vegetables. Vegetable carbs are mostly consumed by gut bacteria, whose assistance we need to break down vegetable matter, or by intestinal cells which consume glucose during digestion.
Throughout my 2 years on this zero-carb diet, I had dry eyes and dry mouth. My eyes were bloodshot and irritated, and I had to give up wearing contact lenses. Through repeated experiments, I established that two factors contributed to the dry eyes – vitamin C deficiency and glucose deficiency. After I solved the vitamin C issue, I did perhaps 50 experiments over the following few years, increasing carbs which made the dry eyes go away and reducing them which made them immediately come back. This established unequivocally that it was a glucose deficiency alone that caused the dry eyes.
Rebecca reports similar symptoms in herself and her low carb friends.
This is also a well-known symptom during starvation. As a review cited by LynMarie Daye (and referenced by CarbSane in the comments) notes,
Since hepatic glycogen stores are depleted within 24 h of fasting, blood glucose concentrations are maintained thereafter entirely through gluconeogenesis. Gluconeogenesis is mainly dependent on protein breakdown (a small amount comes from the glycerol released during lipolysis) and it thus results in protein wasting. It is the effects of protein malnutrition that lead to the eventual lack of ability to cough properly and keep the airways clear, in turn leading to pneumonia and death during prolonged starvation; hypoglycaemia does not occur. [1]
Another common symptom of very low carb diets is constipation. This is often attributed to lack of fiber, but I am skeptical. I will get to the various possible causes of constipation in a future post, but for now I’ll just point out that a deficiency of gastrointestinal mucus would create a dry colon and cause constipation.
What connects a zero-carb diet to dry eyes, dry mouth, dry airways, and dry gastrointestinal tract?
Tears, saliva, and mucus of the sinuses, airways, and gastrointestinal tract are all comprised substantially of glycoproteins called mucins. Mucins are primarily composed of sugar; they typically have a number of large sugar chains bound to a protein backbone.
For instance, the main mucin of the gastrointestinal tract, MUC2, is composed of a dimerized protein – each protein weighing 600,000 Daltons individually, so 1.2 million Daltons for the pair – plus about 4 million Daltons of sugar, for a total mass of 5 million Daltons. In the mucus, these large molecules become cross-linked to form “enormous net-like covalent polymers.” (source)
If, for whatever reason, mucin production were halted for lack of glucose, we would have no tears, no saliva and no gastrointestinal or airway mucus.
Mucin Deficiency Causes Cancer
There is a strong association between mucus deficiency and gastrointestinal cancers.
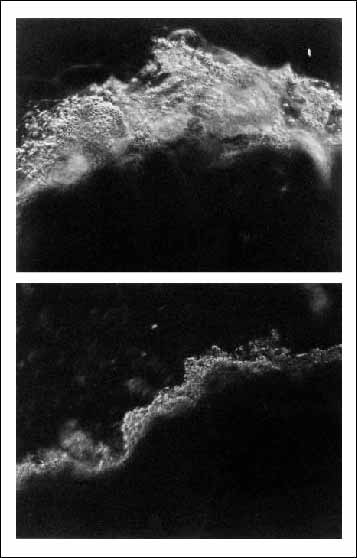
H. pylori is the strongest known risk factor for stomach cancer. [2] H. pylori infection is found in about 80% of gastric cancers. [3] One reason H. pylori promotes stomach cancer so strongly may be that it diminishes mucus in the stomach, as this photo shows:
Top: Normal stomach mucosa. Bottom: Stomach mucosa in an H. pylori infected person.
Scientists have created mice who lack genes for the main digestive tract mucins. These give us direct evidence for the effects on cancer of mucin deficiency.
Experiments in Muc1 knockout mice and mice with Muc1 knockdown have shown that under Helicobacter infection, mice deficient in Muc1 develop far more cancer-promoting inflammation than normal mice. [4]
The main mucin of the intestine is Muc2. The group of Leonard Augenlicht of the Albert Einstein Cancer Center in New York has studied mice lacking Muc2. They develop colorectal cancer. [5]
Tracing backward one step toward the source of mucin deficiency, the sugars in mucin are built from smaller pieces called O-glycans. It has been shown that mice that are deficient in O-glycans are prone to colorectal cancer: “C3GnT-deficient mice displayed a discrete, colon-specific reduction in Muc2 protein and increased permeability of the intestinal barrier. Moreover, these mice were highly susceptible to experimental triggers of colitis and colorectal adenocarcinoma.” [6]
Nutrient Deficiencies Can Also Play a Role
Some micronutrients are required for mucin production – notably vitamin D. [7, 8] Poland is fairly far north, and many of the Optimal Dieters could have been low in vitamin D.
Other important micronutrients for cancer prevention are iodine and selenium. Poland in particular had the lowest iodine intake and among the highest stomach cancer death rates in Europe. After Poland in 1996 began a program of mandatory iodine prophylaxis, stomach cancer rates fell:
In Krakow the standardized incidence ratio of stomach cancer for men decreased from 19.1 per 100,000 to 15.7 per 100,000, and for women from 8.3 per 100,000 to 5.9 per 100,000 in the years 1992-2004. A significant decline of average rate of decrease was observed in men and women (2.3% and 4.0% per year respectively). [9]
So among the Polish Optimal Dieters, the elevated gastrointestinal cancer risk caused by mucin deficiency may have been aggravated by iodine and sunlight deficiencies.
Conclusion
A healthy diet should be robust to faults. The Optimal Diet is not robust to glucose deficiency.
There’s good reason to suspect that at least some of the Optimal Dieters developed mucin deficiencies as a result of the body’s effort to conserve glucose and protein. This would have substantially elevated risk of gastrointestinal cancers. Thus, it’s not a great surprise that many Optimal Dieters have been coming down with GI cancers after 15-20 years on the diet.
We recommend a carb plus protein intake of at least 600 calories per day to avoid possible glucose deficiency. It’s plausible that a zero-carb diet that included at least 600 calories per day protein for gluconeogenesis would not elevate gastrointestinal cancer risks as much as the Optimal Diet. But why be the guinea pig who tests this idea? Your body needs some glucose, and it’s surely less stressful on the body to supply some glucose, rather than forcing the body to manufacture glucose from protein.
Fasting and low-carb ketogenic diets are therapeutic for various conditions. But anyone on a fast or ketogenic diet should carefully monitor eyes and mouth for signs of decreased saliva or tear production. If there is a sign of dry eyes or dry mouth, the fast should be interrupted to eat some glucose/starch. Rice is a good source. The concern is not only cancer in 15 years; a healthy mucosal barrier is also essential to protect the gut and airways against pathogens.
Related Posts
Other posts in this series:
- Dangers of Zero-Carb Diets, I: Can There Be a Carbohydrate Deficiency? Nov 10, 2010.
- Danger of Zero-Carb Diets III: Scurvy Nov 20, 2010.
- Dangers of Zero-Carb Diets, IV: Kidney Stones Nov 23, 2010.
References
[1] Sonksen P, Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth. 2000 Jul;85(1):69-79. http://pmid.us/10927996.
[2] Peek RM Jr, Crabtree JE. Helicobacter infection and gastric neoplasia. J Pathol. 2006 Jan;208(2):233-48. http://pmid.us/16362989.
[3] Bornschein J et al. H. pylori Infection Is a Key Risk Factor for Proximal Gastric Cancer. Dig Dis Sci. 2010 Jul 29. [Epub ahead of print] http://pmid.us/20668939.
[4] Guang W et al. Muc1 cell surface mucin attenuates epithelial inflammation in response to a common mucosal pathogen. J Biol Chem. 2010 Jul 2;285(27):20547-57. http://pmid.us/20430889.
[5] Velcich A et al. Colorectal cancer in mice genetically deficient in the mucin Muc2. Science. 2002 Mar 1;295(5560):1726-9. http://pmid.us/11872843.
[6] An G et al. Increased susceptibility to colitis and colorectal tumors in mice lacking core 3-derived O-glycans. J Exp Med. 2007 Jun 11;204(6):1417-29. http://pmid.us/17517967.
[7] Paz HB et al. The role of calcium in mucin packaging within goblet cells. Exp Eye Res. 2003 Jul;77(1):69-75. http://pmid.us/12823989.
[8] Schmidt DR, Mangelsdorf DJ. Nuclear receptors of the enteric tract: guarding the frontier. Nutr Rev. 2008 Oct;66(10 Suppl 2):S88-97. http://pmid.us/18844851.
[9] Go?kowski F et al. Iodine prophylaxis–the protective factor against stomach cancer in iodine deficient areas. Eur J Nutr. 2007 Aug;46(5):251-6. http://pmid.us/17497074.











I definitely started noticing that my eyes got bloodshot and dry after about 9 or 10 months of eating low carb paleo (I ate lots of low carb veggies and some berries, but avoided most starchy fuits like bananas and plaintains and veggies like potatoes and sweet potatoes). From your blog, I figured out that I was likely Vitamin C deficient and started supplementing 500 mg a day, which helped quite a bit. I also started drinking a bit of orange juice here and there (I know it has fructose, but I like it and am young and relatively healthy and not looking to lose weight), and started making sure to eat some banana, potato, and/or sweet potato every day. I have DEFINITELY noticed that my eyes feel a lot better and are moist again. I, like you, was starting to have problems with my contacts, but now they feel great even at the end of the day. If my eyes felt like this, I can’t even imagine what the rest of my body was going through–unless I’m having gastrointestinal issues, I can’t really “feel” how moist my intestines are!
I worry about this issue in particular because I’ve taken Zyrtec for about 15 years (and Seldane before that before it was pulled for cardiac safety issues) for severe allergies. I’ve tried going off it, but my allergies get too difficult to handle–I get sneezy and watery eyed and get bad headaches. I know that the allergy medicine decreases saliva production in my mouth. Have you seen anything about long term allergy medicine use and gastrointestinal cancer rates? Have you run into anything about how to reverse (or at least lessen) life-long serious allergies? I know I won’t be able to stay on Zyrtec while I’m pregnant and nursing, and I’m a bit anxious about it.
Since going low-carb I’ve had issues with wearing my contacts and very dry eyes as well. I started adding back in tubers and a bit of rice and my eyes are starting to have normal moisture again.
I had a question: I was wondering if you have ever come across any evidence that there might be a connection between stomach cancer/colon cancer and Celiac disease? My Polish-American father died from colon cancer at 58. He wasn’t on the OD. He ate a typical high carb diet, plus a lot of cured meats. He had constant digestive issues, but he was never diagnosed with Celiac Disease. Last year I learned through a DNA test and fecal test for gluten intolerance that I am gluten intolerant and that my father (and my mother as well) had the Celiac gene. I too have had digestive issues for a long time. I have been totally gluten-free for a year, but that doesn’t make up for 53 years of eating gluten. I am hoping that I don’t end up with colon cancer like my father. I am 50 pounds overweight, and I have tried various low-carb/paleo/primal methods to lose the weight, but it doesn’t seem to want to come off. Thanks.
Your book is awesome, as is this blog!
A few related questions…. I realize that you don’t see vegetables don’t count as a carb source, but I wonder what your thoughts are on some of the ‘heavier’ veggies like parsnips, carrots, beets, and squash. The markets are full of them! Would they fall somewhere in the middle zone?
Also, and I realize this is a bit off topic, what about the protein content of veggies? While I realize it’s minimal, it’s still there (and, yes, I do eat a fair number of veggies), though incomplete in the amino acid profile. When you give your recommendation for protein, is it in reference only to animal proteins?
Finally, I’m wondering if once one loses weight, is it possible to require more fat/calories? Strange question, but…. The reason I ask is that I adopted a fairly paleo style of eating about 6 months ago and shed about 5-7 lbs and felt fantastic (ratios were about 55%F-23%P-22%C, though the C contained very little starch — still eat close to this, though am slowly started adding carbs back — the weight loss made me a little paranoid about them, but your book has helped clarify — hopefully the dry eyes and other issues will clear up, too). Anyway, I was feeling great — and not just because my pants were fitting better! I just felt very clear-headed and alert. Then my weight plateaued, and I wasn’t feeling so wonderful. My body fat got to/is still about 16% (I’m a 41 year old active female), so I’m guessing my body is fine with this. BUT, because my body was no longer losing fat, I lost fat as an energy source. Do you think increasing my fat would help me get back into that zone of mental clarity again (and, yes, adding real carbs)? Does my thought train/question make sense? Sorry , it’s a little off topic, but makes me wonder if I need to increase my fat?
Thank you!!
Can a diabetic eat 400 starchy carb calories and keep blood glucose levels normal?
I’m not diabetic, but my MIL is pre-diabetic, obese, and has been controlling her blood sugars by restricting carbs to non-starchy veggies.
She has a meter, so I guess she could try and see what reintroducing safe starches does to her sugars.
For myself, maybe I need to do a food diary and plug the info into one of those online counters. I’m sure I’m not eating 400 calories safe starch carb calories per day. I usually have a potato with eggs for breakfast, and that’s it.
Dr. Jaminet,
Great blog and thanks for finally tackling this topic. I’ve been waiting for this post since your comment on Peter’s blog.
I’ve been a follower of the optimal diet over the past two years since I discovered Peter’s blog. The biggest question I now have with following the diet is the amount of carbohydrates required. At first, the site that you’ve referenced is the one I was using for ratios for some time.
However, I discovered a document called, “Optimal Nutrition versus Atkins Diet”, and in the document Dr. K states that, “Nutritional recommendations based on the present biochemical knowledge stipulate a daily requirement for protein of 30 to 40g, for carbohydrates of 50g to 100g.” The lower end is close to glucose deficiency as your stated above; however, the upper end is close to your ideal ratios.
Also, while using Google translate, I read some articles on Dr. K’s website (http://dr-kwasniewski.pl/) in which he states that the 1P-2.5-3.5F-0.5C ratio should only be an introductory diet until health problems disappear or the body adjusts to the new diet. Once the body adjusts to the diet, the ratios should be in the range of 0.6-0.8P-2F-0.8-1.5C. He states that protein should be reduced to eliminate extra work by the liver, and carbs should be increased on an individual basis to keep out of ketosis. (I would link to the article, but it doesn’t work with the translation software.) These ratios are close to the ratios that you suggest.
With that being said, my questions with the high cancer rates are as follows: Could the larger percentage of cancer be occurring because they strictly follow the introductory OD ratios for long periods of time instead of adjusting to the ratios of lower protein and higher carbs after their bodies adjust to the diet? Are the dieters focusing too much on macro-nutrient ratios at the expense of micro-nutrient deficiencies? With these deficiencies causing the health problems. Finally, are they not excluding certain foods (e.g. wheat) that have a detrimental effect on health?
Now I know these questions might not be answered, but they are what I’ve been wondering about since I learned of the cancer deaths.
Thanks for the post, and I look forward to your further research.
Shane
P.S. Any idea when the Kindle/PDF version of the book will be ready?
Yeah, I thought I was really cool and in the know in my big war on insulin by eating a diet revolving mostly around fat. I lost weight and my emotions were stable at first and I had more energy. Whoopdie doo! I got fully seduced and ended up with severe indigestion problems (cured in days by pizza), decline in sexual function, severe tooth pain (perhaps from deficiency, but white flour easily clears it up so I doubt it), and other issues. Fat is great and all, but you can definitely have too much of a good thing. There are many advantages to supplying an adequate supply of glucose.
Hi Katie,
Very similar experience to mine with the carbs and vitamin C curing the dry eyes!
I haven’t heard about allergy medications causing GI cancers, but it would make sense that they would.
My wife got rid of her allergies by normalizing vitamin D. I think in general good diet and nutrition goes a long way.
Hi suzan,
I do believe there is a connection between celiac and cancers. Here’s a paper with some relevant data: http://www.ncbi.nlm.nih.gov/pubmed/21046648. Celiac doubles the risk of esophageal cancers, perhaps by causing acid reflux. Ulcerative colitis doubles the risk of colon cancer.
Joyful Fig – Thanks!
Yes, you do get carbs from carrots, beets, parsnip. But I doubt you get much from squash (only 72 calories per pound according to nutritiondata.com).
I do think we can digest plant proteins, but at least in the vegetables I eat there’s not a lot of protein, aside from potatoes and other tubers.
Definitely while you were losing weight your body was contributing a little extra fat to your “diet.” You could experiment with a little extra fat, a little less protein, and shifting the carbs from fructose toward starch. I’m not sure this would increase your mental clarity, but it might be a slight improvement in your nutrient profile.
Hi Michelle,
For diabetics we suggest the ketogenic variant of the diet, with about 200 glucose calories from starches, 400+ protein calories possibly including whey protein, and coconut oil for ketones.
A potato isn’t very much in the way of carbs.
Hi Shane,
Thanks for the info about Dr. K’s recommendations.
I think on any diet, people will vary from the recommendations in both directions. I think on very low carb diets it’s tempting to go even lower. You get out of the habit of eating carbs, and it’s easy to think that if less is good, then none is best. I wouldn’t be surprised if a lot of ODers were eating near zero-carb diets, even if that’s below Dr. K’s recommendations.
Yes, it’s certainly possible that micronutrient deficiencies are a big factor. I believe those are mainly responsible for the problems that have arisen on clinical ketogenic diets for epilepsy. And I mentioned vitamin C, vitamin D, iodine, and selenium in this post alone as possibly relevant to mucus deficiency and GI cancers.
I think the micronutrient needs on very low-carb diets are still being worked out.
There’s a lot of good about the Optimal Diet. As they say, the pioneers are the ones with the arrows in the book. As the first really popular low-carb high-fat diet, the ODers acted as guinea pigs for the rest of us. We should learn what we can from them and fix their mistakes. I still believe in high-fat diets.
And it’s ironic that ODers are dying of GI cancers, because the OD is probably therapeutic for most other cancers!
PS – Kindle. I’m sorry, I’m swamped in consulting work and haven’t gotten to it. No idea when it will be out.
Hi Matt,
Welcome! You’ve done a great job compiling stories of zero-carb troubles.
I’m not surprised by the indigestion issues developing, that fits in with the mucus deficiency idea. Certainly the chance that some problem will pop up seems to get higher as carb intake approaches zero.
I fully agree about the glucose. Not something you want to be deficient in.
I have eaten VLC for 3 years now and I have not had this dry eye problem, however I have been strictly gluten free. I seem to react to very small amounts of gluten but there are no autoimmune or digestive disorders in family family medical history. I wonder about these low gluten diets and if they are actually “optimal” for many gluten intolerants. Have you seen this study looking at mortality rates for gluten intolerants vs celiacs?
http://www.gastroendonews.com/index.asp?section_id=187&show=dept&article_id=16015#
“Mounting evidence shows that gluten sensitivity is associated with a higher risk for mortality than in the average population. In a retrospective cohort study of more than 35,000 Swedish patients, researchers found that patients with a spectrum of gluten-related disorders had an increased risk for mortality (Ludvigsson JF et al. JAMA 2009;302:1171-1178). For people with celiac disease, the absolute mortality rate was 10.4 (95% confidence interval [CI], 10.0-10.8) per 1,000 person-years; for those with inflammation but no villous atrophy in duodenal biopsies, 25.9 (95% CI, 25.0-26.8); and for those with latent celiac disease, 6.7 (95% CI, 5.7-7.6). Patients with latent celiac disease were defined by the presence of anti-tissue transglutaminase antibody, antigliadin antibodies or antiendomysial antibodies.”
Hi NoGluten,
Thanks for the link! I hadn’t seen that one. Looks interesting.
I can’t remember if it was on the blog or the book, but we did comment about a paper showing that people who DON’T develop IgA antibodies to wheat have worse health outcomes than those who do. The antibodies help clear the wheat toxins, which would otherwise build up.
Minor constipation is something that happens to me from time to time (I am trying to go for the Perfect Health Diet), but I have been eating my potatoes. I hope to hear more from you about the causes of constipation.
Hi Jeremy,
I assume you’re doing our supplements. Glutathione deficiency, vitamin C deficiency, selenium deficiency, magnesium deficiency, and hypothyroidism are all possible causes of constipation. You could try N-acetylcysteine if you’re already doing the others.
You could experiment with fiber to see if it fixes it.
Also, drink lots of water. If you’re not retaining water, you could be deficient in electrolytes – fairly common on Paleo diets. Potassium, salt, other minerals are important.
Try pressing hard on skin above bone, say on your shin. If it bounces back, then you’re well hydrated. If it leaves a depression that doesn’t bounce back, I would work on electrolytes and water.
My skin on my shin bounces back, so no worries about hydration. I’ll look into the other causes. I might need to take more selenium.
On selenium, Emily Deans posted today to this link saying that Brazil nuts have a lot of radium. Any concern on your part, as I know you eat a lot of Brazil nuts? Also, you aren’t worried about the omega 6’s in Brazil nuts?
http://www.orau.org/PTP/collection/consumer%20products/brazilnuts.htm
How does this theory explain the health of the Inuit and other healthy cultures on animal based diets that did not appear to suffer from cancer? I would think the Arctic would be the worst place to have dry eyes! Did they eat enough protein?
I’ve increased my intake of good fats, and lowered the carbs, (though I’ve never calculated the percentages). I’ve gotten rid of every type of processed food from my diet.
Rather than dry eyes, on some days my eyes tear for no reason. It’s no big thing, but what would cause the opposite of dry eyes? I don’t use contacts.
Before the dietary changes, I had a lot of eye strain which has pretty much disappeared. Yea healthy eating!
Melissa, I’ve also had problems with tearing eyes and found that large doses of vitamin C stopped the problem.
I’d be surprised if one would need 550 protein calories (137g) to maintain lean mass on a ZC diet, this paper (http://www.nutritionandmetabolism.com/content/1/1/2#IDAKYR2R) suggests 1.2-1.7g/kg and that’s in the context of athletes. That would be 84-119g for some-one at my weight.
I was also surprised that you said that the PH diet was higher in protein (75g on 2000 calories), since going by the summary on this site, you said that 200 calories (50g) was “enough.” I also interpret the OD to prescribe me a higher amount of protein: 67.5-82.5.
Re. the two prominent ODers dying of cancer, it should probably be noted that Poland does have absurdly high rates of GI cancer. When I looked into this, one study on the issue noted that all the salted sausages they eat were nothing to do with it but that “risks were positively associated with increased intake of breads/cereals/rice/pasta and other refined grains, as well as a high carbohydrate index.”
Incidentally, why are you sceptical that carbohydrate, rather than fibre is the protective element (other than your n=1 where you didn’t get along with eating only vegetables)? My first suspicion would have been that fibre (which you can’t easily avoid when eating carbs) stimulates mucus production more than pure (non-resistant) starch would. I suspect incidentally that the culture of OD dieters probably tends to an avoidance of vegetables along with the reduction in carbs, as you allude to.
Michelle,
You may be interested in my posts on various LoBAG Diets: Stands for Low BioAvailable Glucose as pertains to 400 calories of starch. I think added slowly, if one is VLC to begin with, this produces a more optimal result in the long haul.
High Protein LoBAG Diet for Type II Diabetes (20% carb which equates roughly to PH’s 400 cal recommendation), and LoBAG diets for treatment of Type II diabetes (this one compares three versions ranging from 20-40% carb).
I second David Moss’s question: the OD group’s GI cancer rate could simply be a subset of Poland’s abnormally high GI cancer rate overall and not a result of the OD. I read in an abstract that their consumption of highly processed meats was the problem but didn’t delve further.
Hi Jeremy,
We take selenium supplements most days, occasionally we use Brazilnuts as a substitute. But only 2-3 nuts per day. Omega-6 is undesirable but not an insuperable objection, as 2 Brazilnuts use up about 30% of our omega-6 quota. Radium is also undesirable but the site Emily references says they are cleared quickly from the body. That information does make me more inclined to the supplements however.
Hi Greg,
First, I don’t think anyone knows what the GI cancer rates were among the Inuit. I would expect overall cancer rates among the Inuit to be reduced, as they would be on any low-carb diet, but even there I’m not aware of good data.
It’s possible, even likely, that GI cancer rates would be lower on a high-protein diet, but this has not been adequately tested.
Hi Melissa, Thanks Robert!
@Paul, yes, one potato a day isn’t much, but I was not counting carbs from non-starchy veggies.
@CarbSane, thanks for the links. I’ll look them over, and see if I can follow.
Hi David,
Ketosis does substitute for some of those glucose and protein needs. I don’t believe that nutrient needs scale linearly with body weight – I think fixed calorie requirements are closer to the mark. I think 600 calories is a good number because it is sufficient to avoid the body’s adaptations to starvation / low nutrient intake which reduce nutrient usage — and which are not necessarily healthy in the long run.
Also, keep in mind that glucose needs vary among persons. Chronic infections increase glucose needs significantly and it seems to be people with chronic infections who run into the most problems on very low-carb diets. When my infections were at their most severe I couldn’t even tolerate a 12 hour overnight fast.
Re our diet, we have healthy ranges which for protein is pretty wide, 200 to 600 calories per day, or roughly 10% to 30% of calories. Our typical “mid-range” recommendation is 400 carb calories, 300 protein calories, but you can adjust that to your taste and personal needs.
I think we need someone to gather statistics on the ODers to see exactly how elevated their GI cancer rates are. I am going by the statements of Flo on Peter’s site implying that GI cancer rates among ODers are elevated even by Polish standards.
I do think wheat elevates GI cancer risk but since ODers were eating less of it, that shouldn’t be the primary cause of their cancers. A low-carb diet that stuck to our “safe starches” only would be healthier, but I don’t believe that that would eliminate the GI cancer risk.
Fiber is an interesting question. Yes, it’s possible that reduced fiber intake is a factor in the GI cancers. But I don’t think that would affect stomach cancer rates — only colorectal cancers. And half of our known cases are stomach cancer.
Also, I am not completely sold on a fiber-rich diet and diverse abundant gut flora being necessary for gut health. Infants do well on a breast-milk-only diet with an extremely limited gut flora.
Fiber does stimulate mucus production … but it also increases gut bacterial populations. Pathogens and bacterial toxins are risk factors for cancer. We need more evidence about how these interactions play out on different diets.
So, a lot of avenues for further study. One goal of this series is to generate hypotheses which maybe biomedical researchers will pick up on and investigate.
Best, Paul
Hi Lacie,
As I said, we need an epidemiological investigation to get good statistics, but the anecdotal accounts are that GI cancers are elevated among ODers compared to other Poles.
Highly processed meats are a danger, probably due to AGEs, and it’s plausible that ODers were eating more of them than other Poles.
@ Melissa,
Excess tears can also be a symptom of ‘dry eyes’. The mucus layer of the eyeball is there to hold moisture to the surface of the eye. If it is deficient, then your body compensates by producing more tears in an attempt to keep the eyeball moist.
I’ve been suffering from dry eyes for over 2 years now, and have seen 6+ doctors, (incl 2 opthalmologists).. none of whom have helped at all, and none of them bothered to ask me about my diet. After following Paul’s advice to increase my glucose and Vit C intake*, I can honestly say that my eyes are 90% better, and getting better each day.
* although I’ve been generally low carb/paleo for 2 years, I just recently started taking the supplements suggested by the Perfect health diet, so I can’t be certain exactly what helped improve my dry eye condition.
thanks again Paul, for you help.
Great point, Pete, you need the mucin sugars to hold the tears in the eye. Otherwise the water just dribbles out.
I don’t see why glucose shouldn’t correspond at least somewhat to body weight. When we eat glucose or foods that are converted to glucose, the glucose is quickly released into the blood, and our bodies work to keep the concentration at an acceptable level, a process that takes a few hours after a meal. The concentration depends on the volume, however, and bigger people have a greater volume of blood and interstitial fluid. Protein is needed for the repair of all tissues, and the bigger the organism, the more tissue there is to repair. So it makes sense that protein and carb “requirements” should depend on weight.
I’m on the OD, or at least the macronutrient ratios part of it. My goal weight is about 93 kg, which means I should get about 93g/day of protein. The OD prescribes either .5g or .8g per day of carb for each gram of protein, so that has me between 46 and 73g/day. I use that as a range, rather than trying for a specific carb target each day. As a result, my daily carb+protein intake is generally pretty close to 150g, or 600 calories. If my goal weight were less, it would of course be less than that but, as I argued above, it only makes sense that it would.
Hi Ubizmo,
The major glucose-consuming parts of the body are brain and nerves, gut, immune system, red blood cells, kidneys, and a few others. These scale slower than linearly with body mass.
Volume of the blood isn’t a big factor. There is a total of 5 g / 20 calories glucose in the blood, less than one hour’s needs.
I think your carb plus protein intake is safer than the levels the OD would recommend to a smaller person.
The Inuit actually eat a great many plants. This has been documented by botanist Anore Jones. Jones is with the US Fish and Wildlife Service and has spent the last 40 years saving food lore and recipes from the Inupiat of northwest Alaska. Her book, “Plants That We Eat,” is a guide to the abundant edible plant life of Alaska. From the Amazon description: Drawing on centuries of knowledge that have kept the Inupiat people healthy, the book uses photographs and descriptions to teach newcomers to the north how to recognize which plants are safe to eat. Organized by seasons, from spring greens through summer berries to autumn roots. http://www.amazon.com/Plants-That-Eat-Niginaqtaut-traditional/dp/1602230749
To clarify, when you say you suspect a high protein diet (referring to Inuit, above) are likely to be less GI-cancer-promoting, do you mean because, unlike in the OD, the protein(+carbs) would now total more than 600 calories, and thus not be glucose deficient?
Presumably, this would also allow for sufficient glucose to synthesize mucins?
However, there still may be a case for reduced mucin production on a low carb diet. I am not a biochemist, but from what I understand, mucin production and colon health is enhanced by (dependent on?) butyrate, which can be scarce on a low carb, low fiber diet, since butyrate is made by gut bacteria from undigested carbohydrate. The only other source I’m aware of is butter.
Now that I’m poking around, it seems that butyrate might be made from undigested protein as well, even though the literature seems focused on resistant starches.
Two other things that people on the OD may do that leads to cancer: lots of omega 6 oils and heat/smoke damaged meats/fats.
Hi Gary,
Thanks much. I knew that the Inuit ate plants when seasonally available and use them in soups and other dishes, but don’t know how much carbs and nutrients they got. It’s nice to find a resource.
Hi Amber,
Yes, the idea is that 600 calories protein would at least provide sufficient substrates for gluconeogenesis. However, that may not be the only bottleneck for glucose production, so I don’t know that high protein makes the zero-carb diet safe.
The butyrate-mucin-protein connection is interesting, thanks for suggesting it.
Hi Dan,
Yes, agreed.
I’m enthralled by this post and wonder if you could contextualize this for me to people who are doing the Specific Carbohydrate Diet (SCD) for inflammatory bowel disease. This diet doesn’t allow for starches, grains, lactose, but veggies, fruits, honey, butter, meat are all allowed.
I’m having trouble seeing where the SCD fits into this picture. It’s not low carb per se, but it is zero starch. What advice do you have for us on the SCD?
Hi Matt,
Well, we have a few points of difference with the SCD. We don’t think the problem is with starch per se but rather with the toxic proteins that starchy plants often contain. Thus, we recommend eliminating nearly all grains and legumes, which are relatively toxin rich. However, we think most tubers are fairly non-toxic upon cooking, and can be included.
That said, pathogen activity in the bowel is increased by high fiber diets, and so for many IBD patients with bad gut flora it is desirable to reduce fiber/carbs, and re-orient plant food intake toward foods with antibiotic or anti-biofilm activity like cranberries, berries, spices, some vegetables, even honey. Meats and fats are fairly benign.
Bowel diseases are a bit complicated. We did a bowel disease series last summer – click on “Bowel Disease” in the Categories list. That covers the basics. But definitely there are a lot of fine points we didn’t cover.
Bowel diseases are also variable — no one’s disease is quite the same. Some benefit from fiber to help commensal bacteria, others benefit from starvation of pathogens. I would suggest reading our book in combination with GAPS or SCD diet advice and then experimenting to see what works best for you.
Best, Paul
You never removed the vegetables from you diet you only added back carbs and assumed that was the reason for the dryness. Perhaps if you had removed the plant matter instead of adding carbohydrates the dryness issue would have gone away.
Darn those confounding variables.
Hi Bill,
I did try cutting vegetables. That had nothing to do with it. Vitamin C and glucose — I did many experiments, turned it on and off at will, it was very clear.
Do you consider nuts such as filberts and almonds and pistachios etc and seeds such as pumpkin etc to count as “starch” since they contain carbohydrate and are not green veggies? If so, do you advocate toasting them or eating them raw?
Paul,
Do you believe itss the glucose that is essential to cure the mucus deficiency or the glyconutrients present in many fruits and starches. It would be interesting if a food like white rice alone could solve the problem (or if we really do benefit from some fruit consumption <— doesn't seem like vegetables here would do the trick).
Also, I'd be interested in your take on Matt's ideas at 180 degree health — that high starch low sugar consumption with low polyunsaturates can really speed up your metabolism. I still don't think you have a clear cut answer to why there are many healthy high carb cultures that don't seem to have issues with a low intake of choline or fat for that matter (especially when you expose eating high fat at the expense of carbs). It's also interesting to think that most high fat followers might have a problem with eating high quality animal fat that is apart from high protein consumption <—- which may be something people do not want.
Hi Annie,
Toasting is safer but some nuts are fine raw. Most nuts tend to have more sugar (half fructose) than starch (all glucose) so we would not consider them as starches.
Hi Aaron,
I do believe it’s the glucose. White rice fixes dry eyes very quickly for me.
Matt’s diet advice is mostly good. We are advocates of “safe starches” and recommend minimizing fructose and PUFA intake. I think “speed of metabolism” is a very complicated subject and it’s not just a simple function of starches, sugars, and PUFA, but Matt’s diet advice is fairly healthy. I would avoid wheat flour however.
The healthy high carb cultures I’m aware of, like the Kitavans, eat seafood and eggs and mushrooms, so they do get choline. Now, it does seem that high carb diets reduce the need for choline. But I don’t know the mechanism.
I’m not quite sure what the problem is that you’re alluding to in the last sentence. We eat relatively low protein intake (~10-15% of calories) and get sufficient choline (we believe) from a mix of sources.
Paul,
What would you recommend for yeast overgrowth and your thoughts on the standard candida diet of eliminating starches? Im hesitant to do so, yet really needing to reduce yeast overgrowth symptoms brought on by antibiotics and years of disordered eating.
Thanks!
Devi
Thanks for the reply, Paul! Will give it a shot…. 🙂
Hi Devi,
I’ve been struggling with yeast myself. It’s much better than it was but not gone — once it gets entrenched it’s hard to get rid of.
The best thing I’ve found is cranberries, which are in season now. I’m eating a half pound raw cranberries a day. Other berries are also good – blackberries for instance. And many spices. Coconut oil is good.
I think you should have some starches, but rice is best. You need glucose for the immune response to fungi, but they’ll benefit from resistant starch that reaches the colon. Chew the rice well, expose it to saliva, and it should be digested and absorbed in the small intestine.
I also think intermittent fasting helps.
Here’s a page with some antifungal remedies: http://cpnhelp.org/antifungals_and_probiotic.
Intermittent fasting seems to help.
I was looking on amazon today for coconut oil. Nutiva (mentioned in earlier comments a couple of times) is obviously a good bet, but I was wondering if anyone has any experience with Paragon brand. It’s about half the price per ounce. It says it’s for popping corn, but as far as I can tell there are no additives besides beta-carotene for coloring. Just trying to save a bit of money on this ketogenic thing :).
http://www.amazon.com/Paragon-Coconut-Popcorn-Popping-Gallon/dp/B002YLI9E2/ref=cm_cr_pr_product_top
Hello Mr. Jaminet,
Thank you for sharing with us your ideas. This blog is really informative.
I wonder if there was any difference if I was obtaining the required daily 400-600 carbohydrates calories from dairy/yogurt rather than from healthy starches?
thank you!
George
Wouldn’t raw nuts be safer than roasted? You’d think the roasting would oxidize some of those omega-6s.
Hi Paul, Thank you so much for sharing your knowledge with everyone, especially when the search for the perfect diet is something that many of us are looking for.
2 quick questions:
Which type of vitamin C do you recommend? (in supplement form)
I´m currently eating 2 sweet potatoes a day as my starch source, my hand & feet soles are orange(carotenosis I guess?),is the high betacarotene intake something to worry about?
Thank you,
Best
Marc
This discussion about glucose deficiency is particularly fascinating and important for me. I have diabetes type 2 (DT2) which I manage through a low carb diet along the lines of the excellent website and book Blood Sugar 101 and the publications of Dr Bernstein. The key strategy is to restrict carbs to prevent post meal BG spikes.
For me this means that I can’t eat more than around 15 or 20 grams of carbs at a meal (mostly from green and non-starchy vegetables, cheese and yogurt), and pretty much zero at breakfast due to the dawn phenomenon, without blowing my blood glucose unacceptably high. With snacks I typically consume around 20-40 grams per day (not counting fibre).
There is nothing borderline about my diabetes. At diagnosis my a1c was 10. Hence I expect to be doing this sort of low carb diet for life, which I hope will be several more decades. The only alternatives for me are toxic BG levels with very clear and catastrophic long term consequences, toxic drugs, or elaborate and difficult insulin protocols. Obviously perfect health is not really within reach for me, but I still want as good as I can get!
The group of people participating in this discussion is incredibly well informed and thoughtful. It would be tremendously useful if some of you could turn a thought to strategies that people who just don’t have an option of consuming 100g+ of carbs per day can use to avoid the some of the potential negative consequences. For example, what I am hearing from Paul is that I need 600 calories of carbs plus protein to support adequate gluconeogensis, so I need to be eating around 150 of protein a day. That is very useful information.
Incidentally at what non-zero carb intake would glucose deficiency cease to be an issue? Do I need to worry at 10g but not really at 30g? For me these options involve measurable differences in BG which I need to trade off against the possible consequences of glucose deficiency.
Paul – because I have a pretty much non-existent first phase insulin response I am a very sensitive glucose detector. I can confirm that leafy green vegetables have an almost negligible accessible glucose content as I can eat well over 100g with essentially no impact on BG. However, many other non-starchy vegetables definitely supply glucose to the bloodstream when consumed in normal amounts, including especially onions, tomatoes, carrots, peas and snow peas. So do most berries and nuts.
Hi D Williford,
No experience with that product, but usually coconut oil intended for cooking usually doesn’t taste that good by itself. Also, we advise against supplemental beta carotene, which has increased mortality in clinical trials.
But cheaper is valuable. If you give it a try, let us know your opinion!
Hi George,
Our carb range is 200 to 600 calories per day; 400, middle of the range, is a recommendation for most people.
Dairy/yogurt sugars are fine, just watch out for sensitivity to the proteins that come with them. We recommend avoiding milk but we do eat yogurt. Also, keep an eye on added fructose in your yogurt.
Hi Poisonguy,
Yes, heat will denature some of the fats, but may detoxify some of the proteins. We need some clinical research to figure out which is better.
Hi Marc,
Vitamin C – any kind will do. We go with cheapest.
Carotenoids – In studies the mixed carotenoids found in food are associated with improved health, beta carotene in isolation from supplements damages health, perhaps by blocking absorption of other carotenoids.
It’s probably prudent to diversify your starches a little. If there is toxicity, eating the same food in large quantities day after day will produce it.
One thing we really like is the Asian sweet potato. It has a yellow, not orange, color and a delightful chestnut flavor. Asian supermarkets generally have it, it is popular in Japan and Korea. I would assume from the yellow color that its beta carotene content is smaller.
If you eat egg yolks, that will also diversify your carotenoid intake.
Hi ForInfo,
This is a great topic and I think I’ll be doing a blog post on it shortly.
If you look back in the comments to the first post in this series, Nigel Kinbrun (http://perfecthealthdiet.com/?p=1032#comment-7079) gave us a link to a professor’s exposition asserting that when basal insulin is eliminated by Type I diabetes, then glucose production shoots up from 400 calories per day to 1600 calories per day.
In normal people, the 400 calorie per day limit seems to be enforced even during starvation, as a way to conserve protein.
In your Type 2 diabetes, if insulin is also suppressed sufficiently, glucose production might be over the needed 600 calories per day and you may have no risk on a zero-carb diet. Do you know your fasting insulin levels? How close to zero do they go?
Of course, you also have the issue that protein needs some insulin for proper metabolism. Do you have issues with protein-rich meals?
I do believe you should aim for at least 600 calories protein plus carbs to prevent risk of lean tissue wasting. One way or another, your body needs these calories.
Our book recommendation for diabetics is the 200 carb calorie / 400 protein calorie diet, but maybe we should modify that carb level lower in the special case of “non-existent insulin” diabetics.
We also recommend ketogenic diets for diabetics. That involves taking some coconut oil (ketogenic fats) and also favoring ketogenic amino acids (such as in whey protein).
You can see in papers like this one: http://www.jbc.org/content/236/11/2868.full.pdf that ketogenic amino acids like phenylalanine do very little to raise blood glucose.
Also, vitamin B6 (for transamination) and biotin are needed in gluconeogenesis, so you should add these to your supplement list.
Paul,
Thank you for the reply and links re: yeast issues. Interestingly, some of the info in the links mentions that caprylic acid can be an irritant to the GI tract, does this translate to coconut oil having a similar irritant impact–Im currently up to 4-5 TBSP a day with a very fragile gut.
Also wondering why white rice is the best starch for candida overgrowth, in terms of resistant starch would white/sweet potatoes be equally effective or are these discouraged with yeast issues?
Lastly, Im having trouble digesting anything raw at this point, do cooked cranberries/cranberry juice have the same antifungal impact?
Thanks again,
Devi