Alan Smith’s remarkable recovery from a seemingly fatal infection, discussed here and here, thanks to administration of 100 g/day vitamin C over vigorous opposition from his doctors, highlights both the slow pace of medical progress and the potential benefits of natural healing methods that cooperate with human biology.
The doctors’ adamant opposition to vitamin C treatment is hard to fathom. There is ample clinical experience demonstrating that high doses of vitamin C can help the body defeat viral infections. Moreover, it is among the safest of known interventions.
Vitamin C in Animals
Vitamin C apparently first developed in plants and land animals about 500 million years ago. An ability to synthesize vitamin C has been retained by most land animals and birds. [1]
Over 4,000 species of mammals can synthesize vitamin C from glucose. In good health, mammals synthesize the equivalent in humans of 2 to 13 g/day; under disease or stress, vitamin C synthesis increases up to 100-fold. [2] Under such conditions, vitamin C synthesis may constitute over 90% of glucose utilization – placing a heavy burden on the liver and arguing that vitamin C must have exceedingly important functions in diseased and stressed states.
Three times in mammals – in bats, certain rodents (guinea pigs and capybaras), and the Haplorrhini branch of the primates (containing tarsiers, monkeys, apes, and humans) – the ability to synthesize vitamin C was lost. [1] The loss in the Haplorrhini line was triggered by a retroviral infection about 60 million years ago.
The loss of vitamin C must have had a selective advantage at the time in order to triumph. Whether that selective advantage would still hold today is unknown. Since most Haplorrhini today obtain the human equivalent of 1 to 4 g/day of vitamin C from diet, it’s plausibly the case that any advantage from loss of C synthesis would hold only for those obtaining gram doses of vitamin C through diet or supplements.
Clinical Experience With High-Dose Vitamin C Therapy
A few unconventional doctors have generated most of the clinical experience with high-dose vitamin C therapy.
Fred R. Klenner, a general practitioner from Reidsville, North Carolina, was the pioneer. In the 1940s and 1950s, he found that viral diseases, notably pneumonia and polio, could be cured or greatly improved by intravenous sodium ascorbate of up to 200 g/day. (He favored the pH-neutral sodium ascorbate over conventional acidic versions.) Vitamin C was first isolated in 1932 and first synthesized in 1934, so Klenner was a very early adopter. [3]
Klenner’s maxim was that the patient should “get large doses of vitamin C in all pathological conditions while the physician ponders the diagnosis.” [4]
Irwin Stone and Linus Pauling popularized vitamin C therapies in the late 1960s and early 1970s.
Persuaded by Stone and Pauling, a doctor named Robert Cathcart, who had previously invented an improved artificial hip, began using high-dose vitamin C when he took up general practice in Incline Village, Nevada.
He soon made an interesting discovery:
In 1970, I discovered that the sicker a patient was, the more ascorbic acid he would tolerate by mouth before diarrhea was produced. At least 80% of adult patients will tolerate 10 to 15 grams of ascorbic acid … The astonishing finding was that all patients … can take greater amounts of the substance orally without having diarrhea when ill or under stress. [5]
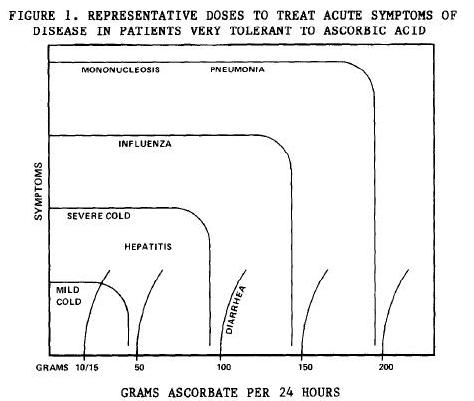
Cathcart presented this figure showing how various diseases affected vitamin C tolerance:
Over the next two decades, Dr. Cathcart treated over 12,000 patients with high-dose vitamin C. He found that vitamin C “markedly alters the course of many diseases.” [3] In his experience, Dr. the limit of bowel tolerance was a “convenient and clinically useful measure of ascorbate need”:
The maximum relief of symptoms which can be expected with oral doses of ascorbic acid is obtained at a point just short of the amount which produces diarrhea. The amount and timing of the doses are usually sensed by the patient. The physician should not try to regulate exactly the amount and timing of these doses because the optimally effective dose will often change from dose to dose… The patient tries to TITRATE between that amount which begins to make him feel better and that amount which almost but not quite causes diarrhea. [5]
Recall that in animals, vitamin C synthesis rises as much as 100-fold under disease. In humans, the limit of bowel tolerance rises up to 20-fold during illness. This suggests that bowel tolerance limit is an indicator of need.
Dr. Cathcart found that vitamin C was helpful in combination with antibiotics against bacterial infections:
The effect of ascorbic acid is synergistic with antibiotics and would appear to broaden the spectrum of antibiotics considerably….
A most important point is that patients with the bacterial infections would usually respond rapidly to ascorbic acid plus a basic antibiotic determined by initial clinical impressions. [5]
Unfortunately, vitamin C didn’t help much against fungal infections:
Although ascorbic acid should be given in some form to all sick patients to help meet the stress of disease, it is my experience that ascorbate has little effect on the primary fungal infections. Systemic toxicity and complications can be reduced in incidence. [5]
Overall, Dr. Cathcart’s experience was that benefits of vitamin C therapy could be huge.
The method produces such spectacular effects … as to be undeniable. [5]
It’s Not Easy to Test Vitamin C In Clinical Trials
Cathcart notes:
Either this titration method or large intravenous doses are absolutely necessary to obtain excellent results. Studies of lesser amounts are almost useless. The oral method cannot by its very nature be investigated by double blind studies because no placebo will mimic this bowel tolerance phenomenon. [5]
The Danger of Induced Scurvy
I developed scurvy at the nadir of my own chronic infection, so I pass this from Dr. Cathcart along as a warning:
Well-nourished humans usually contain not much more than 5 grams of vitamin C in their bodies….
If a disease is toxic enough to allow for the person’s potential consumption of 100 grams of vitamin C, imagine what that disease must be doing to that possible 5 grams of ascorbate stored in the body. A condition of ACUTE INDUCED SCURVY is rapidly induced. [5]
Anyone with a chronic infection, certain or suspected, should be careful to supplement gram doses of vitamin C.
How Does Vitamin C Work?
Dr. Cathcart’s explanation for the benefits of high-dose vitamin C is that exogenous vitamin C comes with high-energy electrons suitable for transfer to the molecules involved in respiratory bursts:
Conventional wisdom is correct in that only small amounts of vitamin C are necessary for this [antioxidant] function because of its [recycling and] repeated use. The point missed is that the limiting part in nonenzymatic free radical scavenging is the rate at which extra high-energy electrons are provided through NADH to re-reduce the vitamin C and other free radical scavengers. When ill, free radicals are formed at a rate faster than the high-energy electrons are made available. Doses of vitamin C as large as 1-10 g per 24 h do only limited good. However, when ascorbate is used in massive amounts, such as 30-200+ g per 24 h, these amounts directly provide the electrons necessary to quench the free radicals of almost any inflammation. Additionally, in high concentrations ascorbate reduces NAD(P)H and therefore can provide the high-energy electrons necessary to reduce the molecular oxygen used in the respiratory burst of phagocytes. In these functions, the ascorbate part is mostly wasted but the necessary high-energy electrons are provided in large amounts. [6]
This explanation would be consistent with cell biology studies showing that vitamin C is consumed rapidly during phagocytosis:
The high concentration of ascorbate in leucocytes and its rapid expenditure during infection and phagocytosis suggests a role for the vitamin in the immune process. Evidence published to date shows an involvement in the migration and phagocytosis by macrophages and leucocytes … [7]
However, other mechanisms have been proposed by which vitamin C may support immunity:
- Another early view was that vitamin C helps by destroying histamine, which may be produced in excess under conditions of stress. [8]
- A 2008 paper from Japan points to a third mechanism: that the oxidized form of vitamin C, dehydroascorbate, has strong antiviral activity in vitro. It may be that the benefit from ingesting high-dose vitamin C comes not from the C itself, but from higher levels of its oxidized waste product, dehydroascorbate [9].
The Japanese finding may supply the best explanation for why, in clinical experience, vitamin C is most effective against viral infections. Phagocytic respiratory bursts are more important for bacterial than viral defense.
Since animals upregulate ascorbate production under all kinds of stress, not just viral infections, it seems probable that vitamin C aids health by multiple pathways, not only by antiviral activity.
Safety
Vitamin C is extremely safe. Intravenous doses of 120 g/day given to cancer patients have been well tolerated. [10]
One of the reasons doctors give for avoiding vitamin C is fear that it might cause kidney stones. However, Cathcart believed vitamin C was beneficial for kidney stones:
It is my experience that ascorbic acid probably prevents most kidney stones. I have had a few patients who had had kidney stones before starting bowel tolerance doses who have subsequently had no more difficulty with them. Acute and chronic urinary tract infections are often eliminated; this fact may remove one of the causes of kidney stones. [5]
Veterinarians Aren’t Afraid to Supplement Vitamin C
In animals such as chickens that lack the ability to synthesize vitamin C, vitamin C is recognized as a means of supporting bacterial and viral immunity. [11]
Conclusion
Based on Cathcart’s testimony, thousands of patients with infectious diseases have benefited from high-dose vitamin C. Although mechanisms are not well understood, vitamin C probably helps along multiple pathways.
A well-tested therapeutic strategy would be to take 4 g vitamin C every hour with water until bowel intolerance is reached. The therapy is extremely safe, and its effectiveness is usually apparent within days.
Given its safety and the ease of testing its effectiveness, why shouldn’t every seriously ill person try this therapeutic strategy? Is there any good reason NOT to try it for at least a few days to see if it has an effect?
References
[1] “Vitamin C,” http://en.wikipedia.org/wiki/Vitamin_C.
[2] Lewin S. Vitamin C: its molecular biology and medical potential. New York: Academic Press, 1976, p 109. Cited in Ely JT. Ascorbic acid role in containment of the world avian flu pandemic. Exp Biol Med (Maywood). 2007 Jul;232(7):847-51. http://pmid.us/17609500. Full text: http://ebm.rsmjournals.com/cgi/content/full/232/7/847.
[3] Klenner FR. Massive doses of vitamin C and the virus diseases. South Med Surg. 1951 Apr;113(4):101-7. http://pmid.us/14855098.
[4] “Fred R. Klenner,” http://en.wikipedia.org/wiki/Fred_R._Klenner
[5] Cathcart RF. Vitamin C, titrating to bowel tolerance, anascorbemia, and acute induced scurvy. Med Hypotheses. 1981 Nov;7(11):1359-76. http://pmid.us/7321921.
[6] Cathcart RF. A unique function for ascorbate. Med Hypotheses. 1991 May;35(1):32-7. http://pmid.us/1921774.
[7] Thomas WR, Holt PG. Vitamin C and immunity: an assessment of the evidence. Clin Exp Immunol. 1978 May;32(2):370-9. http://pmid.us/352590.
[8] Nandi BK et al. Effect of ascorbic acid on detoxification of histamine under stress conditions. Biochem Pharmacol. 1974 Feb 1;23(3):643-7. http://pmid.us/4132605.
[9] Furuya A et al. Antiviral effects of ascorbic and dehydroascorbic acids in vitro. Int J Mol Med. 2008 Oct;22(4):541-5. http://pmid.us/18813862.
[10] Riordan HD et al. A pilot clinical study of continuous intravenous ascorbate in terminal cancer patients. P R Health Sci J. 2005 Dec;24(4):269-76. http://pmid.us/16570523. Hoffer LJ et al. Phase I clinical trial of i.v. ascorbic acid in advanced malignancy. Ann Oncol. 2008 Nov;19(11):1969-74. http://pmid.us/18544557.
[11] Andreasen CB, Frank DE. The effects of ascorbic acid on in vitro heterophil function. Avian Dis. 1999 Oct-Dec;43(4):656-63. http://pmid.us/10611981.











Recent Comments