Here’s what caught my eye this week:
[1] Interesting posts this week: Do people biangulate? Chris Highcock gives us more reason to use a standing desk. A question I never would have seen before reading PaleoHacks: “Do you brush your teeth with bacon?” Peter notes mice that become obese on a “high-fat diet” can lose weight rapidly if their diet gets even fattier.
Dr. John Briffa discusses the link between HbA1c and mortality (also discussed in our book) and the vast scale of publication bias in medical journals. The issue of publication bias has a counterpart among the public which we might call readership bias. Once people become convinced something is good, they are reluctant to credit evidence that it may be bad. So, for example, the genuinely good evidence in favor of omega-3s can retard acceptance of evidence for harmful effects in some contexts.
Emily has a great post on the links between diet and violence . Mark’s Daily Apple has a nice overview of some things I’ll be talking about in the months to come – traditional cooking herbs.
Via O Primitivo, a Mediterranean diet reduces risk of cancer by 4%. I think we can do better than that.
Last week, when Gary Taubes reported his cholesterol, he also reported his diet:
I do indeed eat three eggs with cheese, bacon and sausage for breakfast every morning, typically a couple of cheeseburgers (no bun) or a roast chicken for lunch, and more often than not, a ribeye or New York steak (grass fed) for dinner, usually in the neighborhood of a pound of meat. I cook with butter and, occasionally, olive oil (the sausages). My snacks run to cheese and almonds.
This week, Anthony Colpo disapproves — twice.
Via Craig Newmark, pro surfer Laird Hamilton has a health tip:
One of my favorite things to do in the morning is to stand on golf balls and roll them along my arches. You have seventy-four hundred nerve endings on your feet, so you stimulate your whole metabolism when you do that.
[2] Is the DHA-cancer connection drug-driven?: Via Dennis Mangan, I’m informed of a helpful comment on the Brasky study by commenter Karl at FuturePundit. Key points: Half of the subjects in the study were on the drug finasteride (Propecia, Proscar). The finasteride arm had 78% more high-grade cancers than the placebo arm.
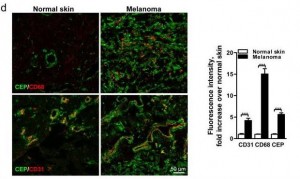
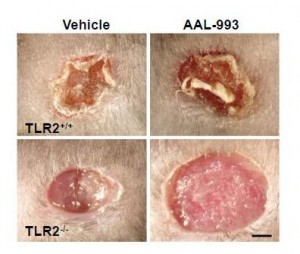
While tissue DHA levels were strongly associated with high-grade cancer, EPA levels weren’t. On the one hand this is consistent with our idea that high tissue DHA drives cancer via the DHA-angiogenesis mechanism we’ve been discussing: only DHA, not EPA, produces high-grade cancer.
However, normally tissue DHA and EPA are obtained from food and levels go up or down together. Few people in the study supplemented DHA alone; so DHA and EPA levels should have been high or lower together and both should have shown the association.
A plausible explanation would be that the drug was raising DHA levels artificially, and triggering high-grade cancers.
Unfortunately the study doesn’t report the level-response relationship between DHA and high-grade cancers separately in the finasteride and placebo arms – only in the two groups combined. I see this as a failure of the reviewers and an embarrassment to the authors.
Taking Propecia for an enlarged prostate may be much more dangerous than eating salmon.
This plausible hypothesis makes me more comfortable maintaining our recommendation to eat a pound of cold-water marine fish per week.
[3] Vanishing symbol of love: Will the turtle dove disappear?
[4] At least we’ll still have kittens:
Via Yves Smith.
[5] Heh, heh: Denise Minger says we “make DHA seem a little fishy.”
[6] Stabby hearts Denise!: They’d make a cute couple. I can see them 20 years from now:
[7] Because the purpose of government is to harass the citizenry: Feds sting Amish farmer for selling raw milk locally. Via Liberation Wellness.
[8] Carbs for weight loss: Barbra is worried that adding carbs to her very low-carb diet to fix her dry eyes might prevent weight loss. The experience of NourishedEm at Mark’s Daily Apple forum may reassure her:
I find it really interesting that a lot of us who’ve been at this for 6 months or more are finding that we do better with more starch.
When I started PB, I was all about the sub 30g of carbs as my main aim was to lose weight. Well, 7 months of that saw me lose precisely nothing. In the last 6 weeks (after having read PHD), I have added potatoes, rice, taro and sweet potatoes to my diet; in addition I have started eating in a 6 hour eating window. I’ve been losing 2-3lbs a week ever since, it’s like a magic formula for me!
The best part is no longer having to think so hard about what to eat. A lot of ‘normal’ foods have made their way back into the roster with the addition of more starch. I use rice noodles as pasta and can have carbonara and bolognaise again, a baked potato stuffed with chilli and cheese is a great, quick meal, asian stir fries, sushi, risotto, etc….
(Related: Perfect Health Diet: Weight Loss Version, Feb 1, 2011.)
[9] Kate did the wrong diet!: She ate the Dukan Diet before her wedding.
As it happens, I had a correspondent who got very sick on the Dukan Diet; it seems to have re-activated a dormant infection. I rather agree with this nutritionist:
[10] McDonald’s diet produces big baby: What strikes me about this Daily Mail story is that their measure of a baby’s health is its size:
When Suzanne Franklin fell pregnant, she was at a loss as to how she would eat for two.
The 23-year-old had suffered from extreme food allergies for years from eggs to dairy and fruit and vegetables.
Burger baby: Suzanne Franklin and baby son Harry with a Big Mac, which helped sustain both of them during Suzanne’s pregnancy
Doctors warned her that pregnancy would make the symptoms worse but that antihistamines could harm her baby.
But Ms Franklin knew she wasn’t allergic to McDonald’s burgers – so she ate a Big Mac burger everyday throughout her pregnancy.
Any worries about her unusual diet affecting her baby’s growth were unfounded – as she has given birth to her own 10 lb 2 oz whopper.
Miss Franklin said: ‘All those burgers definitely didn’t do him any harm. It was the only thing I could eat safely during my pregnancy, so I just lived on them….
Baby Harry is now three months old – and he has shown signs of inheriting Miss Franklin’s allergies too. He is already allergic to seven different types of milk.
Via John J. Ray.
[11] Has science degenerated?: Bruce Charlton, former editor of Medical Hypotheses, reflects on the negative consequences of the professionalization of science:
There is a dark side to science … in the sense that science is done for reasons of power rather than love.
There was a time when science really was done – mostly – for love; by people who loved knowledge, and were not intending to *use* it….
[O]riginally even medical science was done for love, by doctors and other clinicians, as an overflow from their practice: they wanted to understand, not to control.
As a by-product, in practice, the old medical scientists actually made more frequent, more useful, more powerful discoveries than we do nowadays …
[12] He doesn’t even need 30 bananas: This guy hasn’t stopped bicycling all day:
Via Zero Hedge.
[13] Money does buy happiness!: According to a new review in the Lancet by Bill Easterly.
[14] Another reason not to eat at the Road Kill Café: The New York Times reports that Armadillos Can Transmit Leprosy to Humans, Federal Researchers Confirm:
Armadillos have never been among the cuddly creatures routinely included in petting zoos, but on Wednesday federal researchers offered a compelling reason to avoid contact with the armored animals altogether: They are a source of leprosy infections in humans.
Using genetic sequencing machines, researchers were able to confirm that about a third of the leprosy cases that arise each year in the United States almost certainly result from contact with infected armadillos. The cases are concentrated in Louisiana and Texas, where some people hunt, skin and eat armadillos.
[15] Ella Fitzgerald: Born on April 25, she deserves a listen:
[16] Celiacs do react to oats: This came up long ago in a comment thread. It turns out that some varieties of oats do trigger gluten autoantibodies.
[17] Shou-Ching’s photo-aphorism project: Shou-Ching likes photography and her latest art project is to combine her photograph with an apposite aphorism. Here’s one – click to enlarge:
[18] Weekly video: The Aurora by Terje Sorgjerd.
The Aurora from Terje Sorgjerd on Vimeo.


















Recent Comments