A while back I noted that hypothyroidism is a circadian rhythm disorder and that dietary steps that restore circadian rhythms, like intermittent fasting and daytime eating, should be therapeutic (“Intermittent Fasting as a Therapy for Hypothyroidism,” Dec 1, 2010).
Many other disorders besides hypothyroidism feature disturbed circadian rhythms:
- Sleeplessness and poor sleep
- Depression, bipolar disorder, and other psychiatric disorders
- Dyslipidemia, metabolic syndrome and obesity.
- Neurodegenerative disorders
Circadian rhythm disruption also suppresses immune function and increases vulnerability to infectious disease.
Restoring or strengthening circadian rhythm may be therapeutic for all of these conditions. Even for healthy people, tactics for enhancing circadian rhythms may improve health.
Which brings us to Seth Roberts.
Seth Cured a Sleep Disorder With Circadian Therapy
Seth is a well-known blogger, a Paleo dieter and psychologist, author of The Shangri-La Diet, and a great self-experimenter.
Seth recently gave a talk that tells the history of his self-experimentation.
It turns out he suffered from disturbed sleep for many years. He experimented to find cures for 10 years; nothing worked. But then he got a lead.
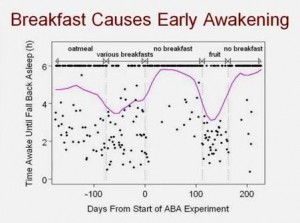
When a student suggested he eat more fruit, he started eating fruit for breakfast. His sleep got worse! This was exciting to Seth because it was, in 10 years, the first thing he tried that changed his sleep.
He had the idea of trying no breakfast. It turned out that skipping breakfast improved his sleep. One of his slides:
This directly supports our idea that intermittent fasting (confining eating to an 8-hour window each day) should be therapeutic for circadian rhythm disorders such as disturbed sleep and hypothyroidism.
But what’s exciting is that Seth continued his experiments to find other ways to improve his sleep. As a psychologist, he knew that human contact controls when we sleep: people are most awake at the times they have contact with other people, and asleep when isolated.
He knew that watching TV can have effects similar to socializing. So he tried watching Jay Leno one morning. He slept very well the next night.
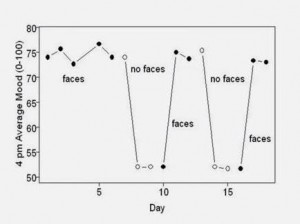
It turns out that looking at human faces is almost as good as real socializing. Here is Seth’s data relating mood to whether he looked at faces:
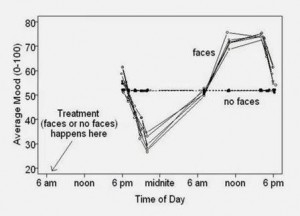
Seth also tracked his mood over the course of the day. The response of mood to seeing pictures of human faces clearly followed a circadian (24-hour) rhythm:
Another thing that relates to circadian rhythms is exercise: we normally exercise during the day and rest at night.
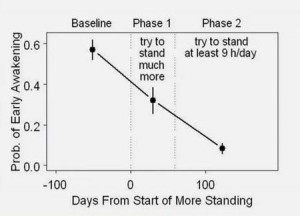
For a scholar, the easiest way to exercise is to stand rather than sit (for instance, by working at a standing desk). Seth tried standing 9 hours a day – and it cleared his sleep problem!
Of course, standing is not a very strenuous exercise. Seth found that if he just stood on one leg, the effect was much more intense, and he could fix his sleep problem with only minutes of one-legged standing per day.
He also found that eating more animal food improved his sleep. It’s possible that animal fat may enhance circadian rhythms more than other foods.
Conclusion
I found this fascinating – because it adds more evidence regarding the centrality of circadian rhythms in health – and exciting, because it shows that simple tactics can be therapeutic for circadian rhythm disorders.
In the hypothyroidism post, I suggested the following tactics for improving circadian rhythms:
- Light entrainment: Get daytime sun exposure, and sleep in a totally darkened room.
- Daytime feeding: Eat during daylight hours, so that food rhythms and light rhythms are in synch.
- Intermittent fasting: Concentrate food intake during an 8-hour window during daylight hours, preferably the afternoon. A 16-hour fast leading to lower blood sugar and insulin levels, and the more intense hormonal response to food that results from concentration of daily calories into a short 8-hour time window, will accentuate the diurnal rhythm.
- Adequate carb intake: Eat at least 400 “safe starch” carbohydrate calories daily during the afternoon feeding window. Relative to a very low-carb diet, this will increase daytime insulin release and, by increasing insulin sensitivity, may reduce fasting insulin levels. It will thus enhance diurnal insulin rhythm.
To these, we can add several more based on Seth’s findings:
- Looking at human faces: If you work at a computer, keep a window up that cycles among photos of faces, or shows a video of a talk show; keep photos of your family near your screen.
- Standing: Work at a standing desk or, failing that, get in the habit of standing on one leg rather than two.
- Animal fat: Eat a diet high in animal fats.
These tactics cured Seth’s sleep disorder. Might these tactics also cure or greatly improve other circadian rhythm disorders – including hypothyroidism and psychiatric disorders like depression and bipolar disorder? Could looking at human faces help the obese lose weight and improve their lipid profiles?
I don’t know but I’d certainly give these techniques a try before pharmaceutical drugs. I believe these techniques deserve clinical testing as therapies for all diseases associated with disrupted circadian rhythms. I believe that they may be just as beneficial for the healthy: by improving immune function, they may delay aging and extend lifespan.
A few weeks ago, when I posted a video of Don Rumsfeld defending the use of a standing desk (the same video was later linked by John Durant and Mark Sisson), I brashly stated, “There are few single life adjustments more likely to improve your health than working at a standing desk.”
Perhaps that statement wasn’t as exaggerated as it may have seemed!
Seth’s Talk











Recent Comments