Jan Kwasniewski developed his Optimal Diet something like 40 years ago and it has become extremely popular in Poland.
Kwasniewski recommended that adults should eat in the ratio
(Source).
In terms of calories this is roughly 240 calories protein / 1640 calories fat / 120 calories carbohydrate on a 2000 calorie diet.
The Perfect Health Diet proportions are more like 300 calories protein / 1300 calories fat / 400 calories carbohydrate. So the diets would be similar if about 300 calories, or 15% of energy, were moved from fat to carbohydrate in the form of glucose/starch (not fructose/sugar!).
Note that we recommend obtaining at least 600 calories per day from protein and carbs combined. This ensures adequate protein for manufacture of glucose and ketones in the liver. But the Optimal Diet prescribes only 360 calories total (less in women), suggesting that gluconeogenesis cannot, over any long-term period, fully make up for the dietary glucose deficiency.
In the book, we note that a healthy body typically utilizes and needs about 600 glucose calories per day. On the Bellevue All-Meat Trial in 1928 Vilhjalmur Stefansson ate 550 protein calories per day, which is probably a good estimate for the minimum intake needed to prevent lean tissue loss on a zero-carb diet.
With only 360 carb plus protein calories per day, the Optimal Diet forces ketosis if lean tissue is to be preserved. Since at most 200 to 300 calories per day of the glucose requirement can be displaced by ketones, the Optimal Diet is living right on the margin of glucose deficiency.
Gastrointestinal Cancers in Optimal Dieters
I learned over on Peter’s blog that Optimal Dieters have been dying of gastrointestinal cancers at a disturbing rate. Recently Adam Jany, president of the OSBO (the Polish Optimal Dieters’ association), died of stomach cancer at 64 after 17 years on the Optimal Diet. Earlier Karol Braniek, another leader of the OSBO, died at 68 from duodenal cancer.
A Polish former Optimal Dieter who has now switched to something closer to the Perfect Health Diet noted that gastrointestinal cancers seem to be common among Optimal Dieters:
The impression we get is that there’s rather high occurrence of gut cancer, including stomach, duodenum, colon … [source]
I want to talk about why I think that is, since the danger that the Optimal Dieters are discovering was one of the key factors leading us to formulate and publish the Perfect Health Diet.
Zero-Carb Diets Can Induce Mucus Deficiency
I ate a high-vegetable but extremely low-carb diet from December 2005 to January 2008. At the time I thought I was getting about 300 carb calories a day, but I now consider this to have been a zero-carb diet, since I don’t believe carb calories are available from most vegetables. Vegetable carbs are mostly consumed by gut bacteria, whose assistance we need to break down vegetable matter, or by intestinal cells which consume glucose during digestion.
Throughout my 2 years on this zero-carb diet, I had dry eyes and dry mouth. My eyes were bloodshot and irritated, and I had to give up wearing contact lenses. Through repeated experiments, I established that two factors contributed to the dry eyes – vitamin C deficiency and glucose deficiency. After I solved the vitamin C issue, I did perhaps 50 experiments over the following few years, increasing carbs which made the dry eyes go away and reducing them which made them immediately come back. This established unequivocally that it was a glucose deficiency alone that caused the dry eyes.
Rebecca reports similar symptoms in herself and her low carb friends.
This is also a well-known symptom during starvation. As a review cited by LynMarie Daye (and referenced by CarbSane in the comments) notes,
Since hepatic glycogen stores are depleted within 24 h of fasting, blood glucose concentrations are maintained thereafter entirely through gluconeogenesis. Gluconeogenesis is mainly dependent on protein breakdown (a small amount comes from the glycerol released during lipolysis) and it thus results in protein wasting. It is the effects of protein malnutrition that lead to the eventual lack of ability to cough properly and keep the airways clear, in turn leading to pneumonia and death during prolonged starvation; hypoglycaemia does not occur. [1]
Another common symptom of very low carb diets is constipation. This is often attributed to lack of fiber, but I am skeptical. I will get to the various possible causes of constipation in a future post, but for now I’ll just point out that a deficiency of gastrointestinal mucus would create a dry colon and cause constipation.
What connects a zero-carb diet to dry eyes, dry mouth, dry airways, and dry gastrointestinal tract?
Tears, saliva, and mucus of the sinuses, airways, and gastrointestinal tract are all comprised substantially of glycoproteins called mucins. Mucins are primarily composed of sugar; they typically have a number of large sugar chains bound to a protein backbone.
For instance, the main mucin of the gastrointestinal tract, MUC2, is composed of a dimerized protein – each protein weighing 600,000 Daltons individually, so 1.2 million Daltons for the pair – plus about 4 million Daltons of sugar, for a total mass of 5 million Daltons. In the mucus, these large molecules become cross-linked to form “enormous net-like covalent polymers.” (source)
If, for whatever reason, mucin production were halted for lack of glucose, we would have no tears, no saliva and no gastrointestinal or airway mucus.
Mucin Deficiency Causes Cancer
There is a strong association between mucus deficiency and gastrointestinal cancers.
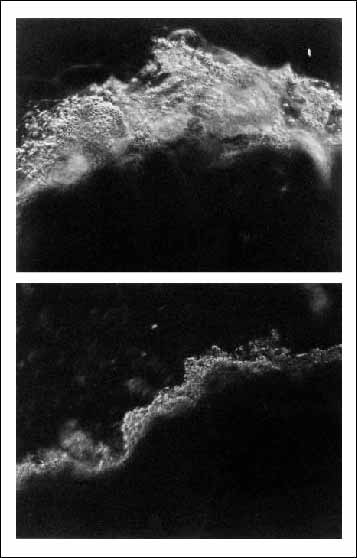
H. pylori is the strongest known risk factor for stomach cancer. [2] H. pylori infection is found in about 80% of gastric cancers. [3] One reason H. pylori promotes stomach cancer so strongly may be that it diminishes mucus in the stomach, as this photo shows:
Top: Normal stomach mucosa. Bottom: Stomach mucosa in an H. pylori infected person.
Scientists have created mice who lack genes for the main digestive tract mucins. These give us direct evidence for the effects on cancer of mucin deficiency.
Experiments in Muc1 knockout mice and mice with Muc1 knockdown have shown that under Helicobacter infection, mice deficient in Muc1 develop far more cancer-promoting inflammation than normal mice. [4]
The main mucin of the intestine is Muc2. The group of Leonard Augenlicht of the Albert Einstein Cancer Center in New York has studied mice lacking Muc2. They develop colorectal cancer. [5]
Tracing backward one step toward the source of mucin deficiency, the sugars in mucin are built from smaller pieces called O-glycans. It has been shown that mice that are deficient in O-glycans are prone to colorectal cancer: “C3GnT-deficient mice displayed a discrete, colon-specific reduction in Muc2 protein and increased permeability of the intestinal barrier. Moreover, these mice were highly susceptible to experimental triggers of colitis and colorectal adenocarcinoma.” [6]
Nutrient Deficiencies Can Also Play a Role
Some micronutrients are required for mucin production – notably vitamin D. [7, 8] Poland is fairly far north, and many of the Optimal Dieters could have been low in vitamin D.
Other important micronutrients for cancer prevention are iodine and selenium. Poland in particular had the lowest iodine intake and among the highest stomach cancer death rates in Europe. After Poland in 1996 began a program of mandatory iodine prophylaxis, stomach cancer rates fell:
In Krakow the standardized incidence ratio of stomach cancer for men decreased from 19.1 per 100,000 to 15.7 per 100,000, and for women from 8.3 per 100,000 to 5.9 per 100,000 in the years 1992-2004. A significant decline of average rate of decrease was observed in men and women (2.3% and 4.0% per year respectively). [9]
So among the Polish Optimal Dieters, the elevated gastrointestinal cancer risk caused by mucin deficiency may have been aggravated by iodine and sunlight deficiencies.
Conclusion
A healthy diet should be robust to faults. The Optimal Diet is not robust to glucose deficiency.
There’s good reason to suspect that at least some of the Optimal Dieters developed mucin deficiencies as a result of the body’s effort to conserve glucose and protein. This would have substantially elevated risk of gastrointestinal cancers. Thus, it’s not a great surprise that many Optimal Dieters have been coming down with GI cancers after 15-20 years on the diet.
We recommend a carb plus protein intake of at least 600 calories per day to avoid possible glucose deficiency. It’s plausible that a zero-carb diet that included at least 600 calories per day protein for gluconeogenesis would not elevate gastrointestinal cancer risks as much as the Optimal Diet. But why be the guinea pig who tests this idea? Your body needs some glucose, and it’s surely less stressful on the body to supply some glucose, rather than forcing the body to manufacture glucose from protein.
Fasting and low-carb ketogenic diets are therapeutic for various conditions. But anyone on a fast or ketogenic diet should carefully monitor eyes and mouth for signs of decreased saliva or tear production. If there is a sign of dry eyes or dry mouth, the fast should be interrupted to eat some glucose/starch. Rice is a good source. The concern is not only cancer in 15 years; a healthy mucosal barrier is also essential to protect the gut and airways against pathogens.
Related Posts
Other posts in this series:
- Dangers of Zero-Carb Diets, I: Can There Be a Carbohydrate Deficiency? Nov 10, 2010.
- Danger of Zero-Carb Diets III: Scurvy Nov 20, 2010.
- Dangers of Zero-Carb Diets, IV: Kidney Stones Nov 23, 2010.
References
[1] Sonksen P, Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth. 2000 Jul;85(1):69-79. http://pmid.us/10927996.
[2] Peek RM Jr, Crabtree JE. Helicobacter infection and gastric neoplasia. J Pathol. 2006 Jan;208(2):233-48. http://pmid.us/16362989.
[3] Bornschein J et al. H. pylori Infection Is a Key Risk Factor for Proximal Gastric Cancer. Dig Dis Sci. 2010 Jul 29. [Epub ahead of print] http://pmid.us/20668939.
[4] Guang W et al. Muc1 cell surface mucin attenuates epithelial inflammation in response to a common mucosal pathogen. J Biol Chem. 2010 Jul 2;285(27):20547-57. http://pmid.us/20430889.
[5] Velcich A et al. Colorectal cancer in mice genetically deficient in the mucin Muc2. Science. 2002 Mar 1;295(5560):1726-9. http://pmid.us/11872843.
[6] An G et al. Increased susceptibility to colitis and colorectal tumors in mice lacking core 3-derived O-glycans. J Exp Med. 2007 Jun 11;204(6):1417-29. http://pmid.us/17517967.
[7] Paz HB et al. The role of calcium in mucin packaging within goblet cells. Exp Eye Res. 2003 Jul;77(1):69-75. http://pmid.us/12823989.
[8] Schmidt DR, Mangelsdorf DJ. Nuclear receptors of the enteric tract: guarding the frontier. Nutr Rev. 2008 Oct;66(10 Suppl 2):S88-97. http://pmid.us/18844851.
[9] Go?kowski F et al. Iodine prophylaxis–the protective factor against stomach cancer in iodine deficient areas. Eur J Nutr. 2007 Aug;46(5):251-6. http://pmid.us/17497074.











Recent Comments