A lot of people have asked about the Atlantic article by Paul Offit, “The Vitamin Myth: Why We Think We Need Supplements.” Offit, a pediatrician, is best known for his defense of childhood immunizations. In arguing against benefits from vitamins, as he did in arguing against harm from vaccines, he takes a strong stand.
Before I take a look at his article, let me mention a competing publication about supplements that became available today, and might be more worthy of your time.
Examine.com’s Supplement Goals Reference Guide
A friend of the blog, Sol Orwell, has been an expert on nutritional supplements for many years and has consulted extensively for vitamin and supplement manufacturers. He and his colleagues have spent years compiling the most extensive database of peer-reviewed literature available, and have compiled the data into a 762 page reference guide that has a comprehensive overview of the supplement literature. It is an encyclopedic resource with background information about almost every supplement that has been studied, including herbal remedies, each graded for quality of evidence, and easily searchable by:
- supplement, to view the evidence for effects, good and bad, of each supplement; and
- health goal or biomarker, to see which supplements may help you achieve your health goal (such as, “blood glucose,” “breast tenderness,” “glycemic control,” “canker sores,” “fecal moisture,” “fat oxidation,” “free testosterone,” “food intake,” “memory,” “migraine,” “pain,” “postpartum depression,” and even, I kid you not, “penile girth”).
If this sounds interesting, read more about it here.
The Atlantic Article
OK, so what evidence does Offit compile against supplements?
Central to his case is a paper that we’ve already discussed on this blog (“Around the Web; The Case of the Killer Vitamins,” October 15, 2011): the 2011 analysis of the Iowa Women’s Health Study by Jaakko Mursu and collaborators in Archives of Internal Medicine. [1] Offit highlights it in the very first sentence of his article:
On October 10, 2011, researchers from the University of Minnesota found that women who took supplemental multivitamins died at rates higher than those who didn’t.
Apart from this reference he discusses two issues:
- Linus Pauling’s argument that vitamin C can prevent colds and cancer has not been supported. A history of Pauling’s romance with vitamin C occupies about two-thirds of the article, and Offit seems to think the whole idea of supplementation was originated by Pauling and persists due to his influence (“What few people realize, however, is that their fascination with vitamins can be traced back to one man,” Pauling.).
- Multiple studies have shown that supplementing vitamins A and E is often harmful.
This is hardly a comprehensive case against supplementation; it only shows that a few supplements tend to be harmful or lack benefits.
Regarding vitamins A and E, we agree; they are noted in our book as nutrients that should generally not be supplemented, or should be supplemented in low doses from natural sources. For example, we recommend eating a quarter pound of liver per week for vitamin A and other nutrients.
Regarding vitamin C, that it may not prevent colds or cancer does not mean it has no benefits. A few:
- NZ Man Left for Dead by Doctors, Cured by Vitamin C, Aug 26, 2010.
- Nutrients Are Needed to Heal Wounds and Injuries, Oct 7, 2010
- Fighting Viral Infections by Vitamin C at Bowel Tolerance, Sep 26, 2010
Our book has more evidence for benefits of vitamin C supplementation. Many people notice improved skin, hair, nails, gums, and teeth when supplementing with vitamin C, and faster wound healing. Vitamin C needs rise dramatically in sickness and stress.
It would be easy enough to compile further evidence of benefits of supplementation. Indeed, it was not so long ago that pellagra was rampant in the US South, and beriberi in East Asia. Many foods are subject to mandatory micronutrient fortification – a form of supplementation – to prevent iodine, folate, niacin, and thiamin deficiencies. So at least one branch of the government is convinced some supplementation is desirable.
So Offit’s case basically comes back to the Mursu et al paper. [1] Let’s revisit that one.
The Iowa Women’s Health Study
The study followed a large number of women in Iowa, and queried them several times about supplement use. In 1986, the baseline, the women had an average age of 62 (range of 55 to 69) and 66% were taking supplements. By 2004, the surviving women had an average age of 82 and 85% were taking supplements.
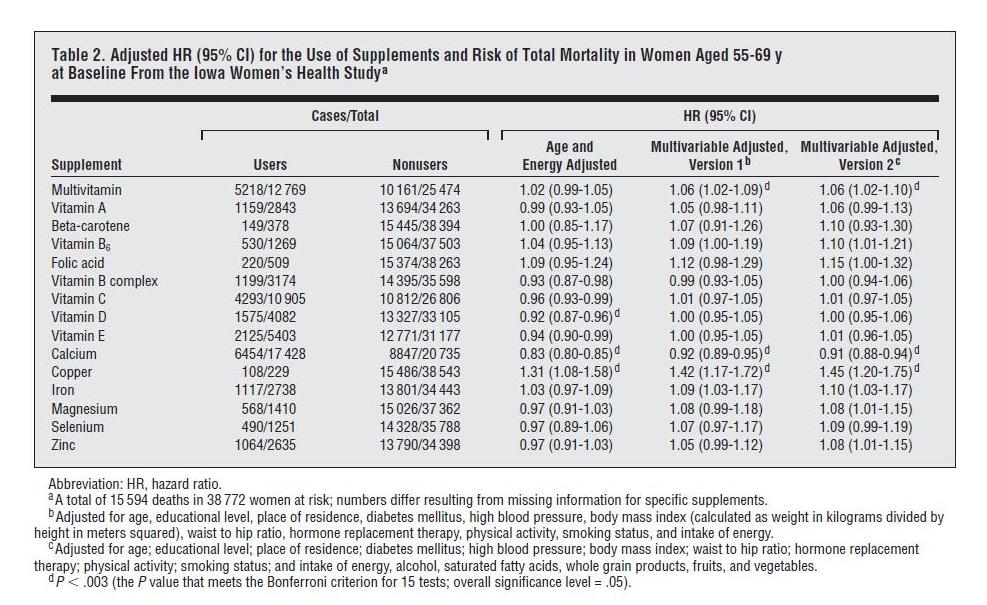
Here is the data on overall mortality vs supplement use:
“Cases” are instances of someone dying. “HR” or hazard ratio is the likelihood of dying if you supplement divided by the likelihood of dying if you don’t. Note that all the hazard ratio estimates are “adjusted.”
We can calculate the raw data from the Users and Nonusers columns. In general, supplements had no obvious effect – certainly no statistically significant effect. The fraction of Users and Nonusers who died was essentially identical. If we eliminate copper which only had 229 supplementers, the hazard ratio of supplementers averaged 99.8% that of non-supplementers – i.e., supplementers were very slightly less likely to die.
But – and this is a key point – supplement use increased with age throughout the study. Roughly, 66% of 62 year olds took supplements and 82% of 82 year olds took supplements. But mortality at age 82 is about five times higher than mortality at age 62. So the high-mortality 82 year olds were supplementing more than the low-mortality 62 year olds, but supplementers had the same mortality as non-supplementers! This indicates that with age adjustment, supplementation would have shown a clear benefit.
Did Mursu et al offer an age-adjusted analysis? No, they did not. The next column in the table is age-and-energy-adjusted. “Energy” means calories of daily food intake. But the purpose of eating is to supply our body with nutrients, and supplementing nutrients reduces appetite and energy intake. (This is discussed in Chapter 17 of our book.) Lower energy intake is associated with better health, largely because a high proportion of the elderly are diabetic: 27% of those over age 65 or older are diabetic, and 50% are diabetic or prediabetic; diabetics and prediabetics benefit from lower energy intake. By adjusting for energy, they are removing credit from the supplements for the health improvements due to reduced energy intake.
Nevertheless, after age-and-energy adjustment, we find that supplements generally decreased mortality. Nine of the fifteen supplements decreased mortality, five increased mortality. At the 95% confidence interval, five supplements decreased mortality, only one increased mortality.
Making the Elephant Wiggle His Trunk
The mathematician John von Neumann gave us the insight we need to understand this paper’s analysis:
With four parameters I can fit an elephant, and with five I can make him wiggle his trunk.
Mursu et al used multivariable adjustments with 11 parameters and 16 parameters respectively to obtain their “results.” Using so many parameters lets the investigators generate whatever results they want.
I don’t think it’s a coincidence that both multivariable adjustments substantially increased the hazard ratio of every single one of the 15 supplements. The 11-variable adjustment increased hazard ratios by an average of 7%, the 16-variable adjustment by an average of 8.2%.
Rest assured, it would have been easy enough to find multivariable adjustments that would have decreased hazard ratios for every single one of the 15 supplements by 7 or 8 percent.
I may as well quote my earlier analysis:
I believe it verged on the unethical that the variables chosen include dangerous health conditions: diabetes, high blood pressure, and obesity. These three health conditions just happen to be conditions that are improved by supplementation.
Anyone familiar with how regression analyses work will immediately recognize the problem. The adjustment variables serve as competing explanations for changes in mortality. If supplementation decreases diabetes, high blood pressure, and obesity, and through these changes decreases mortality, the supplements will not get credit for the mortality reduction; rather the decreased diabetes, blood pressure, and obesity will get the credit.
It’s appropriate to ask: if it’s proper to include health conditions like diabetes as variables in the regression, why not include other health conditions like cancer? The likely answer: Supplementation does not generally help conditions such as cancer, so including such conditions as adjustment factors would not have made the supplements seem more harmful. Rather, by giving greater weight to diabetes and obesity – conditions supplementation benefits – it would have made supplements look more beneficial.
It is impossible to take seriously studies that provide 11- and 16-variable adjustments, with arbitrarily chosen adjustment factors and no sensitivity analysis showing how alternative choices of adjustment factors would have altered the results.
Conclusion
The great economist Ronald Coase (in his essay “How should economists choose?”) said, “If you torture the data enough, nature will always confess.”
The Mursu paper was an exercise in torturing data until it declared, “Supplements are harmful!”
The Offit piece is a polemical exercise pretending that an unsettled part of biology – our nutrient needs, and the circumstances in which food fails to meet them – is a settled subject with a simple answer.
Now, it’s quite difficult to establish the healthfulness of supplementation in general, because you can always get too much of a nutrient, nutrient needs differ among persons depending on their health and age, and whether a person will benefit from a nutrient depends on whether the rest of the diet is deficient in that nutrient. So any given supplement is going to be harmful in some circumstances, beneficial in others.
A proper scientific approach would be to try to determine the circumstances under which supplements (or dietary changes eliminating the deficiency) would be beneficial.
Offit’s piece doesn’t attempt that. Our book does, and would make a much better resource to those considering supplementation. So would the Examine supplement goals reference guide.
References
[1] Mursu J et al. Dietary supplements and mortality rate in older women: the Iowa Women’s Health Study. Arch Intern Med. 2011 Oct 10;171(18):1625-33. http://pmid.us/21987192.












Recent Comments