A note from Paul: I’m happy to introduce Kamal Patel’s first post on PHD! Kamal is the funniest and maybe smartest guy in the ancestral health movement. A Ph.D. candidate in nutrition and a leader in the Ancestral Health Society, you may know him from PaleoHacks or Paindatabase.com. For more, check out Kamal’s bio on our About Us page. Welcome Kamal!
Goal: Do some computer work outside a couple times a week. Get maximal benefits from the sun in a minimum amount of time, while fitting all the necessary gear inside a backpack.
Resources: Tiny budget, free Amazon Prime shipping, access to a sunny park.
Why do computer work outside?
Hi, Kamal here (see below Shou-Ching for a short bio). I love sunlight. You probably love sunlight too. Turns out the sun is important for things outside of just vitamin D production. Ever wonder why indoor cats gravitate towards sunlight, even though they get their vitamin D from food? Probably not, since it just makes intuitive sense that animals want to be outdoors. The desire to be free of inside confines applies not just to indoor cats but also to indoor humans. Yet indoor humans sometimes need to see peer-reviewed articles before changing their habits. Don’t fret, we’ll start with a couple of those before delving into five specific steps for creating an outdoor workstation.
Sun exposure increases production of endorphins and nitric oxide, which can translate into benefits for both pyschological well being as well as disease prevention. Light boxes benefit not only seasonal affective disorder but also non-seasonally linked depression. Brief but regular exposure to ultraviolet light from tanning beds can help the mysterious and painful chronic condition called fibromyalgia, and sunlight may benefit pain after surgery. The draw of UV radiation is so powerful that frequent tanners can literally get addicted to catching rays. Unfortunately, the “pro-sunshine” lobby isn’t pouring billions into research on sun exposure, so the specific mechanisms of sunlight benefit will likely remain more mysterious than the mechanisms of blockbuster medications like Viagra and Prilosec.
Step 1: Dress for success
Look at your skin. Does it look more like Paul’s, or does it look more like Kamal’s?
If it looks like Kamal’s, you might be getting vitamin D not-at-alls (PS: that’s a rhyming mnemonic). Let me explain. I first got my vitamin D tested in 2008, and it came in at a whopping 19 ng/ml…even with taking a multivitamin most days and getting sunlight at lunchtime! As you probably know, pigmented and/or tanned skin serves as sunscreen, making it tough for darker people to synthesize vitamin D without very long sun exposure times. Indians may also produce less active vitamin D (calcitriol) from a given amount of sun exposure due to genetic predisposition.
But my problems apply to you lighter-skinned folk as well — my outdoor lunch excursions were done while wearing business casual clothing with short sleeves. This means covered torso and legs, leaving only about 25% of my skin exposed for vitamin D production. If you factor in things that can lower vitamin D production further, such as cloud cover, not laying down horizontally, higher BMI, and increased age, then it might be worth it to create a “sunlight maximization” strategy.
How serious are you about getting that extra sunlight? If you’re moderately serious, consider small changes like taking off your shoes and rolling up your pantlegs a bit while sitting in the park. If you’re extremely serious and okay with looking strange, consider occasional use of…mesh basketball jerseys! Yup, those cheapo mesh tops are made of thin material covered with tiny holes. One day I’ll buy a UV meter and check the actual numbers, but my suspicion is that wearing such a jersey would greatly increase skin exposure to the sun, perhaps doubling it or more. I bought my jersey for about $10 on Amazon, and sometimes change into it before leaving for the park. If you don’t already have blue-light blocking glasses to ratchet down light exposure before bedtime, you can buy a pair of those plus a jersey on Amazon in order to level up to free shipping.
Step 2: Acquire tiny chair and tiny laptop
Now that you’ve freed up enough skin to get some substantial sunlight, the next step is to assemble your outdoor office. This part is fun. Eventually you’ll want a small chair, especially if you’re planning on spending many hours working outside. To get a chair that you can stuff in your backpack, just head to REI or any place that sells camping gear. I chose a collapsible model at REI called “Flex Lite” that weighs only 1.75 pounds and folds down to 14×4 inches.
Laptops are expensive, so you can totally just use whichever model you have. BUT…if you have a few bucks to spare or your current model is in need of replacement, I’d recommend getting an ultra-light laptop, at under 3 pounds. That way, you can fit the tiny laptop and tiny chair along with a hearty lunch in your backpack. Just remember that a laptop with a matte screen works much better than a glossy screen for outdoor use.
Step 3: Optimize ergonomics
The name of the game when working at a computer is to avoid repetitive stress injuries. Simply by being outside, it will give you more incentive to get up and walk around once in a while. But there are other ways to introduce some structured change-of-posture. You can set a timer for every 20 or 30 minutes or get an app on your phone that reminds you to get up. You could also take a break from sitting in the chair to sit on the grass. Note that sitting with feet in contact with the earth (aka “earthing” or “grounding”) is speculated to have some health benefits, which is another bonus for getting in some outdoor office time.
For those with wrist problems, consider switching up your input method every now and then. Switching from right to left hand on occasion is the easiest way to do this. Other ways are switching from trackpad to mouse or trackball and using keyboard shortcuts more. Later this summer, a motion-detecting input device called “Leap Motion” is coming out that will allow you move the cursor with your MIND! Just kidding, not with your mind. But it does allow you to move the cursor with your hands in the air, Minority Report style, reducing much pressure from overstressed wrist tendons and ligaments. Fancy gadgets aside, if you’re going to spend more time outside, it’s a perfect opportunity to think more about varying your working position and revisiting ergonomics.
Step 4: Get pumped
This is going to sound cheesy, but so be it. Working outside can make you feel more alive. The transition from typical cubicle to standing desk is exciting. Work typically takes up the majority of one’s adult life, and standing cracks the mold of being a robotic office cubicle worker. Incorporating some outside work time removes so much of the drudgery aspect from work that it can confuse the most pessimistic of brains.
Normalizing circadian rhythm is an essential part of the health equation, and a complementary factor is being outdoors in the sun. “Sick building syndrome” doesn’t get a ton of research attention, but it’s a very real thing. One reason outdoorsy vacations provide a sense of well-being could be a lack of droning artificial light, stale air with concentrated indoor pollutants, and disgruntled coworkers. Even an office full of windows isn’t perfect. Office windows filter out UVB rays (meaning no vitamin D production or improved mood through endorphin release) but allow some UVA through (meaning staying indoors behind a window doesn’t keep you risk-free from skin damage and cataracts).
Step 5: Get outside already!
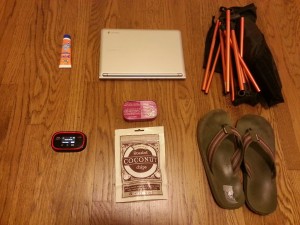
Above are my typical outdoor office supplies, all of which easily fit into a normal-sized backpack with room to spare. From the top left, there’s a travel-sized sunblock, laptop, collapsible chair, flipflops, coconut chips plus sardines in olive oil, and mobile wifi device. If you don’t want to get a mobile wifi device, you can usually get free or cheap mobile wifi from your smartphone.
In terms of practical recommendations, I advise people with school or office work to gradually spend more time working outside. If you find yourself able to be productive working outside, only then consider buying a chair or other outdoor accouterments. Wearing a mesh jersey might seem drastic, but it has a couple benefits. For darker-skinned individuals, it can substantially decrease the prolonged time needed to produce vitamin D. Very light-skinned individuals who are at higher risk of skin cancer could wear sunblock on parts of the body that are more prone to skin damage (like the face) and couple that with producing vitamin D from a jersey-clad torso.
To reiterate because of its importance, a critical concept for office work is VARIATION. The capital letters are to show that I’m not joking around. Combining typical indoor seated work with at least occasional standing work and occasional outdoor seated work is a solid ergonomic base. Increasing the standing to a few hours a week may result in weight loss of several pounds a year. When indoors, a “microbreak” of under a minute could be spent grabbing some water, taking a lap around the office, or climbing a set of stairs. These microbreaks have been shown to reduce muscular discomfort without compromising productivity. When outdoors, microbreaks are pretty much just awesome. Breathe in some fresh air, stare at the clouds, say hello to the doggies at the park. All the studies in the world can’t relay just how nice it is to work outside a couple times a week.














Recent Comments