Items that caught my eye this week:
(1) Would You Be My Meatheart?: I wasn’t clever enough to give this to Shou-Ching for Valentine’s Day, but would have known to use genuine hearts from the Asian market. Wait till next year honey!
(2) By the way: Who knew Manolo has a food blog?
(3) Ronaldo Forced Out of Soccer for Lack of Thyroid Hormone. Famed soccer star Ronaldo is retiring because he has hypothyroidism and he says soccer authorities consider treatment to be doping – so he has to retire to fix his health.
Absurd! Mary Shomon agrees.
(4) Ronaldo may play the “beautiful game,” but we Americans play the crazy game. This running back plays football like I used to:
(5) Startling if True: Paleo Pepper abridges a talk by Dr. Flechas at iodine4health.com claiming that thyroid hormone replacement may actually increase risk of breast cancer among hypothyroid women – what is needed is high-dose iodine:
A women with hypothyroidism has a 6% chance of developing breast cancer. Once she starts taking thyroid hormone, it doubles her chances. Once she’s been on thyroid hormone replacement for 15 years, it more than triples it – she now has a 19.6% chance of developing breast cancer.
I have not seen such statistics before and would have to check these claims. We recommend iodine and selenium as the first steps in dealing with hypothyroidism, but generally support thyroid hormone replacement.
(6) Burying the Lede: Is “strengthens pelvic floor muscles” really the number one benefit?
(7) Another Perfect Health breakfast idea: Emily suggests cream of rice with cream, butter, and apricot applesauce.
(8) Paleolithic Dairy?: Ravi at Daia Sol Gaia argues that dogs may have been domesticated and goats tamed and used for milk as early as 35,000 years ago – the start of the Upper Paleolithic. Is goat milk a Paleo food?
(9) The authentic way to drink Paleo goat milk: Paleolithic settlers at Gough Cave in England, c. 13,000 to 10,000 BC, ate human bone marrow and brain and used the skulls as drinking chalices:
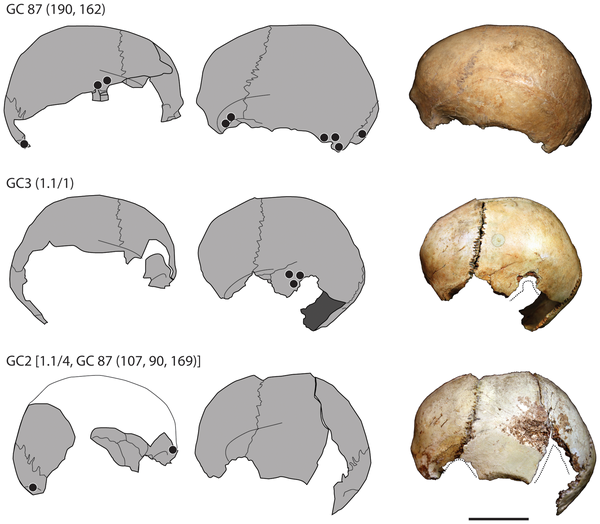
Via Dienekes. Apparently drinking from human skulls is a widely attested practice, both in Paleolithic and historical times – see e.g. the Krum and Herodotus’s Scythians.
Reference: Bello SM et al. Earliest Directly-Dated Human Skull-Cups. PLoS ONE 6(2): e17026. doi:10.1371/journal.pone.0017026. Link.
(10) Avoid vegetable oils if you want a baby: Chris Highcock found a paper showing that infertile women eat 23% more polyunsaturated fat, and 17% less saturated fat, than fertile women. Infertile men eat 20% more polyunsaturated fat than fertile men.
Reference: Revonta M et al. Health and life style among infertile men and women. Sex Reprod Healthc. 2010 Aug;1(3):91-8. http://pmid.us/21122604.
(11) Never give up:
“I had the head doctor of surgical I.C.U. say, ‘Miracles happen.’“
(Via Craig Newmark)
(12) Which Machine for the Hippo? I thought this was a cool picture:

(From NPR via John Durant)
(13) Finally, our video: We’ve had a bit of discussion of eating disorders this week, in the comments to the “Therapy AND Life” post. That reminded me of this CBS News interview of a “Biggest Loser” contestant who said she developed an eating disorder during the show:






















Recent Comments