We had a delightful tour today at Green Meadows Farm in Hamilton, Massachusetts; I’ll write more about it tomorrow. Thanks to Andrew and Diana Rodgers for showing us around.
Also on Sunday October 23, Paul will be on Cary Nosler’s Wide World of Health radio show at 4 pm Eastern / 1 pm Pacific. It’s possible to listen live on the Talk 650 KSTE web site.
[1] Perfect Ego-Gratifying Book Review: Over at Health Correlator, Ned Kock has reviewed our book. Ned is one of the smartest and most interesting bloggers in the Paleosphere, so we were delighted that he liked our book. In his first paragraph, he links “Perfect Health Diet” to “Facebook”, and later he speaks of Shou-Ching and me in the same breath with well-known scientists:
Their main PhD disciplines are somewhat similar to Einstein’s and Curie’s; which is an interesting coincidence. What the Jaminets have written about nutrition is probably analogous, in broad terms, to what Einstein and Curie would have written about nutrition if they were alive today.
If they were alive today, they’d be 132 and 144 years old respectively, and everyone would be intensely interested in their nutitional tips! So we take that as high praise indeed.
Ned’s wasn’t the only pleasing review we got this week; Dr. Srdjan Andrei Ostric wrote a generous endorsement of our book. I was also pleased that one of Dr Ostric’s readers did NOT directly compare me to her emotionally abusive ex.
[2] Interesting posts this week:
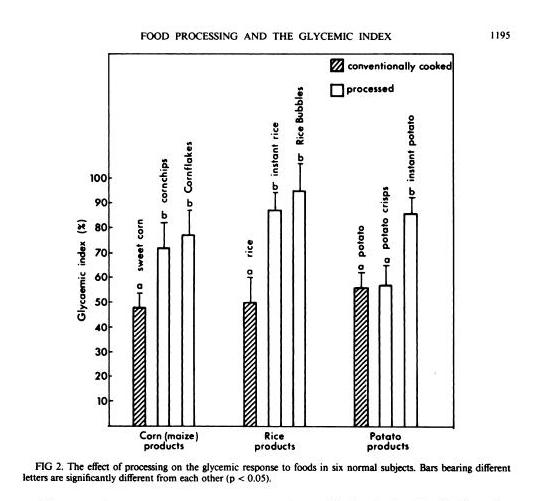
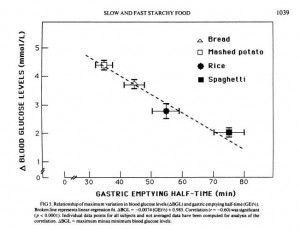
Andrew Badenoch of Evolvify downgrades potatoes and rice to “sneaky untrustworthy bastards” and bok choy to “I’m not making out with you if you eat that.” This was in response to that interesting miRNA study I mentioned in a previous Around the Web. Richard Nikoley offered his thoughts.
One of Richard’s commenters hopes we’ll critique the study. It’s not an easy study to critique because it’s the first of its kind; everything about it is interesting, but very likely not all the results will be reproducible. Also, it’s premature to draw any conclusions about how it affects diet, since all plant and animal cells contain microRNA, and there’s nothing special about the miRNAs of rice or potato. If rice miRNAs can survive cooking and digestion and cross cellular membranes and affect gene expression, so will miRNAs from every other plant and animal food. That would imply that we evolved with a background level of dietary miRNAs in our cells. The implications for diet are hard to fathom, except that it probably strengthens the case for eating in an ancestral manner, since an ancestral diet would deliver a mix of miRNAs we evolved to handle.
Emily Deans summarized yesterday’s talks at TEDx Cambridge. A line that caught my eye:
Lustig seems to feel that fructose, MCTs, and BCAAs are damaging to the mitochondria and lead to insulin resistance (thus he is anti-corn fed beef, as corn-fed beef is higher in BCAAs than grassfed, apparently.)
I’m pro BCAAs. Is that a reason to favor corn-fed beef?
Two PaleoHackers, Kamal and Aravind, tried to reduce food reward and lost weight. Stephan Guyenet recounts their story.
J Stanton has another blockbuster exposition on food reward, which contains a challenge to Stephan’s recommendations for weight loss: eating food you like decreases quantity of food consumed more than eating bland food.
Lucas Tafur reports that some mouth bacteria can digest gluten, making wheat safer for their hosts.
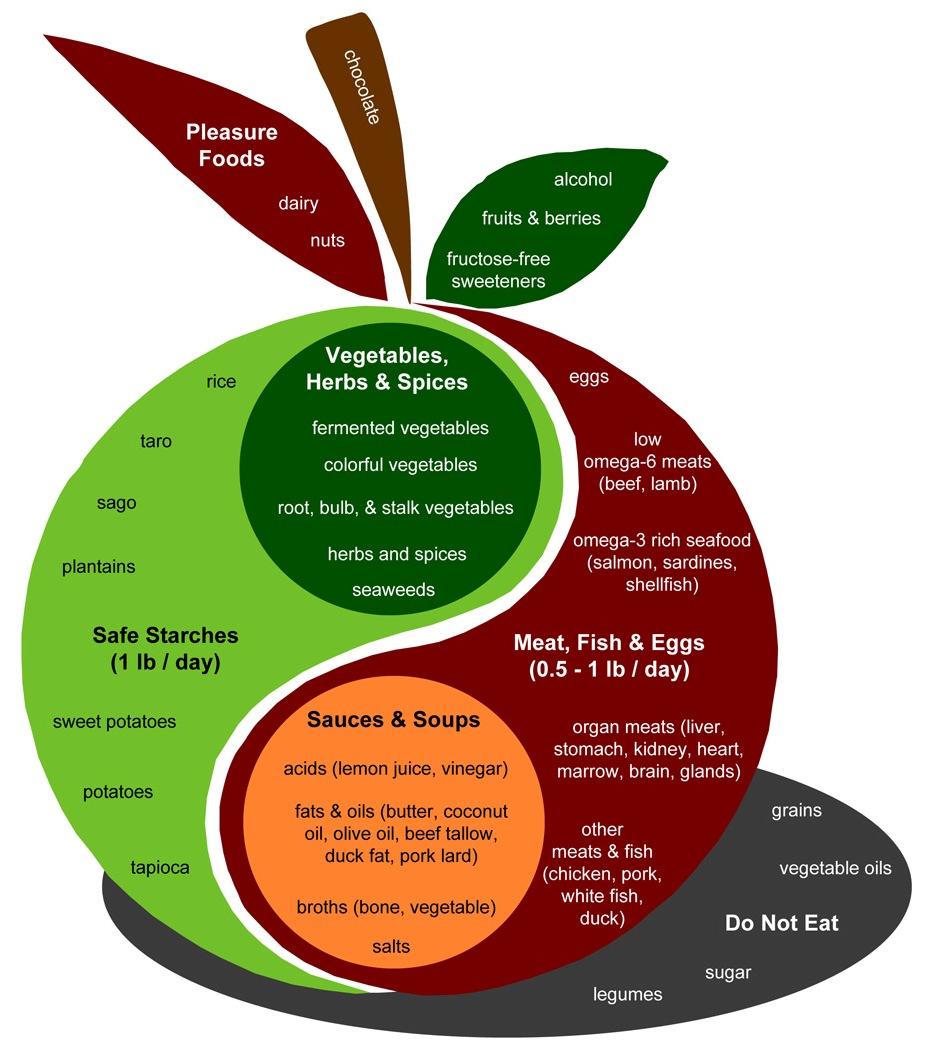
Mike Gruber’s triglycerides went down after he added starches and supplements in line with Perfect Health Diet recommendations. Was it the starch, or the micronutrients?
Melissa McEwen compares overeating to porn addiction and discusses Paleomedicine.
Oetzi the Iceman had Lyme disease. Folks with Lyme infections are more likely to be diagnosed with psychiatric disease. Oetzi was discovered in a reclining posture. Coincidence?
Dr Steve Parker links to Vitruvius at The Sagacious Iconoclast, who explains how Paleolithic man might have made cheese: “transport milk in mammal stomach vessels containing natural rennet, in the heat, thousands of years ago, and voila: curds and whey.”
In the New York Times, a woman has survived a dangerous cancer by retreating to national parks. She’s not the only one; the combination of sunshine, exercise, and nature seems to have a strong anti-cancer effect.
Darrin Carlson wrote on The Five Failings of Paleo. You might have seen the piece reprinted at Free the Animal.
John Durant is manly, in a Jack Sparrow Dances with Wolves kind of way.
Jamie Scott says: Make your own antioxidants.
Mark Sisson says: For healthy mitochondria, eat fat.
Dr BG fostered a kitty, and reflects on human evolution.
Nourished Kitchen has tips for a healthier Halloween.
Let’s see, there was the Permian-Triassic Extinction, the Cretaceous-Tertiary Extinction – the 1883 Extinction?
[3] Cute animal photo:
Via Yves Smith.
[4] A mini-debate on protein and longevity: In the comment thread to Ned Kock’s review of our book, Ned has an excellent counterargument about protein and longevity:
Here is another counterpoint to the notion that increased protein intake leads to decreased longevity. A BMI of 25 is generally associated with the lowest mortality: http://bit.ly/fWdsPC
Now, we know that as people age they generally tend to lose body mass (contrary to popular opinion), primarily due to loss of lean body mass, which seems to outpace body fat gain.
Increased protein consumption seems to counter that, and this appears to be related to both bone and muscle retention, contributing to a higher BMI.
So it is not unreasonable to conclude that the relatively high BMI of 25 is associated with retention of lean body mass with age, even as body fat gradually increases as well, leading to the perception that the fat are the ones living the longest.
Of course I am not talking about 600 g/d of protein. These seniors seem to have done quite well in terms of bone retention at around 85-90 g/d: http://bit.ly/f1Pi3T
In another comment Ned mentions receiving from O Primitivo a link to a paper that looks fascinating.
[5] The End of Human Progress: Via Joshua Newman, an aphorism from Ben Franklin:
I have always thought that one man of tolerable abilities may work great changes, and accomplish great affairs among mankind, if he first forms a good plan, and, cutting off all amusements or other employments that would divert his attention, make the execution of that same plan his sole study and business.
A corollary from Paul Jaminet:
Humanity will stagnate until the Internet becomes boring.
[6] Autism Updates:
Weston A Price might have something to say about possible nutritional factors behind this finding: Autistic children have an altered facial structure, characterized by wider eyes, a broader upper face, wider mouth and philtrum, but shorter middle region of the face including cheeks and nose.
There seems to be a connection between maternal gestational diabetes and autism. A Rice University professor discusses the link:
[7] Not the Weekly Video: Why Paleolithic man didn’t bicycle:
[8] Shou-Ching’s Photo Art:
[9] Weekly video: Never trust an animal that wears a tuxedo!
Via Bix.





















Recent Comments