So it looks like pork consumption is correlated with cirrhosis of the liver, liver cancer, and multiple sclerosis (Pork: Did Leviticus 11:7 Have It Right?, Feb 8, 2011). Why?
There are a number of potential dangers from pork, and to give each due consideration will require two posts. I’ll look at a few candidates today, and save my top candidate for Thursday.
Omega-6 Fats
Omega-6 fats are a health villain: Excess omega-6 contributes to general inflammation, fatty liver disease, metabolic syndrome, obesity, and impaired immune function.
And pork can be a major source of omega-6 fats. Nutritiondata.com lists the omega-6 fraction of lard at 11%. But the omega-6 fraction can be highly variable, depending on the pig’s diet. Chris Masterjohn recently reported that the lard used in the “high-fat” research diet was 32% polyunsaturated, nearly all of it omega-6:
The graph shows the difference between the actual fatty acid profile as determined by direct analysis of the lard and the previously reported fatty acid profile, which had been estimated using the USDA database. We can see that the actual fatty acid profile is much higher in PUFAs, at the expense of both saturated and monounsaturated fats. In fact, the company had originally estimated the diet to provide 17 percent of its fat as PUFA, but now estimates it to provide a whopping 32 percent!
Chris further reported that feeding the pigs a pasture and acorns diet would reduce lard PUFA levels to 8.7%, and feeding them a Pacific Islander PHD-for-pigs diet of coconut, fish, and sweet potatoes would reduce lard PUFA levels to 3%.
So the omega-6 content can cover a 10-fold range, 3% to 32%, with the highest omega-6 content in corn- and wheat-fed pigs who have been caged for fattening. Corn oil and wheat germ oil are 90% PUFA, and caging prevents exercise and thus inhibits the disposal of excess PUFA. Caging is a common practice in industrial food production; here is a picture of sows in gestation crates:
And here are some Chinese pigs in shipping cages for transport to market:
The Wall Street Journal reported Monday that McDonald’s, following Chipotle, has asked its pork suppliers to stop using gestation stalls, and the largest US hog producer, Smithfield Farms, has begun a 10-year plan to move pigs from small stalls into roomier “group housing systems.” So perhaps the omega-6 content of commercial pork will come down.
How much omega-6 are people actually getting from pork? In the Bridges database, the range in pork consumption across countries was 2 to 80 kg/yr, or 5 to 200 g/day. If this is from industrially raised pigs whose fat is 30% omega-6, then this works out to 0.25% to 10% of energy as omega-6 fats from pork. In most countries, pork is either the primary source of omega-6 fats or the second source after vegetable oils.
Moral of the story: If you’re going to eat a lot of pork, there are real benefits to finding a source of naturally raised pigs fed a healthy diet.
Aside: On a similar diet, human adipose tissue develops almost identical omega-6 levels to pig lard. The Finnish Mental Hospital Study [1] [2] [3], discussed in our book on pages 63-65, showed that on a normal dairy-rich hospital diet human adipose tissue is less than 10% omega-6, but on a soybean oil rich diet adipose tissue becomes 32% omega-6.
American diets have traversed this range in recent decades. Here is a plot of subcutaneous fat omega-6 levels from Stephan Guyenet:

But can omega-6 fats explain the remarkable correlation between pork consumption and liver cirrhosis mortality, hepatocellular carcinoma, and multiple sclerosis?
Polyunsaturated fats are usually a factor in liver diseases. As we discuss in the book (pp 57-58), polyunsaturated fats – either omega-6 or omega-3 – combined with alcohol or fructose are a recipe for fatty liver disease and metabolic syndrome, especially if micronutrient deficiencies figure in the mix. Two of the studies cited in the book:
- Mice fed 27.5% of calories as alcohol developed severe liver disease and metabolic syndrome when given a corn oil diet (rich in omega-6), but no disease at all when given a cocoa butter diet (low in omega-6). (The first line of this paper reads, “The protective effect of dietary saturated fatty acids against the development of alcoholic liver disease has long been known”.) [4]
- Scientists induced liver disease in mice by feeding alcohol plus corn oil. They then substituted a saturated-fat rich mix based on beef tallow and coconut oil for 20%, 45%, and 67% of the corn oil. The more saturated fat, the healthier the liver. [5]
George Henderson, who got us started on this series, links to more papers connecting omega-6 fats to liver cirrhosis.
So: Pork can be a major source of omega-6 fats; and omega-6 fats are a cause of liver cirrhosis.
However, there are several reasons for thinking that omega-6 fats cannot be the primary reason pork raises mortality from our three diseases.
First, vegetable oil consumption seems to be largely uncorrelated with the pork-associated diseases. If omega-6 fats were the primary cause then vegetable oils should have been as strongly correlated as pork. Yet there are plenty of cases of high vegetable oil and low pork consumption (eg Israel), or low vegetable oil and high pork consumption. Disease rates track pork consumption only.
Second, high intake of omega-6 fats causes a mild elevation of risk for a wide range of diseases, much like obesity (which high omega-6 intake causes). Yet pork is associated with extreme elevation of three diseases, and little association with other diseases – not at all the pattern we would expect for omega-6 fats.
Overall, I think we can say that omega-6 fats are probably a contributing factor in liver disease and liver cancer, possibly in multiple sclerosis, but they are unlikely to be the primary factor in the high correlation between pork consumption and liver cirrhosis mortality, liver cancer mortality, and multiple sclerosis.
Processed Meat Toxins
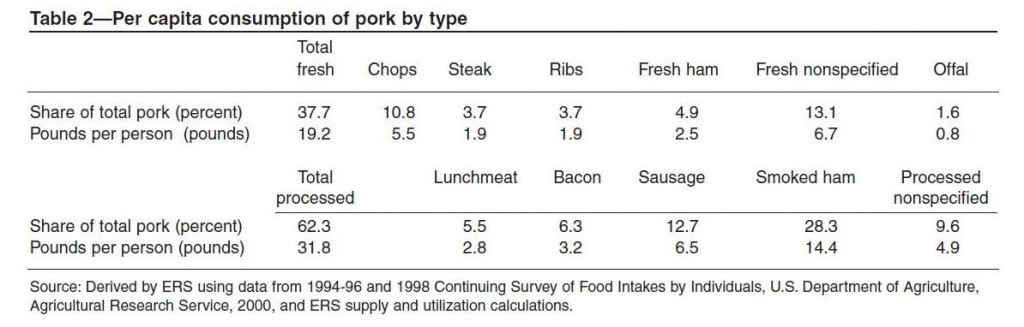
In many countries, most pork consumption is in the form of processed meats. In the United States, about two-thirds of pork is processed. Here is a table (hat tip: Mary Lewis):
Smoked ham is 28% of US pork consumption, sausage is 13%, bacon 6%, processed lunchmeat 6%, and other forms of processed pork another 10%. Among fresh pork cuts, pork chops lead with 11% of US consumption.
In epidemiological studies, processed meat consumption is often associated with poor health. The strongest association is for colorectal cancer [6] and other cancers of the digestive tract, liver, and prostate.
The main types of processing are curing and smoking. Smoking introduces to the meat smoke toxins such as phenols, aldehydes, and polycyclic aromatic hydrocarbons. Curing uses salt, sugar, and nitrite, and while these are fairly benign on their own, various toxins can be formed from them, notably glycation products from the sugar and “N-nitroso compounds” such as nitrosamines from the nitrite.
Some people have concerns about the salt in processed pork. MScott provided evidence that the salt could promote peroxidation of omega-6 fats. Vladimir Heiskanen sent me a link to a blog post arguing that upsetting the sodium-potassium balance could be important:
Dr. Kublina also stressed that people must understand the massive impact that processing has on foods. She cites, for example, that 100 g of unprocessed pork contains 61 mg of sodium and 340 mg of potassium, but turning this into ham alters that ratio significantly, to yield a whopping 921 mg of sodium and, to boot, reduces the potassium content to 240 mg.
On the other hand, john linked to a paper showing that bacon protected against colon cancer, probably due to its salt content. Personally, I think salt is quite healthy, even at the levels contained in bacon, as long as one drinks water and eats vegetables for potassium.
Of all the toxins in processed pork, the most plausible causal agent for our three diseases are the N-nitroso compounds. These compounds are highly abundant in processed pork:
N-nitroso content of food items ranged from <0.01?g/100 g. to 142 ?g/100 g and the richest sources were sausage, smoked meats, bacon, and luncheon meats. [7]
The most common N-nitroso compound in pork products is N-nitrosodimethylamine (NDMA), followed by N-nitrosopiperidine (NPIP), N-nitrosodiethylamine (NDEA), N-nitrosopyrrolidine (NPYR), N-nitrosomorpholine, and N-nitrosothiazolidine (NTHZ).
Nitrosamine levels are increased by high-temperature cooking: “Frying of bacon and cured, smoked pork bellies led to substantially increased levels of NPYR.” [8] In general, high-temperature cooking of meats is a bad idea, as it can generate mutagenic and carcinogenic compounds even in fresh meat. [9]
N-nitroso compounds are known causal agents for liver cancer. Scientists commonly use N-nitrosodiethylamine (NDEA) to induce hepatocellular carcinoma in rats (669 citations, eg [10]). In primates, N-nitroso compounds specifically cause cancers of the liver:
Conversely, all except two of the N-nitroso compounds were carcinogenic. Diethylnitrosamine (DENA) was the most potent and predictable hepatocarcinogen in cynomolgus, rhesus, and African green monkeys. [11]
A Finnish study found an increased risk of colorectal cancer with exposure to N-nitrosodimethylamine (NDMA) from smoked and salted meats, mainly fish and pork [12]. In China, intake of N-nitroso compounds correlates with the incidence of esophageal cancer. [13]
So it seems like we have a likely causal agent here linking pork to liver cancer.
But not so fast!
Although N-nitroso compounds undoubtedly can cause liver cancer, there is a big obstacle to attributing the correlation of human liver cancer with pork consumption to the N-nitroso compounds in processed pork. This is that human liver cancer rates seem to be more strongly related to consumption of fresh pork than processed pork.
I’ve seen several studies showing this, and none showing the reverse. Here’s an example: “A prospective study of red and processed meat intake in relation to cancer risk” [14]. Remember, red meat includes pork, and pork is the most dangerous red meat; processed meat is mainly processed pork.
Here is the hazard ratio of various cancers for the top quintile versus bottom quintile of red meat intake:
Liver cancer has the highest hazard ratio, 1.61.
Here are the hazard ratios for processed meat:
Liver cancer is eleventh most likely among the cancers, and the hazard is insignificant.
Here’s another study, an analysis of colorectal cancer rates in the European Prospective Investigation into Cancer (EPIC), which also supports the idea that (a) pork is worse than beef and (b) fresh pork is worse than processed pork:
In analyses of subgroups of red meats, colorectal cancer risk was statistically significantly associated with intake of pork (for highest versus lowest intake, HR = 1.18, 95% CI = 0.95 to 1.48, Ptrend = .02) and lamb (HR = 1.22, 95% CI = 0.96 to 1.55, Ptrend = .03) but not with beef/veal (HR = 1.03, 95% CI = 0.86 to 1.24, Ptrend = .76). In analyses in which intake of each meat was mutually adjusted for intake of the other meats, only the trend for increased colorectal cancer risk with increased pork intake remained statistically significant (Ptrend = .03). Intakes of ham (for highest versus lowest intake, HR = 1.12, 95% CI = 0.90 to 1.37, Ptrend = .44), of bacon (HR = 0.96, 95% CI = 0.79 to 1.17, Ptrend = .34), and of other processed meats (mainly sausages) (HR = 1.05, 95% CI = 0.84 to 1.32, Ptrend =.22) were not independently related to colorectal cancer risk. [15]
Beef is harmless, lamb is not statistically significant after adjustment for pork intake, but pork was harmful in all analyses. However, processed pork had lower hazard ratios than fresh pork, and bacon even appeared protective!
Before I conclude this post, let me present one more fact. This is that fiber consumption is protective against pork-induced cancer. Here is representative data, from [15]:
Look at panel B: With high fiber intake there is essentially no additional cancer risk; but if fiber intake is low, then pork consumption is much more effective at elevating cancer rates.
Conclusion
So let’s add up the evidence and see where it leads:
- First, the only potentially dangerous component of fresh natural pork, omega-6 fats, can’t account for the data.
- Second, processed pork, which has other dangerous compounds like N-nitroso compounds, actually appears safer than fresh pork.
- Third, fiber is protective against pork dangers.
To me these suggest that an infectious pathogen is the cause we are looking for.
Consider: Traditional methods of processing pork, such as salting, smoking, and curing, are antimicrobial. They were developed to help preserve pork from pathogens. So if processed pork is less risky than fresh pork, we should look for a pathogen that is reduced in number by processing.
If a pathogen is the cause, then it makes sense that fiber would be protective. Fiber increases gut bacterial populations. Gut bacteria get “first crack” at food and release proteases and other compounds that can kill pathogens. Also, a large gut bacterial population makes for a vigilant immune system at the gut barrier, making it more likely that pathogens will fail to enter the body. The gut flora are a valuable part of the gut’s immune defenses.
In my next post I’ll look at the pathogens that can infect both pigs and humans, and see (1) if there is a likely candidate for the association of pork consumption with liver cirrhosis, liver cancer, and multiple sclerosis, and (2) how we can best protect ourselves against this threat.
Related Posts
Posts in this series:
- Pork: Did Leviticus 11:7 Have It Right?, Feb 8, 2012
- The Trouble with Pork, Part 2, Feb 15, 2012
- The Trouble With Pork, Part 3: Pathogens, Feb 22, 2012.
References
[1] Miettinen M et al. Effect of cholesterol-lowering diet on mortality from coronary heart-disease and other causes. A twelve-year clinical trial in men and women. Lancet. 1972 Oct 21;2(7782):835-8. http://pmid.us/4116551.
[2] Turpeinen O et al. Dietary prevention of coronary heart disease: the Finnish Mental Hospital Study. Int J Epidemiol. 1979 Jun;8(2):99-118. http://pmid.us/393644.
[3] Miettinen M et al. Dietary prevention of coronary heart disease in women: the Finnish mental hospital study. Int J Epidemiol. 1983 Mar;12(1):17-25. http://pmid.us/6840954.
[4] You M et al. Role of adiponectin in the protective action of dietary saturated fat against alcoholic fatty liver in mice. Hepatology. 2005 Sep;42(3):568-77. http://pmid.us/16108051.
[5] Ronis MJ et al. Dietary saturated fat reduces alcoholic hepatotoxicity in rats by altering fatty acid metabolism and membrane composition. J Nutr. 2004 Apr;134(4):904-12. http://pmid.us/15051845.
[6] Santarelli RL et al. Processed meat and colorectal cancer: a review of epidemiologic and experimental evidence. Nutr Cancer. 2008;60(2):131-44. http://pmid.us/18444144.
[7] Stuff JE et al. Construction of an N-nitroso database for assessing dietary intake. J Food Compost Anal. 2009 Dec 1;22(Suppl 1):S42-S47. http://pmid.us/20161416.
[8] Ellen G et al. N-nitrosamines and residual nitrite in cured meats from the Dutch market. Z Lebensm Unters Forsch. 1986 Jan;182(1):14-8. http://pmid.us/3953157.
[9] Sinha R. An epidemiologic approach to studying heterocyclic amines. Mutat Res. 2002 Sep 30;506-507:197-204. http://pmid.us/12351159.
[10] Peto R et al. Effects on 4080 rats of chronic ingestion of N-nitrosodiethylamine or N-nitrosodimethylamine: a detailed dose-response study. Cancer Res. 1991 Dec 1;51(23 Pt 2):6415-51. http://pmid.us/1933906.
[11] Thorgeirsson UP et al. Tumor incidence in a chemical carcinogenesis study of nonhuman primates. Regul Toxicol Pharmacol. 1994 Apr;19(2):130-51. http://pmid.us/8041912.
[12] Knekt P et al. Risk of colorectal and other gastro-intestinal cancers after exposure to nitrate, nitrite and N-nitroso compounds: a follow-up study. Int J Cancer. 1999 Mar 15;80(6):852-6. http://pmid.us/10074917.
[13] Lin K et al. Dietary exposure and urinary excretion of total N-nitroso compounds, nitrosamino acids and volatile nitrosamine in inhabitants of high- and low-risk areas for esophageal cancer in southern China. Int J Cancer. 2002 Nov 20;102(3):207-11. http://pmid.us/12397637.
[14] Cross AJ et al. A prospective study of red and processed meat intake in relation to cancer risk. PLoS Med. 2007 Dec;4(12):e325. http://pmid.us/18076279.
[15] Norat T et al. Meat, fish, and colorectal cancer risk: the European Prospective Investigation into cancer and nutrition. J Natl Cancer Inst. 2005 Jun 15;97(12):906-16. http://pmid.us/15956652.
















I’m not sure I’ll be dropping my ham and bacon for a bagel any time soon, but if an option of seafood or beef or ham . . . you’ve got me hesitant about the pork now. But my eyes are full of squinty suspicion. Impressive series, I’m rather riveted and can’t wait for the conclusion!
Really fascinating stuff. Count me into the ‘riveted’ group – can’t wait for the next installment.
I felt physically ill seeing those hogs in cages. I have been trying to buy all our pork from local farms that raise hogs on pasture. I will be doing more than just “trying” from here on in, if we continue to eat it….
Even though I was pretty off the mark with that salt guess it’s awesome getting a mention in a PHD post. I should’ve guessed the infectious pathogens angle as I’m currently doing a research project on Clostridium botulinum and just read about how nitrite inhibits the formation of botulinum toxin.
Fascinating posts, looking forward to the next one.
Pathogens make the most sense in the light of the blood-coagulation study were fresh pork scored.
Also, in wide parts of Germany there’s a tradition to eat raw ground pork (“Mett”) on bread.
There are also some types of only slightly cured/processed sausages like “Rohesser” (lit.: raw-eater)or “Teewurst” which are smoked for a very short duration and have less salt content, they even taste almost raw.
It might be also that due to the preference for thick sliced Pork-Schnitzel (as opposed to the thin vienna-style Veal-Schnitzel), chops and thick burgers (which are usually half/half, pork/beef) sometimes (by mistake) the meat won’t be well done in the center, thus giving the pathogens higher chances to survive.
Wow!
Excellent post
Nice investigation Dr. House style 🙂
Thank you, Paul, for this post!
Wow. The idea of eating an infectious pathogen and seeing those photos – very disturbing and turns me off of pork and other meat too. With my hectic schedule, difficult access to quality grocery stores, having to eat out alot and only having a small freezer, it’s nearly impossible for me to get decent PHD-acceptable meat. Sardines, salmon and eggs seem to be much less risky and much easier to swallow! 🙂
Nice post. So the moral of the story is to cook pork well enough to kill the pathogens.
Bacon here in the UK has ascorbic acid added to it, which apparently stops the nitrites turning into the more carcinogenic nitrosamines.
http://en.wikipedia.org/wiki/Sodium_nitrite
Very interesting series. As you know pork and poultry(both with large amounts of Omega 6’s) are consumed in Asia. Granted portions are smaller, but level of heart disease is lower for one than what we see in the West,and many Omega 6 oils are used as well. Are you aware of magnitude of liver disease in these populations?
How does O6 in pork compare to chicken and duck?
Wonderful work, Paul.
Are you familiar with Sally Fallon’s take that pork consumption immediately causes noticeable changes in the blood and that the curing process somehow prevents this?
You have me wondering about the PUFA variation in other animals now!
Ugh. Those pictures are sobering. Don’t think I’ll buy anymore supermarket pork for that reason alone. As for the destination of this series, I don’t think I am going to like it. I keep thinking about those scrumptious belegtes broetchen mit mett und zwiebeln (raw pork sandwich with onions) that I used to relish in the early 80s. Yum and probably dumb.
This makes me wonder if there is a reason for eating sauerkraut with pork. Although it is usually heated, which might negate it’s good properties.
I am really hoping I don’t have to give up bacon, liverwurst and pork tenderloins.
A famous herbalist, Dr. Wheelwright, used to say that the amino acid profile of pork was different — if I’m remembering correctly, that the amino acid chains were very long in comparison to other meats, and therefore, difficult to digest by most. Also, one of the most recent journal from the Weston A. Price Foundation showed live blood cell analysis effects from eating port — the effects weren’t good. I don’t remember there being an explanation for why that is. Interesting.
It’s all very interesting. I wonder if, since curing (even with nitrites! amazing!) reduces risk factors, would other traditional preparations such as brining in acid, also do the same. Perhaps it’s merely a factor of non-traditional prep of fresh pork. (ala this, which I am sure you’ve seen http://www.westonaprice.org/cardiovascular-disease/how-does-pork-prepared-in-various-ways-affect-the-blood)
thanks!
i only get pasture pork & chicken from now on.
(chickens are treated most poorly i read)
regards,
You are probably looking for a live pathogen, but consider that even deactivated pathogens might have imflammatory effects in a pro-inflammatory milieu.
This is analogous to killed probiotic lysates like Del-immune V, which can have the immunomodulatory effects of live probiotics – sometimes more so – without the risks to immunosuppressed patients.
If a live pathogen would lead to an inflammatory response by liver immune cells, it is possible that dead pathogenic antigens that reached the liver could initiate a similar response.
Just as a killed virus triggers immune reactions in a vaccine.
Another possibility is a combination of two or three factors – iron in the context of a food high in arachadonic acid, plus perhaps retinol.
(we might have to look at preformed arachidonic acid as being more problematic than shorter-chain omega 6s).
If the pig is already suffering inflammation itself its iron stores might not be as heme-bound as those of beef, and would react with AA, as the beef iron does not react with SFA.
Does curing lower the iron content of pork? It does become less red.
I buy pig hearts and kidneys for my dog occasionally, and like to compare them to sheep organs. A sheep heart is firm where a pig heart is flabby and soft. A sheep kidney is well-made and distinct in its parts, a pig kidney is soft and pulpy and in one case a pig kidney I froze was malformed with a half-inch ball of frozen urine in a cavity.
From Hell, indeed.
Regarding killed antigens, one of the findings in the beef fat/coconut oil/corn oil/alcohol experiments was that SFA inhibited LPS (antigens or endotoxins, usually from bacteria) activation;
it is mentioned here
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1858404/
Our results suggest that enhanced LBP and CD14 expression correlates with the presence of pathological liver injury in alcoholic liver injury. Furthermore, unsaturated fatty acids may prime cells to respond to endotoxin by enhancing CD14 expression.
Endotoxin in this case is cell walls of dead pathogens. Infmammatory immune cells like Th17 are more likely to react to antigens when self cells are being damaged at the same time (the danger hypothesis).
Off topic: what to make of the news of high levels of arsenic in brown rice syrup?
I checked the Ludenberg site, no info there. Unfortunately they don’t tell us what products were tested.
I’m switching to sugar for baking for my kids for now til I know more, and switching from white rice flour back to sprouted wheat, or white. Sigh. Parenting is so humbling, you think you’re making good choices for your family, and then news like this makes you want to curl up into a ball.
Yay, I approve. It is rare to see bloggers and authors talk about mitigating factors, especially with meats, but there we have it, and elsewhere. I’m looking forward to the next post.
Look at this; Forsythe, Volek et al. appear to be saying that AA is oxidised less on a carb-restricted diet.
Comparison of Low Fat and Low Carbohydrate Diets on Circulating Fatty Acid Composition and Markers of Inflammation
Cassandra E. Forsythe, Stephen D. Phinney, Maria Luz Fernandez, Erin E. Quann, Richard J. Wood, Doug M. Bibus, William J. Kraemer, Richard D. Feinman and Jeff S. Volek
Abnormal distribution of plasma fatty acids and increased inflammation are prominent features of metabolic syndrome. We tested whether these components of metabolic syndrome, like dyslipidemia and glycemia, are responsive to carbohydrate restriction. Overweight men and women with atherogenic dyslipidemia consumed ad libitum diets very low in carbohydrate (VLCKD) (1504 kcal:%CHO:fat:protein = 12:59:28) or low in fat (LFD) (1478 kcal:%CHO:fat:protein = 56:24:20) for 12 weeks. In comparison to the LFD, the VLCKD resulted in an increased proportion of serum total n-6 PUFA, mainly attributed to a marked increase in arachidonate (20:4n-6), while its biosynthetic metabolic intermediates were decreased. The n-6/n-3 and arachidonic/eicosapentaenoic acid ratio also increased sharply. Total saturated fatty acids and 16:1n-7 were consistently decreased following the VLCKD. Both diets significantly decreased the concentration of several serum inflammatory markers, but there was an overall greater anti-inflammatory effect associated with the VLCKD, as evidenced by greater decreases in TNF-?, IL-6, IL-8, MCP-1, E-selectin, I-CAM, and PAI-1. Increased 20:4n-6 and the ratios of 20:4n-6/20:5n-3 and n-6/n-3 are commonly viewed as pro-inflammatory, but unexpectedly were consistently inversely associated with responses in inflammatory proteins. In summary, a very low carbohydrate diet resulted in profound alterations in fatty acid composition and reduced inflammation compared to a low fat diet.
Here’s the bit:
In our recent study comparing low fat to VLCKD [8], we proposed that the increase in plasma arachidonate in response only to the low-carbohydrate diet was best explained by decreased degradation presumably due to less interaction with reactive oxygen species [122]. Increased production from 18:2n 6 was unlikely since the metabolic intermediates 18:3n 6 and 20:3n 6 were reduced in all three circulating fractions measured (TG, CE, and PL)and there was no increase in 20:3n 9, which typically occurs in cases where PUFA anabolism is increased. Since arachidonate was elevated in all circulating fractions in the low-carbohydrate diet, a shift from other pools was unlikely. Thus, an increase in the proportion of arachidonate resulting from a diet that restricts carbohydrate may be due to lower catabolism (i.e., better preservation) and, therefore, reduced formation of proinflammatory products. Scenarios associated with less oxidative stress should result in better preservation of the substrate arachidonate since free radicals take part in several steps in its metabolism. Inflammatory
cytokines are known to increase production of hydroxyl radicals which in turn initiate arachidonic acid release and breakdown.
The VLCKD in this study resulted in significantly greater reductions in several proinflammatory markers including TNF-a, E-selectin,
ICAM-1, and IL-8, that were associated with the increase in arachidonate. The significantly greater reduction in TNF-a in subjects following the VLCKD is of interest in that it is one of the agents
known to activate NF-jB a major transcription factor regulating cytokines, chemokines and adhesion molecules (TNF-a, MCP-1,IL-8, E-selectin, and ICAM-1) [123,124].
Hi Steph,
I discussed the arsenic in rice issue here: http://perfecthealthdiet.com/?p=5231, #6.
It’s mostly in the bran and highest in rice from former cotton-growing regions of the American South, since arsenic was used against boll weevils in the 19th century.
So white rice syrup would be better, but also rice from places other than the US south. Asian rice is low in arsenic.
Lundberg brown rice syrup is from California, I wouldn’t expect it to have a large amount of arsenic.
Best, Paul
Oh Paul, thank you for the reply! Sorry, I had missed your earlier post addressing this.
Kindly ignore the parent freak-out above.
🙂
You are still not getting your hands on my pork belly strips! 😀
I think that people should take more notice of the following song:- http://www.youtube.com/watch?v=d-diB65scQU
The point that should be emphasized, and almost NEVER is, is that the key is EXCESS omega six fats are harmful, not omega six fats themselves, which are essential.
Many patients have actually been found to be deficient in o-6’s and have excess o-3’s in studies done by Patricia Kane PhD.
Google for more info.
Awesome! I have been thinking about this lately since I am a BIG fan of bacon, but over the last 6 months have not eaten it as much as I have followed the PHD and it does not appeal to me. The idea of eating fresh pork is gross to me…never liked it and don’t now. Not sure why. I never liked fresh pork. Bacon and cured pork I loved however in the past. I don’t eat much now.
I wonder if the negative health effects has to do with how similar pigs are to us. The same pathology? Almost like cannibalism?
Thanks for the great information!
Robin
In the book http://www.amazon.com/Art-Science-Low-Carbohydrate-Living/dp/0983490708/ref=sr_1_1?s=books&ie=UTF8&qid=1329577342&sr=1-1
on page 47:
“Similarly, between 1929 and 1978, two essential fatty acid families (the omega-6 and omega-3 classes) were defined. If these polyunsaturated fats are not sufficient in the diet over months (omega-6) or over decades (omega-3), then overt disease and dysfunction occur. Omega-6 deficiency causes skin rash, growth stunting and sterility. Omega-3 deficiency causes heart disease (and possibly) dementia) in the first generation, plus impaired neurological/visual/intellectual development in the second generation.”
Hi Ron,
Yes, but the amounts needed to avoid a deficiency are small. 1% of energy. Most foods have substantially more than that. This is discussed in our book; it was very difficult to prove a human need for these fats, because no one is deficient on natural diets.
My post was, actually, to add weight to Kelly’s post (above)that addressed the “essential” qualities of these fatty acids. That post also pointed out the imbalance of those elements that sometimes occurs in the human diet.
Robin,
the paleoanthropological record doesn’t support the idea that cannibalsm is bad for us… I half suspect that aquiring an appetite for soylent green was what made us fully human in the first place.
Ray Peat has done a great service in calling into question the essentiality of EFAs. You can get a deficiency of carnitine quite easily, but that doesn’t mean that carnitine is essential in the diet, just that its deficiency is a product of other deficiencies or pathologies.
They didn’t used to put omega-3 in baby formula, but I’ve met people raised on the old omega-6 formula whose brains have obviously developed properly.
There are endogenous omega-9 PUFAs called meade acids that pinch-hit for the putative EFAs when these are not supplied.
Oxidative stress will break down PUFAs and this can create deficiency; there is a case like this in Paul’s blog. It can be established that it is good to have the PUFAs found in animal foods in a natural balance, and if not to get the EFA precursors from plants, but this does not of itself constitute proof of essentiality. Because EFAs are found in all cells even fruitarians do not become deficient through diet.
About killed probiotics being more immunogenic than live ones, see this article http://www.nutritiondynamics.com/nutrinews/novdec/
Apply this to killed or easily killed pathogens, arriving at the liver through a leaky gut (the alcohol connection) and you can see how, in a certain milieu, chronic inflammation might result from repeated unsuccessful ATTEMPTS at infection, without necessarily leaving the signs of a live infestation.
Otherwise, wouldn’t the CDC and USDA be all over it?
I’ve been eating quite a lot of pork lately as there is a really tasty roast pork dish at a Cuban takeout place near my office. I’ve definitely noticed some gut irritation, and have wondered whether it is the spicing, the omega-6 content or the meat quality. I don’t have these reactions at all when I eat bacon, despite frying eggs in the bacon’s grease as well.
so at one point they say stay away from cured bacon and now we should stay away from uncured bacon? How about all the preservatives and chemicals that are placed in our foods.
How does that come in to play as well with the high Omega 6 Ratios?
Would it be safe just to avoid pork all together? If we do buy bacon, can we buy one that is naturally cured without preservatives or should we go to the preservative route?
Does anyone have information about how to pickle pork at home? From the Weston A Price link, it looks like some processing; pickling, marinating; is what is required. You can preserve pork with celery nitrates if you like, but celery contains other toxins such as psoralens and coumarins. Nitrates don’t look like the worst additives at reasonably low levels, but levels used can vary a lot.
Naturally fermented pork salami is great if you can get it.
Paul:
What are your thoughts on inflammation and consumption of eggs – particularly the yolks – and poultry
as increasinginflammation because of
their alleged high levels of Arachidonic (sp?) acid?
Linda
Hi Linda,
I think it’s a valid concern. After liver and bones, eggs would be my highest priority for shifting to pastured animals with natural feed. I wouldn’t go overboard on eggs, but I think 3 a day is a good amount to eat, the nutrition outweighs the concerns.
have you considered the fact that the pork Generally consumed by the public has been bred to produce “white” meat? so perhaps there is a genetic component to the production of the omega 6 fats? Heritage pork (pork that is genetically not interbred and has been the same for a really long time) is not “white meat” but is “red”. Just a thought, let us know what you think about this idea.
Hi Angela,
It’s a good question. I haven’t seen analysis of what the breeding has done to meat quality, so I don’t know. But I think diet and lifestyle has a much bigger influence on omega-6 levels than genes. I think heritage breeds in a CAFO setting will have high omega-6 levels, and the “white meat” breeds in a natural setting will have lower omega-6 levels.
We always select organic when possible and grass-fed. If we buy bacon we buy unprocessed no nitrates and we don’t eat it often. What really concerns me is that my Savannah cat, yes cat, eats mostly fresh raw pork. She is extremely picky about the store I buy it from, too! Only one place and only boneless loin chops that I slice up for her (and freeze first for 3 days to kill any pathogens). I know cats are carnivores and eat what they catch in the wild and I can’t see a cat catching a pig but this is her choice! She alternates eating raw organic chicken breast and supplements with a dry grain free cat food. Now I’m even more concerned about what to feed her. Us “cat parents” worry, too!
The biggest problem with this article and the articles cited, is the persistence of the “bad fats, bad cholesterol” myths we have subjected to for the last 50 – 60 years. I suggest everyone read Gary Taubes, “Good Calories, Bad Calories” for background on the bad science that resulted from decades of people in positions of power using that power instead of science to make their pet theories gain acceptance. We have suffered for it and will continue to do so until enough doctors learn how to do science instead of merely following “received knowledge”.
The bad things that can happen to your body leading to metabolic syndrome and related problems like diabetes myelitis are not caused by fats, but refined and concentrated carbohydrates.
Medical school curricula need serious revisions in biochemistry and nutrition, to name just two subjects touched on here. For example: Some day soon you will be reading about how they had it wrong… cholesterol does not causes the plaque in atherosclerosis, it is an innocent bystander, ubiquitous and necessary in numerous bodily functions; the disease is a result of inflammation and the cause appears to be bacterial.
BTW, just because it does appear to be true that Omega 3 fatty acids are beneficial, that does not mean that Omega 6’s are in and of themselves bad for you; your body needs both (and others) and animal fats are good sources. Beware fish oil and while krill oil may be a good source of Omega 3, beware the hype used to sell it.
I will now prepare my usual breakfast of bacon and eggs.
Hi MaryEllen,
Well, there’s a fair chance that these pig/human pathogens may not be that good at infecting cats. Also, they often require decades to generate disease in humans; they might not have time in a cat to cause serious disease.
As we know from Pottenger’s cats, cooking meat destroys taurine and possibly other nutrients cats need. So, though no solution is perfect, it seems reasonable to let your cat enjoy her raw pork!
Hi Steve,
The problem with polyunsaturated fats is well attested and is not bad science. It does not derive from the lipid hypothesis, in fact 40 years ago people thought polyunsaturated fats would be good because they can reduce serum cholesterol. So they actually advocated vegetable oils!
Unfortunately there are other things that can harm us beside carbohydrates.
As we discuss in our book, omega-3 fats are only beneficial up to a point; like omega-6 fats they are toxic in excess.
Best, Paul
It was wonderfully refreshing to read an article in which the quality of supporting documentation was so through. As as research scientist with a strong passion about food quality I get so tired of reading articles that spew out unreferenced and/or unproved comments. Those types of articles usually end up with a three hour adventure at the NCBI website pulling journal articles…ugg.
Fantastic article, Thank you!