In Food Fortification: A Risky Experiment?, Mar 23, 2012, we began looking at the possibility that fortification of food, especially the enriched flours used in commercial baked goods, with niacin, iron, and folic acid may have contributed to the obesity and diabetes epidemics.
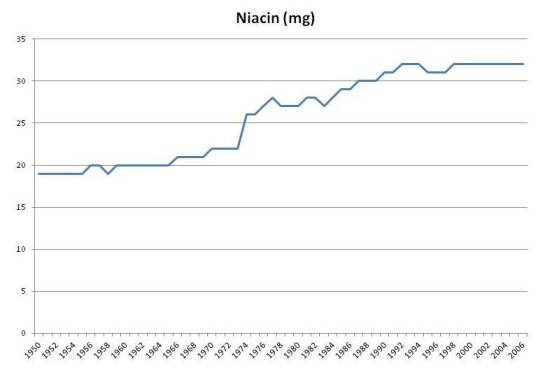
As this plot shows, fortification caused intake of per capita niacin intake in the United States to rise from about 20 mg/day to about 32 mg/day:
Multivitamins typically contain about 20 mg niacin, so (a) a typical American taking a multivitamin is getting 52 mg/day niacin, and (b) if the increase of 12 mg/day due to fortification is dangerous, then taking a multivitamin would be problematic too.
There wasn’t evidence of niacin deficiency at 20 mg/day. The RDA was set at 16 mg/day for men and 14 mg/day, levels that equalize intake with urinary excretion of niacin metabolites [source: Dietary Reference Intakes]. Fortification of grains with niacin was designed to make refined white wheat have the same niacin content as whole wheat, not to rectify any demonstrated deficiency of niacin.
B-vitamins are normally considered to have low risk for toxicity, since they are water soluble and easily excreted. But recently, scientists from Dalian University in China proposed that niacin fortification may have contributed to the obesity and diabetes epidemics. [1] [2]
Niacin, Oxidative Stress, and Glucose Regulation
The Chinese researchers note that niacin affects both appetite and glucose metabolism:
[N]iacin is a potent stimulator of appetite and niacin deficiency may lead to appetite loss [10]. Moreover, large doses of niacin have long been known to impair glucose tolerance [23,24], induce insulin resistance and enhance insulin release [25,26].
They propose that niacin’s putative negative effects may be mediated by oxidative stress, perhaps compounded by poor niacin metabolism:
Our recent study found that oxidative stress may mediate excess nicotinamide-induced insulin resistance, and that type 2 diabetic subjects have a slow detoxification of nicotinamide. These observations suggested that type 2 diabetes may be the outcome of the association of high niacin intake and the relative low detoxification of niacin of the body [27].
The effect of niacin on glucose metabolism is visible in this experiment. Subjects were given an oral glucose tolerance test of 75 g glucose with or without 300 mg nicotinamide. [1, figure source]
Dark circles are from the OGTT with niacinamide, open circles without. Plasma hydrogen peroxide levels, a marker of oxidative stress, and insulin levels were higher in the niacinamide group. Serum glucose was initially slightly higher in the niacinamide group, but by 3 hr had dropped significantly, to the point of hypoglycemia in two subjects:
Two of the five subjects in NM-OGTT had reactive hypoglycemia symptoms (i.e. sweating, dizziness, faintness, palpitation and intense hunger) with blood glucose levels below 3.6 mmol/L [64 mg/dl]. In contrast, no subjects had reactive hypoglycemic symptoms during C-OGTT. [1]
Of course 300 mg is a ten-fold higher niacinamide dose than most people obtain from food, but perhaps chronic intake of 32 mg/day (52 mg/day with a multivitamin) daily over a period of years have similar cumulative effects on glucose tolerance as a one-time dose of 300 mg.
Is There a Correlation with Obesity?
OK. Is there an observable relationship between niacin intake and obesity or diabetes?
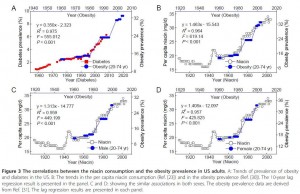
There may be, but only with a substantial lag. Here is a figure that illustrates the possible connection [2, figure source]:
Niacin intake maps onto obesity rates with a 10-year lag. After niacin intake rose, obesity rates rose 10 years later. Note the scaling: a 60% increase in niacin intake was associated with a doubling of obesity rates 10 years later.
Obesity leads diabetes by about 15 years, so we could also get a strong correlation between niacin intake and diabetes incidence 25 years later. The scaling in this case would be a 35% increase in niacin associated with a 140% increase in diabetes prevalence after a lag of 25 years.
How seriously should we take this? As evidence, it’s extremely weak. There was a one-time increase in niacin intake at the time of fortification. A long time later, there was an increase in obesity, and long after that, an increase in diabetes. So we really have only 3 events, and given the long lag times between them, the association between the events is highly likely to be attributable to chance.
It was to emphasize the potential for false correlations that I put the stork post up on April 1 (Theory of the Stork: New Evidence, April 1, 2012). Just because two data series can be made to line up, with appropriate scaling of the vertical axis and lagging of the horizontal axis, doesn’t mean there is causation involved.
Is There Counter-Evidence?
Yes.
If niacin from wheat fortification is sufficient to cause obesity or diabetes, with an average intake of 12 mg/day, then presumably the 20 mg of niacin in multivitamins would also cause obesity or diabetes.
So we should expect obesity and diabetes incidence to be higher in long-time users of multivitamins or B-complex vitamins.
But in fact, people who take multivitamins or B-complex vitamins have a lower subsequent incidence of obesity and diabetes.
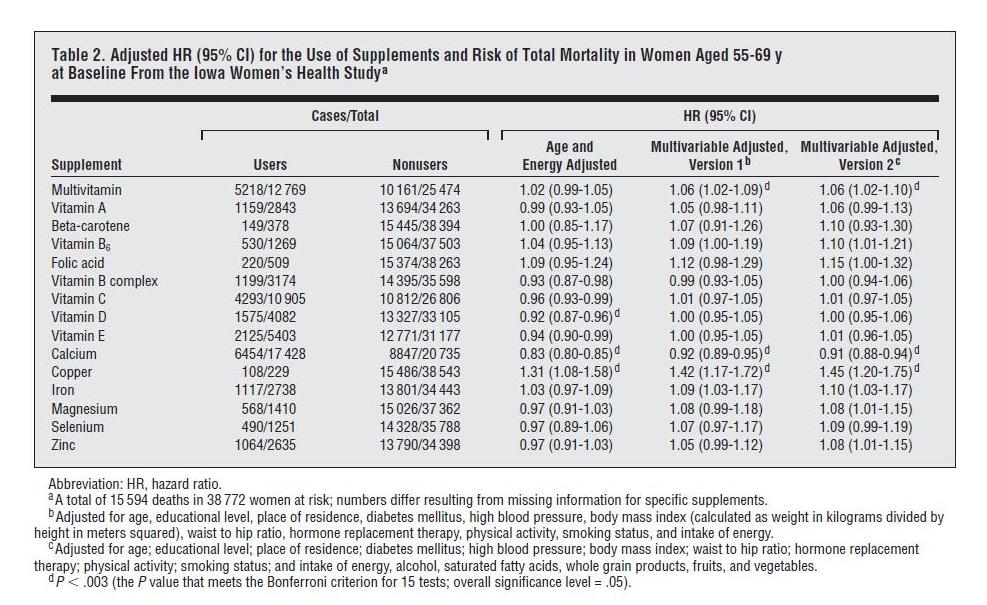
One place we can see this is in the Iowa Women’s Health Study, discussed in a previous post (Around the Web; The Case of the Killer Vitamins, Oct 15, 2011). In that post I looked at a study analysis which was highly biased against vitamin supplements; the authors chose to do 11-factor and 16-factor adjustments designed to make supplements look bad. The worst part of the analysis, from my point of view, was using obesity and diabetes as adjustment factors in the regression analysis. As you can see in the table below, multivariable adjustment including obesity and diabetes significantly raises the mortality associated with consumption of multivitamins or B-complex supplements:
This increase in hazard ratios (“HR”) with adjustment for obesity and diabetes almost certainly indicates that the supplements reduce the incidence of these diseases.
Multivitamins are protective in other studies too. The relation between multivitamin use and subsequent incidence of obesity was specifically analyzed in the Quebec Family Study, which found that “nonconsumption of multivitamin and dietary supplements … [was] significantly associated with overweight and obesity in the cross-sectional sample.” [3]
Does this exculpate niacin supplementation? I don’t think so. In general, improved nutrition should reduce appetite, since the point of eating is to obtain nutrients. So it’s no surprise that multivitamin use reduces obesity incidence. But multivitamins contain many nutrients, and it could be that benefits from the other nutrients are concealing long-term harms from the niacin.
Conclusion
At this point I think the evidence against niacin is too weak to convict in a court of law.
Nevertheless, we do have:
- Clear evidence that high-dose (300 mg) niacinamide causes oxidative stress and impaired glucose tolerance. If niacinamide can raise levels of peroxide in the blood, what is it doing at mitochondria?
- No clear evidence for benefits from niacin fortification or supplementation.
Personally I see no clear evidence that niacin supplementation, even at the doses in a multivitamin, is likely to be beneficial. Along with other and stronger considerations, this is pushing me away from multivitamin use and toward supplementation of specific individual micronutrients whose healthfulness is better attested.
I also think that food fortification was a risky experiment with the American people, and stands as yet another reason to avoid eating grains and grain products. (And to rinse white rice before cooking, to remove the enrichment mixture.)
References
[1] Li D et al. Chronic niacin overload may be involved in the increased prevalence of obesity in US children. World J Gastroenterol. 2010 May 21;16(19):2378-87. http://pmid.us/20480523.
[2] Zhou SS et al. B-vitamin consumption and the prevalence of diabetes and obesity among the US adults: population based ecological study. BMC Public Health. 2010 Dec 2;10:746. http://pmid.us/21126339.
[3] Chaput JP et al. Risk factors for adult overweight and obesity in the Quebec Family Study: have we been barking up the wrong tree? Obesity (Silver Spring). 2009 Oct;17(10):1964-70. http://pmid.us/19360005.












The effect on glucose tolerance – I predict that subjects would quickly adapt to this effect if the study was prolonged. Personally I never noticed that 500mg niacinamide 3x a day for a couple of years caused any blood sugar problems, and I was alert to the possibility.
At lower doses niacin levels are regulated by variations in tryptophan conversion. Tryptophan is a significant source of niacin (B6 is required); this needs to be factored in.
In addition to its synthesis from dietary niacin, NAD may also be synthesized in the liver from the dietary amino acid, tryptophan. The relative ability to make this conversion varies greatly from mice to humans. The synthesis of niacin from tryptophan also depends on enzymes that require vitamin B6 and riboflavin as well as an enzyme containing heme (iron). On average, 1 mg of niacin can be synthesized from the ingestion of 60 mg of tryptophan. Thus, 60 mg of tryptophan are considered to be 1 mg of niacin equivalents (NE). However, studies of pellagra in the southern U.S. during the early twentieth century indicated that the diets of many individuals who suffered from pellagra contained enough NE to prevent pellagra (3), challenging the idea that 60 mg of dietary tryptophan are equivalent to 1 mg of niacin. In particular, one study in young men found that the tryptophan content of the diet had no effect on the decrease in red blood cell niacin content that resulted from low dietary niacin (7).
Causes of niacin deficiency
Niacin deficiency or pellagra may result from inadequate dietary intake of niacin and/or tryptophan. As mentioned above, other nutrient deficiencies may also contribute to the development of niacin deficiency. For instance, patients with Hartnup’s disease, a hereditary disorder resulting in defective tryptophan absorption, have developed pellagra (2). Carcinoid syndrome, a condition of increased secretion of serotonin and other catecholamines by carcinoid tumors, may also result in pellagra due to increased utilization of dietary tryptophan for serotonin rather than niacin synthesis. Further, prolonged treatment with the anti-tuberculosis drug, Isoniazid, has resulted in niacin deficiency (8).
http://lpi.oregonstate.edu/infocenter/vitamins/niacin/
Recently, a large case-control study found increased consumption of niacin, along with antioxidant nutrients, to be associated with decreased incidence of oral (mouth), pharyngeal (throat), and esophageal cancers in northern Italy and Switzerland (17, 18). An increase in niacin intake of 6.2 mg was associated with about a 40% decrease in cases of cancers of the mouth and throat, while a 5.2 mg increase in niacin intake was associated with a similar decrease in cases of esophageal cancer.
This is really interesting:
Nicotinamide has resulted in decreased insulin sensitivity at doses of 2 grams/day in adults at high risk for insulin-dependent diabetes (20).
http://www.ncbi.nlm.nih.gov/pubmed/8866571?dopt=Abstract
Niacinamide/niacin might promote IR via the ketone body receptor.
Too many variables in all these vitamins/supplements. Lots of recommendations and then counter-recommendations. It is a lot cheaper and easier to just log your food with one of the many websites or apps and then adjust intake to meet needs.
once again, a great blogpost, Paul.
I see you dug deeper into this issue after our last conversation.
I like your conclusion “Personally I see no clear evidence that niacin supplementation, even at the doses in a multivitamin, is likely to be beneficial.”
… but want to bring up another point of great importance that speaks AGAINST using nicotineamide at all
now if nicotinamide riboside is the only precursor that elicits the beneficial effect, we got a serious problem with the tons of nicotine amide everyone is getting from his “non-flush” vitamin pills, since the former (nicotinamide) has to be hydrolized of the pyrophosphate bond to yield nicotinamide mononucleotide, which must then be dephosphorylated to nicotinamide riboside and this could be a problem / bottle neck, since
Now this does not tell us that appropriate conversion does not happen at later stages, but something tells me that we would not have “groundbreaking” research (http://www.sciencedirect.com/science/article/pii/S1550413111003469) stating that nicotinamide mononucleotide supplementation can heal diabetes, if the conversion of the tons of nicotinamide in our “food” (+supplement) chain would in fact take place.
Riboside appears to be better, but if you were researching it, you would say that other alternatives are useless, wouldn’t you?
Another angle is how supplementing NAD+/NADH precursors in any form affects the NAD+/NADH ratio; does supplementing B3 increase NAD+ in situations (reductive stress) where NADH is too high?
Niacinamide also improves insulin output and protects beta cells; this in itself could result in “insulin resistance” type readings.
Niacinamide (and especially N riboside, but where do you get it?) is an antiinflammatory wonder drug, and should be used more often (for example, in arthritis, liver fibrosis) but of course, healthy people don’t need drugs.
Also, B3 supps are more effective used with carnitine, Co-Q10, whatever mitochondrial antioxidants are needed.
http://www.ncbi.nlm.nih.gov/pubmed/21479726
Virchows Arch. 2011 Jun;458(6):689-96. Epub 2011 Apr 9.
Nicotinamide inhibits hepatic fibrosis by suppressing DNA synthesis and enhancing apoptosis of hepatic stellate cells.
Jin J, Lee KB, Park SY, Jang JJ.
SourceDepartment of Pathology, Seoul National University College of Medicine, 28 Yongon-Dong, Chongno-Gu, Seoul, South Korea.
Abstract
Liver fibrosis and its end-stage disease, cirrhosis, are major worldwide healthcare burdens. In this study, we evaluated the inhibitory effects of nicotinamide (NA) on rat hepatic fibrogenesis and investigated its underlying mechanism. We examined the inhibitory effects of NA in vivo by using F344 rats in a thioacetamide (TAA)-induced fibrogenesis model and assessed the inhibitory effects in vitro by using the rat hepatic stellate cell line THSC-Cl6. In vivo, NA significantly attenuated liver fibrosis in TAA-treated rats as assessed by histological analysis using hematoxylin-eosin and Masson’s trichrome staining. In vitro, NA inhibited viability of THSC-Cl6 cells in a dose- and time-dependent manner, suppressed DNA synthesis, and induced apoptosis. Transcription of collagen mRNA and expression of alpha smooth muscle actin (the hallmark of activated hepatic stellate cells) were reduced by NA. Expression of the cell cycle-related proteins cyclin E, cyclin D1, and cyclin-dependent kinase (cdk)4, was reduced by NA treatment, but expression of cyclin A and cdk2 was not. Expression of the cdk inhibitors p16 and p21 was decreased by NA treatment, whereas expression of p27 was increased. It appears that NA inhibits rat hepatic fibrogenesis by suppressing DNA synthesis and enhancing apoptosis of hepatic stellate cells.
How do you rinse white rice? Is it sufficient to put it in a colander and run cold water over it for a couple of minutes?
Hi Andrea,
Yes, I think so. Shou-Ching puts the rice in cold water and pours the mixture through a strainer, repeating three times. But once is probably enough. If you get rid of 80-90% of the enrichment mixture then there should be no problem.
Are the benefits of high-dose niacin purely due to the flushing that it causes? I’ve experienced the niacin flush and it comes on quite suddenly. Whew!
Wine & intense exercise also cause flushing and they are both beneficial in the right amounts.
Paul,
What do you make of reports on high-dose niacin as a treatment for restless leg syndrome[1]? Can we hypothesize anything about its method of action that would point toward alternatives?
Sam
[1] http://boingboing.net/2010/05/17/restless-legs-syndro.html
The enriched bread products were just replacing the niacin that would be present if it was a whole-wheat product. So does that mean that the 20 mg/day might have been low because that was for a non-whole-wheat product? If you looked further back in history, would you find that people were consuming 32 mg/day when they were still eating whole-wheat?
How lond do you recommend soaking white rice? Overnight, as if you’re soaking beans or lentils?
Hi Mumsy,
Sorry, white rice doesn’t need soaking. I mis-wrote when I said Shou-Ching soaks it before rinsing. I’ve edited the comment.
Hi Jeremy,
If we look far enough back, people weren’t consuming whole wheat products at all, and were healthier.
Hi Sam,
There are other illnesses for which high-dose niacin has been reported to be therapeutic. I saw Dennis’s post about RLS and niacin, glad to see he’s getting publicity.
I’m not sure what the mechanism is, I’ll think about that.
Paul, do you know if fortified rice is always labeled as such? I use WF organic jasmine which doesn’t indicate that it is fortified.
Hi David,
I think it’s labeled as “enriched.” Not all rice is enriched.
Thanks Paul. Now that you mention it, I do recall seeing one of their other rices labeled “enriched”. Mine should be “un-enriched” 🙂
I can propose a number of reasons why niacin might help with RLS;
– vasodilation if RLS is caused by constricted blood flow
– NAD+ replenishment if RLS is caused by reductive stress
– Ketone body receptor activity improving neural function
In my case RLS cleared up on a low-carb diet; lower blood lipids and more ketones perhaps. Ketone bodies also supply NAD+ (from conversion of acetocetate + NADH to hydroxybutyrate + NAD+) and NAD+ allows beta-oxidation of fatty acids. NAD+ is the “carbohydrate flame” but ketones can also supply it.
What is more, niacin and niacinamide can adjust dopamine levels in their role as methyl acceptors, perhaps by competing for methyl groups used by COMT to degrade dopamine.
This effect probably also has a lot to do with hepatotoxicity of very high doses, as choline production will decrease (homocysteine is elevated by niacinamidde in excess of 1.5g daily). If so, this can be corrected easily with choline and methyl donors. The cholesterol-lowering effect of niacin may perhaps also be hepatotoxic if taken too far.
Tolerance to the niacin flush shows an unusual decrease in one prostagladin (E2 I think), not neccesarily a deficient intake of the vitamin, but it does indicate that niacin is likely to produce results; but a flush doesn’t mean it won’t help.
No-flush niacin (inositol hexanicotinate) is just as good for many uses, if the flush is a problem; but you do get used to it if you take small amounts regularly for a couple of days.
Paul..with due respect, I find this post perplexing.
The title is NIACIN (nicotonic acid / vit B3)
The evidence you present is on NIACINAMIDE.
They work on 2 very different pathways.
Niacin dosage at up to 3 grams p/day does substantially increase HDL with a side effect of flushing and no negative data has surfaced.
The slow release formula/no flush is inferior.
So! My questions are:
(1) Is raising HDL, albeit synthetically, significantly beneficial to a lipid profile and heart disease.
(2) Is high dose niacin deleterious to the liver?
BTW: I have used your PHD book as framework for my macro/micro nutrient eating habits.
@ michael,
for yr question #2, I have used 1.5g daily of niacinamide or no-flush niacin and somewhat smaller doses of niacin for antifibrotic and symptomatic treatment of hepatitis C for years at a time.
My liver function improved over this period.
I supplemented methyl donors as a precaution.
Clearance of niacin and niacinamide requires methyl groups and supplementing high doses while in a hypomethylation could be the cause of occasional toxicity.
Hepatotoxicity is however rare and reported cases were associated with poorly manufactured time-release niacin (not the same as no-flush niacin) and a niacin-contaminated niacinamide product.
That both these products were contaminated with other impurities is also possible.
Hi Michael,
At low doses, I’m assuming there’s not much difference in mode of action of nicotinic acid vs niacinamide. At 300 mg doses, there’s generally considered to be more toxicity from nicotinic acid than from niacinamide. So I was showing potential for harm at that dose from the “safer” form.
Niacin at high doses does cause liver damage, and the skin flushing is a toxicity reaction. The slow release form greatly increases the liver damage, that is why it is dangerous.
We have a post on “How to Raise HDL”: http://perfecthealthdiet.com/?p=3204. We recommend using coconut oil / occasional ketosis to raise HDL rather than niacin. They work on the same pathway, via the ketone receptor, but ketosis is safer.
Best, Paul
“Plasma hydrogen peroxide levels, a marker of oxidative stress, and insulin levels were higher in the niacinamide group. Serum glucose was initially slightly higher in the niacinamide group, but by 3 hr had dropped significantly, to the point of hypoglycemia in two subjects:”
It is known that Niacin suppresses free-fatty acids in the blood by inhibiting lipolysis:
“Nicotinic acid (NA), or niacin, lowers circulating levels of lipids, including triglycerides, very low-density lipoprotein-cholesterol, and low-density lipoprotein-cholesterol. The lipid-lowering effects have been attributed to its effect to inhibit lipolysis in adipocytes and thus lower plasma free fatty acid (FFA) level.” (Kang, et. al, 2011)
When lypolysis is inhibited, it is obvious that serum glucose would rise, because the liver will release glucose from the glykogen stores to provide fuel in the absence of fats.
Inhibiting the level of FFA will result in a greater demand of glucose. It is possible that those subjects didn’t had enough glykogen stores, thus serum glucose falls more rapidly, because it is consumed by the cells in a greater quantity in the absence of free fatty acids.
The effect of Niacin on glucose metabolism in the study cited as evidence that it impairs glucose-metabolism was carried out on subjects in risk for diabetes, which may not be applicable to the general population.
Anyway, the increased glucose demand explains both elevated and later dropped glucose as elevated insulin levels.
In 2011, Oh, et. al found an alternative explanation for niacin induced insulin resistance.
A 24 hour nicotinic acid (NA) infusion paradoxically resulted in a higher rate of lipolysis. Stopping NA treatming resulted in an even higher rate of lipolysis than before treatment.
The study concludes that “a 24-h continuous NA infusion in rats resulted in an FFA rebound, which appeared to be due to […] increased basal lipolysis in adipose tissue. In addition, our data support a previous suggestion that insulin resistance develops as a result of FFA rebound during NA treatment. Thus, the present study provides an animal model and potential molecular mechanisms of FFA rebound and insulin resistance, observed in clinical studies with chronic NA treatment.”
This may be the reason of the elevated hydron peroxide: There is a NA rebound which relases free fatty acids, probably highly polyunsaturated (especially in pre-diabetics, which likely have an damaged metabolism due to PUFA toxicity) thus resulting in a higher rate of peroxidation of fats.
I am not sure, but maybe the rebound happens when not enough glucose is consumed, which may lead to the release of originally suppressed fatty acids to provide fuel.
Is it true that niacin can be used as a chelator to remove heavy metals from the body?
I’ve also seen it recommended as an antidote to taking too many methylated vitamins-supposedly it stops methylation (or should I say some methylation-not all!) I guess this is what George is saying? So somebody who unknowingly has impaired mythelation would have a bad reaction to niacin? Correct me if I’m wrong please- just trying to put it all together.
Oh how I wish I was smart enough to understand all the science, If I take niacin my blood sugar goes up, but even worse I have trouble with irrational sudden anger with the sliest provocation. Even a couple of table spoons of nutritional yeast fortified with niacin will make me irritable. I have been searching for the answer, as to why niacin has such a negative effect on me, for a couple of years. Anyone with a suggestion of where I should be looking would ne greatly appreciated.
Hi Jim,
Try doxycycline and see if niacin still has that effect.
Dietrich Klinghardt claims great success reversing insulin resistance in Lyme patients using high-dose niacinamide: 1g t.i.d. (plus berberine).
Can anyone explain how this might work, given the argument here that niacinamide leads to or exacerbates insulin resistance? Not to mention Paul’s repeated claim that niacinamide feeds bacterial infections?
(I am a Lyme sufferer with severe insulin resistance, and I am considering giving the niacinamide a try — so this is not an idle question for me!)
Hi MM,
NAD+ which is produced from all the forms of niacin is used to produce superoxide/ROS which are the killing compounds of the immune system.
In a healthy person you don’t want a lot of this but in a sick person you may benefit from empowering the immune system with high doses of niacinamide.
Microbes cannot produce the same level of antioxidants as human cells (they are in a foreign environment, after all) and are vulnerable to very high levels of oxidative stress.
Chronic low doses of niacin will promote bacterial replication. Very high doses may promote immunity more. There are papers showing that high-dose niacinamide helps in some infections.
It’s a double-edged sword, my guess is the niacin will help systemic issues but may hurt neurological ones. But empirical evidence is the best guide.
Best, Paul
Paul,
What are your thoughts on high dose Niacin for mental health disorders. Have you ever looked into the research/clinical work by Abram Hoffer. Among other mental health disorders, he used high dose niacin to successfully treat schizophrenics. I believe, if I’m not mistaken, he pioneered a lot of work with orthomolecular medicine. And he was a big fan of high dose niacin for various conditions. I remember learning about him from one of my professors during naturopathic medical school.
Also, in regards to the B-vitamins as a whole, and your suggestion to avoid supplementation. From a clinical standpoint, when you have a patient with heart disease and high homocysteine levels (indicating likely poor methylation in the homocysteine cycle), and they don’t have a sound diet, outside of encouraging following a paleo/perfect health diet template (if they follow it fully or not), would there not be reason to provide methyl donors to methylate the homocysteine in order to decrease risk further, at least for a period of time?
I find so much of what you write about fascinating, as so much of it is counter to a lot of what I learned in my naturopathic medical training. However, sometimes I find it tough to utilize clinically with patients, especially when you have patients who aren’t willing to make the big changes necessary with the diet.
Any thoughts.
Thanks for your time,
Shawn
Hi again Paul,
Well, a quick search about Hoffer, wikipedia had this to say at the end….
Controversy
Hoffer’s claims regarding schizophrenia and his theories of orthomolecular medicine have been criticized.[21] In 1973, the American Psychiatric Association reported methodological flaws in Hoffer’s work on niacin as a schizophrenia treatment and referred to follow-up studies that did not confirm any benefits of the treatment.[22] Multiple additional studies in the United States,[23] Canada,[24] and Australia[25] similarly failed to find benefits of megavitamin therapy to treat schizophrenia. The term “orthomolecular medicine” was labeled a misnomer as early as 1973.[22] Psychiatrist and critic of psychiatry Thomas Szasz called Hoffer’s ideas about schizoprhenia “pure quackery” and his claims “arrogant” for attributing the condition to a nutrient deficiency as well as their support for Schizophrenics International, a group that attempts to deal with schizophrenia similar to alcoholism in Alcoholics Anonymous.[26]
In a 2006 interview, Hoffer stated that while he felt that current mainstream psychiatric care was “terrible”, his theories and treatments were starting to become more accepted. “We’re at a transition point. If I live another four or five years, I’ll see it.”[8]
I read a couple of his papers on the adrenochrome theory or neurotoxicity and it sounded so interesting. And, when I posed the question I was merely recalling the information taught to us by said professor, who himself was fond of Hoffer, high dose niacin, and orthomolecular medicine. Plus, I remember learning about the high dose niacin for cholesterol, but being aware to monitor liver enzymes during treatment. So, outside of a response to the Hoffer question, I’d still like to hear your thoughts on the latter questions.
Thanks,
Shawn
FWIW, in the last interview Hoffer gave he stated that one of his long-term high-dose niacin patients was a centenarian who still skied.
I think Hoffer was absolutely correct and thousands can testify that his is the right approach. I’ve seen it work myself.
@ Jim E
For bad reaction to niacin, see Pfieffer’s theory of high- and low-histamine types. Niacin elevates histamine, other supps such as calcium lower it – but look up this theory. You may be at the histadelic end of the spectrum.
Niacin is not recommended for all brain states.
I can also suggest that perhaps the specific vasodilatory prostaglandin released by niacin is something you are especially sensitive to.
No-flush niacin (with inositol) is NOT time release niacin, it has no record of liver reactions.
I consider it intermediate between niacin and niacinamide in its action.
Hi Shawn,
I don’t oppose B vitamin supplementation, I take some myself. But I don’t think it’s necessary to take them frequently. I don’t take any B vitamin more than once a week, take niacinamide rarely, and never folic acid. I think B1, B2, B5, biotin, B12 and B6 are reasonable things to take from time to time.
Of course, with evidence of deficiency such as high homocysteine there may be more reason to take B12 and B6.
High doses of B3 I consider a pharmaceutical drug rather than a vitamin. It’s an intriguing therapy for some conditions but last time I checked the literature, a few years ago, it seemed still in a rather speculative stage. But some papers indicated promise in certain conditions.
IMO, if you only had time to study one vitamin you’d find B3 the most rewarding.
You have tryptophan and its metabolism through kynurenic acid etc. to nicotinic acid (niacin) and picolinic acid, conversion to nicotinamide (niacinamide), N-riboside and NAD+/NADP+/etc.
Tryptophan (and its other metabolites serotonin and melatonin), and every metabolite of this degradation has its own activity and potentially has its level altered by niacin supplementation.
There is thus a kind of polypharmacy involved with B3 supplementation. Which is perhaps why it is the most effective vitamin for drug-type interventions.
Niacinamide from NADH breakdown is deactivated by methylation.
Histamine is also deactivated by methylation.
http://www.ajcn.org/content/85/5/1185.full
http://www.google.co.nz/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=4&ved=0CEcQFjAD&url=http%3A%2F%2Ffindarticles.com%2Fp%2Farticles%2Fmi_m0FDN%2Fis_6_7%2Fai_96416605%2F&ei=9WybT66ZEKSXiAf4nLS9Dg&usg=AFQjCNFg-_aCvEIt8e7XZLFiyzNNZFGvyQ&sig2=wlXVjuV10-m0rXGd1gltHg
(niacinamide monograph)
The best use for niacinamide I’ve found is as a substitute for benzodiazepines in anxiety disorder; niacinamide sensitizes to GABA and spares tryptophan, elevating serotonin.
Given the high addiction potential and cognitively dysfunctional effects of anxiolytic drugs, this is an especially valuable effect.
I also found niacin very useful when coming off meethadone, frequent small doses helped maintain an even sense of temperature and suppressed cravings when taken on top of l-carnitine and a high-fat, low-carb, no-allergen diet.
There is a brand of white rice called “Verde Valle – Morelos rice” that appears to be un-enriched. I found it in a Mexican grocery store.
Histamine is also deactivated by methylation. How would someone with allergies due to high generation of histamine address the issue of high histamine release via methylation?
Thanks.
Hi Steve,
You can support methylation by getting plenty of choline from egg yolks and liver, folate from green leafy vegetables, and supplementing a bit of B12 and B6.
Thanks Paul:
Have all the above incorporated in my diet except the supplemental B12 and B6 which i only get via my Centrum 50+ muli vitamin. Suggested dose level for B12 and B6 t0 be taken separately? With my atopic eczema, and airborne allergies am willing to try anything! Zyrtec,and its competitors really do nothing for me.
Thanks.
Hi Steve,
B12 is fairly non-toxic … 500 mcg is a safe dose, 5 mg is a pharmacological type dose that will make hair and nails grow much faster, it promotes cell division, might cost you some stem cells and accelerate aging but might promote healing … you decide.
B6 can be toxic so I would keep it under 100 mg on any one day and under 200 mg per week. I think 25 mg per day would be good, but take B12 along with it and don’t become folate deficient.
Thanks Paul:
Now in my 60’s I do not want to accelerate the aging process; seems to be going fast enough on its own!
Regards,
Paul,
Regarding: “Along with other and stronger considerations, this is pushing me away from multivitamin use and toward supplementation of specific individual micronutrients whose healthfulness is better attested.”
Any chance that we can get a blog entry on what you suggest for those “specific individual micronutrients”?
Thanks!
Hi Matt,
Yes, of course. But it may take a couple months to work through a bunch of posts and to analyze our own micronutrient intake across a few diet variations.
Hi Paul,
I could use your advice. My major problems are intestinal pain and gas, rosacea flushing (bright red nose, irritated eyes, headache, sometimes general itching at random places on my body), low energy (especially in the afternoon), and reactive blood sugar (fasting around 70-80, sometimes goes as high as 200 if I eat a lot of carbs, sometimes drops to around 45). I think I’ve been prone to low blood sugar my whole life. It seems to run in my family, although diabetes doesn’t. I just got a glucometer, so I can’t say for sure. The other problems appeared or got noticeably worse over the 9 or 10 years I was mostly vegan, especially the intestinal pain and low energy. I don’t know what to do because trying to fix any one problem seems to make others worse!
I started eating fairly low carb paleo-ish in January to try to fix my energy problems and intestinal pain. I probably ate 100-130 total carb g/day, but not much in the way of starches. I was a in-practice-mostly-vegan pescatarian before, and I started eating fish and eggs much more often. It initially seemed to help. I felt like I had more energy, especially in the afternoon when I would frequently be falling asleep before. My intestinal pain basically went away.
However, my rosacea flushing got much worse. I started flushing really badly after almost every meal. I seem to flush when I have either too much or too little stomach acid, and have taken betaine HCL for acid reflux off and on. Since I started eating more paleo, my acid production has become unpredictable, which is probably exacerbating the flushing, but doesn’t seem to be the whole story there. I often flush after eating lunch and dinner, but not always. Fish and shrimp cause it pretty reliably, although not always. I seem to be sensitive to something, but I’m not sure what it is (maybe histamine intolerance?).
Since discovering PHD, I’ve been trying to add more starchy carbs. The problem is that they seem to make my energy more uneven (which is why I stopped eating them in the first place). I often get really lethargic, slow-thinking, and almost drugged-feeling, like I’ve been tranquilized, after eating meals with any substantial amount of starch, even safe starch. It sometimes starts as soon as half an hour after I eat and it tends to last somewhere between half an hour and two hours. This is usually in the afternoon, when my energy is already not great normally. Eating starchy carbs also seems to make me constipated, though I’m not positive this is the cause.
I’m also worried because I recently went to the doctor to try and unravel some of these problems and he ran some blood tests. Here are those results:
Cholesterol
Total 268
LDL 161 (actually more like 124 if you use the Iranian equation, since I have low triglycerides)
HDL 88
Tri 47
A1c 5.3% (below the 5.7% reference, but seems high to me)
TSH 1.23 mIU/L
D3 202 ng/mL (I’ve been supplementing but I stopped when I got this result)
B12 >2000 pg/mL (this is in my multivitamin, but I’m not sure why it should be so high)
I had a high sed rate (73 mm/h) and low white cell count (3.5 thousand/uL; all the white blood cell types were normal but on the low end of their range), implying some kind of infection and maybe other inflammation.
The flushing after eating is driving me crazy. I feel like there’s nothing I can eat because everything makes me flush and gives me a headache. But then randomly I’ll eat a meal where I don’t flush at all! I don’t know what to do, or which of my problems to try to tackle first. What should I do?
Tess
Wow, sorry for that long post! Maybe I should also add that I’m 30 and normal weight (125 lbs at 5’6″).
Tess
Hi Tess,
First, your cholesterol and A1c and TSH are normal. D levels are way too high, good that you stopped. B12 levels are often high in bacterial infections.
Inability to regulate glucose often indicates an infection of the small bowel which may have reached the pancreas. Judging from your other numbers this is most likely to be bacterial.
High sed rate is consistent with bacterial infection.
The itching indicates an immune response to something, unclear what. Could be some kind of microbial toxins originating in the gut.
The rosacea could be due to amines generated in the gut. Some amines are vasoactive and cause flushing/redness.
Lethargy and brain fog indicates high immune activity, probably clearing toxins generated in the gut.
So, cumulatively, the likely issue is a gut infection which is generating amines from dietary protein as well as plenty of toxins which enter your body and trigger immune activity, itching, and fatigue.
I would get a stool profile and maybe SIBO & H pylori tests to try to diagnose the gut infection. I like the Metametrix microbial ecology stool test.
I would consider antibiotics, but try to get the diagnostic testing done first.
I would consider detox aids. These include salt, potassium-rich vegetables, magnesium, calcium from bone broth, and fluids for kidney detox; glutathione, vitamin C, taurine for liver detox and bile flow; possibly binding agents to carry fat-soluble toxins out in the stool (eg bentonite clay, activated charcoal, many plant fibers). These will help reduce symptoms and
Methylation precursors may help with amine disposal. B12, B6, green leafy vegetables, choline, are good supplements.
I would consider efforts to change the ecology of the gut. Eg betaine hydrochloride and more salt to promote stomach acid production which will help sterilize the small intestine; enzymes, especially polysaccharide digesting enzymes and proteases; and probiotics.
In general, recovery is a gradual process, but all of these things can help tip the balance of power and give your immune system a better chance.
Best, Paul
Paul,
Thank you for your detailed response to Tess, which was immensely helpful to me — and no doubt many others — as well. The time you devote to answering questions here is appreciated more than you can know!
Following up on something you wrote (as I am still struggling to get to the bottom of what is causing my own dysglycemia): how could one determine whether an infection of the small bowel had in fact reached the pancreas?
Thanks again.
Hi MM,
I’ve seen papers showing that pancreatic infections cause dysregulation of glucose, but I don’t know if there are clinical tests available for this.
I’m not sure that the treatment would be different than that for SIBO, either, so perhaps one doesn’t need to know.
Paul,
Your response is incredibly helpful. Thank you! I can’t tell you how much it means to have someone take enough interest to look at all of my symptoms together, instead of sending me to a different specialist for each one.
What kind of diet do you think I should be on? How low carb should I go, given my apparent blood sugar sensitivity and constipation problems? On the other hand, if I go very low for any length of time I seem to start getting the kind of symptoms you talk about—dry eyes, low energy, etc.