UPDATE: The Daily Mail article cited below was not only silly, it appears to have been dishonest. I’ve received the following email:
There is an article on your website about me (17/2/2011). Yes, I’m Judith Fine and that article was in the Daily Mail. Firstly, they completely twisted everything that I said so that it makes it look as if I have severe eating problems. Most of that article was a complete pack of lies, neither is it me in the photograph. Could you please, immediately remove it from you website as I am in the process of picking this up with the Daily Mail.
I’ve edited the post to remove content related to Judith. — PAJ
“Orthorexia” has been in the news recently, for instance in this Valentine’s Day article by Diana Appleyard in the Daily Mail:
We all know the type. They never let wheat, yeast or dairy pass their lips. They’ve cut out alcohol and caffeine. They’re obsessed with healthy eating — yet every day, they look more unwell and unhappier.
These are the symptoms of a condition called ‘orthorexia’ by dieticians….
Orthorexia was coined in 1997 by Californian doctor Steven Bratman in his book Health Food Junkies, and means ‘correct appetite’ (from the Greek orthos for right and orexis for appetite). It is a fixation with eating ‘pure’ food that, far from doing you good, can become so extreme that it leads to malnutrition, chronic ill health and depression.
Well, I don’t eat wheat; I didn’t even know yeast was a food; and though dairy is a big part of my diet, alcohol and caffeine modest parts, I recognize that milk proteins, alcohol, and caffeine can be problematic.
Given that none of these foods are necessary for good health, it’s not obvious to me why excluding them would lead to malnutrition, chronic ill health and depression.
But from the rest of the article, it looks like the real trouble with orthorexia is not the fixation with healthy eating, but faulty ideas of what constitutes a healthy diet. The article’s leading example of an unhealthy “orthorexic” diet is one that excludes fat.
Any fat-less diet is bound to be malnourishing. Perhaps the trouble is not orthorexia, but mistaken ideas about nutrition. Diets people think are therapeutic are, in fact, damaging.
Therapy versus Life … sometimes
Which brings me to a recent essay by Kurt Harris, “Therapy versus Life.”
It’s almost impossible to excerpt, so I’ll just assume you’ve read it. It’s strongly worded, but the ideas are familiar: I suspect at least 90% of medical doctors would agree.
Doctors are healers, God bless ’em; but every day they have to face patients they cannot heal. This breeds a certain mental toughness.
As I often say, malnutrition, food toxins, and chronic infections are the primary causes of ill health. In some cases, like Judith Fine’s inability to have periods, it’s easy to recognize malnourishment as a likely cause. But the causes of most patients’ impaired health are much less obvious.
Unfortunately, doctors generally cannot diagnose or treat either bad diets or chronic infections. Doctors are great at treating acute disease, and can mitigate many symptoms that chronic diseases generate, but most are helpless to remedy mild, chronic ill health.
Doctors may believe that a patient’s declining health is simply natural aging; or that genuine health impairments may be undiagnosable, untreatable, or incurable. Kurt says it in his forum:
[T]he healthy should not assume they are sick and even the sick may be wasting their time trying to fix what can’t be fixed.
When patients learn that doctors can’t help them, they often turn to experimental self-treatment.
99% of the time, this works out badly. As Kurt’s car metaphor shows, there are many more ways to damage your body than to heal it.
And the 1% of the time it works, the patient doesn’t go tell the doctor. But when it backfires, the patient goes back to the doctor worse than ever. So the doctors see this method fail 100% of the time.
This reinforces the doctors’ consensus: Be prudent. Try to live normally – as healthy people do. Eat like healthy people, live like healthy people, and bear with your incurable maladies as best you can. Thrashing and groping for cures will only do harm.
Therapy – experimental self-therapies – are damaging to life. Choose life, not therapy.
But Diet Is Therapy
But that’s not all there is to it … because the right diet can fix many health problems.
Kurt says this himself:
[T]here is a dietary metabolic milieu that we are adapted to, and the best chance we have of optimizing our health is to try and emulate it …
The human body often can [fix itself] if we just stop ruining it.
We agree. The Perfect Health Diet is, in essentials, identical to Kurt’s PaNu. And when people in ill health eat this way, they commonly get better.
So the right diet is therapy. Choose this diet as therapy, and you’ll have a better life.
What If Your Life is Malady-Inducing?
I chose life over therapy for decades. I rarely went to the doctor. I focused all my energy on life. But I ate a lousy diet.
This isn’t the place to tell my story – that’s coming – but a lousy diet and a focus on life, not therapy, gave me a disabling chronic disease.
And a therapeutic diet gave me my life back. The Four Steps of our book are essentially the steps I took to cure a disabling neurodegenerative condition. With antibiotics, they worked.
So when Kurt asks,
Do you think every problem in your life can be fixed by changing your diet?
I can honestly say: every health problem was fixed!
Therapy for Life
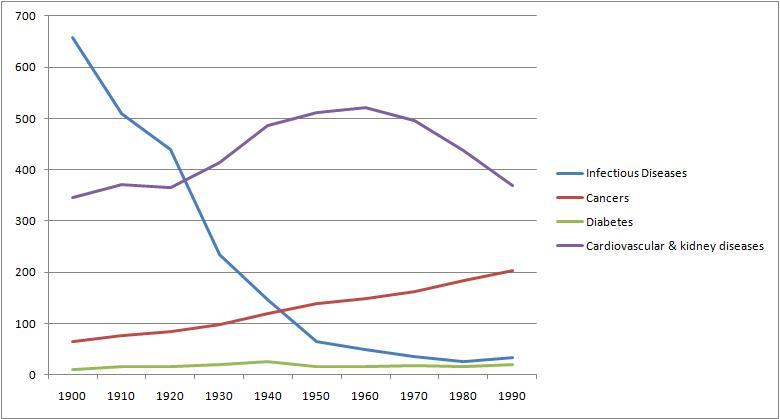
If the Ewald hypothesis and Jaminet corollary are right, then we all stand in need of dietary therapy. As we age, our infectious burden increases and our immune system gets less effective. Sooner or later, infectious diseases threaten us all.
Our rescue is not from medicine, which does not yet know how to treat chronic infections. Our best chance for a long, healthy life lies in diet, nutrition, and immunity-enhancing behaviors like fasting.
Fortunately, the scientific evidence is accumulating to tell us what the right diet is. Specialist professionals still can’t see the forest for the trees, the elephant for its parts; but generalists, aided by respect for ancestral/traditional diets and for evolutionary selection, have blazed the trail. Kurt lists some reliable guides.
Conclusion
Diet is the best therapy. A good diet is life-giving. Good diet and nutrition may cost a few extra minutes a day, but can add decades of happiness.
So I say: choose therapy AND life. We can be healthy centenarians together. Let’s do it!











Recent Comments