Chris Highcock of Conditioning Research mentioned a fascinating paper yesterday, and then Dr. Emily Deans blogged about it. The paper tells about mice who tore their fur out – akin to the condition of “trichotillomania” in which humans tear their hair out – after being put on a high-tryptophan diet. [1]
Dr.Deans points to the paper’s importance:
As far as I know, it may be the only paper showing a definitive development of psychopathology with an adjustment of diet. So that’s a big deal!
Since I suspect that most psychopathologies are induced by diet in the context of infection, I think this shows that psychiatric researchers have barely begun to understand their diseases.
As soon as I saw Chris’s post I knew I had to blog about it, because I had similar symptoms to these mice.
My Experience
Briefly, I had a chronic bacterial infection of the brain and nerves, probably from Chlamydophila pneumoniae, plus a few other problems which masked the bacterial infection until I fixed my diet.
C. pneumoniae is a parasitic intracellular bacteria whose main activities are reproduction and diversion of the immune system. Its main effects are:
- Neuronal hypoglycemia. C. pneumoniae steals glucose products like pyruvate for energy. This can create hypoglycemia in neurons even if blood glucose levels are normal.
- Serotonin deficiency. C. pneumoniae steals key amino acids like tryptophan, tyrosine, and phenylalanine for protein and niacin synthesis. Of these tryptophan is most important. To block C. pneumoniae activity, the innate immune response triggered by interferon gamma sequesters tryptophan. This denudes neurons of the neurotransmitter serotonin, which is made from tryptophan.
- Inflammation. C. pneumoniae is able to trigger inflammation which re-directs the immune response away from itself toward extracellular pathogens.
Thus common symptoms of a bacterial infection of the brain are those of cognitive hypoglycemia and serotonin deficiency. Symptoms include:
- Hypoglycemia : Feeling nervous or jittery; mood changes such as irritability, anxiety, restlessness; confusion, difficulty in thinking, and inability to concentrate; poor coordination.
- Serotonin deficiency: Anxiety, depression, impaired memory or cognition, low self-esteem, loss of pleasure, poor impulse control, insomnia.
These lists don’t fully capture the experience however.
I started having these symptoms in 1992 during a year-long course of antibiotics, and they would get worse for about the next 15 years. I experienced a dramatic loss of happiness and positive emotions. I had always been happy; now suddenly I wasn’t. Along with this came a weird mental state which is hard to describe, because it has no normal analog. Irritability or anger come closest, so I’ll use those words. But understand that it was a generalized state, not irritation or anger directed at anyone in particular; being naturally phlegmatic, I doubt in 20 years I was uncivil to anyone on more than a few occasions. It was just a persistent irritated/angry emotional state that I was well aware was unnatural and could consciously control.
It seemed like this negative emotional state would build up, and could be discharged a bit by a few expressive habits. I would wring my hands; I still have some slightly twisted finger bones and calluses from over a decade of hand-wringing. And, when alone, I would sometimes scratch my head. This sometimes led to hair loss and bare patches.
Trichotillomania
This kind of behavior turns out to be not that rare. About 4% of the population is said to have “trichotillomania,” compulsive pulling or twisting of the hair causing hair loss. Trichotillomania strikes women more frequently than men. [Wikipedia, “Trichotillomania” ]
Serotonin depletion is a common feature of mood disorders. I wouldn’t be surprised if most of these disorders are due to brain infections, and the serotonin deficiency is due either to theft of tryptophan by bacteria or to the immune response to intracellular infections, which increases interferon gamma and decreases serotonin.
Evidence, such as it is, is consistent with that idea. People with mood disorders or depression are far more likely than normal people to test positive for antibodies to chronic intracellular pathogens like coronaviruses. [2]
Drugs Help At First, But Often Do Long-Term Harm
The first impulse of modern medicine is to fight the body’s response to disease. If the body has downregulated serotonin, doctors look for drugs that upregulate it.
That is why people with depression and mood disorders are commonly given SSRI’s, drugs that raise serotonin levels.
If these diseases are due to infections, then we would expect the SSRI’s to improve mood immediately, but also to defeat the body’s immune response, supply the pathogens with tryptophan, and promote their replication. As a result, the disease should progress faster. In time, the patient will become worse than would have been the case without the drugs.
And, more often than not, this is what actually happens. Drugs are often “unsafe at any dose”. Antidepressant treatment increases mortality in men by 30%.
The Mice Who Tear Their Hair Out
One of the common breeds of mice used in laboratory research is the C57BL/6 breed. This breed has “an easily irritable temperament … [and] a tendency to bite … [and] display barbering behavior.” [Wikipedia, “C57BL/6”] In barbering, “individuals pluck whiskers and/or fur from their cage-mates and/or themselves.” [1]
C57BL/6 mice also have a modified immune response:
The immune response of mice from the C57BL/6 strain distinguish it from other inbred strains like BALB/c. For example the immunological response to the same pathogen in C57BL/6 mice is often of an opposite spectrum compared to BALBb/c mice, namely C57BL/6 shows Th1 and BALB/c shows Th2 response in response to intracellular pathogen Leishmania major, where a Th1 response results in a resistant ie healer phenotype (since the pathogen is intracellular), whereas a Th2 response results in a susceptible (nonhealer) phenotype. [Wikipedia, “C57BL/6”]
This Th1 response increases interferon gamma levels:
The Th1 response is characterized by the production of Interferon-gamma … [Wikipedia, “Adaptive Immune System”]
Interferon gamma, of course, sequesters tryptophan and diminishes neuronal serotonin levels.
All this sounds familiar: C57BL/6 have lower serotonin; they become irritable and will bite and tear fur out.
Like trichotillomania in humans, tearing of fur is more common in female mice than males: “Barbering is more frequently seen in female mice; male mice are more likely to display dominance through fighting.” [Wikipedia, “C57BL/6”]
Research Idea: Treat the Mice As We Do Humans
If these mice went to a human psychiatrist (and had health insurance), they’d be prescribed SSRIs to raise their serotonin levels.
A group at Purdue led by professor of animal sciences Joseph Garner decided to see if they could cure barbering through an alternative dietary therapy that would raise serotonin levels just like SSRIs.
[W]e wished to test the hypothesis that a diet which increases serotonin metabolism would decrease the hair-plucking behavior of barbering mice. [1]
The treatment diet was essentially identical to the control diet, except for these differences: Tryptophan levels were four times higher, methionine levels were the same, and other amino acids were halved. Overall protein levels were cut from 24% to 13.3% of calories. Since tryptophan competes with other amino acids for entry to the brain, this shift in amino acid composition led to much larger tryptophan entry to the brain. [1, Table 2] The lost protein calories were made up by increasing carb intake from 57.3% to 68.0%, which I consider a relatively marginal change. In both diets fructose was minimal, 2.5% of calories, and glucose, mostly from starch or dextrose, provided the bulk of the carbs.
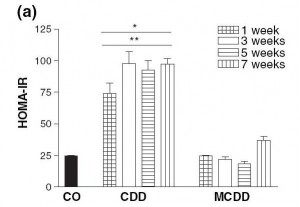
The tryptophan was converted to serotonin in the brain, but not for long. Serotonin levels were 55.5 ng/ml in brains of mice on the control diet, 57.6 ng/ml in brains of mice on the high-tryptophan diet [1, Table 3]. However, levels of serotonin metabolites – the leftovers after serotonin destruction – were much higher in the treatment mice.
The results weren’t good:
[E]levating brain serotonin metabolism by tryptophan and carbohydrate supplementation increased the severity of barbering, and induced ulcerative dermatitis. In humans, the induction of compulsive skin-picking by serotonergic agents (SSRIs) has been reported. (24,43) Thus, the current data suggest a homologous outcome in mice, achieved nutritionally instead of pharmacologically. [1]
If you don’t like scientific-ese, here’s Professor Garner in the press release:
[The] diet … was expected to reduce abnormal hair-pulling. Instead, mice that were already ill worsened their hair-pulling behaviors or started a new self-injurious scratching behavior, and the seemingly healthy mice developed the same abnormal behaviors….
“We put them on this diet, and it made them much, much worse,” Garner said.
This does indeed sound like a “homologous outcome” to the experience of human patients treated with SSRIs!
Very likely if the mice had been interviewed at Day 1 after initiation of the high-tryptophan, they would have reported mood improvements, just as human patients do on SSRIs. As with humans on SSRIs, the negative effects took some time to appear. The increase in scratching behavior was not apparent at 6 weeks after initiation of the high-tryptophan diet, but was apparent at 12 weeks (3 months) [1, Figure 4]. Ulcerative dermatitis tended to appear after about 10 weeks on the high-tryptophan diet [1, Figure 3].
Conclusion
I’ll follow up in my next post, on Monday, with speculation about what is happening in these mice.
In the meantime, I think it is worth remarking how an intervention thought to be beneficial – restoring serotonin levels to “normal” – has health-impairing consequences over time in both mice and people.
In many ways, contemporary medical practitioners resemble the Sorcerer’s Apprentice. They have at their disposal powerful magic drugs, whose long-term consequences they do not fully understand. The drugs come into wide use, and only years later do we learn that they do more harm than good. And the data showing they don’t work is always “surprising” and “paradoxical.”
In my view, the philosophy behind drug-based medicine is misplaced. Too often drugs are designed to fight or defeat the body’s natural mechanisms. As my parable argued, I believe it is much more effective to cooperate with the body through diet and nutrition.
References
[1] Dufour BD et al. Nutritional up-regulation of serotonin paradoxically induces compulsive behavior. Nutr Neurosci. 2010 Dec;13(6):256-64. http://pmid.us/21040623.
[2] Okusaga O et al. Association of seropositivity for influenza and coronaviruses with history of mood disorders and suicide attempts. J Affect Disord. 2010 Oct 26. [Epub ahead of print]. http://pmid.us/21030090. Hat tip Dr. Deans, http://evolutionarypsychiatry.blogspot.com/2010/11/depression-flu-and-to-do.html.












Recent Comments