We have friends in Japan, living both north and south of the damaged reactors, and Shou-Ching asked me to do a post about how to protect against radiation.
The Concern
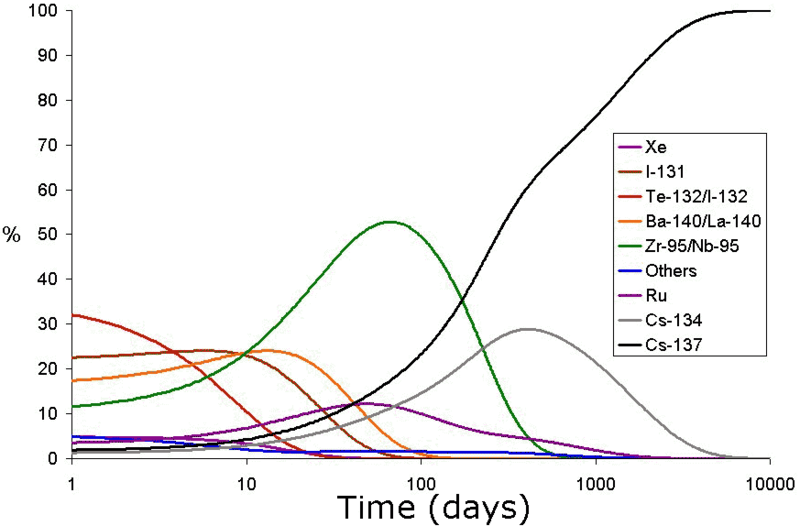
The radioactive substances released by the Chernobyl nuclear power plant meltdown are represented in this chart:
(Source. If you’re wondering what the other radioactive elements are, or why radioactive iodine is a byproduct of uranium fission, a possible place to start is Wikipedia, “Fission products by element” ).
Note first of all that the chart presents percentages of radioactive substances, not amounts. The amounts are highest on the first day and then decline rapidly. The great danger comes in the first few days.
During these dangerous first days, iodine-131 is, along with tellurium-132 and its decay product iodine-132, the dominant source of radioactivity. These radioactive iodine species account for over 50% of the radiation.
Not only its abundance, but also its effectiveness at causing biological damage make iodine far and away the greatest danger. Iodine radiation is highly effective at causing cellular damage:
Due to its mode of beta decay, iodine-131 is notable for causing mutation and death in cells which it penetrates, and other cells up to several millimeters away. [Source: Wikipedia, Iodine-131]
Worse, iodine is an important biological molecule that gets concentrated in the thyroid. So the dose of radiation becomes very high in the thyroid, and this leads to DNA damage producing a high risk for thyroid cancer.
Thyroid cancer is “the only unequivocal radiological effect of the Chernobyl accident on human health.” [1] Since Chernobyl released a great deal more radiation than the Japanese reactor meltdowns are likely to do, it’s likely that this will be the case in Japan also.
The rate of thyroid cancer after Chernobyl was higher the younger the age at time of exposure. Children and infants are at greatest risk:
It is now well documented that children and adolescents exposed to radioiodines from Chernobyl fallout have a sizeable dose-related increase in thyroid cancer, with the risk greatest in those youngest at exposure and with a suggestion that deficiency in stable iodine may increase the risk. [2]
The last point is crucial – iodine deficiency increases the risk.
Iodine deficiency and radiation risk
In iodine deficiency, the thyroid gland has difficulty generating enough thyroid hormone. T4 thyroid hormone, manufactured in the thyroid and so named because it has 4 iodine atoms, is 65.4% iodine by weight, so iodine is the key ingredient in thyroid hormone.
To compensate for an iodine deficiency, the body does two things:
- The thyroid gland grows, so that it can more aggressively scan the blood for iodine. An enlarged thyroid is called a goiter.
- The pituitary gland issues thyroid stimulating hormone (TSH), which induces the thyroid to aggressively scavenge iodine from the blood and turn it into thyroid hormone.
So in iodine deficiency the thyroid is aggressively scavenging all available iodine. This means that when a large dose of iodine-131 or iodine-132 arrives during radiation fallout, these radioactive iodine atoms are quickly picked up by the thyroid. There, they release their radiation and damage the thyroid.
On the other hand, in thyroid replete persons, the thyroid has all the iodine it needs and takes up little iodine from the blood. In this case, iodine that enters the body is distributed throughout the body, or excreted. Doses in any single cell are much lower. The danger to the thyroid is not much greater than that to other organs – which, the Chernobyl experience tells us, is not detectable to epidemiology. (There is even a theory that low-level radiation may be beneficial through hormesis.)
How can the thyroid be made replete with iodine?
The best way, which we recommend in our book, is to supplement with iodine and gradually build up the dose over a four to six month period. Start below 1 mg/day, take that for a month, then double the dose. After a month, double the dose again. Continue doubling until you reach your desired maintenance dose; we recommend at least 3 mg/day (a quarter Iodoral tablet), with 12.5 mg/day a reasonable dose. Some people taking as much as 50 mg/day.
At 12.5 mg/day, it can take a year or more to become replete with iodine in all tissues and to fully drive out other halogens, such as bromine, from the body. This has great benefits for immune function. So, it is best to get started!
Risks of high-dose iodine supplementation
If a person’s thyroid gland is adapted for iodine scarcity and the person takes a large dose of (non-radioactive) iodine, the likely course of events is:
1. Hyperthyroidism. The thyroid, aggressively scavenging for iodine to repair a deficiency of thyroid hormone, scoops up all the iodine and makes a large amount of thyroid hormone. The person develops symptoms of hyperthyroidism (too much thyroid hormone): anxiety, intolerance of heat, muscle aches, hyperactivity, irritability, hypoglycemia, elevated body temperature, palpitations, hair loss, difficulty sleeping.
2. Wolff-Chaikoff effect. As thyroid hormone levels become too high, the body induces mechanisms for suppressing thyroid hormone production. Simply reducing TSH output is not effective to suppress thyroid hormone production if a very large iodine influx is received. Fortunately there is another mechanism for suppressing thyroid hormone formation, mediated by iodine itself: the formation of iodine-rich proteins (iodopeptides) in the thyroid that inhibt synthesis of the thyroid peroxidase (TPO) enzyme. Normally, this mechanism operates for a few days and wears off, restoring normal thyroid function. [3]
3. Reactive hypothyroidism? Usually, everything will normally return to normal after a few days. But sometimes in previously iodine-deficient adults and more commonly in newborns and fetuses and some diseased persons, after very high doses of iodine the Wolff-Chaikoff effect can persist. In this case the early hyperthyroidism is followed by a period of hypothyroidism (too little thyroid hormone). This “hypothyroidism is transient and thyroid function returns to normal in 2 to 3 weeks after iodide withdrawal, but transient T4 replacement therapy may be required in some patients.” [3]
4. Risk for lasting hypothyroidism. People who develop a reactive hypothyroidism following a large dose of iodine are at high risk for later development of persistent hypothyroidism. [3]
So most people will experience transient hyperthyroid symptoms for a few days and then do fine. Some will develop a reactive hypothyroidism lasting a few weeks and then be OK, save for an elevated risk of hypothyroidism later which may or may not be due to the reactive episode.
Advice of the authorities to fallout victims
The advice from public health authorities is a compromise between the protective effects of high-dose iodine and the risk of messing up the thyroid.
A US Center for Disease Control (CDC) fact sheet explains the recommendations. A single large dose of iodine offers protection for about 24 hours. Recommended intakes are:
- Adults should take 130 mg/day while exposure persists.
- Children older than 3 and smaller than adults should take 65 mg/day while exposure persists.
- Infants and toddlers aged 1 month to 3 years should take 32 mg/day.
- Newborns should take 16 mg/day.
Our advice
The CDC dosage advice strikes us as very reasonable.
If you are not currently exposed to fallout, but think you may be exposed in the near future, you should consider beginning with small doses of iodine now – say, 3 mg/day. If that does not produce any symptoms, then try 6 mg/day; if it does, back off to half that dose. This will begin the adaptation process for your thyroid gland and help minimize hyperthyroid or hypothyroid reactions if you do have to take high doses.
Also, obtain your iodine tablets in advance. If fallout does occur, it may be hard to find iodine pills. NukePills.com says they are out of stock and have a large order backlog. I saw a story the other day that a 14-dose packet of potassium iodide was being sold at one site for $200, up from the normal $10 list price.
We recommend Iodoral 12.5 mg tablets. This is a good size for supplemental use; to reduce it to a 3 mg dose, cut the tablet in quarters with a razor blade. If fallout arrives, you can use ten Iodoral tablets to get a 125 mg adult dose.
For doses below 3 mg, smaller iodine tablets or liquid iodine solutions may be best; you can dilute liquid solutions to your desired dose. Some brands were recommended by readers in comments on our Supplement Recommendations page.
Conclusion
Outside of Japan, the risk is minimal, and even in Japan those who are replete with iodine are unlikely to develop thyroid cancer from exposure. After Chernobyl, thyroid cancer rates were high in Russia, the Ukraine, and Belarus which did not distribute iodine, but low in Poland which did. Fortunately, Japan has one of the highest iodine intakes in the world thanks to its high seaweed consumption. With that preparation plus proactive distribution of iodine tablets, we can expect and hope that the health effects of the reactor meltdowns will be minimal.
References
[1] Thomas GA et al. Integrating Research on Thyroid Cancer after Chernobyl-The Chernobyl Tissue Bank. Clin Oncol (R Coll Radiol). 2011 Feb 22. [Epub ahead of print] http://pmid.us/21345659.
[2] Cardis E, Hatch M. The Chernobyl Accident-An Epidemiological Perspective. Clin Oncol (R Coll Radiol). 2011 Mar 9. [Epub ahead of print] http://pmid.us/21396807.
[3] Markou K et al. Iodine-Induced hypothyroidism. Thyroid. 2001 May;11(5):501-10. http://pmid.us/11396709.













Recent Comments