The gut is the front line of health. The human gut houses 100 trillion bacteria from a thousand different species [1]; they weigh several pounds and make up about half the dry weight of stool. To control these bacteria 70% to 80% of the body’s immune cells are normally found in and around the gut.
A healthy gut is protected by a mucosal layer that is designed to promote commensal (friendly) bacteria, while providing a barrier to pathogenic bacteria. Humans have evolved ways to “feed” commensal species of bacteria. For instance:
- Human mucus is made of glycoproteins, or compounds made of protein and sugar. Certain probiotic bacteria, such as Bifidobacterium bifidum, are able to digest human mucus. [2] Thus, the human intestine has evolved to produce “food” for beneficial gut bacteria, assuring that they are maintained even during long fasts.
- Mother’s milk contains special sugars, called human milk oligosaccharides, which specifically feed Bifidobacterium bifidum and assure that this species successfully colonizes the baby’s intestine and wards off infection. [3]
The absence of this protective barrier of mucus and friendly bacteria makes the intestine extremely vulnerable to infectious disease. Premature babies who are fed formula, not human breast milk, often contract a dangerous intestinal infection, necrotizing enterocolitis. [3]
In addition to pathogenic bacteria, the gut is confronted by a heavy load of toxins. Bruce Ames and Lois Gold have estimated that the average person eats 5,000 to 10,000 different plant toxins, amassing to 1500 mg per day, plus 2000 mg of burnt toxins generated during cooking. [4]
Today’s post will focus on how those 1500 mg of natural plant toxins damage the intestinal wall and its mucosal barrier, thereby bringing about infectious bowel diseases.
Cereal Grain Toxicity
Grasses became the staple foods of agriculture because of their rich yields: a single plant may generate tens of thousands of seeds annually.
Yet this prolific seed production has always made grasses attractive to herbivores, and caused seeds to evolve high levels of toxins designed to poison mammalian digestive tracts, thus enabling their seeds to pass through herbivore guts undigested. It is these toxins that make the cereal grains so dangerous to human health.
The effectiveness of grain toxins at sabotaging human digestion is illustrated by the increase in fecal mass they produce:
For every gram of wheat bran eaten, fecal weight increases by 5.7 grams. [5]
By inhibiting human digestion, wheat toxins dramatically increase the amount of undigested starch reaching the colon. This increased food supply substantially increases the bacterial population – and the presence of starch, which is ordinarily unavailable in the colon, favors the growth of pathogenic species.
Unfortunately wheat toxins do much more than inhibit digestion of food. They also damage the gut itself.
Wheat contains an ingenious cocktail of toxins:
- Gluten, a complex of proteins, inspires on immune response which inflames the intestine in at least 83% of people [6], and makes the intestine permeable, allowing gut bacteria and their toxins to enter the body. [7] Gluten triggers anti-wheat antibodies in at least 30% of the population, and auto-antibodies – that is, antibodies that attack human cells – in at least 0.4% of the population. [8] These unlucky folks suffer celiac disease, which devastates the intestine, as well as autoimmune thyroiditis. [9]
- Opioid peptides produce effects similar to morphine and heroin. Wheat opioids have been implicated as causes of schizophrenia. [10]
- Wheat germ agglutinin is a lectin, or protein that binds sugars. At extremely low doses, a few parts per billion, WGA causes gut inflammation and leakiness. At typical dietary doses, WGA causes shedding of the intestinal brush border and shrinkage in the surface area of the intestine. [11] WGA alone can induce celiac disease in rats. [12]
By unknown mechanisms, grains can induce vitamin deficiency diseases. Wheat and oats induce rickets [13] while corn induces pellagra. [14]
Since as little as 1 milligram of gluten per day can prevent recovery from bowel disease [15], it is essential that grains be eliminated entirely from the diet.
Legume Toxicity
Legumes also contain an array of toxins which suspend digestion and damage the gut. Some examples:
- Phytohaemagglutinin, a kidney bean lectin, makes the gut leaky; blocks stomach acid production, promoting bacterial overgrowth of the small intestine; overpopulates the gut with immature cells that are easily colonized by E. coli and other pathogens; disturbs the mucus and shortens villi. [16]
- Alpha-amylase inhibitors in legumes prevent starch digestion and leads to gut bloating and multiplication of pathogenic gut bacteria. [17]
- Antibodies to soy proteins have been identified in duodenitis, Crohn’s disease, ulcerative colitis, and coeliac disease, and these diseases are sometimes cured when soy is removed from the diet. [18]
It should be noted that peanut and soybean allergies are among the most common allergies. This testifies to the significant immune response legume toxins can generate.
Omega-6 Toxicity
Most people are familiar with the evidence linking the omega-6 to omega-3 ratio to cardiovascular disease. Most Americans have an omega-6 to omega-3 ratio in tissue that is ten-fold too high; cultures with a better omega-6 to omega-3 ratio, such as Greenland Inuit and Japanese, have much lower rates of heart disease.
Since the effect of an excessive omega-6 to omega-3 is to greatly increase inflammation while impairing immune function, it’s logical that an elevated ratio would worsen inflammatory bowel disease.
And it does. The EPIC (European Prospective Investigation into Cancer and Nutrition) study took food diaries from 203,193 people and followed them for four years [19]:
- Being in the upper quartile of intake of omega-6 fatty acids raised the risk of ulcerative colitis by 149%.
- Being in the upper quartile of intake of the omega-3 DHA, which is abundant in salmon and sardines, reduced the risk of ulcerative colitis by 36% – 77% after adjustment for omega-6 intake. (Apparently those who ate more omega-3s also ate more omega-6s.)
Another study found that being in the upper third of DHA intake reduced the risk of ulcerative colitis by about 50%. [20]
The upshot: anyone with inflammatory bowel diseases should strictly limit omega-6 consumption and strive to eat a pound per week of salmon or sardines.
Fructose Toxicity
Fructose is a sugar that is toxic and useless to humans – but it is a rich source of energy to bacteria. Fructose consumption strongly promotes bacterial growth in the intestine and increases levels of bacterial endotoxins in the body. [21]
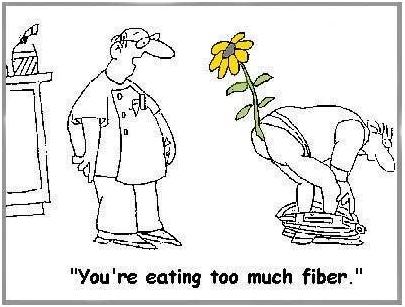
Of Fiber
Most people think that fiber is indigestible, and that it comes out in their stool. This is not true. Fiber is indigestible to humans, but not to bacteria. Fiber is bacterial food that enables gut bacteria to multiply. Bacteria, not undigested food, make up most of the dry weight of stool. [22]
Doctors often recommend fiber to bowel disease patients. While not wholly without merit, this advice usually backfires.
There are three problems: helping bacteria feed and multiply may be undesirable; fiber, such as the brans of cereal grains, often contains toxic proteins; and, finally, whole grain fibers and other “roughage” scrape and injure the intestinal wall. Dr. Paul L. McNeil explains that:
When you eat high-fiber foods, they bang up against the cells lining the gastrointestinal tract, rupturing their outer covering. [23]
That can’t be a good thing.
And it isn’t. In the Diet and Reinfarction Trial (DART), published in 1989, 2,033 British men were divided into a high-fiber group and a control group. The high-fiber group ate whole grains and doubled their grain fiber intake from 9 to 17 grams per day. The result? Deaths in the high fiber group were 22% higher over the course of the study – 9.9% of the control group died versus 12.1% of the high-fiber group. [24]
Softer soluble fibers from fruits and some vegetables are much more likely to help than wheat bran, but even they may be a good thing only in moderation, or only in a healthy bowel. Fiber feeds pathogenic bacteria as well as probiotic bacteria, and increases the populations of both. When the gut is damaged and leaky, more bacteria mean more bacterial toxins and more pathogens infiltrating the body. A low-fiber diet, leading to reduced bacterial populations in the gut, may be desirable for bowel disease patients.
Yes, it is possible to get too much fiber!
(via Peter at Hyperlipid)
Other Toxic Foods
Nightshade plants and seeds of all species can also contain toxins and may also need to be restricted in people with damaged intestines.
Dairy proteins, especially pasteurized cow casein, are also often problematic for people with damaged intestines.
In general, any foods that commonly produce allergies are likely to give trouble to people with damaged intestines.
All plant proteins are risky, as are dairy and egg proteins. It is possible to minimize risk by:
- Eating clarified butter, but refraining from protein-rich dairy foods.
- Eating cooked egg yolks, but avoiding the protein-rich egg whites.
Summary of Toxic Foods to Eliminate or Avoid
In short, bowel disease patients should eliminate toxic foods from their diet:
- Eliminate all grains except rice. Wheat, oats, and corn, and their products such as wheat flour, cornstarch, bread, and pasta, must be eliminated.
- Eliminate all legumes, especially soy, beans, and peanuts.
- Eliminate omega-6 rich oils, such as soybean oil, safflower oil, corn oil, peanut oil, and canola oil.
- Eliminate fructose sugars, except from fruits and berries. Drink no sugar-containing beverages.
- Minimize fiber to keep down gut bacterial populations and avoid mechanical injuries to the intestinal wall.
- Minimize other potentially toxic protein sources. In general, protein should be obtained from animal and fish meats, not eggs, dairy, or plants. However, fats from dairy and eggs are highly desirable.
When gut health is restored, dairy and fiber may be restored to the diet. However, the major toxic foods – grains, legumes, omega-6-rich oils, and most fructose – should be eliminated for life.
Filling the Gaps in the Diet
For most people, eliminating grains will leave a large gap in the diet. Foods that should be used to fill that gap include:
- Healthful plant foods are the safe starches, such as white rice, taro, sweet potatoes and yams, and fruits and berries.
- Saturated-fat rich oils and fats, like beef tallow, clarified butter, coconut oil, palm oil, cocoa butter (yes, chocolate desserts are healthy!), along with modest quantities of olive oil and lard. Make homemade salad dressings with these oils, rather than buying supermarket dressings made with soybean or canola oil.
- Further balance the omega-6 to omega-3 ratio by eating low-omega-6 meats, such as the red meats (beef and lamb) and seafood, and eating 1 lb per week salmon or sardines for fresh omega-3 fats.
When the small intestine is damaged, fatty foods may be difficult to tolerate, since the enzymes that digest dietary fats and proteins may also digest human cells. In such cases the diet must focus on starchy foods like rice until bowel health is restored. Be sure to supplement with vitamins and minerals in such cases.
Conclusion
Eliminating food toxins may cure bowel diseases and always improves prognosis. Pedro Bastos of The Paleo Diet Update writes:
From the feedback we have received over the years, IBS patients respond dramatically and rapidly to the Paleo Diet. Their experience indicates that milk, grains and legumes seem to be the main culprits in this condition via a number of mechanisms. [The Paleo Diet Update v.4, #18]
Auto-antibodies generated by wheat against the thyroid, pancreas, and gut typically disappear within 3 to 6 months after removal of wheat from the diet. [25, 26] This is probably a reasonable estimate for the time frame in which bowel disease patients can expect significant improvements from the elimination of dietary food toxins.
Related Posts
Other posts in this series:
- Bowel Disorders, Part I: About Gut Disease July 14, 2010
- Bowel Disease, Part III: Healing Through Nutrition July 22, 2010
- Bowel Disease, Part IV: Restoring Healthful Gut Flora July 27, 2010
References
[1] Fujimura KE et al. Role of the gut microbiota in defining human health. Expert Rev Anti Infect Ther. 2010 Apr;8(4):435-54. http://pmid.us/20377338.
[2] Ruas-Madiedo P et al. Mucin degradation by Bifidobacterium strains isolated from the human intestinal microbiota. Appl Environ Microbiol. 2008 Mar;74(6):1936-40. http://pmid.us/18223105.
[3] Bode L. Human milk oligosaccharides: prebiotics and beyond. Nutr Rev. 2009 Nov;67 Suppl 2:S183-91. http://pmid.us/19906222. Hat tip Dr. Art Ayers.
[4] Ames BN, Gold LS. Paracelsus to parascience: the environmental cancer distraction. Mutation Research 2000 Jan 17; 447(1):3-13. http://pmid.us/10686303
[5] Cummings JH. The effect of dietary fibre on fecal weight and composition. Pp 547–73 in: Spiller GA, ed. Handbook of dietary fibre in human nutrition. 2nd ed. Boca Raton, FL: CRC Press, 1993.
[6] Bernardo D et al. Is gliadin really safe for non-coeliac individuals? Production of interleukin 15 in biopsy culture from non-coeliac individuals challenged with gliadin peptides. Gut 2007 Jun;56(6):889-90. http://pmid.us/17519496.
[7] Drago S et al. Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scand J Gastroenterol. 2006 Apr;41(4):408-19. http://pmid.us/16635908.
[8] Not T et al. Celiac disease risk in the USA: high prevalence of antiendomysium antibodies in healthy blood donors. Scand J Gastroenterol. 1998 May;33(5):494-8. http://pmid.us/9648988.
[9] Sollid LM, Jabri B. Is celiac disease an autoimmune disorder? Curr Opin Immunol. 2005 Dec;17(6):595-600. http://pmid.us/16214317.
[10] Singh MM et al Wheat gluten as a pathogenic factor in schizophrenia. Science. 1976 Jan 30;191(4225):401-2. http://pmid.us/1246624. Dohan FC et al 1984 Is schizophrenia rare if grain is rare? Biol Psychiatry. 1984 Mar;19(3):385-99. http://pmid.us/6609726.
[11] Lorenzsonn V, Olsen WA. In vivo responses of rat intestinal epithelium to intraluminal dietary lectins. Gastroenterology. 1982 May;82(5 Pt 1):838-48. http://pmid.us/6895878.
[12] Sjölander A et al. Morphological changes of rat small intestine after short-time exposure to concanavalin A or wheat germ agglutinin. Cell Struct Funct. 1986 Sep;11(3):285-93. http://pmid.us/3768964.
[13] Mellanby E. (March 15 1919) An experimental investigation on rickets. The Lancet 193(4985):407-412.
[14] Carpenter KJ, Lewin WJ. A critical review: A reexamination of the composition of diets associated with pellagra. J Nutr 1985 May;115(5):543–552. http://pmid.us/3998856.
[15] Biagi F et al. A milligram of gluten a day keeps the mucosal recovery away: a case report. Nutr Rev. 2004 Sep;62(9):360-3. http://pmid.us/15497770.
[16] Kordás K et al. Phytohaemagglutinin inhibits gastric acid but not pepsin secretion in conscious rats. J Physiol Paris. 2001 Jan-Dec;95(1-6):309-14. http://pmid.us/11595455. Pusztai A et al. Kidney bean lectin-induced Escherichia coli overgrowth in the small intestine is blocked by GNA, a mannose-specific lectin. J Appl Bacteriol. 1993 Oct;75(4):360-8. http://pmid.us/8226393. Prykhod’ko O et al. Precocious gut maturation and immune cell expansion by single dose feeding the lectin phytohaemagglutinin to suckling rats. Br J Nutr. 2009 Mar;101(5):735-42. http://pmid.us/18644165.
[17] Pusztai A et al. Inhibition of starch digestion by alpha-amylase inhibitor reduces the efficiency of utilization of dietary proteins and lipids and retards the growth of rats. J Nutr. 1995 Jun;125(6):1554-62. http://pmid.us/7782910.
[18] Haeney MR et al. Soya protein antibodies in man: their occurrence and possible relevance in coeliac disease. J Clin Pathol. 1982 Mar; 35(3):319-22. http://pmid.us/7040491.
[19] IBD in EPIC Study Investigators. Linoleic acid, a dietary n-6 polyunsaturated fatty acid, and the aetiology of ulcerative colitis: a nested case-control study within a European prospective cohort study. Gut. 2009 Dec;58(12):1606-11. http://pmid.us/19628674.
[20] John S et al. Dietary n-3 polyunsaturated fatty acids and the aetiology of ulcerative colitis: a UK prospective cohort study. Eur J Gastroenterol Hepatol. 2010 May;22(5):602-6. http://pmid.us/20216220.
[21] Bergheim I et al. Antibiotics protect against fructose-induced hepatic lipid accumulation in mice: role of endotoxin. J Hepatol. 2008 Jun; 48(6): 983-92. http://pmid.us/18395289.
[22] Stephen AM et al. Effect of changing transit time on colonic microbial metabolism in man. Gut. 1987 May;28(5):601-9. http://pmid.us/3596341.
[23] Quoted in Science Daily, http://www.sciencedaily.com/releases/2006/08/060823093156.htm. Hat tip Dr. Michael Eades.
[24] Burr ML et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989 Sep 30;2(8666):757-61. http://pmid.us/2571009. Hat tip Stephan Guyenet.
[25] Berti I et al. Usefulness of screening program for celiac disease in autoimmune thyroiditis. Dig Dis Sci. 2000 Feb;45(2):403-6. http://pmid.us/10711459.
[26] Mainardi E et al. Thyroid-related autoantibodies and celiac disease: a role for a gluten-free diet? J Clin Gastroenterol. 2002 Sep;35(3):245-8. http://pmid.us/12192201.











Recent Comments