I’m going to deviate from my original plan for the “Dangers of a Zero-Carb Diet” series to discuss a topic that came up in the comments to the first post.
Leonie’s Diabetes and the Rose Corn Oil Trial
What prompted this diversion is Leonie’s interesting comment from Wednesday’s post:
I developed diabetes several years after being on a low carb diet. Continuing low carb to manage the diabetes did not halt its progress. It has taken about 18 months of adding more carbs (60 – 100 gr/day) to my diet to bring my fasting glucose down by a couple of mmol and eating more carbs has also lowered my Hba1c and post meal spikes significantly. I wonder if the liver is another organ that may be affected by carbohydrate deficiency.
I had not heard of such cases before, or so I thought, but Dr. Deans in the comments reminded us that Peter at Hyperlipid had noticed two similar cases in the Rose Corn Oil trial. [1] (The Rose Corn Oil trial, of course, figures prominently in our book’s discussion of PUFA toxicity.)
In the Rose Corn Oil trial, there were three arms – a normal diet arm, a high corn oil arm, and a high olive oil arm. The normal dieters were expected to eat “fried foods, fatty meat, sausages, … ice cream, cheese, … milk, eggs, and butter” while the oil arms were supposed to restrict these foods and replace them with corn or olive oil.
Here’s what happened:
Four patients were removed from the trial for other reasons. Two developed non-cardiac thromboembolism and were given anticoagulant therapy. The other two were removed because of diabetes mellitus. One of them already had mild diabetes, but glycosuria increased considerably soon after he started oil. Oil was stopped and glycosuria disappeared. Oil was restarted, but was stopped a month later because heavy glycosuria recurred. The other patient, not a previously recognized diabetic, developed glycosuria with a diabetic glucose-tolerance test a few weeks after starting oil. [1]
The patients who developed diabetes came one from the corn oil arm and one from the olive oil arm. Likewise, the patients who developed thromboembolisms came one from the corn oil arm and one from the olive oil arm. No such disasters occurred on the “fatty meat” arm.
Since all three diets were similarly fatty, it doesn’t appear to be the quantity of fat that was the issue. Rather it was the type of lipid, or some micronutrient that was present in the animal and dairy foods but lacking in the plant oils.
For insight into what the problem might be, let’s look at how scientists poison lab animals.
Insights from Diet Animal Poisoning Research
You have to pity diet researchers. It takes 60 years for bad diets to poison humans enough to significantly raise mortality rates. Yet a diet researcher is supposed to gain a Ph.D. in 4 years (or in 5 while simultaneously obtaining an MD!), do a postdoc in 2 years, win a grant in the first years of an entry-level position with PI status, and then demonstrate productive results within the term of a 2-to-5 year grant. Deadlines are pressing: A study needs to start rats or mice on two diets, and have one diet produce much better health than the other, in considerably less than a two-year time frame.
Just comparing McDonald’s fast food with a Mediterranean diet won’t do. Two years later both sets of mice will die happily of old age, with no significant differences between groups. Peer reviewers judge you to have discovered no new results. No new results means no paper, no grant, no job.
So “diet” researchers first have to become experts at quickly inducing disease in rats and mice. Find a diet that poisons animals in a few months, compare it to another diet that doesn’t, and you have a paper. Look for variations that slow or hasten the poisoning, and you have more papers. To be a highly productive scientist, one must be a skilled animal poisoner.
Various techniques have been developed for this purpose, including: knocking out some crucial gene; breeding a mutant strain that naturally develops disease; giving the animals poison with their food; or depriving them of crucial nutrients. Almost every study of diet in mice or rats uses one of these techniques.
If a missing nutrient can cause diabetes within a few years for Leonie and 12 to 18 months for the Rose Corn Oil trial volunteers, it’s likely to be pretty good at inducing disease in animals too. There’s a good chance diet animal poisoning researchers have already stumbled upon it in rats or mice.
Choline Deficiency Diseases
One of the most popular deficiency diets among researchers is the choline-deficient diet. A useful paper by Dutch scientists [2] gives a nice look at the impact of choline deficiency on rats.
Choline deficiency (CD) by itself induces metabolic syndrome (indicated by insulin resistance and elevated serum triglycerides and cholesterol) and obesity.
A combined methionine and choline deficiency (MCD) actually causes weight loss and reduces serum triglycerides and cholesterol, but induces more severe liver damage. The MCD diet prevents the body from manufacturing choline from methionine, vitamin B12, and folate, so MCD diets severely reduce choline levels; and without choline VLDL particles are not produced. Without VLDL particles, fats and cholesterol are trapped in the liver and never reach the blood and adipose cells.
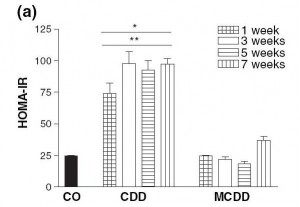
Here is a measure of insulin resistance on the two diets:
The induction of insulin resistance by the CD diet is very rapid, requiring less than a week.
Induction of insulin resistance is thought to be mediated by elevated TNF-alpha production by adipose cells and by hypertriglyceridemia. Since the MCD diet neither raised serum triglycerides nor caused obesity which induces TNF-alpha production in adipose cells, it did not cause insulin resistance.
What Does This Have to Do With Diabetes?
Insulin resistance is a key step in the development of diabetes:
- Insulin resistance in the liver causes the liver to release more glucose into the blood (since insulin inhibits glucose release by the liver). This is discussed in a nice paper [3] found by LynMarie Daye and cited in the comments by CarbSane.
- Peripheral insulin resistance means that the rest of the body is less sensitive to insulin. The pancreas has to produce more insulin to dispose of the excess glucose that the liver is releasing.
This elevation of insulin and glucose levels is a crucial step toward diabetes; it is “pre-diabetes.”
Persistently elevated glucose levels can then poison the beta cells of the pancreas, diminishing insulin secretion capability and causing diabetes. [4]
The Rose Corn Oil trial was not a low-carb diet, so postprandial glucose levels could easily have risen to toxic levels.
If a CD diet can cause insulin resistance in a week, it’s plausible that it might cause diabetes in 12 to 18 months, which is when the Rose Corn Oil trial patients developed it.
What About the Thromboembolism Cases?
MCD diets induce fibrinogenesis. In the blood, excess fibrin formation leads to clotting, and clots can block vessels to cause thromboembolisms. It may be that the thromboembolism cases in the Rose Corn Oil trial had methionine, folate, or B12 deficiencies to go with their choline deficiency.
Why Do Plant Oils Induce Diabetes But Not Animal Fats?
So why did diabetes develop in the corn and olive oil arms of the Rose Corn Oil trial but not the “fatty meat and dairy” arm?
Well, look at the choline content of these foods:
Choline content of one cup (~200 g) oil or fat or 227 g (1/2 lb) meat
| Beef liver | 968.0 mg |
| Cube steak (beef) | 290.0 mg |
| Beef tallow | 164.0 mg |
| Butter | 42.7 mg |
| Olive oil | 0.6 mg |
| Corn oil | 0.4 mg |
Source: http://nutritiondata.com.
Take away meat and dairy and replace them with plant oils, and it’s very easy to have a choline deficiency.
What Does This Have to Do With Zero-Carb Diets?
Maybe nothing … without carb consumption, postprandial glucose levels are not as high, and beta cell poisoning is less likely … but it may be that a zero-carb diet aggravates a choline deficiency in some fashion. I will leave this as a topic for further research.
UPDATE: Leonie in a new comment gives us more information: she has PCOS, goiter with nodules, and auto-antibodies. This suggests autoimmunity as a more likely explanation for her zero-carb diabetes.
Conclusion
In the book, we recommend the use of animal fats such as beef tallow for cooking, and recommend that pregnant women and vegetarians supplement with choline. We thought seriously about recommending that everyone supplement choline, but were reluctant to recommend too many supplements.
In retrospect, we should have recommended choline supplements for everyone who is overweight, has elevated blood glucose or lipids, or has elevated liver enzymes.
We have been using beef tallow as our cooking oil for several months now. It might be good practice for everyone to favor animal fats like beef tallow over plant oils for cooking.
References
[1] Rose GA et al. Corn oil in the treatment of ischaemic heart disease. Br Med J. 1965 Jun 12;1(5449):1531-3. http://pmid.us/14288105.
[2] Veteläinen R et al. Essential pathogenic and metabolic differences in steatosis induced by choline or methione-choline deficient diets in a rat model. J Gastroenterol Hepatol. 2007 Sep;22(9):1526-33. http://pmid.us/17716355.
[3] Sonksen P, Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth. 2000 Jul;85(1):69-79. http://pmid.us/10927996.
[4] Leibowitz G et al. Glucose regulation of ?-cell stress in type 2 diabetes. Diabetes Obes Metab. 2010 Oct;12 Suppl 2:66-75. http://pmid.us/21029302.











A quick chemistry lesson
Your digestive tract is full of bacteria. Some of them feed on choline and carnitine, nutrients in red meat, egg yolks and high-fat dairy products. As they feed, they give off a chemical called TMA (trimethylamine). Your liver turns TMA into TMAO (trimethylamine-N-oxide).
TMAO in your blood affects the inner wall of your blood vessels, causing cholesterol buildup. If you have chronically high TMAO, you have double the risk of heart attack, stroke and death. Studies show that levels of TMAO in your blood can help predict your risk of heart disease.
A natural treatment
So, if TMAO is harmful, how do we get rid of it? One way is to stop gut bacteria from making TMA in the first place.
The new study by Dr. Hazen and his team found that a natural substance called DMB (3,3-dimethyl-1-butanol) could do this in mice. The result was lower TMAO levels and fewer clogged arteries.
“We were able to show that drugging the microbiome is an effective way to block diet-induced heart disease,” says Dr. Hazen. “It’s much like how we use statins to stop cholesterol from forming in a body’s cells.”
DMB is found in some olive and grapeseed oils. Because it’s not an antibiotic, DMB doesn’t kill “good bacteria.” And, unlike antibiotics, there’s little risk of overusing it or building resistance to it.
What this means for you
There’s a long way to go before treatments are fully tested and approved for humans.
“My hope is that, down the road, this type of approach to lowering TMAO can be used to augment other approaches for reducing risk of cardiovascular events,” says Dr. Hazen.
In the meantime, should you stop eating meat and other animal products? Dr. Hazen says moderation is key.
“Omnivores usually do have higher levels of TMAO than vegetarians and vegans, but not always,” he says. “TMAO level is determined more by your gut microbes than your diet. Other factors also play a role, such as the microbes you’re exposed to and other aspects of your health, like kidney function and genetics.”
A test to measure TMAO levels is now available at Cleveland HeartLab.
December 31, 2015 / By Heart and Vascular Team
Red Meat Linked to Kidney Failure -Red meat increases your risk for kidney failure, according to a study published online in the Journal of the American Society of Nephrology. Researchers assessed data from 63,257 participants as part of the Singapore Chinese Health Study and tracked diet and kidney failure. Those who consumed the most protein from red meat increased their risk for end-stage kidney disease. Results showed that replacing a single serving of red meat with another source of protein, such as soy products or legumes, cut the risk for disease by over 60 percent. These findings support previous research that suggests diets high in processed meats increase risk for disease and mortality.
Lew QLJ, Jafar TH, Koh HWL, et al. Red meat intake and risk of ESRD. J Am Soc Nephrol. Published online July 14, 2016.
I was diagnoised pre-diabetic in my 20’s. I eventually corrected it (or so I thought) my adopting low carb eating.
Fast forward a decade or so and I was shocked to discover that my fasting blood glucose as back in the pre-diabetic range.
After much searching I came up with my own theory: Peripheral Insulin Resistance. Essentially I was depriving my body of carbs (roughly 50 grams per day at the most). My body recognized this and eventually caused my periphery to become ‘resistant’ to insulin.
Why? Because it wants to shunt any available glucose in the body to the brain because glucose is it’s preferred fuel source.
Fast forward to today. Still not eating as many carbs as I would like but I have been increasing them steadily and feeling better.
Fasting sugars and A1C are now back in ‘normal’ limits.