Last year we ran a series on “Zero-Carb Dangers,” which are health problems that can appear if carb intake – or carb+protein intake, since protein can to some degree make up for a deficit of glucose – are too low. Anthony Colpo has recently argued that hypothyroidism should be added to the list of potential zero-carb dangers; and that low-carb high-fat diets in general might create a risk of hypothyroidism. Similar arguments have been made by Matt Stone and others. Our resident thyroid expert, Mario Renato Iwakura, decided to look more deeply into the matter. What does the literature say? Here’s Mario.
There have been anedoctal reports on low carb forums about people becoming hypothyroid after following a low carb, high fat diet. Anthony Colpo recently wrote a blog post about carbohydrate, fat and protein intake and their effects on thyroid hormone levels, concluding that a high fat or high protein diet is detrimental and that a high carbohydrate diet is good for the thyroid [1].
What I will try do demonstrate here is that the sole conclusion we can draw from the literature, including the studies cited by Anthony and others, is that a high polyunsaturated fat (PUFA) diet is detrimental to thyroid health. There is no evidence that a diet, such as the Perfect Health Diet, that is high in saturated and monounsaturated fat, low in PUFA, and provides sufficient, moderate levels of protein and carbohydrate, has any detrimental effect on the thyroid. On the contrary, I believe that such a diet is optimal for thyroid health.
What Has Been Tested: High PUFA Diets
Colpo’s post is extensive and covered most, but not all, relevant studies published to date about the subject. Many of those studies have problems like short duration or calorie restriction. But in almost all, with the exception of one study by Jeff Volek and collaborators [2], the fat used in the high fat diet was predominantly polyunsaturated fat from vegetable oils. An example is the Vermont long term study [3]:
“The long-term study of fat overfeeding included four subjects studied before and after overeating fat for 3 mo. The excess fat in these diets averaged 895 kcal/d consisting of margarine, corn oil, a corn oil colloidal suspension, and fat enriched soups and cookies. The ratio of saturated to unsaturated fatty acids in these diets was ~1:2.5.”
This ratio is precisely that found in corn oil. So, this diet’s fat was probably 13.5% saturated, 29% monounsaturated, and 57.5% polyunsatured.
Or in Ullrich et al 1985 [4]:
“One diet was high in polyunsaturated fat (HF), with 10%, 55%, and 35% of total calories derived from protein, fat, and carbohydrate, respectively.”
Polyunsaturated Fat and the Thyroid.
Let’s look at the literature, starting with two studies not cited by Anthony.
In 1995, Vasquez et al tested four very low calorie diets, with variable amounts of carbs, fats and protein, in 48 obese women for 28 days [5]. All diets were in liquid form, and fat was predominantly PUFA. The composition of the four diets was:
| 50P/10C | 50P/76C | 70P/10C | 70P/86C | |
| Energy (kcal) | 590 | 590 | 615 | 615 |
| Protein (% cal) | 35.5 | 33.7 | 45.8 | 43.0 |
| Fat (% cal) | 57.8 | 15.1 | 48.1 | 4.1 |
| Carb (% cal) | 6.7 | 51.2 | 6.1 | 52.9 |
| T3 Day 0 | 2.0 | 2.2 | 1.6 | 1.8 |
| T3 Day 28 | 1.1 | 1.7 | 1.0 | 1.4 |
| Variation | -45% | -23% | -37% | -22% |
T3 thyroid hormone levels decreased on all of these severely calorie restricted diets. However, when PUFA was high (50P/10C and 70P/10C) the decrease in T3 was much larger than when PUFA was low (50P/76C and 70P/86C).
In a 1992 paper, Vasquez et al compared two very low calorie diets (600kcal/day), one ketogenic and the other nonketogenic [6]. The fat sources were soybean oil and refined and stabilized vegetable oils.
| Ketogenic | Nonketogenic | |
| Protein | 35% | 34% |
| Fat | 58% | 15% |
| Carbs | 9% | 51% |
| T3 Day 0 | 1.4 | 1.5 |
| T3 Day 28 | 0.8 | 1.3 |
| Variation | -43% | -13% |
The various studies cited by Colpo also show decreases in T3 levels in diets high in PUFA. In Ullrich et al 1985 [4], a study of healthy young adults, although TSH, T4, and rT3 did not change significantly, T3 levels on a high polyunsaturated diet decreased more than on a high protein diet:
“The triiodothyronine (T3) declined more (P less than .05) following the HF diet than the HP diet (baseline 198 micrograms/dl, HP 138, HF 113). Thyroxine (T4) and reverse T3 (rT3) did not change significantly. Thyroid-stimulating hormone (TSH) declined equally after both diets”
In the Vermont study [3], where the low carb diet was high in PUFA fat, that was the case too:
“During maintenance eating, levels of T3 (triiodothyronine) were higher on the high-carb diet. When subjects on the low-carb diet began eating the higher-carb mixed weight gain diet, their T3 levels rose. T3 levels among those who went from the high-carb maintenance diet to the mixed diet remained unchanged. In contrast to T3, serum concentrations of T4 were unchanged by overeating or changes in dietary composition.” [1]
Low-PUFA High-Fat Diets and the Thyroid: Lack of Direct Evidence
Unfortunately we don’t have human studies comparing diets high in saturated fat and polyunsaturated fat and their effect on thyroid hormones synthesis. Neither do we have studies showing what happen to T3 levels after a high saturated/monosaturated fat diet is eaten. We will have to rely on indirect evidence.
Indirect Evidence: Calories Required to Maintain Weight.
There is a connection between thyroid activity and obesity. Reduced thyroid activity reduces energy expenditure (“calories out”) and promotes weight gain; normal thyroid function tends to promote normal weight. So we can use the vast number of obesity studies as indirect evidence for the effects of different types of diet on the thyroid.
Anthony emphasized this relationship in his post, noting findings of the Vermont study on overfeeding:
“Again, that both groups gained weight should come as no surprise. However, the group overfed the mixed diet required more calories (2,625 kcal/m2 per day) to maintain their new heavier weights than did the group overfed fat (1,840 kcal/m2 per day). Baseline differences in metabolism between the two groups were ruled out, as there was no difference in total calories required to maintain initial lean weights.”
So the high-PUFA diet promoted weight gain: it caused excess weight to be retained at a lower calorie intake. This is consistent with reduced thyroid activity.
Is this effect due to a high-fat diet generally, or to high-PUFA diets only? Some insight into this question may be found in a blog post by Stephan Guyenet [7]. Rats fed isocaloric diets in which the fat source was varied among three groups – a beef tallow group (primarily saturated fat, 3% PUFA), an olive oil group (primarily unsaturated, 10-15% PUFA), and a safflower oil group (78% PUFA) – had highly variable weight gains. The olive oil group gained 7.5% more weight than the beef tallow group, and the safflower oil group 12.3% more weight. This is exactly the same pattern found in the Vermont overfeeding study in man: reduced energy expenditure as the consumption of PUFA increases.
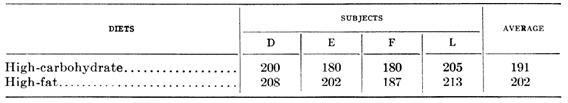
Since 1945, it has been known that men fed a high carbohydrate and then a high saturated fat diet needed about the same amount of calories to mantain their weight in cold temperature [18]. Here is the data, expressed in terms of the percentage of baseline calorie intake that the men had to eat to maintain their weight:
The high-fat diet consisted largely of butter and cream; the high-carbohydrate diet of extra sugar. When eating the butter and cream, subjects had to eat more calories to maintain weight than when eating the sugary diet – 202% of baseline calorie intake vs 191%. Every subject had to increase calories when eating high-fat. This suggests higher thyroid hormone levels on the high-saturated fat diet than on a high-carb diet.
The Volek Study
Anthony cited a study by Jeff Volek and others [2] on body composition and hormonal responses to a carbohydrate-restricted diet and said that:
Upon commencement of the low-carbohydrate diet a small calorie deficit and a significant increase in protein intake occurred, resulting in a mean 3.3 kilogram fat loss and a 1.1 kilogram lean mass gain. There was a significant increase in total T4 (+10.8%), but for some reason the researchers did not directly measure T3 nor rT3. They instead tested T3 uptake, an indirect measure of thyroxine binding globulin (TBG) in the blood, which tells us little of any real value about changes in actual thyroid hormone levels. The researchers also measured IGF-1, glucagon, total and free testosterone, sex hormone-binding globulin (SHBG), insulin-like growth factor-I (IGF-I), and cortisol. The only significant change noted was a reduction in insulin following the low-carbohydrate diet.
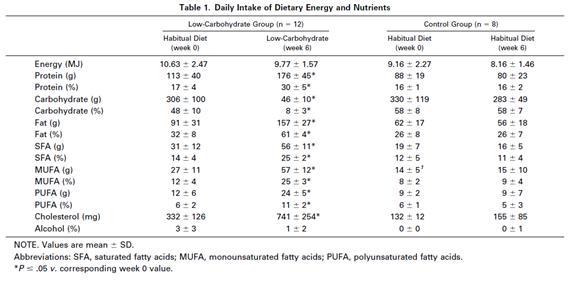
The Volek study is very interesting because it was not calorie restricted (only carbohydrate was restricted) and was done in normal-weight man. The amount of polyunsaturated fat increased a little (from 6 to 11% of calories), but was still low; saturated and monosaturated fats were the main fats of the low carb-high fat diet. Although he did not directly measured T3 nor rT3 we have indirect evidence that they were not impaired.
One very well known fact is that hypothyroid patients, even when taking T4 hormones, usually struggle to lose fat. This occurs because, when thyroid hormones are low, especially when T3 (triidothyronine) is low [8], the basal metabolism is decreased. If the LCHF diet was impairing the thyroid these healthy normal weight men, who had been advised to eat enough calories to maintain their weight during the intervention, should have struggled to lose fat mass. In fact they lost 3.3 kg (7.3 pounds) in 6 weeks on an 8% reduction in calorie intake. The control group did not lose any weight despite an 11% reduction in calorie intake.
More, testosterone levels usually decrease when thyroid hormones are low [9][10]. IGF-1 levels are also decreased in hypothyroidism [11][12]. Glucagon levels are higher in hypothyroid patients [13]. Sex hormone-binding globulin (SHBG) is low in hypothyroidism [14][15][16]. But none of these parameters changed during the LCHF diet.
So this diet which was low in carb (8% of calories) and moderately high in protein (30%) and PUFA (11%) does not seems to affect the thyroid if saturated and monosaturated fat (50% of calories) are the main fat of the diet. Let’s compare the fatty acid profile of the Volek diet with that of human milk:
| Saturated | Monounsaturated | Polyunsaturated | |
| Volek diet | 41% | 41% | 18% |
| Human milk | 47.5% | 40.5% | 12% |
Not too much difference. Perhaps PUFA intake needs to be higher than 11% of calories or 18% of fat to impact the thyroid.
Effects of high fat and thyroid responses to cold.
In 1945, Mitchell et al published two articles comparing the effects of proteins versus carbohydrates and fat versus carbohydrate on man’s tolerance to cold exposure [18][19]. Carbohydrate does better than protein, but worse than fat, at maintaining internal temperature as measured by rectal temperature.
On the first experiment, five men consumed a high protein diet (41% P, 40% F, 19% C) and five a high carbohydrate diet (11% P, 41% F, 48% C) for 5.5 months. Food intake was adjusted to mantain a constant body weight.
The effect of decrement in rectal and mean skin temperature during eight hour exposure to cold with light clothing:
| Rectal Temp | Skin Temp | |
| High Protein | 1.63 | 5.21 |
| High Carb | 1.05 | 3.65 |
| Significance | P=0.017 | P=0.0096 |
On the second experiment, five men consumed a high fat diet (10% P, 73% F, 17% C) and five a high carbohydrate diet (10% P, 23% F, 67% C) for 56 days. Food intake was adjusted to maintain a constant body weight. The excess fat of the high fat group was provided by butter and cream.
Decrement in rectal temperature from the first two hour to the last two hours of 6 hours exposures to -20º F (-29º C), with variable number of intervening meals:
| Number of intervening meals | Difference
0 and 1 meal |
Difference
0 and 2 meals |
|||
| None | One | Two | |||
| High Carb | 0.71 | 0.72 | 0.68 | -0.01 | 0.02 |
| High Fat | 0.60 | 0.36 | 0.33 | 0.24 | 0.27 |
| Significance | None | P=0.034 | P=0.018 | P=0.083
P=0.051* |
P=0.11
P=0.009* |
* These probabilities pertain only to the high fat diet
What is clear here, is that 6 hours exposures to -20º F decreased rectal temperature equally in both groups if no meal was ingested. Eating a high carb meal between the intervention did not produced any alteration. But, eating a high fat meal cut the decrement in rectal temperature in half.
Thyroid hormones are responsible for basal metabolic rate and heat production.
So, if a high saturated fat diet maintains body temperature better than a high carbohydrate diet when the body is subjected to cold, it would seem fair to assume that the thyroid functions better on this high saturated fat diet.
Conclusion
A diet with sufficient but not excess protein, moderate carbohydrate comprising a minority of calories, and high intake of saturated and monounsaturated fat but low intake of polyunsaturated fat would seem to be optimal for thyroid function. But this is the Perfect Health Diet!
References:
[1] Anthony Colpo. Is a Low Carb Diet Bad For Your Thyroid?. http://anthonycolpo.com/?p=1743
[2] Volek JS et al. Body composition and hormonal responses to a carbohydrate-restricted diet. Metabolism. 2002 Jul;51(7):864-70. http://pmid.us/12077732
[3] Danforth E Jr et al. Dietary-induced alterations in thyroid hormone metabolism during overnutrition. J Clin Invest. 1979 Nov;64(5):1336-47. http://pmid.us/500814
[4] Ullrich IH et al. Effect of low-carbohydrate diets high in either fat or protein on thyroid function, plasma insulin, glucose, and triglycerides in healthy young adults. J Am Coll Nutr. 1985;4(4):451-9. http://pmid.us/3900181
[5] Vazquez JA et al. Protein metabolism during weight reduction with very-low-energy diets: evaluation of the independent effects of protein and carbohydrate on protein sparing. Am J Clin Nutr. 1995 Jul;62(1):93-103. http://pmid.us/7598072
[6] Vazquez JA et al. Protein sparing during treatment of obesity: ketogenic versus nonketogenic very low calorie diet. Metabolism. 1992 Apr;41(4):406-14. http://pmid.us/1556948
[7] Whole Health Source. Vegetable Oil and Weight Gain. http://wholehealthsource.blogspot.com/2008/12/vegetable-oil-and-weight-gain.html
[8] Danforth E Jr, Burger A. The role of thyroid hormones in the control of energy expenditure. Clin Endocrinol Metab. 1984 Nov;13(3):581-95. http://pmid.us/6391756
[9] Cavaliere H et al. Serum levels of total testosterone and sex hormone binding globulin in hypothyroid patients and normal subjects treated with incremental doses of L-T4 or L-T3. J Androl. 1988 May-Jun;9(3):215-9. http://pmid.us/3403362
[10] Kumar A et al. Hypoandrogenaemia is associated with subclinical hypothyroidism in men. Int J Androl. 2007 Feb;30(1):14-20. Epub 2006 Jul 24. http://pmid.us/16879621
[11] Akin F et al. Growth hormone/insulin-like growth factor axis in patients with subclinical thyroid dysfunction. Growth Horm IGF Res. 2009 Jun;19(3):252-5. Epub 2008 Dec 25. http://pmid.us/19111490
[12] Soliman AT et al. Linear growth, growth-hormone secretion and IGF-I generation in children with neglected hypothyroidism before and after thyroxine replacemen. J Trop Pediatr. 2008 Oct;54(5):347-9. Epub 2008 May 1. http://pmid.us/18450819
[13] Stanická S et al. Insulin sensitivity and counter-regulatory hormones in hypothyroidism and during thyroid hormone replacement therapy. Clin Chem Lab Med. 2005;43(7):715-20. http://pmid.us/16207130
[14] Dittrich R et al. Thyroid hormone receptors and reproduction. J Reprod Immunol. 2011 Jun 3. http://pmid.us/21641659
[15] Krassas GE et al. Thyroid function and human reproductive health. Endocr Rev. 2010 Oct;31(5):702-55. Epub 2010 Jun 23. http://pmid.us/20573783
[16] Carani C et al. Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. J Clin Endocrinol Metab. 2005 Dec;90(12):6472-9. Epub 2005 Oct 4. http://pmid.us/16204360
[17] Bandini LG et al. Metabolic differences in response to a high-fat vs. a high-carbohydrate diet, Obes Res. 1994 Jul;2(4):348-54. http://pmid.us/16358395
[18] Mitchell HH, Glickman N, et al. The tolerance of man to cold as affected by dietary modification; carbohydrate versus fat and the effect of the frequency of meals. Am J Physiol. 1946 Apr;146:84-96. http://pmid.us/21023298
[19] Mitchell HH, Glickman N, et al. The tolerance of man to cold as affected by dietary modifi-cation; proteins versus carbohydrate and the effect of variable protective clothing. Am J Physiol. 1946 Apr;146:66-83. http://pmid.us/21023297
[20] Smith RE et al. Metabolism and cellular function in cold acclimation. Physiol Rev. 1962 Jan;42:60-142. http://pmid.us/13914396











I just read the Anthony Colpo post the other day so this is prescient. What caught my eye in Colpo’s article was lowering serum ferritin to improve insulin sensitivity. In another comment I think he said he took his from over 200 to around 50. I recently checked mine at 130 and am seriously considering getting it lower to see if it helps lower A1c and postprandial BG readings. On the other hand low ferritin seems to be a problem for people who are hypothyroid. Do you have an opinion on the ferritin-thyroid-insulin sensitivity angle? Regular blood loss and/or blood loss from parasite infections seems to fit well into the paleo framework.
Hi Yves,
I do favor low ferritin because iron is highly beneficial to many pathogens and some have evolved the ability to grab it from ferritin. So I make a point to give blood at every opportunity.
Iron deficiency can contribute to hypothyroidism, however, so you don’t want levels to get too low. I think if you include red meats and liver in the diet, but give blood, this should be a good balance.
Great stuff, this guy should post more often. More PUFA-bashing is always appreciated.
I think that this study that Anthony cited actually refutes the notion that low carb diets impair the thyroid, but it wasn’t mentioned in this article http://www.ncbi.nlm.nih.gov/pubmed/1249190
It is in the context of caloric restriction, but can make a point. Those who consumed no carbohydrates at all had reductions in serum T3 similar to fasting, but those who consumed 50g of carbohydrate did not despite caloric restriction.
This appears to be evidence for a dangerous aspect of very-low-carb diets but effectively refutes the notion that you need to consume more carbohydrates to keep your thyroid happy. Paul and Shou-ching are recommending more carbohydrate than that, and even Anthony’s mortal enemy Mike Eades says to have 50g of carbohydrate in his book. Most “low-carbers” get 50g, or at least say they do. As is pointed out in Perfect Health Diet, glucose from non-starchy vegetables doesn’t always make it through the gut to be utilized due to being consumed by bacteria. So people who are on a “50g carbohydrate” diet usually aren’t. They should include some starch from potatoes or other safe starches. Then we would probably see less low-carbers whose thyroids slow down.
However I find his article on low carb diets for athletes to be more compelling, and there is something to be learned from it. Most people should be exercising, but too little carbohydrate for activity level seems to be detrimental with regards to chronically elevated cortisol. So 50g of carbohydrate might not be for everyone. However it’s probably not a problem for non-athletes following this site’s recommendations.
Hi Stabby,
Yes, in that study 50 g / 200 calories carbs eliminated the problem. It just happens that’s our minimum carb intake.
I agree with your analysis – if people took 50 g digestible carbs from starches daily, we wouldn’t see problems.
I also agree that exercise, especially endurance exercise, raises glucose requirements, typically by 100-400 calories per hour of exercise. The minimum carb requirement should rise accordingly.
Best, Paul
Great stuff. I’ve read most of Mr. Colpo’s stuff in the past, and had never thought of looking at the issue from the angle of “types of fat” at the time, at least when addressing the issue of general macronutrient ratios.
Of course, through researching some of Ray Peat’s and a host of other people’s work and writings (Matt Stone, whom you’ve mentioned, comes to mind, but also Lita Lee, Josh Rubin, etc.), I have been made aware of the issue of PUFAs in negatively affecting thyroid function.
It’s great to see that this information is becoming more mainstream, and also great to see once again that, as Kurt G. Harris has said in the past (and I paraphrase): “Paleo” diets may ultimately prove useful due to the fact that, by accident, it removes neolithic agents of disease (namely, fructose, gluten and other toxins and, of course, PUFAs!!!). Again, thanks for the great post 🙂
Ferritin below 40-60 is associated with restless legs and poor sleep quality – I have to say I see far more low ferritins in clinical practice than high.
The thyroid issue and pufa intake is clear cut clinically as well in humans. High pufa intake leads to excess series two prostagladins (omega 6) and this causes leptin resistance at the hypocretin neurons via increased cytokines signal blocking at SOCS3 and other receptor changes. When this occurs there is a biologic rise in reverse T3. Reverse T3 is a competitive inhibitor to T3 and blocks conversion to T4 from T3. This effectively shuts the thyroid down completely and accounts for the weight gain seen with PUFA’s. The real clinical conundrum is that most physicians are not aware of this mechanism because they never order rev T3 and rely too heavily on a regular thyroid panel. You can have. Completely normal thyroid panel and still be markedly hypothyroid. This is published in every endocrine book used in med school but most have forgotten this clinical pearl. All the data you supplied is just verifying something we have known about in human biochemistry for some time now. They new key link is the pufa socs3 link at the hypothalamus. Clinicians and patients a like need to be aware of this situation. This can also happen with excess Ach from fructose metabolism in great excess to form palmitic acid. It has the same affect on the thyroid,
How does fatty acid oxidation and its effect on uncoupling proteins relate to interpretations in studies involving body temperature?
How do uncoupling proteins themselves affect thyroid levels?
The PHD has been a big help in getting my carbs from safe starches like potatoes, sweet potatoes and rice. I’ve never been a big PUFA consumer so I kind of lucked out there, mostly using EVOO. However you along with Stephan at WHS have convinced me to start using butter from pasture raised cows as well as coconut oil.
Thanks, Emily, for the reminder – there’s more than one way iron deficiencies can hurt.
Thanks, Jack.
Hi John,
Well, thyroid hormone directly influences mitochondrial uncoupling and heat generation.
Fatty diets and fat oxidation affect thyroid activity in part via PPAR nuclear receptors / transcription factors.
But I prefer not to trace pathways unless I’m in desperate need of clues because it’s always more complicated than we know.
Colpo is a bloody idiot. not the first time i’ve concluded this!
having been hypothyroid ALL MY LIFE, i’ve made a particular study of how to ameliorate the condition, especially since the “shortage” last year (sarcasm alert). looking at his photo, i doubt that Anthony has any first-hand experience.
where do i start?!
FORTY YEARS AGO, it was known that omega-6s inhibited thyroid function. it was proposed at that time that vegetable oils could be useful to combat hyperthyroidism.
iodine was the treatment of choice, with excellent results all during the 1800s, till those jerks, Wolff and Chaikoff (in the 1940s) promoted their iniquitous campaign against it — and even then it was a bloody lie, as their study didn’t prove what they said it did. it was very recently that Mario Renato Iwakura revealed to us laypeople that only in the deficiency of selenium is iodine deleterious to thyroid function.
YES, we need to scrupulously avoid wheat, millet, and other known goitrogens. YES, sufficient iron supplementation is important for thyroid function, because the poor absorption of stomach-acid-impaired people keeps us from benefitting from our theoretical intake, and iron is important for hormone manufacture. YES, we need to make sure our real, animal-source vitamin A is higher than normal, as vitamin A is crucial for thyroid function, a lot of people can’t convert beta-carotene, and protein metabolism eats A up rapidly. YES, we need to watch our magnesium, selenium, and copper ingestion levels, get adequate sleep, and manage stress. these are all important to maximize hormone production and the conversion of t4 to t3.
i get sick of seeing the half-informed enunciating sweeping conclusions about what’s good for those of us with a problem! we’re not all alike — what a surprise (i commend Chris Kresser for his recent article on this subject, in respect to weight loss). personally, i do HORRIBLY on a high-carb diet, thrived on Atkins’ induction, and am encouraged by my first attempts at ingesting a LITTLE more on the PHD….
please forgive my rant — it’s been building for years, listening to people who have nothing to lose, pontificating to those of us who can’t afford to make the mistake of following their advice!
Has sufficient attention been paid to ensure that it’s indeed PUFA and not trans fats (in corn oil and other veggie oils). Also, it’s high PUFA in general, not any specific PUFA? I would tend to think the n-6 PUFA would be implicated more in damaging thyroid rather than n-3 PUFA? Is it not reductive to conclude that the PUFA from nuts, fish, olive oil, and avocados are not any better than the PUFA in vegetable oils that are also replete with trans fats?
Bashing Colpo and PUFA in one single post! It can’t get better then that! 😀
thanks tess, good rant.
I must be one of the few hypothyroid patients who NEVER have a problem with iron. When pregnant, I was told I had good iron levels for someone who wasn’t pregnant! I did give blood recently, and it sank like a stone. Maybe I have too much? I should try to find my numbers. I do plan on giving blood more, though.
This whole post just made me sigh… again. It calls to mind all my dear friends and family who are striving for good health, but who are consistently mislead. My oldest and dearest friend is the best example.. she is an avid exerciser and food addict. In her attempts to “make good,” with herself she is taking nutrition advice from her personal trainer. He has prescribed oatmeal, low fat greek yogurt, almonds, fish, baked chicken and flax seed oil. Limited veg and fruit and little else that was not mentioned there. With the nuts, fish and flax seed oil he has basically prescribed a diet high in PUFA and has told the people he trains that to keep in mind that although the diet seems tough to stick with that they are receiving ALL of their essential nutrients so not too worry. Wow.. when she told me this I nearly feel out of my chair. It is people like him that look fit (somehow even though they are clearly damaging their metabolism) and preach a false gospel that I would really love to punch right in the kisser.
Truth be told my arguments generally fall on deaf ears as nearly all mainstream “experts,” i.e, Dr. Oz are in favor of fats only in the MUFA and PUFA categories. Surely a medical doctor with a successful daytime television show knows more than me. 😉
Good article but I have a question about the natural PUFAs from real foods, not industrial oils.
I eat a fairly low-carbohydrate, high-saturated fat diet myself but I eat a decent amount of nuts pretty much every day. I’m sure Omega-6 PUFAs aren’t a major source of calories in my diet, but they definitely do contribute somewhat.
What is the perfect health diet’s view on natural Omega-6 PUFAs from nuts?
Thanks to both Paul and Tess for some more reminders of how to maximize thyroid function! Ironically my blood counts are always a bit high, despite my mild hypothyroidism, so I took one gentle reminder and donated blood again today. Hgb was 17.2, but was 18.4 a couple of years ago. I still can’t get my am body temp above 97.3 despite making many changes these past 2-3 years.
Paul, I wonder if you might consider a nice summary table at the end of your thyroid series to put all of the Must Do and Must Avoid ideas in one easy to reference spot. Also, possibly some sort of hierarchy based on biggest bang for the buck, most scientifically proven, etc would help focus my efforts.
…. I was thinking after writing the last post about my temp readings. If body temp is a good indication of thyroid function then for me that must be that alcohol consumption depresses my thyroid. I drink on a regular basis and check my body temp occasionally after reading about the connection on Matt Stone’s blog. Generally, my body temp is between 97.3-97.8. Recently, for the past week or so I have no had any alcohol and took my temp this morning and it was the highest it has ever been at 98.2. This seems logical, but I am wondering Paul (or anyone) if you can explain the mechanism by which this occurs. Or if this is just anecdotal and there is little correlation.
Mario,
Did you see Anthony Colpo’s reply in an article on my email exchange concerning PUFA in the studies being the problem and not saturated fat? I posed your comment response on his article on thyroid to him. I would have given you credit if I knew he was going to use it in an article for all to view. I think you covered the same ground in his response but just wanted to make sure his reply was considered.
http://anthonycolpo.com/?p=1792
I really liked the “indirect” section. Maybe with so many paleo and low carb community growing this last decade some more high-saturated and monounsaturated diets will be studied and get direct evidence. I can dream can’t I? 🙂
Jaybird,
Yes, I saw his replay to your e-mail, but nothing he said convinced me. In the Stephan post there is also an example of a human study that man gained more body fat on a diet high in linoleic acid, just like the rat study.
And, if you look at the study cited by Stabby, in a severe calorie deficient diet, 50g (FIFTY GRAMS) of carbs was enough to restore T3 and rT3 levels. Based on this, how on the hell one can conclude that only a high carb diet is the best for thyroid?
“Based on this, how on the hell one can conclude that only a high carb diet is the best for thyroid?”
But… but… but… I got nothing. 🙂
All kidding aside, great work Mario!
Paul,
Paul, what do you think of this:
People keep a virulent debate about the “metabolic advantage”. But if eating a high saturated fat diet makes the thyroid work better and adjust up the resting metabolic rate (as seem to be the case of this post), why do people feel personally offended by the conclusion:
In a isocaloric condition, people with a high fat diet can loose more weight (through elevated metabolic rate).
But, I agree that the degree of this advantage is variable, e perhaps not so big.
I would appreciate your thoughts on this.
Tiago.
Hi Paul, question for you – I’m one of the many “women of a certain age” (ok, 52) who started on low-carb, rapidly lost 35 lbs & have now been stalled for several months well short of my goal weight. In addition to the very depressing news I just read here about the difficulty (I refuse to say impossibility!) of losing weight while in peri/menopause, my thyroid & 2 of my parathyroids were removed several years ago due to a tumor. I was on Synthyroid initially but my doc discontinued it as my bloodwork was apparently normal. It has not been tested recently.
What do you recommend in my situation? Should I be taking iodine as per PHD? I should mention that I don’t have the book (yet!), just found this site from CarbSane & know very little about the workings of the thyroid. So any suggestions you have for me are gratefully appreciated!
Hi Randle,
Trans-fats are a problem but they can form in foods such as nuts as well. I think the evidence against PUFA, whatever the source, is pretty solid.
Hi Kris,
We believe omega-6 from all sources should be limited, preferably to 3% of calories or less. This allows a balance between omega-6 and omega-3 to be established with a reasonable fish intake (1 lb salmon per week).
This requires pretty stringent avoidance of high-omega-6 foods including nuts. But some nuts are low in omega-6. Macadamia nuts have only 3%. Many are between 10% and 20% omega-6. So moderate amounts of these can be eaten.
Hi Rodney,
It’s a good idea, I’ll have to do summary posts like that from time to time.
Hi Lindsay,
It’s a good question to look into. Alcohol is known to lower core body temperature via vascular dilation (http://www.uihealthcare.com/topics/medicaldepartments/pharmacy/alcoholandcold/index.html, http://www.ncbi.nlm.nih.gov/pubmed/6974036). I would have to look into whether it has any thyroid effects.
Hi Mario,
As Jaybird says: Great work!
Hi PrimalBR,
I do think metabolic advantages are pretty small in calorie terms. To me it’s much more important to sustain proper body temperature for health reasons, than as a weight loss device. But I do think it’s an argument for high saturated fat diets.
Hi Leila,
I do recommend iodine, it’s a general purpose aid to immunity and driver-out of toxins. It won’t necessarily do much for you but it’s a good thing to take — with selenium and magnesium and vitamin K2 my favorite supplement.
I don’t understand how you can get by with no thyroid hormone if your thyroid was removed. You should interpret your bloodwork yourself, the “normal” ranges are way too wide and your doctor may not be aware of that. I would have thyroid levels tested routinely given that your thyroid was removed. Also, know the symptoms of hypothyroidism and watch yourself carefully for them.
Best, Paul
Is there any way to reduce ferritin levels besides giving blood or introducing intestinal parasites? I ask because I tried giving blood for the first time about three years ago and passed out when I was already lying down (no medical problem, I’m just squeamish). I was politely told not to come back.
I have Hashimoto’s. I spent many years seeing traditional Endocrinolgists only to continue to feel horrible. I gained weight, could not sleep and was constantly depressed. I had a very hard time concentrating. I was told to exercise more and eat less.
How does that work when just taking a shower causes exhaustion? It was frustrating and feeling like no one was listening only made matters worse.
I did some homework and found a new doctor, one who orders lab tests but also listens to me and evaluates my symptoms and together we came up with a treatment plan.
Since that time, about 10 years, we have had to tweak the plan a couple of times.
The current plan includes Synthroid, Cytomel T3 since I have become a poor converter and Low Dose Naltrexone to help regulate my immune system. Prior to that I used Armour but when they changed the formulation it stopped working for me. Originally it worked very well.
I also eliminated all grains because of their inflammatory response, GMO issues and celiac symptoms. Rice and potatoes do not cause the GI disturbance however, I am careful because of glucose issues.
My body temp. has increased from a low of 96.5 to now 98.
No longer do I battle depression, I sleep better, I can exercise, no mid afternoon crashes, no crazy hunger, balanced moods, and I lost significant weight, all but 10 pounds.
Vitamin D levels were 40 now at 67.
Low magnesium levels have been corrected.
Stealth bowel infections were found and treated.,
I cleaned up my diet, pay attention to supplements, work on detoxifying, getting proper rest and exercise and avoiding toxic people, places and things.
None of that would have been possible had I not continued to look ( yes, I wanted to give up) for a health care provider who would work with me and who ordered the complete tests for Thyroid disease and looked at the whole patient (me) instead of just relying of a lab value.
We must be informed health care consumers.
Outwardly, I looked fine, a bit tired. Many of my complaints were viewed as looking for attention or psych. in origin.
Knowing if you do have autoimmune thyroid disease is important because of the risk of developing another autoimmune disease. Similar to snakes, if you see one watch out for another one.
A particular ANA pattern gives hints on what to watch for.
It’s easy to get a TSH test even a Free T4 but getting the TPO test is a bit trickier. Treatment is the same, hormone replacement, but the overall outlook depending on the results will give information on how to manage going forward.
On the blood donating issue, I don’t. Years ago I had multiple tick bites. I was not in the Northeast nor did I have the hallmark EM rash so nothing was no treatment or follow up.
I do have a positive WB but it does not meet “the” criteria. So in an abundance of caution and my own peace of mind, I do not donate.
Ticks prefer tissue as opposed to blood.
Still, taking no chances.
I have some issues and most probably always will but they are managed. They don’t manage ME.
Today I had a doctor’s appt.
He said I looked great!
Thank you Paul for your informative website. I appreciate your thoughtful posts.
Any chance your great doctor is in NY? If so, I need a good one.
Thanks, Scarlett. Very nice story. I’m glad you’re doing better.
Paul, I was eating LCHF for about 2 years, and lost about 55 pounds.But I could not stop losing,despite eating 5000 cal.a day,lost alot of muscle mass.6 months ago I started eating Dr. Peat style,have gained back 22 pounds,body fat went from 23% to 17%, am temp. 96.5 up to 97.9, and am sleeping all night! For me, adding back to fruit,and eating a balanced ratio has been great,will see where it takes me.
nice article.
i also found higher SFA makes me more cold resilient (i have mild Raynauld syndrome)
regards,
can you donate without a paypal account? it wants me to open an account.
Hi Kevin,
You might have had scurvy, be sure to supplement vitamin C.
Hi Pam,
I’m puzzled too. Paypal says you can donate with just a credit card, no account needed, but then the donation page says “Create a Paypal Account or Login.” I’ll ask them about it. Maybe the email address and password are not required.
Pam, you may want to investigate the idea of an infectious cause of Raynauld’s. “The New Arthritis Breakthrough” by Henry Scammell is excellent, and Roadback.org is good, too.
So is potatoe chips fried in coconut oil o.k. ?
http://anthonycolpo.com/?p=2028
Uh oh. Now what?
Hi Ron,
Yes.
Hi Monte,
I’ve written Anthony an email, cc’ed Mario. I’ll decide tomorrow whether it’s worth putting my response up on the blog. The gist of it was this: Mario’s post explicitly advocates “moderate” carb consumption and never denies that glucose-deficient diets may contribute to hypothyroidism, so I can’t find any conflict over science. Anthony’s reaction was intemperate.
Best, Paul
Oh great! Where can I get some coconut oil? I live in Surrey, England. There are chips everywhere I look. But no one seem’s to sell coconut oil.
I do think metabolic advantages are pretty small in calorie terms.
Paul,
Do you believe in metabolic advantages? People like Calpo and Carbsane are arguing that metabolic advantages are basically junk science and that its all about calories and energy deficits or surpluses.
-Doug
Low carb, blood lipids and thyroid
Some people eat low carb in an effort to normalize blood lipids. Many people have sub clinical hypothyroid symptoms and don’t know it. Suboptimal thyroid might be the proximate cause of high lipids in the first place.
I suspect I fell into this category. At first triglycerides were high (300, 500) but were controlled by cutting carbs to around 100gpd (TG:100 – 200). Then cholesterol started rising over months. I cut carbs to 30g per day and noticed both triglycerides and cholesterol rising more rapidly. I cut carbs further to around 15g per day and the lipids took another jump. TC got as high as 350. I did lose about 10% of my body weight in the first six weeks, then stabilized.
There are competing theories for this lipid surge:
i. That the surge is temporary as fat is being purged from the body. A few writers claim that the situation will right itself in about six months;
ii. That the metabolism has gone into hibernation mode and that rT3 is blocking LDL receptors in the liver, preventing clearance and causing a surge of LDL;
iii. That a diet high in saturated fat causes a ‘superabundance’ of cholesterol which the liver can’t handle.
iv. In March Paul wrote that malnutrition in general and copper deficiency in particular “… is, I believe, the single most likely cause of elevated LDL on low-carb Paleo diets. “http://perfecthealthdiet.com/?p=2547
In fact this theory need not be exclusive of the rT3 hibernation theory. It might be that mineral deficiency contributes to thyroid deficiency, or the inability of the metabolism to come out of hibernation mode once the conditions have returned to normal.
What to do?
Option 1: Do nothing. The simplest thing to do would be do nothing, wait six months and see. But one person reported LDL around 300 for up to three years. Paul’s article on morbidity studies suggests that LDL above 200 puts one at the highest risk of death. http://perfecthealthdiet.com/?p=3836
Option 2: cut saturated fats. This was my last option. I prefer to try other things first.
Option 3: supplement with copper and eat liver. I’ve been doing this for a couple of months. No change.
Option 4: increase net carbs to 50g per day or more. I did this with no apparent result.
Option 5: test and supplement T3 thyroid. I discovered I had high free T4 and below range free T3. This led to a presumption of high rT3. (The test for rT3 is not available in Thailand.) Being impetuous, curious and keen to prove that the problem was one of clearing, not superabundance of LDL from eating too much saturated fat, I opted for the T3 cynomel supplementation, taking counsel from the yahoo group. (This required weeks of preparation: iron test, saliva cortisol test, order cynomel.)
Results were profound. After one week on a tiny dose of cynomel triglycerides dropped from 150 to 90. After two weeks TC dropped from 350 to 300. After three weeks TC dropped from 300 to 220. Now in the fourth week the lipid numbers are stable. The yahoo group protocol requires continuing for 12 weeks.
I suspect that I had a long term rT3 issue and that the low carb diet exacerbated it. This might have been due to mineral deficiency. It might be due to high cortisol. It might be due to both.
The challenge is to try and address the underlying causes and eventually wean off the T3 supplement.
Anthony Colpo reminds me a bit of Lyle McDonald and Alan Aragon, they all respond with a lot of arrogance.
Therefore I don’t read their blogs, nothing I dislike more in this world than arrogant people.
He appears to view things from his own perspective and his blog seems to be more fitness and bodybuilding oriented.
Personally a very low-carb diet is not something I would recommend for these athletes, but I think it’s great for regular people that need to lose weight and it has been supported by numerous studies that low-carb is very effective for weight loss in these people.
@Ron in Surrey: I have taken to ordering Nutiva coconut oil from Amazon – this is an organic, extra virgin product and you can get it in 54 oz plastic containers. Indian grocery shops and the larger branches of some supermarkets also sell coconut oil, but I haven’t seen extra virgin in either so far.
Hi Doug,
I believe in “metabolic differences” but a macronutrient that, in a given context, leads to burning of slightly more calories may be either beneficial or harmful for weight loss, so I think it is prejudging the matter to describe these differences as “advantages.”
If extra calories are burned because mitochondria are more responsive to thyroid hormone, then that’s beneficial. If extra calories are burned because the body has an excess of glucose and has to dispose of it, that’s probably unhelpful.
Hi Gregory,
Great comment! Thank you for sharing your experiments.
I think we should probably put the whole story in a blog post for the benefit of others suffering from the high LDL issue.
I’ll write you about it.
Best, Paul
@Michelle,
arthritis can cause Raynaud? i have never heard of it. thanks!
but i don’t have chronic pain in joints. so i’m not sure. will study more.
i got it in one really cold & windy winter when 16 or 17 (severe frost bites on all fingers & toes).
is carb supposed to be more thermogenic than fat? my experience is just the opposite. fat, more specifically, SFA, helps a lot.
regards,
(paypal still insists me to open an account, strange)
@Pam,
Dr. Thomas McPherson Brown recognized that an entire family of connective tissue diseases responded to low dose, pulsing antibiotic therapy.
So, that includes the different forms of RA, Raynauld’s, lupus, fibromyalgia, scleroderma, etc.
The book, TNAB, is a great intro to Tom Brown and his work, and the idea of an infectious etiology to these autoimmune diseases.
Unfortunately, both Dr. Tom Brown and Henry Scammell have both passed.
http://www.amazon.com/New-Arthritis-Breakthrough-Improvement-Inflammatory/dp/0871318431
http://en.wikipedia.org/wiki/Thomas_McPherson_Brown
Another good book is “Why Arthritis?” by Harold W. Clark, one of Brown’s colleagues.
http://www.amazon.com/Why-Arthritis-Searching-Rheumatoid-Disease/dp/093641751X/ref=sr_1_1?s=books&ie=UTF8&qid=1313955820&sr=1-1
It is possible to get tested for pathological strains of mycoplasma, strep, and chlamydia through The Arthritis Research Center, http://www.tarci.net
The director of ARC, Dr. Millicent Coker-Vann used to work with Brown.
ITA with the PHD idea that chronic or stealth infections are an important piece of the puzzle.
Hi! Valda and thanks for the info. I have an Amazon account and will now check that out. But I have another query. The reason I want some extra fat in my diet is for the calories. I was following a Paleoithic diet for a while but could never seem to get my total calorie intake above 1200. In fact if you follow any type of healthy whole food type diet it seem’s impossible to eat enough calories. My query is what is the required amount of calories? Is it the calories recommended for age, sex, height frlom the formula’s you see in health mags and web sites or is there a different lower amount of total calories to be had from a special healthy eating type formula that I have’nt discovered yet. You see I’m not sure whether my lethargy and tiredness is due to my underactive thyroid or just not eating enough overall calories. Is it worth eating empty calories just to reach my calorie count?
Just ordered some Nutiva extra virgin coconut oil from Amazon (can’t wait to fry some chips). Also looked at The Perfect Health book while on the site but they only sell a paperback version for £15. Seem’s a lot for a paperback book to me! Does anyone know of a kindle or e book version available anywhere.
Wow! Colpo even quoted my light hearted comment! What honour! 😀