The results from the Perfect Health Retreats continue to surprise me.
Retreat attendees come for all sorts of reasons. In terms of weight, they have so far had a fairly similar profile to the general middle-aged population, with almost half being obese and another quarter overweight. That’s enough obese and overweight participants to give us insight into the effects of our advice for weight loss.
Weight Loss Experience at the Perfect Health Retreat
When I was preparing my Ancestral Health Symposium talk on weight loss, I noticed a remarkable pattern that I didn’t have time to discuss in my talk. The pattern was that the amount of weight loss during retreats was proportional to the excess weight of the participants.
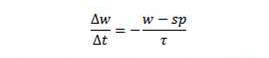
Here are some charts, with the amount of weight loss during the retreat plotted against BMI. From our 2013 retreats, which lasted 30 days, I’ve plotted just the obese participants:
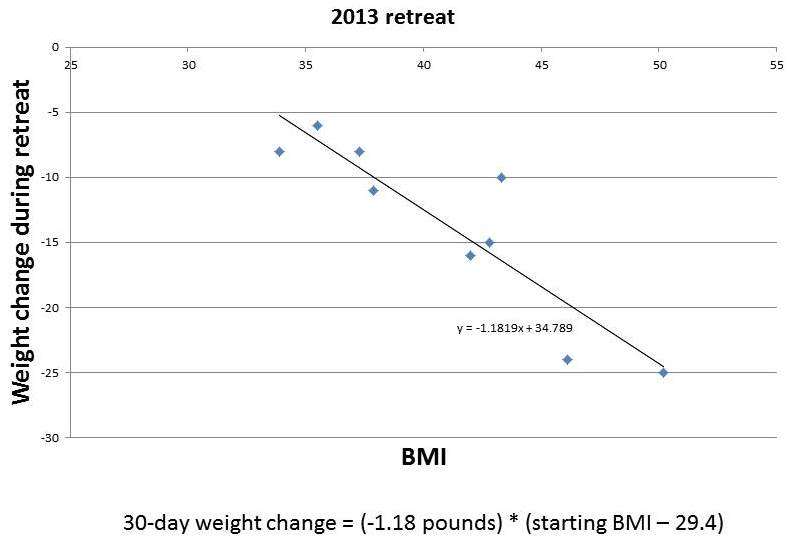
And from our May 2014 retreat, which lasted two weeks, I’ve plotted the obese and overweight participants:
You can see that the amount of weight lost in this short period is roughly proportional to starting BMI. It tracks remarkably closely to a straight line. I’ve put the equations for the lines underneath each figure.
If weight loss follows these straight lines, then you can easily envision what would happen to someone with a high starting BMI, say 50, who lived at the retreat permanently. He would lose weight rapidly at first. As his weight (and BMI) declined, his rate of weight loss would slow, tracking the line. As he approached a destination BMI in the 20-29 range, his rate of weight loss would approach zero. His weight would stabilize at this destination BMI.
(Parenthetically, let me comment on a few features of the charted data. First, it doesn’t surprise me that the destination BMI in the 2013 retreats was higher than that in the 2014 retreats; our program was still under development in 2013, the retreats are much more optimized now; for example, the 2013 retreats were held in a rather dimly lit facility with few windows, yet we know that circadian rhythm entrainment is huge for weight loss. Second, it doesn’t surprise me that the 2014 data is noisier than the 2013 data; the shorter retreat means that other factors, such as jet lag from traveling to the retreat, influence outcomes more significantly; also, in May 2014 we didn’t weigh anyone at the retreat so weights were self-reported from home by guests, making the weights not as reflective of the retreat environment and the time between weighings somewhat variable. Third, it doesn’t surprise me that the rate of weight loss at the 2014 retreat was slower than at the 2013 retreat; 2014 retreat participants were explicitly encouraged not to restrict calories, and wine, snacks, and desserts were served daily, whereas in 2013 the proprietor encouraged some calorie restriction and did not serve alcohol.)
The destination BMIs – the weights at which the fitted lines indicate weight loss would stop – are remarkably close to normal weight.
Implications for a Body Weight “Set Point”
Obesity researchers have found the concept of a body weight “set point” to be useful in explaining obesity. However, they generally find that the “set point” is well above normal weight, even after weight loss interventions.
Our Perfect Health Retreat weight loss experiences are consistent with the existence of a set point. However, Retreat experiences are best understood as telling us that:
- The body has a desired weight – a set point – that weight inexorably migrates toward.
- The pressure or force driving weight change, as indicated by the rate of weight change, is proportional to the deviation of actual weight from the set point. A larger deviation from the set point creates a greater pressure for weight change and a more rapid migration toward the set point. As the set point is approached, the rate of weight change slows down.
- In the context of our retreats, in which people follow the Perfect Health diet and lifestyle, the set point is reset to a normal weight within a few days of their arrival at the retreat.
If PHD does indeed reset the set point to normal in a few days, it is consistent with the theme of my Ancestral Health Symposium talk: it is diet and lifestyle that determine weight; fix those and your weight will inexorably normalize.
But this conclusion is radically contrary to the beliefs of academic obesity researchers. The general view is that changing the set point is extremely difficult, in part because the determinants of the set point extend back in time many decades:
Your heredity and your environment-starting back at the moment of your conception-determine your set point. Over the long term, excess food and insufficient exercise will override your body’s natural tendency to stay at its set point and lead to a higher, less healthy set point.
This implies that normalizing the set point will also require years or decades, because that is how long it takes for the influence of past set-point-raising factors to expire.
The Center for the Study of Nutrition Medicine, led by the distinguished obesity researcher George Blackburn, advises that one can’t sustainably lose more than 10% of body weight in six months:
Scientific evidence supports losing no more than 10% of your body weight at a time. It turns out that the body’s set point and its many regulatory hormones dictate the effectiveness of the 10% loss. That’s the amount of weight you can lose before your body starts to fight back. Many clinical studies have confirmed this phenomenon. Of course, some people can lose more than 10% at a time, but precious few can then maintain that loss.
After you maintain your new, lower weight for 6 months, you can repeat the cycle and reset your set point again by losing another 10%.
Is Dr. Blackburn’s conclusion, confirmed by “many clinical studies,” valid for PHDers? To test that, we need a longer time series.
The largest weight losses at the Perfect Health Retreat have been about 10% of body weight in 30 days. If Dr. Blackburn is right, then after people on PHD lose 10% of the body weight – i.e., after one or two months on PHD – then we should see weight loss stall or enter a yo-yo pattern for the remainder of six months, until the set point adjusts lower and weight loss can resume.
Alternatively, if PHD immediately and permanently resets the set point to a normal weight, the rate of weight loss in PHDers should track a straight line just like in the retreat data. We should see continuous weight loss with no stalls – although there will be a steady slowing of weight loss as a normal weight is approached. In the long run, weight is normalized permanently, and there is no weight regain as long as the person remains on PHD.
Which is it?
The long-term pattern of weight loss on PHD
Fortunately we have a few cases in which PHD readers have faithfully followed our advice, tracked their weight closely, and shared the data with us.
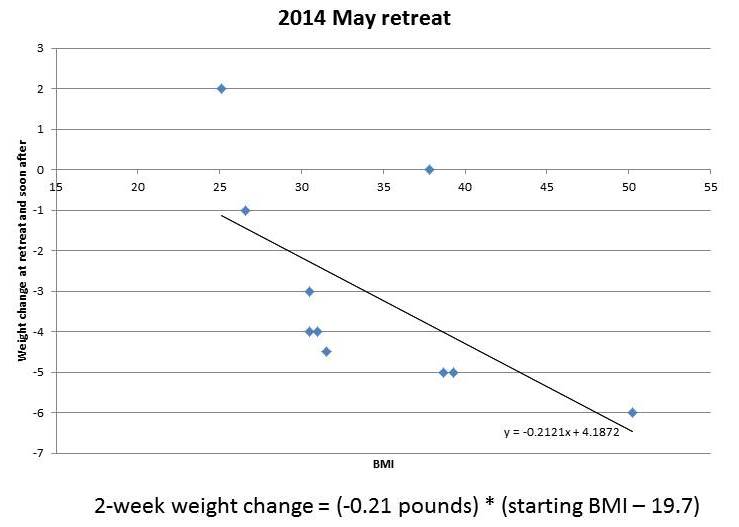
Before I discuss their weight loss experiences, let me describe the weight loss path we would expect to see if the pattern observed at the retreats holds up. The weight loss pattern observed at the retreats is described in a simple equation:
Those of you who took calculus will recognize that as a differential equation which we can integrate. It leads to the following formula for weight as a function of time:
So if PHD is really re-setting the set point to a normal weight within a few days, after which the set point doesn’t change — it just stays at the same weight, normal — then we should see weight loss follow this exponential decay.
OK, now let me get to cases.
The case of Jay Wright
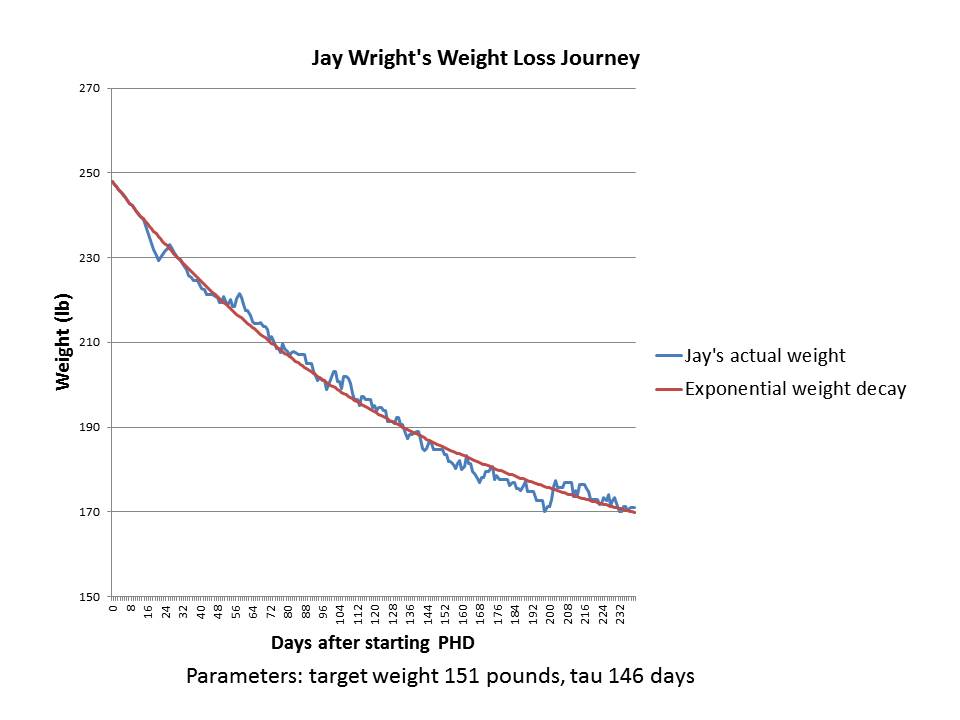
Previously on this site we discussed Jay Wright’s weight loss journey. Here is his weight in blue, and I’ve fitted an exponential decay to it in red:
It’s a pretty good fit with a set point of 151 pounds and a characteristic time of 146 days.
Jay’s weight loss took place in 2011. In several years since then, his weight has remained stable around 170 pounds. I believe Jay’s height is 5’10”, so his BMI at 170 pounds is 24.4 and his BMI at the fitted target weight of 151 pounds would have been 21.7.
As you can see by reading Jay’s story, during his period of weight loss he was intentionally restricting calories to 1200 calories per day; but when he got to his goal weight of 170-175 pounds he stopped restricting calories and ate to appetite. I’ll speculate that intentional calorie restriction may lower the set point by a few BMI points, say from 24.4 to 21.7, so that Jay’s “set point” during his weight loss period was 151 pounds but it reverted to 170 pounds once he began eating ad libitum.
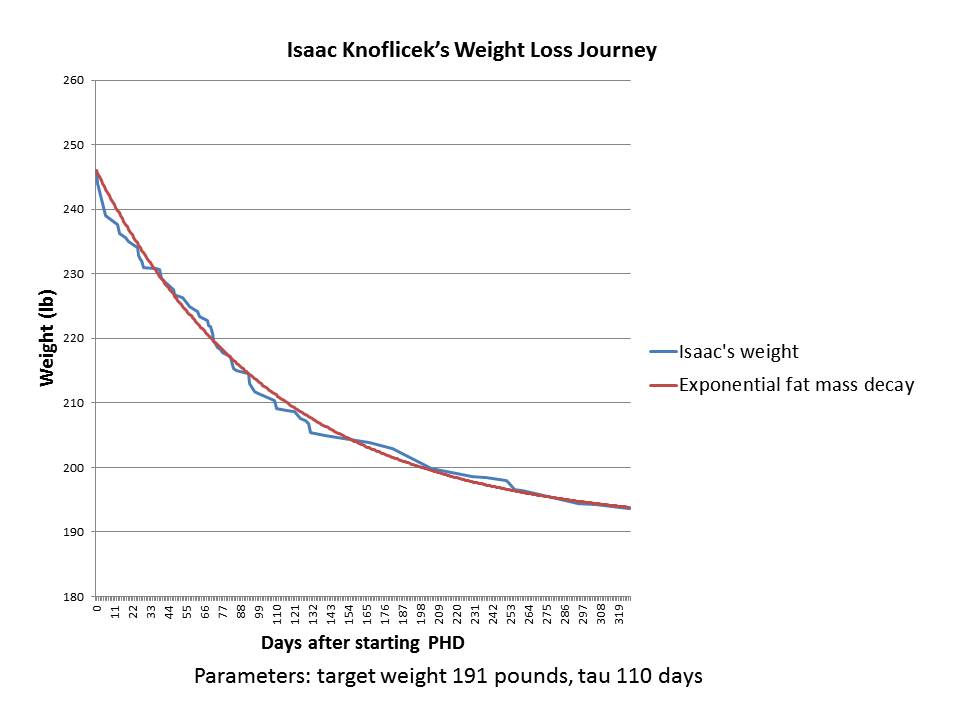
The case of Isaac Knoflicek
Our second case was posted by Isaac Knoflicek on the PHD Facebook group a few weeks ago. Here was his weight loss chart. He described it this way:
~110 lost, first chunk was bike commuting, then after about a year of that I started PHD and the weight came off like crazy.
Isaac gave me his weight loss data. Here is what happened after he began PHD:
As you can see, it’s a great fit to an exponential decay – an even better fit than in Jay’s case.
Isaac is 6’3” (190.5 cm) tall, so the target weight of 191 pounds is a BMI of 23.9 – absolutely normal.
Although Isaac’s data ended in early 2013, he wrote, “I’ve spent the last year and a half making smaller tweaks but generally staying around the same weight.” That’s consistent with him having gotten close to his target weight; and with his set point having been permanently reset to a normal weight, so that there is no biological pressure for weight regain.
Here are Isaac’s before and after photos:


Implications
Every obese person who has come to our retreats has lost weight (save one whose weight was unchanged), and in most cases weight loss tracked closely to the same pattern for all participants: a linear relationship between weight loss rate and starting BMI. The line reaches a zero weight loss rate near a normal BMI.
The implication is that for nearly all retreat participants, PHD actually fixes all the factors of overweight or obesity and leads to a normalization of the body weight set point. Although our experience at the retreats is still limited, the statistics are good enough to infer that PHD should work for most, if not all, non-diabetic obese people.
Another implication is that it’s possible to normalize set point in just a few days. If set point wasn’t normalized in a few days, weight loss rates over a 14-day retreat could not track a straight line.
Very likely, the reason the set point has appeared persistently high to academic researchers is that the weight loss approaches they have studied don’t actually address most factors in obesity. My Ancestral Health Symposium talk explains that weight is set by a multifactorial process and if multiple obesogenic factors are left uncorrected, the set point will remain elevated.
A third implication is that there is a characteristic physiological time for weight loss, and it may not be possible to accelerate weight loss much. The fastest rate of weight loss we observe is about 4 months to move 63% of the way toward normal weight from current weight. Based on rates of weight loss at the retreats, 6 to 8 months is more typical.
Fourth, it’s not obvious that calorie restriction is either necessary or desirable for long-term weight loss. If all calorie restriction does is temporarily lower the set point by a few BMI points, without affecting the characteristic time for weight loss τ, then calorie restriction may have little effect on either the ultimate weight or on how long it takes to reach it. Calorie restriction may be an energy-sapping, misery-inducing tactic that succeeds only in reducing weight slightly for a few months, with no long-term benefit. And it may have health risks.
Finally, the “last ten pounds problem” has produced a lot of angst. People often lose weight successfully to a weight about 10 pounds above their personal target, then find it extremely difficult to lose the last 10 pounds. We can now see why the last ten pounds can be so hard to lose. First, any minor defect in diet or lifestyle may raise the set point slightly. Second, weight generally rises with age, and people may use their younger weights as targets; so they may be underestimating their body’s physiological weight target. But mainly, it may just be that weight loss becomes very slow once you are within ten pounds of the set point. At 10 pounds above the set point, it takes 6 months to lose 6 pounds, even if you do everything perfectly. That’s only 1 pound per month. From 4 pounds above the set point, it takes 6 months to lose another 2.4 pounds – only 0.4 pounds per month. Then the pace of weight loss slows further. Once the rate of weight change slows to 0.1 pounds per week or less, it will appear to have gone to zero.
Conclusion
To convince skeptics, we will need more data. But I’m going to jump directly to these conclusions:
- For most people, PHD (including both diet and lifestyle practices) will cure obesity – in the sense of normalizing body weight set point – in a few days.
- Although the set point is normalized almost immediately, weight loss takes time. Even if you do everything perfectly, it takes about 6 months to shed 63% of excess weight, a year to lose 86%, 18 months to lose 95%, and 2 years to lose 98%. The last few pounds take a long time to go away.
Curious if I’m right? If you are overweight and would like to test this personally, come to our retreats and help us generate more data.












Fantastic!
There is a lot here that reminds me of the experiences Seth and others following the “Shangri La” diet have reported. Rapid drop in body-fat (not body weight) set point followed by a gradual and steady decline in body weight (presumably due to a drop in adiposity). I wonder what role falvor-calorie associations play in the successful weight loss on the PHD?
The brain is so complex, I need help from you psychologists and neurobiologists to figure that out!
But if I had to guess, here’s what my hypothesis would be. There are two semi-independent processes in the brain esp. hypothalamus. One is status assessment: what is our nutrient status, circadian rhythm status, inflammation status? PHD works by improving status — removing nutrient deficiencies and excesses, optimizing circadian rhythms, reducing inflammation. I would predict that when status is good, flavor-calorie associations don’t matter.
However, if status is poor, the brain motivates action to fix it. Commonly, one solution is to obtain more food: this fixes nutritional deficiencies, but also in our evolutionary environment would fix circadian rhythm status (by motivating action/exercise to obtain food, sun exposure in the search for food, higher food intake which is a zeitgeber, also hunting and gathering are social processes which are zeitgebers) and reduce inflammation (typically a product of suppressed immunity or damaged gut barrier, probably mostly due to nutrient deficiencies). But food availability is highly environment-dependent and learning processes are needed to discover what food sources are available in the current environment. When a food source is discovered, the brain learns to exploit it more fully. Flavor-calorie associations serve to motivate the person to go back and look again for more food of the type that was recently available (which makes sense as this is the most likely to be available now). Of course in our ancestral environment, all food was nourishing and healthful.
In our modern environment people have a bad status all the time, motivating the brain to seek food; and they establish flavor-calorie associations that promote appetite and seeking of unhealthy foods. Disrupting these flavor-calorie associations, leaving the brain confused about how to find food, resets appetite to a lower state, leading to a reduced weight.
So my guess is, flavor-calorie associations don’t explain much of the success of PHD, but PHD may lead to a lapse of past flavor-calorie associations. One status is optimized, there is no need to seek food, no appetite, and the brain will probably forget its flavor-calorie associations before long. So I would think the Shangri-La Diet might not add any value to someone who has already fully implemented PHD. Of course the existence of cravings would indicate that the Shangri-La approach would add value.
Thanks for the thoughtful reply, Paul. I agree with what you say, but being a physiological psychologist, I think most folks underestimate the dramatic role the nervous system plays in trying to predict the future to optimize homeostasis. Flavor-calorie associations are developed through the process of Pavlovian conditioning. If those calories (the Unconditioned stimulus or US) are very large, and if the flavors (conditioned stimuli or CSs) are very salient, this sets the stage for very strong flavor-calorie associations. If consuming supernormal flavors that have strong associations to large calorie USs increases the set point well above what is needed, then the body’s homeostatic physiological mechanisms will defend this artificially inflated set point. The way it does this is through the regulation of appetite, increasing appetite to a level that drives the individual to pursue the consumption of foods to achieve the set point. Diets like the PHD and the SLD break this artificially-high set point and bring it back down to a more healthy level by breaking the flavor-calorie associations. As Pavlov himself recognized a century ago, and is still in strong evidence in the learning data today, is that once established, it is virtually impossible to permanently eliminate an association once it has been formed. Extinguished associations spontaneously recover, renew when the individual finds themselves in a new context, or can relapse due to exposure to the extinguished CS (or US). Thus, even when successful, I suspect that someone who was “addicted to food” (loosely speaking) will always have latent associations to those foods and their flavors that could lead to relapse at any time. Maintaining a PHD will go a long way towards preventing this, but the moments of temptation could still ignite binge eating and a fall-back to old habits. But as you say, I think we psychologists and behavioral neuroscientists are just beginning to probe these processes in weight and appetite regulation, and much good empirical work remains to be done on this front. I’ve taken up the clarion call to take this effort into my own lab, and some of my colleagues are doing the same. I’m about to resubmit a grant proposal to NIH to fund this kind of work, but it’s a very difficult funding situation in the US right now, with fewer than 10% of all applications getting funded. As I tell my friends, it’s like trying to play a game of poker among professionals, followed by a Craps shoot. Nevertheless, I will continue to persevere, lest I give up hope and let the food manufacturers take over the entire culinary world.
Good luck getting funded. Shou-Ching is in the same situation, in cancer research and vascular biology, where funding rates are even lower. Recent study sections in her field have funded 1 of 80 proposals. It’s tough.
Hmmm… I read that book. While I think Seth Roberts was well intentioned I don’t really thinking flavorless calories in the form of oil cause weight loss. What I do believe is what Stephan Guyenet says that has a PHD. He cites some of Seth Robert’s ideas but states that long term general good palitability increases or decreases set point weight. That I do believe and I think a simplistic diet away from salt, added sugar, and fat (low reward foods) not oil and sugar WILL decease set point if sustained for the long term.
My doctor wants me to try a Very Low Calorie Diet to get most of this weight off. I’m approx. 60 pounds overweight, pre-diabetic. Meal replacement with one small protein meal a day. She would monitor me every week and has taken bloodwork and EKG. I, of course, want to lose the weight, but I’m afraid of some of the side effects–anxiety, hair loss. That seems wrong. Although the research I’ve read said these are excellent at stabilizing blood sugar levels. Do you think these are safe? What can I do to keep my hair from falling out?
Hi Jenny,
That is wrong. Such extreme diets have been used to good effect in diabetics, but only with enough protein and carbohydrate to prevent those starvation effects.
No, I don’t think starvation diets are safe. I would do PHD with intermittent fasting.
To stop your hair from falling out, eat 600 carb calories and 300 protein calories per day, plus adequate micronutrition, such as iodine and selenium.
Best, Paul
Paul, I still lose hair even on 600 carbs and 300 protein calories a day. The primary factor for that is more the thyroid status than anything else. There is no way extreme calorie restriction diets do not suppress the thyroid.
It would behoove you to start tracking the armpit temperatures and/or TSH levels of all your retreat participants so correlations between body weight, calorie intake and set points could be inferred.
Hi MG, yes, I agree that thyroid status is paramount. We ask for numbers from retreat participants but we don’t want to turn the retreats into a medical visit, so we don’t do measurements ourselves. Maybe we should change that. I’m thinking we may introduce QS devices to the retreat for tracking.
Hello Paul,
Not sure if you are still updating blogs or responding to comments. I sure do hope so though. I ran into your book by accident and started reading it.
Wow what an amazing written book.
I created my diet originally based on nutrient density more than anything else and what traditionally ate as a kid; being Hispanic from Colombian pre north American way of eating.
After reading your book is so crazy how many other cultures were eating super healthy until they started the American pyramid scheme i mean food pyramid.
Also it makes so much sense now why Hispanics pre American food invasion actually had such a low incidence of obesity, heart and diabetic diseases and we ate pretty close to the PHD lifestyle.
I’m trying to make some modification based on the new information that i learned.
My current Goals are: Loose body fat, gain muscle/strength.
I currently am doing a heavy weightlifting workout fasted in the morning (1hr) 5 days week and than extra light walking, light yoga and bike riding here and there.
I calculated appx total calories i need to consume based on my weight and Body fat % plus approximate amount of hours per week I will workout. Total calories are 2043.
Since i am trying to loose fat i went on a 19% deficit bringing me down to 1655 total Calories. (28%) Protein: 456 (29%)CARBS: 484 (43%)FATS: 715.
But after reading the book and reading some comments is it better off to stay at a regular calories 2043 and stick to same amount of protein 456 kcal, but bring my Carbs to 600 kcal and the rest fats?
Hi Cristian,
Thank you. Yes, I think you should eat to appetite. Once you are well nourished your body will realize it has too much weight and will suppress appetite naturally. Carbs of 600 kcal per day is a good target.
Best, Paul
Thanks, Paul. I came to my senses about this. Seems too extreme for me. When I got my blood work back I noticed: elevated wbc (14.7 mine, high is 11)
Absolute Neutrophils (10 mine, high 6)
Absolute Monocytes (1.1 mine, high 2)
My wbc are usually high and my CO2 is usually low. What type of infection should I be looking for?
Hi Jenny,
You need a doctor to evaluate this. This can have multiple causes. See http://en.wikipedia.org/wiki/Neutrophilia.
Hi Jenny, Paul just had a baby, so I’ll chime in (not on his behalf, just according to what has been written on the site, and from the book)
There are a lot of essential nutrients which are crucial in weight loss- Choline, Iodine, Selenium, Zinc, Magnesium, Vitamins B1, B2, C, D, E, B5, B6, B12, K2, Retinol – the list goes on and on. There are others science could have missed, like bone matrix, collagen, gelatin.
With that in mind, I think that Perfect Health Dieters fighting obesity strive to do a couple of things:
1) CIRCADIAN RHYTHM ENTRAINMENT. THIS IS SO IMPORTANT AND CANNOT BE STRESSED ENOUGH – YOU NEED TO SLEEP AND EAT AND PROBABLY MOVE YOUR BODY AT THE SAME TIMES EVERY DAY. FOR THE REST OF YOUR LIFE.
2) it’s advised that people nourish themselves as well as possible with food- things like bone broth, egg yolks, and sea foods, like iodine and salmon, even dark chocolate – which are all very nutrient dense. (For bone broth, BTW, you take bones, stick em in water, bring the water to a boil, and then leave the thing simmering, overnight, 2 days, whatever you want).
3) Fight any infections which could be present and preventing you from making progress – this could include known or unknown infections. H Pylori, Parasitic infections, fungal infections, or simply dysbiosis from too little beneficial bacteria.
Strategies against infections could include confining food intake to 8 or 9 hours a day, including probiotic foods like Kim-Chi, or taking medication to address the issues (such as an anti-parasitic drug or antibiotics), keeping in mind that stool tests (your regular doctor can probably do the H Pylori antigen test, and you would need to see a functional doctor for Doctor’s Data, Metametrix stool and urine tests)
4) Then, to cover your bases a little more in the midst of all of the above, you take vitamins and minerals to make sure you’re in the correct range – not too much, not too little – of every known nutrient the body could possibly need.
I would advise you to watch Paul’s talk on obesity here:
http://perfecthealthdiet.com/2014/08/ancestral-health-symposium-tak-weight-loss/
Obesity is a multifactorial problem, as Paul shows. PHD is the only thing that attacks the problem from multiple fronts, giving obesity the respect it deserves. Your doctor is, to paraphrase something I recently heard, bringing a butter knife to a gun fight.
Also, note that the study on people trying to restrict calories and move more (which is what your doctor is trying to do, correct) – shut down, possibly because the participants they were encouraging to do this were NOT SUCCESSFUL:
http://perfecthealthdiet.com/2012/10/look-ahead-scientists-trying-to-move-the-deer-crossing/
Eating less and moving more is successful against cardiovascular disease, NOT obesity.
Good luck! It’s a lot of information out there, but it is very helpful and healthful. You’re not losing weight, YOU ARE GAINING HEALTH, which is the main thing to focus on.
Thank you Lyn! Great summary.
Hi Paul,
No disrespect intended. Most people know that the fatter you are the quicker you lose weight on pretty much any weight loss diet. And anyone who has dieted also knows that as your time on the diet progresses your weight loss slows, especially for the last 10 pounds. I don’t see how what you are observing differs from this common knowledge. Am I missing something?
Yes. You’re missing first of all that these diets were not calorie restricted. So they weren’t obviously “weight loss diets.” Also you’re missing the consistency of the weight loss, and its persistence. The general experience is that people on “weight loss diets” experience plateaus and yo-yo weight regains. Also larger variations in individual response.
I believe the PHD does a much better job of addressing the many factors contributing to obesity than most approaches. However, I don’t understand how you can claim a setpoint normalization over the course of a few days.
I’m much more a supporter than skeptic, and you have already mentioned the need for more data, but without that data I don’t see how this claim could even be made.
Heavier people losing more weight and lighter people losing less weight might support the idea of a setpoint, but not the PHD itself.
The PHD may lead to inadvertent caloric restriction compared to the SAD or a participants previous dietary habits.
“I’ll speculate that intentional calorie restriction may lower the set point by a few BMI points, say from 24.4 to 21.7”,</i.
This more supports the notion that when he dieted under his set point he wasn't comfortable, and returned to it when he ate adequate calories. Not that his set point ever changed. Not that caloric restriction changed where his body was most comfortable.
I believe to truly support setpoint you would also need data from underweight participants.
At this point, I think the best you can say is that the PHD supports a trend toward the setpoint, not that it regulates or changes the set point itself.
Hi Roddy,
The logic is very simple. If you buy that the pressure to lose weight is proportional to the distance from the setpoint, then the intersection of the fitted line with the axis of zero weight loss tells you where the set point is.
We have had underweight participants and they gained weight. So that too supports setpoint normalization on PHD.
It’s also obvious that PHD changed the set point. If it didn’t, their weight would not have changed.
Thanks for the response, Paul.
My understanding is that they could have been maintaining a weight outside of their setpoint. The PHD doesn’t necessarily change the setpoint, it just could help them return to it where they’re body is most comfortable.
If the PHD does, in fact, normalize the set point, I think it would be hard to gather data to confirm it is done within a few days.
I don’t think anyone is missing that the PHD isn’t necessarily a calorie restricted, that’s why I mentioned inadvertent caloric restriction by putting restrictions on certain types of food and increasing the amount of others. Not to mention, in some cases there was purposeful caloric restriction.
In Jay’s case, restricting as low as 1200 (which is close to a starvation diet) did not halt his progress, but that is well below the healthy amount for any man – particularly someone his size.
The consistent weight loss is promising, but they haven’t necessarily had time to yo-yo yet (and I’m hoping they don’t) but there are many cases from various diets with rather consistent weight loss over months at a time, with an eventual regain.
If I recall correctly, there’s some data to suggest weight loss is rarely sustained over 5 years. Longitudinal data will help to support the case.
“I don’t understand how you can claim a setpoint normalization over the course of a few days.
I’m much more a supporter than skeptic, and you have already mentioned the need for more data, but without that data I don’t see how this claim could even be made” – Roddy
I second Roddy’s sentiment.
A set-point, if we abide by the definition of the Harvard Medical School Teaching Hospital’s, is simply “Your body weight set point is the number on the scale your weight normally hovers around, give or take a few pounds.” Hence, it is a simple statistical average of empirical observations over a certain period of time – not a defined biochemical/physiological state producing a specific phenotype.
I think Harvard’s definition of set-point is pretty useless – why not just call it your weight (or average) weight? (over a defined time period)
Alternatively, we could also say that deviating above from one’s initial set-point makes getting back down to it more difficult the closer one gets. We’re reversing the negative changes first responsible for the deviation. Why does it slow down the more weight is lost? Maybe because ‘building back our normal biochemistry’ is harder than ‘destroying our normal biochemistry’. And building it back up to exactly like it was before (closer to set-point) is harder.
A set-point, if we abide by the definition of the Harvard Medical School Teaching Hospital’s, is simply “Your body weight set point is the number on the scale your weight normally hovers around, give or take a few pounds.” Hence, it is a simple statistical average of empirical observations over a certain period of time – not a defined biochemical/physiological state producing a specific phenotype.
I think Harvard’s definition of set-point is pretty useless – why not just call it you weight (or average) weight? (over a defined time period)
Regardless, congratulations for your results Paul & Sou-Ching!
According to the definition you have quoted, a set point is not a “mere statistical average of measurements”; rather, it is a “stabilized weight”. It is a weight “around which” the body tends to “want” to close in on, give or take a few pounds. So, it is a teleological notion. It invokes what Aristotle called “final causality”.
In any case, simply because Harvard or a dictionary or an institution defines “set point” in such and such a way doesn’t mean that such a definition is accurate as a representation of how psychologists are thinking about this concept. One can define a word however one chooses, but it doesn’t follow that the resulting definition will actually correspond to the actual meaning people intend to convey when they typically use that word. One actually has to think about how people, the actual practitioners, are thinking about the concept. Moreover, if adopting their definition leads us to interpret the practitioners in uncharitable ways, then the definition is probably wrong or at least incomplete.
As psychologists understand it, a “set point” is a telos-weight set by the mind-brain in the context of a homeostatic mechanism. Such a notion is not pedestrian. In fact, the notion is an unclear and indistinct idea that arises from a confusion of categories, specifically, the confusion of the bio-teleological sphere (which pertains to living things) with the human-designed-artifactual sphere (which pertains to a certain kind of non-living thing, namely, artifacts). And this confusion is combined with conceptual misunderstandings surrounding the nature of the human being, psyche, mind and brain.
The result is a compound conceptual confusion, which forms the basis of a conceptually confused theory in psychology that is connected with interesting and important experimental data and sound thinking on the part of accomplished scientists, doing important scientific work.
Our culture must abandon the idea that accomplished scientists are immune from talking nonsense. Scientists are no less likely to talk nonsense than anyone else, since nonsense arises from a lack of clarity regarding categories, which are sorted out in the activity, not of science, but of Western philosophy, e.g., the work of Aristotle. Science discovers truth, but scientists often package important facts and truths and discoveries in nonsensical descriptions that are grounded in conceptually incoherent notions. Our task is then to re-describe the scientific achievements or hypotheses without conceptual confusion.
In the above case, this can be accomplished by framing the hypothesis as follows: a healthy person, or a person who takes on healthy behaviors, tends towards a non-obese weight, and an unhealthy person, or a person who is engaged in unhealthy behaviors, will tend to retain excess weight; perhaps such a person will remain at a stable obese weight for long stretches of time; but this will not be their natural weight. — Or, rather: a flourishing physiology (defined by what is naturally historically optimal or normal) tends towards a non-obese weight; and a physiology that is not flourishing may not do this, whether their weight stabilizes around some obese number or is perpetually changing.
We can also say that it has been observed that a person exposed to abnormal conditions, conditions that break the normal connection between a person’s sensory experience and their act of consuming food, will sometimes lose weight. And future neuroscientists may one day be able to describe the neural-processes that are correlated with this curious phenomenon. But that’s it.
For, it is conceptually confused to try to explain all of this by saying that “the mind-brain, by means of a computational program that takes into account relations between flavors and calories, sets a new set-point, when it cannot taste or see or smell the calories any longer.”
“As psychologists understand it…” ==> nope, sorry, not interested in what past/current psychology have to offer on the subject of weight-loss (of course, there are always exceptional people in any field).
Your treatise on science is not unwelcome but completely irrelevant to the point I (& maybe Roddy) were attempting to make.
Maybe Paul & Sou-Ching have started to gather evidence of a preferred modus operandi for weight-loss protocols. However, the complex & over-extrapolated use of the term set-point does benefit our understanding of weight-loss mechanics. It is redundant.
Yes. The possibility of appropriating the notion of the “set point” as it is understood in current psychological research on obesity is the premise of the above article.
To say that “the room cooled down because the set point of the thermostat was lowered by a person” is not redundant.
But, when we say that “the body sheds weight because the weight-set-point was lowered (by the homunculus)”, this does ultimately strike us as redundant. But why? What accounts for the difference in the two cases?
I believe the answer is as follows: talk of a “set point” in the bio-teleological realm is clearly a metaphor that arises from thinking of a homeostatic bio-phenomenon in the biological sphere as if it were a designed-homeostatic mechanism in the artifactual sphere. That is, talk of a set point stems from drawing an analogy between the biological and the artifactual.
But, if we drop the analogy (i.e., the metaphor), which we must of course be willing to do, if we seek of clarity and distinctness in our understanding of things, then I think you are right that we are left with a redundancy, a mere tautology. For, literally speaking, there is no literal homunculus who is operating a literally extrinsically-designed-mechanism and who is thereby controlling a set point (in our heads).
And, this means that once we drop the metaphor, all we are really able to say is that “the body sheds weight because the body tends towards a new weight”—And you are correct that that is tautological.
Wittgenstein distinguishes between “nonsense” and “senselessness”. “Nonsense” is incoherence. Whereas to say something that is “senseless” is to say something tautological (but not incoherent (i.e., nonsenseical)). (Gary Taubes for example, uses the word ‘nonsense’ to mean ‘senseless’ in this Wittgensteinian sense, when he says, e.g., that it is “nonsense” to say that “the body loses weight because it sheds more pounds than it retains”.)
So, we can say that the set-point theory is either “nonsensical”, when taken literally; or it is “senseless” when the metaphor is dropped. In other words, we can say that the set point theory faces a dilemma.
Or, we can say that the “set point theory” is not a theory at all; it is not something that purports to be an “explanation” of anything; for, it is simply a picturesque “description” of a phenomenon, which we are attempting to explain, a phenomenon that stands in need of an explanatory theory. In other words, it is simply a fanciful “description” that makes use of a simile, in which a biological phenomenon is figuratively compared to a human-designed homeostatic mechanism. This description allows us to paint a colourful picture of an observed phenomenon: namely, the phenomenon in which a body moves from one stabilized weight to another stabilized weight.
But the problem is, why does this happen? For, we need an understanding of the “efficient causal” processes that leads to the change from one stabilized weight to another stabilized weight.
We are told this change might happen if (1) a person goes without sufficient food for long periods of time; if (2) the food one is exposed to is so bland that one doesn’t want to eat it and thereby ends up restricting calories; if (3) under experimental conditions, one is deprived of sensory contact with one’s food; for, this leads to a disruption of normal and healthy neurological function, which results in various changes to one’s physiology, which for whatever reason result in a reduced calorie intake.
However, the Perfect Health Diet explanation, which seems quite plausible, is that this change can happen if (4) a body is healthy or exposed to health promoting stimuli—regardless of how delicious or gourmet one’s food is.
Of course, (1)-(3) would hardly be of any interest to someone who simply wants to be lean AND live a normal and healthy life AND who wants weight loss that is sustainable and permanent.
Indeed, (4) is what one might call “the realistic approach”.
As one who lost weight on the PHD retreat, and has kept it off since, I would agree that the PHD lifestyle affects the set point, but I’m not sure it “normalizes” it completely to what it should be. If it did, then my body would tend to rush towards that new set point right away, which it doesn’t. I still need to work hard at it (and I evidently haven’t been working hard enough at it since my last PHD retreat, since I’m still at a plateau). However I’ve experienced something new this time that I have not experienced in past weight loss attempts, which is that my weight didn’t climb back up to my old set point after I lost it. Which tells me that my set point was adjusted. But I think it was adjusted down by the number of pounds I lost, not “normalized” to where it should be. So I think you need to nuance the way you describe what happens to the set point.
Hi Rosie,
There is certainly a lot we still have to learn. They may be male-female differences, so far the only cases who have reported this exponential weight loss pattern are men. We’ll figure it out in time.
Hi Paul,
My wife and I have been on PHD since April 2013. I’ve lost 21 lbs. and she’s lost more (maybe 32?), which is unusual. I usually lose faster—and she’s postmenopausal. Would it be helpful to you if we posted that data somewhere? We have charts by date which include body fat, water, muscle, and bone. I could summarize by week or month.
Hi Joseph,
Yes, I’d be delighted to see the data. You can email it to me. pauljaminet@perfecthealthdiet.com
Best, Paul
In the past few years I was low carb for 12 years and lost about 20 lbs with lots of ups and downs. This was followed by VLC for a couple of years losing another 20 lbs, becoming fairly unwell in the process. This past 5 months on PHD lost the last 10 lbs (or so) effortlessly and regaining excellent health. My weight has so easily “normalized” at a weight I haven’t been at for almost 30 years. I’m 62. PHD seems to be the set point and good health key for me.
Great news Roz! Thanks for sharing.
I wonder what kind of an effect serving soaked legumes at the retreat would have. Personally, I find chickpeas and lentils to be very satisfying — in some ways even uniquely satiating compared to any other food. Clearly legumes would provide a lot of fuel for the microbiome, and since the PHD surely improves the microbiome of the average person over time, I also wonder if the legumes could make this shift occur more rapidly, or if it may be more optimal to introduce them only once the quality of the microbiome has already improved.
Of course this is all presuming that someone might be so inclined to include legumes in their diet in the first place, though arguably they may be able to offer some agreeable variety, I understand not everyone has an interest in them.
Great post.
It could be beneficial, but we haven’t gone there yet. The retreats are about teaching a convenient way of life people can implement back home; and I don’t think the soaking and cooking regimen for beans is convenient.
I’ll second Carl’s pro-legume vote due solely to their deliciousness. I miss legumes very much and gluten not at all. Overnight soaking and then cooking (especially pressure cooking) seems easy enough.
What I usually do is cook up a big batch containing 500 g of chickpeas/lentils/beans (probably would do even more if I had bigger pots!), and whatever I don’t eat right away that day, I then let cool and subsequently package into 6 or so ziploc bags for individual portions that I put into the freezer.
At that point they’re as convenient to warm up for a meal as frozen peas.
I like the individual-serving-freezer-bag idea. Also, per America’s Test Kitchen, black beans need only cook for 10 minutes on low pressure (followed by natural pressure release) after an overnight soak in salty water. Another tip, which I haven’t tried yet, is coating the beans in oil before adding water to the pressure cooker to prevent foaming.
About a year ago, I switched to a 12-hour light-dark “equatorial” schedule (and kept everything the else— diet, exercise, etc.— the same); in 6 months, my BMI went from 21 to 20, and it has, to this day, normalized at around 20. This roughly accords with what is predicted by your understanding of the rate of healthy weight loss.
I would guess that, strategically speaking, fixing one’s circadian rhythms should take priority over the implementation of intermittent fasting. For, the important thing, it seems, is that one eats food within the 12-hour light-period. And once one gets accustomed to this, one will probably automatically tend towards a fasting window of 14 hours, and perhaps sometimes 16 or more hours, depending on how one feels. But 14 is what I tend towards, for the most part.
Wittgenstein wrote that the “The confusion and bareness of psychology is not to be explained by calling it a “young science”; its state is not comparable with that of physics, for instance, in its beginnings. (Rather with that of certain branches of mathematics. Set theory.) For in psychology there are experimental methods and “conceptual confusion”. (As in the other case conceptual confusion and methods of proof.) — The existence of the experimental method makes us think we have the means of solving the problems which trouble us; though problem and method pass one another by.”
I would like briefly to make some conceptual remarks concerning the notion of a “set-point”, which is said to be “useful” to psychologists who research obesity.
The notion of a set-point is a metaphor: for this reason, it might be helpful to remind ourselves of what it would mean were the notion to be literally construed: literally construed, a set-point is a telos in a homeostatic artifactual-mechanism designed by human beings; as a goal, the set point is determined “extrinsically” by the person setting the set-point. Also, the purpose of setting the set-point to whatever point at which it is set, is also defined extrinsically. So, the concept of a “set-point”, literally construed, belongs to the artifactual order of things. It belongs to the realm of human culture.
By contrast, the concept of a “normal weight” or “natural weight” or “healthy weight” belongs to the bio-teleological order of things. A healthy person tends (naturally and bio-teleologically) towards their normal or natural weight (and the “goodness” or “rightness” or “appropriateness” of this “tending towards this end” is intrinsic). The attainment of the normal weight is an intrinsic goal of the physiological processes of the organism, given that the attainment of the normal or natural weight contributes to the flourishing of the organism—the end of flourishing being an intrinsic good in light of which the processes and functions of organisms must be made intelligible. (Biological organisms are neither machines nor physical objects.)
Obese people do not have an “obese weight” that their physiology aims towards intrinsically. For, an “obese weight” is not an intrinsic good or goal. (Also, I’ve heard that the obese tend to become more obese over time.)
That a human being might lose weight when subjected to abnormal environmental conditions, e.g., in which they cannot taste their food or in which they cannot see their food or in which they cannot smell their food, is perhaps a curiosity. But it should not and cannot be the basis for positing existence of a homeostatic-artifactual-mechanism in the “mind-brain” (since the notion of such as thing is conceptually incoherent). For, there is no such thing as the “mind-brain” and, as a matter of conceptual coherence, there can be no such (literal) thing as a “set-point” “in the brain” or “in the mind”.
Additionally, there is and can be no such thing, conceptually speaking, as a “flavor-calorie association” “made by the brain”. And, as a matter of empirical fact, a person typically will not associate a flavor with a quantity of calories! Moreover, food cannot be “formally causally” defined as “calories”. All one can say is that there are calories in food.
We must distinguish sharply the human motivation to eat delicious or gourmet or healthy meals (with their wonderful tastes, colours, aromas, textures) from the neural-structures in the brain that physiologically underpin this human-animal psychological disposition, as well as from the neurological processes that are correlated with the actualization of this human-animal psychological disposition.
The brain is not and could not be a computer that oversees a homeostatic body-fat regulation mechanism, carrying out operations such as “the setting a “set-point””, since a computer is defined as a symbolic-information processor, and there can be no symbols in the brain, unless we extrinsically regard the brain as containing them.
Thank you for the interesting discussion. However, I feel that the definition of set point is taking us away from the objections with saying it has been “reset” in a couple of days. By certain definitions, it’s overstated. By other’s, it’s less than impressive or too earl to tell.
We’re seeing the rate of loss decreasing as people get close to a healthy weight… that doesn’t say much.
Stable losses (in some cases) great, but again, not exactly unique.
Permanent losses? Too early to tell.
I think his view is that the physiology of the non-diabetic obese is in perfectly good shape. And so, if you provide the right “inputs” (food, light, exercise, etc.), the homeostatic bio-systems will instantly start to work as they are designed to work, and this will result in the person being on track to lose weight according to the above pattern.
I’m going to have to pick up that book. I’ve most weight before and gained it back. This time on a paleo diet I don’t want to ever gain it back again.
Paul,
Thanks for the interesting post. I had the body weight “set point” – losing 10% weight (about 1 lb/week) over 5 months, then a 6 month pause, then losing 5% from the new setpoint (about .5 lb/week) over the next 5 months. (to reach a BMI around 22.5)
Since my weight bottomed out a year ago, I have been closer to a BMI of 23. (adding in more fat with foods like dark chocolate and coconut oil)
2 observations:
-adding in more fat, HDL and Trgs remained about the same but raised LDL, total cholesterol went from 155 to 200 (LDL went from 90 to 135)
-this is hard to describe, but at the lower weight I had a “buzzed” feeling most of the time, maybe I was in ketosis (I did not measure ketones) or perhaps this is typical when a person reaches the end of weight loss
Unfortunately, weight and cholesterol are the only data I have to compare. Is there any way to know which one is the preferable state of health?
Hi David,
Yes. Your LDL was depressed before and is normal now. See our cholesterol category, http://perfecthealthdiet.com/category/biomarkers/hdlldlcholesterol/, for relevant posts.
So your numbers are better now. You don’t want to be underweight, or low in cholesterol.
Paul,
Great, thanks for the info.
If we remove the phrase “set-point” and try to do justice to the hypothesis, we might say, “increased flourishing of the various biological-homeostatic systems in a living organism (in light of some natural-historical ideal of what it would mean for the homeostatic bio-systems to flourish optimally or normally)—brought about by the recommended changes to diet and lifestyle—leads to predicable changes in weight, over a time-period, in which one moves from an unnatural weight towards a natural weight, in accordance with the above pattern, and this increased flourishing of the homeostatic systems occurs within days of making the recommended changes.”
I’m trying intermittent fasting and trying to figure out some logistics.
If limiting food intake to a span of 8 hrs, how are folks getting:
1) 3 servings of fruit worked in without eating them close to meals, since not I’d eal for digestion?
2) all the recommended quantities ( lb ea of protein, starchy, non-starchy, sweet) in just 2 meals, or are people eating a 3rd meal at 4 hrs?
3) when do you eat chocolate?
Also, what brands of 70%+ dark chocolate are people finding that is healthiest? Is raw best? And if not 100%, what sweeteners are in them. All the ones I’ve seen are cane sugar, coconut palm sugar or agave. I usually get the highest % chocolate sweetened with coconut sugar that’s available, but is that the healthiest?
Thanks!
Hi Susan,
I eat 2 meals with the IF. Before I would eat just after I woke up, out of habit. With PHD, I am no longer hungry then so the first meal is closer to noon. Usually full fat organic yogurt, raw almonds, pumpkin seeds and hard-boiled eggs (from pasture raised chickens) Later I typically have fruit (usually banana and blueberries) with almond butter. Dinner may be a small serving of meat/protein with safe starch(es) and vegetables. Then cheese and dark chocolate for dessert.
I go with the higher % dark chocolate, it has less less sugar. I put the sugar content for some of the brands I have bought-
Endangered Species 88%, 10 g sugar/3oz
Taza 87%, 10 g sugar/3 oz
Alter Eco 85%, 12 g sugar/3 oz
Lake Champlain 70%, 22 g sugar/3 oz
Hi David,
Thanks for the great info about your IF food day. I was trying to follow Paul’s recommendations to the letter re ~1 lb. ea of the 4 food categories while IFing, but it looks like others are modifying/reducing those quantities to fit into the 8 hr window. Maybe the target quantities for IF are actually closer to 2/3 of the std recommendations since it’s two meals, not three. In your case, it looks like maybe even a lot less than that (?) since protein (other than eggs), veg and safe starch are at dinner only. I’ve eaten 3 eggs midday for awhile too, but with lots of veg and safe starch.
I LOVE nuts too (!!!), which I still eat, but in lower quantities so that I can fit in the other foods in that he recommends, while still fitting in my pants 🙂
Or maybe the assumption is that most people on IF are trying to lose weight, so reducing calories by 1/4-1/3 is appropriate. But In my case, my weight is close to optimal (5’5″ 118), so that’s not my reason; rather it’s to kill off bad bugs, improve my CRs and overall health. (Truthfully, I’d prefer eating in a wider window, and probably still would be if I wasn’t dealing with a few gut and other health issues.)
On the chocolate, those are great recs and I’ll try them. The ones that I’ve found and like are all raw and organic and only sweetened with coconut nectar/sugar, most with <5g sugar per oz: Gnosis 90%, Santosha 85% and Lucy's 88%, but they can be hard to locate and I'm often looking for other options. BTW, Gnosis also makes an 85% sweetened only with stevia leaf, but the taste is a little "off" IMHO. I've heard great things about Taza but haven't located the 87% yet.
Thanks,
Susan
Susan,
Besides eggs at lunch and meat at dinner, other foods that I listed have some protein- like the almond butter, raw almonds, yogurt and cheese. It may be helpful to track the food you are eating for a few days and record the grams of fat-protein-carbs to get a starting point. I typically only have starches at dinner time, 1 or 2 servings.
Thanks for adding that David. Agreed, definitely some protein in there. I guess I was thinking of protein in the context of the PHD “apple” chart where nuts and dairy were in the class “pleasure foods” thus excluded from the “.5-1lb of meat, fish and eggs” category. Since going PHD I’ve begun to think of nuts and full-fat dairy as being more in the carb and fat categories, though of course they do contain some protein too.
Lindt 90% is one of the smoothest dark chocolates. Better than most higher sugar chocolates.
TR,
Thanks for that! I’ll try it! I’ve come to prefer very dark while on PHD. See my reply to David for some good ones that are close to 90%. Probably not quite as smooth as Lindt though because they are raw, organic and mostly only contain cacao and coconut nectar/sugar.
Thanks,
Susan
ps There’s an “underground” shop in Palo Alto called “chocolate garage” and its owner travels the world seeking amazing chocolate from all corners, mostly dark, and holds tastings and sells it. Very fun if you’re ever in this neck of the woods!
Hi Susan,
My wife and I eat three meals within the IF window—one every four hours. I could eat just two, but my wife can’t eat meals that large and still get the recommended 1 lb. safe starch—and for us it’s critical that we do. After eating VLC for years and suffering all the consequences of it, we are careful to get enough carbs. If we don’t get the full 1 lb., my wife’s arthritis acts up and both of us have problems with thyroid and high LDL, dry eyes, headaches, etc.
We usually have eggs for breakfast with 5 oz. cooked rice, yucca, tapioca, sweet potatoes or plantains, with 4 oz. fruit for dessert. Lunch is often a salad with cold, leftover meats and cold potatoes or taro (5 oz.) with 4 oz. fruit for dessert. Dinner is often soup with rice, potato, or taro boiled (5 oz.) with whatever meat is up. We rotate depending on the day to make sure we get some of everything. Yesterday was oily fish day. Today is bird day. Fruit for dessert again. I eat 4 oz. cooked protein/meal, my wife 3 oz. She also sometimes waits before eating the fruit if she’s too full. We only eat 4 oz. fruit because we eat veggies at every meal, some of which are often sugary veggies like carrots or onions. We also try to eat some raw veggies at every meal. We try to eat our last meal before sunset, but often get a late start. Sometimes we eat a snack before dinner with rice crackers, cheese, maybe some nori. We figure that gives us wiggle room with the extra ounce of carbs. Also, the inevitable restaurant meal is a mystery. We tend to under eat restaurant food because it’s often not very good compared to what we make at home.
My wife is off chocolate for the moment due to GERD problems, but I generally eat 85% chocolate from Trader Joe’s. Don’t remember the name—something French.
Hope this helps, I was confused when I first started PHD. I think eating VLC for so long made us afraid to eat the full lb. of starches, but the fear was groundless. We’ve been eating a pound/day of starches for at least a year, and have still continued to lose weight.
I find the IF to be very important. When I strayed from it due to my wife’s GERD problems and her need to spread out the meals more, I got colds. Since doing IF, I haven’t been sick.
Circadian rhythms, however, are a constant struggle. It’s very hard to turn off the TV every night, but doing so provides so many benefits. I start to have skin problems and stiff joints/neck due to hypothyroidism when I stay up late watching TV too many nights.
Hope this helps, and good luck to you!
Joseph,
Thanks for describing in detail how you achieve IF and covering so many bases — extremely helpful input as I experiment and try to make it work for me! What you’re describing is basically what I was doing daily, but in a 10-12 hour eating window. So I liked hearing how it could morph into an IF schedule with a few mods. Like your wife, I’m finding that I feel better on 3 meals, though one is often a smaller one. I find the starch very important too, probably because I share similar conditions and issues with you both. As a lifelong night owl, CRE is the biggest challenge for me too!
Thanks again for being so generous!
Dear Paul, what is “TAU” in simple terms?
maybe what it corrects is leptin resistance.
if leptin resistance fools the brain into seeing less fat than there is, perhaps it is defending the lower false weight. with a correction to the leptin resistance maybe it suddenly “sees” the real weight and adjusts to cause weight loss to the set point, which actually never changed, as far as the brain was concerned.
just a possible theory, anyway.
is there some cause of leptin resistancethat could be fixed so qjickly? cortisol/stress rezponse comes to mind.
That is an interesting thought, makes me wish I had my leptin tested before starting PHD, to have a comparison
If doing intermittent fasting (specifically to starve bad bugs and also for CRE and good health) is it best to restrict all vitamins, amino acids and supplements to the 8 hour window? And is it more important with some more than others?
Vitamins: B’s, C, D3, E, MK-7
Minerals: Magnesium, Taurine, Chromium, Boron, Zinc, etc
Others: NAC, Lysine, L- Theanine
As I understand it it’s important to avoid calories while fasting. I eat two meals between 11-7 daily. Outside that I drink black coffee in the morning and drink broth if I have it, or water with a little sea salt for electrolytes. I don’t see any harm in taking supplements while fasting.
Thanks, yes I’m clear on calorie restriction. I’m asking only about vitamins, minerals, supplements because I recall reading in the PHD book that some (not all) of them can feed bad bacteria/pathogens. (I thought that was one reason they recommended taking some of them only once per week or once per month vs. daily.)
Many of them I take daily or in higher doses because of immunity and nutrient issues/deficiencies identified in testing. Plus some, like C, lysine and NAC multiple times per day, so I’d normally take them over a wider window than 8 hrs, but if it compromises maximum pathogen die-off in any way, then I wouldn’t want to do that. (I have SIBO, IBS dysbiosis and a skin condition, so my primary motive to do IF is for accelerated pathogen die-off.)
If anyone has input on this I’m all ears.
Several weeks ago, I finished reading the PHD book and I’ve been incorporating the details into the new lifestyle and so far, so good. So, this recent article I find very interesting.
If I can summarize, you are saying that what makes PHD unique is the weight loss without calorie restriction, which resets the body weight set point. I guess I am left wondering how you can know that so soon since isn’t the true test of a lowered setpoint determined over a longer period of time?
Before this article, I was relying on Chris Kresser’s statements that bariatric surgery is the only proven method for defeating the defended level of body fat, over time.
I’ve cut and pasted some comments from his blog. I would appreciate you have any thoughts on what he says – and whether PHD would accomplish this via the same (or similar) mechanisms.
“So, people who have had gastric bypass, on average, they lose about 60% of the excess body weight that they were carrying — at least, morbidly obese people do, and those are the ones who generally have this surgery. And in contrast to calorie restriction and other weight loss programs, the bariatric surgery causes a reduction in hunger and reduced cravings for energy-dense foods, and it doesn’t cause any change in circulating thyroid hormones that would suggest a compensatory homeostatic response to fat loss. In other words, the body doesn’t respond to this surgery in the same way that it responds to caloric restriction that I described earlier by increasing hunger and decreasing resting energy expenditure and decreasing the conversion of T4 to T3 and all of those things. And then we have studies that suggest that gastric bypass alters food reward processing in the brain, and so it’s changing the food reward system in some way, but those mechanisms aren’t entirely clear at this point.”
Thank you and congratulations on the new baby!
Hi Lynn,
It’s not uncommon for people who have had gastric bypass surgery to experience massive weight loss, and then substantial weight regain. Also, they can have problems such as nutritional deficiencies. It is true that bariatric surgery is the only proven medical intervention that leads to weight loss, but it is by no means a cure all. The advantage of PHD is that it achieves weight loss in a health improving way.
You’re right that absolute proof of a normalization of the set point will require actually reaching the set point and staying there without hunger. However, that takes a long time, and our book came out in December 2012, two years is not enough to normalize morbid obesity. However, a number of PHDers, including the two cited in this post, have achieve normalization and maintained it for long periods of time. Not everyone who adopts PHD has had that experience. We will learn more through the retreats about why that is. Is it imperfect implementation of the key weight loss diet and lifestyle steps, or something different about their condition?
Best, Paul
Paul,
A friend recommended the book/diet “Eat to Live” by Joel Fuhrman. Have you read it. To summarize you are to eat mostly fruits and vegetables with some nuts, seeds, beans. No grain, no dairy, no oils. What are your thoughts? My friend and others have lost a decent amount of weight. Is this healthy?
I don’t know if Paul will answer your question but you might want to read his book first! Fuhrman’s guidelines do not coincide with Paul’s. In addition the PHD lifestyle is meant to optimize health, part of which is weight loss for those who need it.
Hi Michelle,
I have read Perfect Health Diet and Eat to Live. They are similar in emphasizing fruits, vegetables and some starches. That’s about it. ETL is basically a vegan diet, only recommending to rarely eat meat, cheese or eggs. ETL also recommends beans and does not exclude wheat, opposite of PHD. Furhman’s emphasis is on micronutrients, which you would get on PHD from eating fruits and vegetables.
I just wanted to say that I recently went back on PHD after having been off it for about a year, and I lost ten pounds in probably around a month (thats an estimate.)
I had been almost exactly 10 lbs overweight, and for a petite person like me, that’s a concern. As the days go by, I seem to be losing even more weight too, espeically since I’ve started eating salmon and egg yolks again, which I had before excluded.
Hopefully I don’t go down too far, but I’m not too worried about that.
I had gone back on PHD just for health reasons, but the weight loss was a welcome surprise!
Thanks for everything, Paul!
That’s terrific Nora, thanks for sharing!
This talks about normalizing a body weight setpoint.
For someone who has been chronically underweight due to malabsorption/SIBO, thyroid, Lyme, autoimmune, etc….. I am hoping to cure the SIBO, gain some weight. PHD has not been enough to cure my SIBO so I am trying to follow the Fast Tract diet which measures the fermentation potential of foods within the PHD guidelines as well (i.e., using tapioca as a safe starch, etc.). However, I hope to eventually be able to eat a more normalized PHD diet.
My question is—do you think PHD would help me gain a normalized weight? I seem to be insulin resistant, blood sugar issues, low metabolism since my body has been in such starvation/malnutrition/deficient/underweight mode for so long. Once things get healthy again in my gut ad I gain weight again, is there hope for a normal body weight, not catapulting to the other end and being overweight?
Does that make sense?
Side note—does anyone have any experience with the Fast Tract diet by Norm Robillard? Or does it make scientific sense? I appreciate PHD because it is so scientifically inclined. I do not have the knowledge to evaluate. Does the Fast Tract diet make scientific sense?
Hi grae,
We’ve had a number of reports of people who were chronically underweight who normalized their weight.
PHD generally does pretty well against SIBO, so perhaps you haven’t fully implemented our advice. It is hard to keep up with everything I know. SIBO continued long enough tends to infect the pancreas and cause prediabetes then diabetes, so it would be good for you to get a handle on this.
Some cases of SIBO can lead to iron deficiency so I would get tested for that, that could explain the underweight.
No, there’s no reason to expect you’ll become overweight.
thank you, so, so much. i have implemented PHD to T–you’d be proud of me– and then tried going lower carb PHD. but i think my immune system was just too compromised with Lyme, autoimmune, and other stuff that it couldn’t fight the SIBO as well.
and yes, my pancreas are already compromised and struggling, and i am extremely iron deficient (as well as deficient in vitamin c, d, b complexes….) according to lab tests. i am seeing a doctor.
but i so appreciate the response and encouragement. it means a lot, i mean a lot. deep, deep gratitude to you, Dr. Jaminet.
Hi grae_bird,
Some points of emphasis: liver weekly, sunshine/vitamin D, vitamin C, intermittent fasting, circadian rhythm entrainment, vinegar, black coffee during the fast, antimicrobial spices on food (including onions, garlic, ginger), lots of salads with green leafy vegetables + olive oil + vinegar, daily exercise, bones/joints/tendons, iodine.
You should consider antibiotics, and test for H pylori.
Thank you for expanding Paul! I’ve used mainly lemon juice, but will add in vinegar. I consume alliums and ginger daily too. Great advice!
Oh, and BTW I have tested twice for H pylori and I’m negative.
Hi susan, just a heads-up – I didn’t test positive for H pylori until I had a stool antigen test. There’s blood, breath (I think) and then the stool antigen.
yup! bone broth, apple cider vinegar, sunlight, circadian rhtyhms, liver once a week… i’ve tried to implement what would be my own “PHD retreat” and lifestyle. i have not tested for h pylori yet, though.
Back to the SIBO–based on your comment on antimicrobial like garlic, I take it you do not place much stock in the FODMAP elimination? Garlic is a FODMAP.
MP, thanks for that. Which lab did you use for the stool antigen test? I’ve done blood and stool. My understanding after doing blood, that it’s not the best way to test, so then I did Doctor’s Data stool. Both blood and stool were negative. My SIBO breath test was negative for hydrogen but positive for methane. I thought that H pylori was more common with the hydrogen type, but that the methane type indicates that archaea are present. Wouldn’t I have tested positive for hydrogen if I had H pylori, or am I confused?
Grae_bird: I have SIBO too and I’ve not undergone any treatment or follow any SIBO diet restrictions yet, but I’m not underweight. I follow PHD. I was underweight (105 lb) before discovering PHD because I’d put myself on a severe elimination diet trying to figure out if I was reacting to specific foods (without success, I might add). Eventually I found PHD and I did gain weight initially, back to my starting point. I’m 5’5″ and 118 lb, and have been stable there for several months.
I have methane type SIBO and I’m about to begin a targeted antimicrobial and probiotic protocol with Chris Kresser. (Chris’ general dietary and lifestyle approach is also ancestral and very similar to PHD.) You might checkout his podcasts and articles on SIBO, low FODMAPs and his most recent one on Jan 16 about Candida overgrowth (he talks a lot about SIBO in that podcast too). I’m mentioning this because I’m pretty sure that in the Candida podcast he cites Norm Robillard’s study. Also I seem to recall some comment posts by Mr. Robillard on some of the earlier IBS and SIBO related postings by Chris. So I get the sense that he reads Chris’ blogs regularly and that there’s at least a mutual respect there. There are also some comments posted by people who have followed the Fast Tract Diet. I haven’t looked into it myself, but would be curious about how it differs from low-FODMAPs, etc.
I’ll also be curious if Paul knows of Robillard’s work and has any comments about it or FTD because I’m pretty sure that Paul’s not a fan of low-FODMAPs for SIBO, but rather following full PHD (which is what I have done so far).
Hi susan,
I know of Norm’s work, and Norm himself has commented here and in our Facebook group. But I’m not sufficiently familiar with it to discuss it.
FODMAPs are a form of fiber and fiber-restricted diets are often a good temporary step in treating gut dysbiosis/infection. It is not that I oppose these strategies, but I think the emphasis should be elsewhere.
Thank you for clarifying and I agree that restricting fermentable fiber may be ok for a short-term stint, but long-term is unhealthy. Would you mind expanding a bit on your last phrase…”the emphasis should be elsewhere”?
(BTW, I’d not heard that prolonged SIBO could lead to pancreas problems and diabetes, so thank you for responding to Grae!)
Thank you, Susan. So much.
The Fast Tract Diet differs from FODMAPs primarily in that it also restricts fiber and resistant starch, unlike FODMAPs. FTD also does not eliminate entirely foods (i.e., “You can NEVER have asparagus”) but FODMAPS will have higher fermentation potential rankings and so thus are limited (i.e., in a target goal of 20-30 FP grams, you can only fit so much in, so you emphasize foods with lower FP, thus lower FODMAP).
I am familiar with Chris Kresser and read the article you mentioned, as well as his others. I know he favors the FODMAP diet for SIBO over GAPS and SCD.
My plan is to follow the FTD within PHD guidelines as much as possible—so, continue to include tapioca and jasmine rice (FP of 5 and 1 respectively) so as to not go low carb. But, according to the FTD theory, these will be less fermentable, easily absorbed, and thus less food for SIBO. The moderate carb level will hopefully avoid ketosis as well, which (I believe Dr. Jaminet has said) can feed SIBO as well.
But fiber will be drastically reduced—and I know fiber is, in the long run, good for healthy gut flora.
And the variety and nutrient dense root/starchy/sugary veggies will be reduced (i.e., butternut, beets, carrots have high fermentation potential).
And of course I will add probiotics. But would love more insight and advice. As Susan said, what the “emphasis elsewhere” is.
I would like to second Susan’s question: Where do you think the emphasis should be?
I assume that first steps should include:
1. Strengthening the immune system: Eating the perfect health diet, recommended supplements, circadian rhythm support, daily exercise, and intermittent fasting.
2. Improving and diversifying gut flora using fermented food (and/or probiotics).
3. Adequate dietary Tryptophan and choline from meat, liver, and egg yolks (as intestinal motility is controlled by serotonin and acetylcholine).
But if problems remain, what should come next? Supplementation of a couple grams of both choline and 5-HTP? Acetylcholinesterase inhibitors and 5-HT4 agonists? Biofilm disruption techniques (e.g. EDTA, enzymes, vinegar, lactoferrin, NAC, etc.)? Antibiotics (e.g. Rifaximin)? Something else? Or is fiber restriction a good next step, and all you meant by “emphasis should be elsewhere” was that 1–3 should be tried first?
Thanks!
Eric, thank you for your comments. I think that Dr. Paul did respond earlier–it was kind of missed as it was in a previous reply: He wrote:
Some points of emphasis: liver weekly, sunshine/vitamin D, vitamin C, intermittent fasting, circadian rhythm entrainment, vinegar, black coffee during the fast, antimicrobial spices on food (including onions, garlic, ginger), lots of salads with green leafy vegetables + olive oil + vinegar, daily exercise, bones/joints/tendons, iodine.
You should consider antibiotics, and test for H pylori.” End quote.
A further question, though. Migrating motor complex (MMC) is not often discussed in SIBO but can be an important part of it. Would Intermittent Fasting (IF) help or hinder MMC? From what I’ve heard, IF could help it. However, would steamed low-fiber veggies and coconut oil be okay while on an IF? Or would the steamed veggies still be too much fiber/bulk for MMC improvement still in regards to SIBO?
Correction: I should have said “couple grams of choline, and couple hundred milligrams of 5-HTP”.
Re: Paul’s earlier comment: What’s the logic behind black coffee during the fast? (Is something in the coffee helpful, or are you just trying to avoid added milk and cream? It sounds like caffeine intake may have positive effects on motility, but the literature is fairly murky.)
Grae, thanks for explaining those differences in diet approach to me. I’ve read some FODMAP lists (they are all different it seems!) that try to achieve the same thing I think by saying “only 1/8 avocado, 1/2 grapefruit, 4 ices of beets” etc.
Referencing page 779, it seems you are saying the percentage of macronutrients is different for weight loss following PHD . What percentages would you recommend for weight loss? Thank you!
“You’re still eating the same PHD foods, and they should still taste delicious. Quantities shouldn’t be much different than a normal diet, since you still need the same amount of carbs and protein. A diet with 500 calories from carbs, 300 calories from protein, and 500 calories from fats (primarily via egg yolks, liver, seafood, beef or lamb, and coconut milk) is the minimum caloric intake consistent with proper nourishment.”
Excerpt From: Jaminet, Paul. “Perfect Health Diet: Regain Health and Lose Weight by Eating the Way You Were Meant to Eat.” Scribner, 2012-12-11T05:00:00+00:00. iBooks.
This material may be protected by copyright.
Hi Dr. Jaminet,
First of all, I want to say thank you for writing your book. Your scientific labor of love has already greatly impacted my own and my fiancé’s sleep, energy, and overall quality of life.
I am writing you because I am unclear as to what ratios I should aim for in regards to achieving better weight loss results. I know you recommend 600 carb calories, 300 protein calories, and 500 fat calories, but I am I am 6’2” and weigh 270.9 pounds. Further, I seem to carry more muscle naturally, so although I am much overweight, people are shocked when they hear how heavy I am. My weight loss goal is to get down to 215-220 pounds. Due to my height and size, would you recommend different macronutrient ratios/a specific daily caloric intake I should aim for?
I have easily adopted intermittent fasting, and I now naturally stop eating around 7pm at night and don’t have anything besides black coffee until around 11am-12pm the following day. I do moderate light walking almost every day, and a strength training exercise 1-2x per week. I am thinking of trying to incorporate yoga into my routine at least 3x per week to increase flexibility and help with stress as I work as a Social Worker. Any advice to help me achieve my best health would be greatly appreciated. Thanks in advance for your time.
– Isaac
Hi Paul,
I have a question/comment about hunger on PHD.
I have been on PHD for 2-3 years, and am one of those funny success stories where all sorts of things improved that others may not have noticed, but made huge differences in my life (huge improvement in dental health, energy levels, achy back in mornings went away, etc.). I’ve never had any issues with weight, I’m somewhat leaner on PHD (can see my abs more) but have remained 150 lbs my whole adult life.
However, the one thing I’ve noticed since switching to PHD is that the word “hungry” seems too generic. When I feel hungry it’s usually for a particular macro-nutrient, e.g. after a workout I may crave a high-protein meal, at other times I crave more fat, etc. If I were to substitute a different macro-nutrient (e.g. eating a banana when I’m craving protein) it wouldn’t satisfy me at all.
I don’t measure my food carefully, but I would say that my “specific hunger” guides me to PHD recommended macro-nutrient ratios quite effortlessly.
Is this sort of “specific hunger” common on PHD?
Given how many people are pre-diabetic, it seems probable that you had a few non-diagnosed attendees at the retreats. You included the caveat about the results being for non-diabetic persons; any thoughts on where the undiagnosed T2 or metabolic syndrome would land on the curve?
Hi Paul;
I would like to see if some weight loss data corresponds to the decay model. Seems like I’m trying to solve for SP and also the characteristic time with only one series. Do you have a way of matching actual data to find an SP value given a series such as in the post?
Hey Paul any plans on a updated book also a cookbook?