Tom Naughton, producer and star of Fat Head, has recently been migrating toward PHD. The resistant starch philia that has been sweeping through the ancestral health world got him started, and after experiencing some benefits from resistant starch and then potatoes, Tom decided to go back and read our book. He liked it and reviewed it positively.
Tom invited me to do a Q&A with his readers, who had lots of great questions. Here it is.
Questions and Answers
Jeanne Wallace: “Should we eat a serving of safe starch daily? And must a baked potato be cold in order to be healthful or is room temp okay?”
You should eat a serving of safe starch several times a day – with every meal! No, baked potatoes do not have to be served cold. Room temperature is OK but body temperature or warmer is even better. Make your potatoes enjoyable.
Vlc eater: “Do you recommend PHD for diabetics and prediabetics? If VLC eliminates fasting glucose issues and leads to better glocose levels overall, do you see a problem? Also, is it possible that the self-reported mood issues reported here are a manifestation of mild carb addiction?”
Yes, I do recommend PHD for diabetics and pre-diabetics.
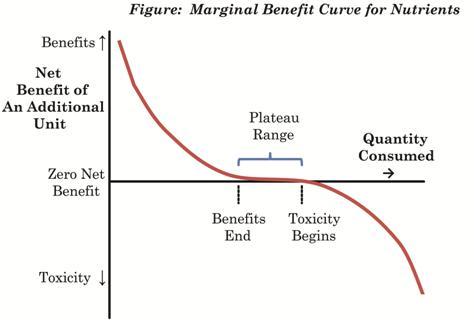
I discussed this question in a previous blog post (“Safe Starches Symposium: Dr Ron Rosedale,” Nov 1, 2011). The basic biology here is that the body’s physiology is optimized for a carbohydrate intake of around 30%. At higher carbohydrate intakes, glucose disposal pathways (such as switching muscle cells from fat to glucose burning) are invoked; at lower carbohydrate intake, “triage” of glucose occurs, reserving it for the brain, and some useful carb-dependent functions are lost. Both extremes are stressful, and in metabolic disorders, both extremes may be difficult to handle.
In diabetes, the body does not dispose of excess carbohydrate properly, so carb intakes above about 30% are harmful. However, all carb intakes of 30% or lower are handled quite well in terms of blood glucose levels. This has been demonstrated in many studies. I like the LoBAG (Low Bio-Available Glucose) diet studies of Mary Gannon and Frank Nuttall, which are quite close to PHD. They tested both 20% carb and 30% carb diets in diabetics, and both carb levels were handled quite well. Here is data from Gannon & Nuttall’s 2004 study of a 20% carb diet (graph is actually from a later paper by Volek & Feinman).
Over a 24 hour period, blood glucose levels were tracked in Type II diabetics on their usual diets (blue and grey triangles) and after 5 weeks on a 55% carb – 15% protein – 30% fat (yellow circles) or 20% carb – 30% protein – 50% fat diet (blue circles):
You can see that on the 20% carb diet blood glucose came close to non-diabetic levels. The same thing happened in later studies of a 30% carb diet.
What happens when diabetics go to very low carb diets, 10% carb or less? The body invokes “triage” mechanisms for glucose conservation under carbohydrate starvation. Among these are hormonal changes including low T3 thyroid hormone and high cortisol. This condition makes fasting problematic and diabetics tend to develop high blood glucose levels in the morning after the overnight fast. Due to high fasting glucose and severe insulin resistance, HbA1c may be elevated by this strategy compared to a 20% or 30% carb diet. Various pathologies, including hypoglycemic episodes, dysregulation of serum fatty acid levels, ketoacidosis, and adrenal dysfunction become more likely. The long-term dangers described in our “zero-carb dangers” series are also present, including a higher risk for some infections, kidney stones, and other ailments.
Evidence that resistant starch helps diabetics also supports the prescription of starchy foods. It’s likely that natural whole foods will be found to be the best source of fiber, and resistant starch in nature is always accompanied by digestible starch.
PHD has generated very good results in diabetics and so, while diabetics might possibly benefit from a slight bias toward lower carbohydrate and higher protein vis-à-vis the healthy, the ordinary version of PHD seems to be very close to optimal for diabetics.
Ben: “Where can I see a very recent photo of you and your wife? (I see the author/advocate’s physical appearance as a data point when considering a proposed approach to nutrition.)”
We haven’t taken many photos lately, but you can see a video of me from January this year at a blog post we did for Dr. Alejandro Junger’s Clean Program. Here’s a look:
Our May Perfect Health Retreat begins next week and we’ll take photos and post them to our blog and social media. Keep an eye out there for up-to-date photos and maybe video.
Allison: “I want to know recommendations of how to use “safe starch” for weight loss.”
Eat it! Getting about 20%-25% of calories as safe starches (30% of calories as carbs) is optimal for weight loss. It’s best to cook them in a batch and save them in the refrigerator until meal time, when you can quickly re-heat them. This is both convenient and generates more resistant starch.
Maggie: “One of my Resting Metabolic Rate test results showed that my fat burning/glucose burning ratio is .98, meaning I burn .98 glucose. I do not burn much fat (a better score would be .85, for example). Does this mean my dietary fat percentage should be lower than Paul’s recommendations for weight loss because my body is a slow fat burner? What can I do to increase my fat burning rate?”
I am not sure what test you took. A standard test to assess fat burning vs glucose burning is the Respiratory Quotient, which is close to 1.0 when burning glucose exclusively and close to 0.7 when burning fats exclusively. But no one gets a number as high as 0.98 at rest, though it can get that high during intense exertion.
At rest, the Respiratory Quotient should approach 0.7, but in the obese it tends to get stuck at maybe 0.85. To enable it to go lower, you want to support mitochondrial health and train yourself to burn fats better. Supplementing vitamin C and pantothenic acid may help, also daily exercise and circadian rhythm entrainment.
Martin: “What’s your opinion on a cyclic-ketogenic diet, with a carb refeed once a week only? Also, does it matter when one eats carbs during a day (e.g. morning vs. evening) and how it is combined with protein and fats?”
I think once a week is too infrequent for carb feeding. I think daily carb feeding is best.
Carbs are best eaten during the daytime in a fairly narrow feeding window. Relative to protein, carbs should be biased later in the feeding window, protein earlier. But both should be eaten together. Just make the first meal a little more protein rich, the last meal a little more carb rich, or follow it with a sweet dessert.
Fritters: “I own your book, but the whole idea of organ meats, bone broth and fish nauseates me. Also, I’ve heard people with AI problems are sometimes fixed by removing nightshades from their diet. In any case, I have an AI problem and am on prednisone all the time, which shoves my blood sugar way up. I’ve felt a LITTLE better on less nightshades, so I want to keep doing that, but I want to eat closer to the Perfect Health diet without gaining too much weight because of the increased blood sugar from the prednisone. What areas do you think I should concentrate on to get closer to perfect health? I’m already avoiding sugars, wheat and crap-oils.”
Yes, it’s true that many people with autoimmune issues benefit from dropping nightshades. In general, autoimmunity originates with foreign compounds entering the body through a leaky gut, which is the same way food sensitivities originate. Nightshade toxins are immunogenic and can easily generate food sensitivities in people with a leaky gut.
PHD with nightshades removed is essentially a Paleo autoimmune protocol.
Prednisone is a drug I don’t like, it suppresses immunity which suppresses symptoms but often worsens the underlying disease – and it has negative side effects as you’ve experienced.
Focus on eating PHD meals in which starches are paired with meats, vegetables, fats, and acids; support immune function with vitamin A (liver, spinach, carrots), vitamin D (sunshine), daily exercise, intermittent fasting, circadian rhythm entrainment, zinc, iodine, and vitamin C; include collagen (bones, joints, tendons in soups and stews) for wound healing and gut barrier integrity.
Teresa Grodi: “My question for Paul is regarding the “Candida Diet”. I know lots of people, especially postpartum women dealing with bad thrush, who are on the anti-candida diet, which prohibits what you would determine “safe starches”. I think I saw in passing that you had some problems with the anti-candida diets, regarding the prohibition of safe starches, and I thought maybe you could elaborate, with an eye to postpartum/breast feeding mothers. I would love to be able to help my fellow mothers.”
Very low-carb diets will flare fungal infections by suppressing antifungal immunity and reducing the population of probiotic bacteria in the gut, which compete with fungi. A balanced diet with 30% carbs is best for candida.
My answer to vlc eater above about why 30% carb is best for diabetes also applies to Candida: you want a well nourished body, including nourishment with glucose, but without an excess that could feed the infection. It’s only carb intakes above 30% that provide that excess. Carb intakes below 30% starve immune function, extracellular matrix maintenance, and mucus production, all of which help defend against Candida.
Eating liver, getting sunshine, intermittent fasting, circadian rhythm entrainment, and eating fermented vegetables are other elements of a good anti-Candida strategy.
Tony: “Dr. Jaminet’s phd proposes safe carbohydrates to replenish daily glucose stores. He proposes safe carbs because of the damaging health effects of grain carbs (except rice). If a subject occasionally (1,2,3 times a week?) consumed bad starches instead of good starches won’t these bad starches still replenish his glucose stores? Won’t the good fats blunt any insulin spike from the bad starches? In other words, phd with bad starches, wholly or partially, occasionally. Would subject’s health still go down the tubes? Would subject gain weight or stall a weight loss?”
Yes, all starches will replenish glycogen (glucose stores). What makes a starch “good” or “bad” (we use the terms “safe” and “toxic”) is not the starch but associated compounds which can be toxic to us.
I can’t say that your health will go down the tubes if you eat bad starches like wheat. Only that they appear to be risky things to eat. They do harm some people. It’s possible that even in people who appear to be unharmed, they do insidious damage. We can’t know for sure, we just think that it’s prudent to avoid wheat.
No, wheat won’t necessarily cause weight gain by itself. It is associated with higher body mass indexes, however, and there may be mechanisms by which it can promote leaky gut which is inflammatory and promotes weight gain. I think it will be slightly easier to lose weight without it.
Lily: “I am sensitive to sugar, and have a huge addiction to it. Starches like white rice tend to raise my blood sugar too much and I end up binging (even if I have it with a fat source). Are there safe starches that I can eat that won’t raise my blood sugar so much? Potatoes seem to affect me the same way white rice does. I would eat potatoes with the peel, or try brown rice, but don’t those have anti-nutrients? Are there starches that are safe for me, a sugar addict with a body that doesn’t handle sugar very well?”
I’ve heard many stories like yours and people are often surprised to find that all of those things clear up pretty quickly on PHD. The pattern:
- Binging and cravings and addictive behaviors typically follow starvation, so I’ll guess you’ve been too low carb for too long. Your brain knows your body needs carbs and when it’s available says, “Ah! We’ve found the nutrient we need! Go eat this precious sugar/starch before this rare and vital food disappears!” To fix this, eat PHD levels of carbs. Over time the craving/addiction will go away.
- Weight gain from eating carbs usually indicates a leaky gut and a dysbiotic gut flora, such that when you expose your gut to carbohydrates you get inflammation which activates adipose tissue (an immune organ) and causes it to grow. It also relates to the binging, after past starvation your appetite is upregulated temporarily when you get a chance to repair malnourishment.
- High blood sugar upon eating starch indicates that (a) you are cooking and eating it incorrectly and/or (b) you lack the gut flora needed for proper glycemic regulation. To fix (a), read this post, and to fix (b), you need more fiber, including some resistant starch, and fermented vegetables.
Above all, you need a balanced, nourishing diet and immune support. See my previous answers to Teresa Grodi and Fritters for some tips. Your mindset should be oriented toward health, not weight. You should accept that an initial weight gain may be “baked in the cake” so to speak, it is already inevitable thanks to past deprivation, accept it and move on to healing yourself and once healed you will be able to re-lose the weight in a natural and healthful way, and reach your goal weight safely.
Carnivore: “My dilemma is when on a VLC diet my blood sugar (A1C test) very good, fasting glucose very high (I am diabetic) When I start some safe starches (tried potatoes and beans) morning fasting glucose excellent – blood sugar throughout the day – way too high after the meals – and even with medication is coming down in a few hours (too slow). So, my question is: how can one determine how much safe starch is safe? (for a female diabetic approaching the retirement age) and what kind of starch: potatoes, beans, sweet potatoes? I assume rice is out of question for diabetics like me.
This is a very common pattern. See my answer to vlc eater above. 20% to 30% carbs is best. If postprandial blood sugars are high, make sure you are cooking and eating starches properly and working on your gut flora with fiber and fermented vegetables.
Chad: “When weight lifting to gain muscle, most experts say you need to consume massive amounts of carbs in order to gain muscle. Then when you wish to slim down you reduce carbs. I prefer paleo style diets and it makes sense, but I also want to lose fat and gain muscle. The instructions to do so seem to directly conflict with the Paleo Diet idea. How do you induce your body to increase muscle size without consuming nothing but carbs only to go LC to get super lean later? Is increased insulin production necessary to increase muscle size? How do you do that and not become insulin resistant? Body builders get huge muscles and super lean all the time on this super high carb/super low carb cycle and its just so confusing.
The main instrument to vary is total calorie intake, and the relationship between calorie intake, periods of fasting, and the timing and intensity of workouts. Macronutrient proportions should be close to PHD ratios at all times, with slight variations synchronized with workout schedule.
High calorie intakes lead to gain of mass (both lean mass and adipose tissue); low calorie intakes lead to slimming (both lean mass and adipose tissue). The type of physical activity you undertake places the focus on a different mass reservoir. When you do intense workouts, you are focusing the body on muscle; you want high calorie intake at this time to promote muscle growth. When you are resting, you are focusing the body metabolically on adipose tissue – at this time you want to fast and reduce calorie intake to promote loss of adipose mass.
Macronutrient ratios should vary toward more fat and carbs when your calorie intake is high (e.g. eat more dessert like foods) and less fat and carbs when your calorie intake is low – in other words, your protein intake should be more stable than your fat and carb intake. But this is something you will do naturally. It doesn’t need to be consciously directed, and it doesn’t need to be extreme. You do need to direct your conscious mind to varying total calorie intake in sync with your workout intensity, and vary your workout intensity.
Work out every day, but vary the intensity, and vary the calories in sync with workload.
Pierson: “Regarding fructose, what is his opinion on foods like fruit, honey, and sweet syrups? While it does make sense to avoid processed industrial anything, what about whole-foods sweeteners?”
A little bit of honey or sweet syrups is OK. I think you’ll find that on low-carb diets without added sugar, your tastes change and very little honey is needed to make foods taste appealingly sweet. If you weighed the honey and calculated how many calories it had, you’d find it was very small. One teaspoon of honey weighs about 6 grams and has about 18 calories, about 9 calories of fructose or 0.4% of daily energy intake. That’s not going to kill you. We recommend getting about 100 calories of fructose daily from all sources, including fruit.
Fruit and berries are excellent foods and not to be avoided. We recommend eating 2-3 pieces of fruit or servings of berries daily.
Charles Grashow: “If LDL-P increases isn’t that bad regardless of the particle size? Larger particles can still get thru the endothelium and become oxidized it just might take longer.”
Yes. The LDL particles get oxidized in the bloodstream and then taken up by white blood cells, activating inflammation and potentially turning them into “foam cells” and assisting formation of atherosclerotic plaques. Endotoxemia (influx of endotoxins from the gut) is usually the biggest driver of LDL particle oxidation. More LDL particles and more endotoxins = more oxLDL reaching white blood cells = more inflammation and faster plaque formation.
Steve Parker MD: “The preface of the Scribner edition mentions your health issues while eating the standard Amercian diet: neuropathy, memory loss, impaired mood, physical sluggishness, and rosacea. You attribute your subsequent scurvy to the very-low-carb paleo diet you adopted to resolve the original issues. Did your personal physician(s) make the diagnoses and say they were diet-related? Uptodate.com says this about rosacea: “The pathways that lead to the development of rosacea are not well understood. Proposed contributing factors include abnormalities in innate immunity, inflammatory reactions to cutaneous microorganisms, ultraviolet damage, and vascular dysfunction.” Your other three SAD-related problems each have easily 10-20 things that can cause them, many of them unrelated to diet. By the way, I enjoyed the book and learned a fair amount from it. Folks eating the standard American diet should be better off switching to PHD.”
My doctor acknowledged the symptoms but was baffled about the cause, as was I. Rosacea was diagnosed by multiple dermatologists. After we optimized PHD my rosacea faded over a period of about 2-3 years. I would not be diagnosed with it today, though at times I still see traces of it.
The memory loss went away during a three month course of antibiotics, taken in the later stages of transitioning from Paleo to PHD.
The things my doctor was clearly able to diagnose were not very helpful to me. For instance, after my VLC and scurvy phase, my belly became bloated and a fairly hard nodule formed which my doctor said was a lipoma. We did a barium enema and it found diffuse diverticulosis. But that was not a cause of my health problems, it was an effect of the VLC-scurvy mistake. I found the various testing we did interesting and educational, but in the end it didn’t show me a path forward. It was diet, lifestyle, and a somewhat speculative round of antibiotics that cleared things up.
Thanks for the praise!
Ryan H: “In your book you explain that fats and acids (ex: vinegar, lemon/lime juice) blunt the insulin spike of starches. To my knowledge you do not mention or recommend cinnamon doing the same. I am just wondering what your take on cinnamon is? I have heard that it lowers blood glucose levels. P.S. Cinnamon on a sweet potato is pretty good!”
Cinnamon is good, but like all good things, it’s possible to get too much. Eating to optimize flavor is a good guide to the optimal amount. I agree, cinnamon and butter on sweet potatoes is delicious!
Mike W: “Do you make any distinction, health-wise, between short-chain saturated fats and long-chain? The reason I ask is that foods heavy in short-chain sat fats (bovine milk, coconut oil, palm kernel oil) seem to give me clogged pores and acne, so I avoid them. This is no hardship for me, I was never big on cheese, butter, or coconut anyway. The fatty foods I do eat – eggs, meat, nuts, chocolate – don’t bother my skin at all, and in my research I’ve found their sat fats are almost exclusively 14-carbons or longer. Besides keeping my skin clear, I can justify my short-chain avoidance from an ancestral standpoint. I doubt my distant ancestors had access to coconuts, and as I understand it, human milk has a lot less short-chain fats than bovine milk. So… are short-chain saturated fatty acids an essential nutrient? Am I missing something by avoiding them?”
Yes, short-chain and long-chain saturated fats are discussed in different chapters of our book because their biological effects are quite different.
I suspect your problem is more related to consuming oils, than to the chain-length of the fatty acids. Try supplementing pantothenic acid, zinc, and choline (or eat egg yolks and liver) and I bet you will tolerate the oils a lot better.
Coconut milk is not an essential food, but it is a healthful one, and we recommend it.
Ryan H: “You advise if one needs to consume something during a fast (for hunger reasons), a spoonful of coconut oil or mct oil is allowed without it hindering the fast. What is your take on butter or cream during a fast (like in coffee)? Will it break the fast and autophagy. I am just wondering since some LC people recommend it and say you are still reaping the benefits of fasting since you’re not consuming protein or carbs.”
Protein disrupts a fast the most, carbs next, fats the least. If you want a bit of cream in your coffee, that’s fine. If you are concerned about its effect on autophagy, delay your breakfast an extra 10 minutes, that will get the lost autophagy back.
Becky: “For the nightshade avoiders among us: Does packaged tapioca starch serve as a resistant starch? If so, can it be eaten like potato starch … in water, raw? I use it to make baked biscuits. Will they, cooled, provide resistant starch? Cassava, sago and taro are not available here. I like to keep rice to a minimum. Plantains, green bananas and sweet potatoes are my starches. I got diverticulitis on VLC and am enormously vested in getting my gut biome fed with resistant starch. I am the Becky quoted in your book, in the thyroid discussion. To update, Hashimoto’s antibodies DISAPPEARED from my TPO blood tests, and my doctor says I no longer have Hashimoto’s. He thinks it was probably giving up wheat.”
Hi Becky, it’s great that your Hashi’s is gone! And thanks for contributing your story to our book!
Detailed questions about resistant starch content of various foods under various cooking methods should be directed to Tim and Grace, who have been researching those things.
I would say however that you should not eat tapioca starch in water raw. Rather, make it into foods like your biscuits and eat them as parts of meals in the PHD manner, accompanied by butter, vinegar, vegetables, and meat. Or at least, as a dessert with butter and vinegar.
Norm: “1. Why do hunger and cravings for carbs increase for some people by introducing rice and potatoes whereas most of the people do not have that being low carb?
2. How do we know that symptoms associated with low carb like cold hands and feet, low thyroid etc are NOT from eating less as hunger is dramatically reduced on a low carb diet?
3. Paul highly recommends 16 hours of fasting, would PHD provide the same benefits especially weight loss without 16 hours of fasting? Probably standard American diet would be a lot healthier with 16 hours of fasting? If calorie restriction is not good or creates problem for people especially in term of weight loss then why calorie restriction is achieved via intermittent fasting on PHD?”
Many people on very low carb diets have hunger and cravings for carbs. Often it gets displaced into a craving for sweets or for alcohol.
For many low-carbers, adding rice and potatoes leads rapidly to a feeling of well being and satisfaction. It quiets appetite.
For others, eating rice or potatoes can trigger strong cravings for more. For reasons why, see my answer to Lily above. There are usually two components to this. First is a need for the body to replenish glucose-dependent proteins such as extracellular matrix; typically this takes at most a few weeks to a month, after which appetite diminishes. Second is an inflammatory reaction from gut pathogens that feed on the carbs. This requires fixing the gut dysbiosis or infections.
The low thyroid is a hormonal reaction to conserve glucose, and associated phenomena like cold hands and feet illustrate the inability of the body to properly maintain homeostasis when it is starved of a key nutrient. As far as reduced appetite on low-carb, there is a difference between reduced appetite due to a body being well nourished, and the anorexic lack of appetite that is induced during chronic starvation. The first is desirable, the second is not.
16 hour intermittent fasting is beneficial for health so long as the 8 hour feeding window falls in the daytime. PHD would still be an excellent (nourishing, low toxicity) diet without intermittent fasting, but this is another opportunity to improve health. Lifestyle is as important as diet for health.
It is not so much that PHD with intermittent fasting restricts calories, it is that it achieves optimal nourishment with the smallest possible caloric intake. In other words, one eats fewer calories without any restriction of nourishment when eating PHD. If this is hard to understand, try reading Chapter 17 of our book.
Gerard Pinzone: “I’m interested in trying this out to see what difference it might make. I’ve heard that there may be an initial period of weight gain. If true, why? Can you provide a recommended schedule? Something like, “1 tablespoon of potato starch in the morning for one week, then increase by 1 tablespoon each week until you reach 4 tablespoons.” Is it better in the morning than night? Also, what issues are signs that we should stop and which should we grin and bear? Can we start/continue to take a probiotic? Should we?”
Coming from SAD, people almost invariably lose weight when adopting PHD. I haven’t heard of any cases of weight gain in people coming from the standard American diet.
Coming from lower-carb diets, the immediate reaction can be either weight loss or weight gain. There are two principal reasons why weight gain may occur. It is partly a matter of low-carbers “adopting PHD” by simply adding starches to their Paleo diet, thus adding calories; and partly a matter of a gut dysbiosis or infection leading to greater inflammation when carbs are added. The solutions are (a) emphasize nutrient density and dietary balance so that hunger abates with lower calorie intake – that is, implement PHD more fully; and (b) address gut health through immune support and fermented foods and fiber.
I recommend just adopting PHD in toto from the beginning. There’s no reason to delay a good thing.
It’s fine to take probiotics but fermented vegetables usually contribute more.
JD says: “Just like all of this rethinking about RS, I’ve been rethinking the theory about optimal omega 3:6 ratios. Everything I remember reading about it recommends the ideal ratio is between 1:1 and 1:4. But what if it’s less about the ratios and more about eliminating bad fats (franken oils, factory farmed animals). Let’s say someone is following the Perfect Health Diet almost to a T, except most of their fat calories are coming from a high quality olive oil so the O3:6 ratio is closer to 1:8; is there any reason to think that person might less healthy than someone with a more ideal ratio? I do remember reading about how essential fatty acids from O3 and O6 fats compete for the same enzymes, but are there any studies out there that suggest excessive olive oil consumption interferes with therapeutic doses of O3 EFAs?
I guess my question could really be simplified to this; Is there any reason I should stop drowning my salads in olive oil?”
Our peak health ranges are about 1% to 4% of calories from omega-6 fats (mainly linoleic acid) and 0.5% to 1.5% of energy from omega-3 fats (mainly from marine sources).
If you eat at the high end of the omega-6 range (4%) and the low end of the omega-3 range (0.5%), you’ll still have perfect health according to our analysis, and you’ll have an 8:1 ratio.
However, you have to hit fatty acid quantities spot on to be the peak health range for both with that ratio. If you have a 3:1 ratio, you could eat omega-6 anywhere from 1.5% to 4% of energy and still be in the peak health range for both. So that is a more desirable ratio to aim for.
Drowning your salads doesn’t sound good. How about flavoring your salads with olive oil?
Amberly: “If using RS as a supplement (ie Potato Starch in a smoothie or cup of warm water), is there a “best” time of day to take it? In the morning? Before bed? All at once? Split into two or three doses?
Also, I am very sensitive to carbs and need to lose quite a bit of weight. What is the lowest number of carbs you would recommend going? Is it possible to stay in ketosis? Can you get the same health benefits from a cyclical ketogenic diet–IE VLC most of the time with one or two evenings a week of safe starches? Can you get health benefits by adding just RS (ie Potato Starch) but not the safe starches?”
Take RS before your first meal. If you do intermittent fasting and your feeding window is 11 am to 7 pm, take the RS at 11 am.
I would recommend getting at least 20% of calories from carbs, but I think 30% is better for most people.
Lower carb diets should be seen as only temporary therapeutic diets, forms of extended fasting, not as permanent diets. Ketosis is fine, unless you have certain infections, but chronic starvation of desirable nutrients is not. I think it’s best to eat starches daily. No, your body needs glucose as well as a healthy gut flora.
Mike G: “I believe you mean the enzyme amylase, rather than lipase? Amylase will hydrolyze the starch into maltose disaccharides first, then maltase (on the villi of the small intestine) will digest the maltoses into glucoses. Then the glucoses can be easily absorbed via transporters on the villi surface. This is why I cannot wrap my head around how fatty acids could blunt glucose spikes, or insulin spikes. Do the fatty acids bind to the glucoses? I suppose they could, given that we have glycolipids on our cell membranes.”
I don’t know what this is referring to. If it’s our recommendation to combine starches with fats in order to reduce their glycemic index, the reason blood glucose is lowered by eating starches with fat has to do with delayed stomach emptying and improved metabolic regulation.
Troysdailybacon: “With regards to Xylitol – I use it as a tooth protocol to fight cavities, but end up injesting a small amount. I’ve heard that it acts like a prebiotic as well. But in the mouth, bad bacteria try to metabolize it, but can’t, so the bacteria die off. How does Xylitol react in the gut? Will it feed the good bacteria and produce butyrate? Or, like in the mouth, will it kill off good and/or bad bacteria in the gut?”
Xylitol like other sugar alcohols can be fermented by some bacteria, and it has antimicrobial effects against others, so it will alter the gut flora (and the oral flora). I am not sure we know enough to say whether the changes are good or bad.
In in vitro studies, xylitol doesn’t seem especially effective at preventing cavities – it doesn’t do nearly as well as fluoride; and it also appears ineffective in human studies. This may be one of those cases where positive early studies don’t seem to be replicable.
Rob: “Do you recommend supplementing with additional resistant starch (potato starch) and other fermentable fibers (inulin, pectin, etc) or just getting these things from food? What are the potential negative effects of too much resistant starch and fermentable fibers?”
I recommend getting fiber from food, but designing one’s diet and preparing food to make it fiber-rich. This can be done by eating natural whole foods, copious fruits and vegetables, and pre-cooking and refrigerating starches.
It is unclear what the negative effects of too much fiber would be, but there is surely a point when you can get too much.
I think of it in ecological terms. You are crafting an ecosystem in your gut, and you want an ecology that favors evolution of a healthful flora.
Humans have an overnight fast of 12-16 hours and a daily feeding window of 8-12 hours. Gut bacteria have a reproductive life cycle of about an hour when food is available. So during your daily feeding, your bacteria have enough food to reproduce and could potentially double their numbers 8 times, or increase their population 256-fold. Then they go through an overnight fast, and their numbers diminish. Ecologically it is a boom-bust cycle similar to deer multiplying when food is abundant and then starving in the winter.
Within the overnight fast, your immune system has an advantage in shaping the ecology. Where probiotic flora are present, it can reward them by generating mucus; where inflammatory pathogens are present, it punishes them with antimicrobial peptides. During the fast, microbes are relatively defenseless due to lack of resources. During feeding, microbes have the upper hand.
Providing lots of fiber creates a boom-bust ecology on a daily cycle, while a low-fiber diet creates more stable bacterial population levels.
In general, you want to eat the amount of fiber that maximizes microbial diversity (that is, genetic diversity) in the gut. Low microbial diversity is associated with disease, high diversity with great health.
Boom-bust ecologies create a different set of selective pressures on bacteria than ecological systems with stable food supplies. Potentially, too great an amount of fiber might reduce microbial diversity by rewarding species that are able to reproduce most rapidly during the food “boom” and preserve their numbers by hibernating during the overnight “famine”. Many beneficial species may not compete successful with hyper-growers like E. coli in such an ecosystem.
Low microbial diversity in the gut is associated with many diseases. Usually low diversity results from starvation of fiber, but conceivably supplementation with large doses of resistant starch could bring about a similar result.
I consider the optimal amount of fiber to still be an open research question. We don’t know the answer. But I am confident the optimal amount is not “infinite fiber.” There will be some amount that is too much.
Incidentally, getting a diversity of fiber types – not just resistant starch – will be important, as this too will promote microbial diversity. This is one reason a natural whole foods approach is likely to be optimal.
TMA: “I haven’t read your book but what I’ve read about your diet on your website sounds appealing. One concern I have though is the number of different supplements you recommend. I’d be leery of low dose lithium for example. Do you discuss your rationale for these supplements in your book? And how would you suggest that people gauge their responses to a given supplement when there are so many and the purported effects are subtle and subjective?”
Yes, we discuss the rationale for supplements in our book. I think if you compare our supplement list to the list of ingredients in a multivitamin, you’ll see that our list is much shorter.
Lithium is a good example. It is one of those compounds we seem to need for optimal health, longevity, and neurological function, yet it is removed from the modern water supply and is depleted in soils by repetitive annual planting of plants in agriculture. Compounding those environmental reductions is the fact that most people don’t eat many vegetables. So it is easy for a diet to be deficient in lithium.
It’s a good practice to stop supplements entirely for a few weeks every once in a while and see if you feel better or worse without them.
Gabe: “I’ve heard you refer to your own experience in dealing with and/or eliminating chronic infections. Can you offer us some insights or advice on the solutions you found to these chronic infections, and/or what kind of medical practitioner one should consult? If one is already seeing a medical practitioner, what kinds of testing would indicate that practitioner is thoroughly considering what you know to be the right kinds of tests?”
My personal solution was PHD plus antibiotics. I would recommend trying PHD (including the lifestyle advice – intermittent fasting, daily exercise, circadian rhythm entrainment) first and trying antibiotics as a last resort.
Testing is a complex question. The patient’s symptoms provide clues, lab tests provide clues, the practitioner has to understand biology and interpret them. There is no recipe that fits every patient, and you can waste a lot of money on uninformative tests. It’s best to find a clinician with good judgment to help you.
Howard Lee Harkness: “Is the “soluble fiber” in chia seed (gel) a suitable “resistant starch” for the PHD? I’ve been experimenting with chia seed gel, and I have noticed that when I eat a serving (about 3 tbl chia seed soaked in 8 oz water about 15 minutes & added to a 20g protein shake with ice, coconut oil and MCT), I am not hungry again for a very long time (12 hours or more). However, I have not noticed any weight loss over the past week. My other main source of soluble fiber is raw carrot (about 1/2 cup per day), which I’ve been trying for about 3 weeks, again with no change in weight. Background: I easily lost a bit over 100 lbs on an Atkins-style diet starting in late 1999, but have remained weight-stable at roughly 50 lbs over goal (give or take about 10 lbs) since 2002.”
I am not familiar with chia seeds, although I do see that they can help rats with dyslipidemia and fatty liver. You might ask Tim and Grace about their resistant starch content.
Kathy from Maine: “1. Tom said at the end of the post, “Perhaps you’ll be persuaded to eat a potato smothered in grass-fed butter.” From my limited reading of PHD, I took away the message that the plan is higher fat (65%), but that fat should come from what naturally occurs in foods and NOT ADDED to foods, like butter on the baked potato, etc. Did I misread this?
2. I’m confused on the 140 degrees. I thought that after the initial cooking and cooling, it was critical that the food NOT be reheated more than 140 degrees to reap the most resistant starch.
3. PHD recommends approximately 15% protein, which on a 2000-calorie diet would be 300 calories, or just 75 grams of protein. How does this correlate to Phinney & Volek’s advice in “Art & Science of LC Living” (and in a podcast I heard from Phinney) that everyone needs three 30-gram servings of protein daily, for a total of 90 – 100 grams or more in order to trigger protein muscle synthesis? In that book, they showed a table of a weight loss plan for a woman, and it advocated 100 grams of protein through all stages of the weight loss from “induction” through maintenance. Also, Dr. Eades notes in his Lifeplan book that women over 50 actually need more protein than men (and recommends at least 100 grams daily) because women of that age don’t absorb as much of the protein as do the men. I’ve always tried to get at least 100 grams a day. Is that too much, in Jaminet’s thinking? Or is 75 – 100 grams a good ballpark figure?”
The recommended PHD macronutrient ratios are 30% carb, 15% protein, 55% fat.
Yes, most fat should come from natural whole foods, but most people will probably eat 2-4 tbsp per day of oils from cooking oil, salad dressing, coconut milk, butter, and other oils. It’s good to put butter or sour cream on a potato.
Resistant starch starts to melt (become digestible) with cooking above the boiling point of water, and the strongest rise in melting occurs between 60˚C and 70˚C (140˚F and 160˚F). Five minutes of cooking at 70˚C / 160˚F will eliminate nearly all resistant starch. It can take several days of refrigeration to restore the resistant starch content.
However, briefly warming a potato in the microwave will not raise the potato temperature to 70˚C, and will not destroy much resistant starch.
It’s true that if you want to maximize muscle mass, you should eat more protein than 15%. However, if you want to maximize longevity, 15% is a good number.
We actually give a peak health range for protein that ranges up to 150 grams (600 calories) per day. So the Phinney & Volek numbers are compatible with PHD. Where you choose to fall within that range is a matter of personal preference.
I’ve seen no evidence that elderly women need more protein than elderly men. All studies of centenarians show that elderly women eat less protein than men, and they outlive the men. It would be strange if they ate less and lived longer even though they needed more.
Amberly: “In creating the most RS from a SS, does it matter how the item is cooked/cooled? IE does it matter if you bake the potato and then eat it immediately after it has mostly cooled (below 140), or does it form more RS if it is baked/boiled then put in the refrigerator overnight, and then reheated? Same type of idea with rice. Does the longer a food is cooled the more RS it creates, or is it pretty much the same?”
General principles, you don’t want starches to become dehydrated. So use gentle water-based cooking methods like boiling or steaming. If you have an autoimmune disease or food sensitivities, favor cooking them in a pressure cooker.
You don’t need to cook starches for a long time to gelatinize them – just cook them as you would normally – but you do need to cool them for a while if your goal is to form extra resistant starch. Refrigerate them at least overnight, and resistant starch content actually continues to increase through 4 to 7 days of refrigeration.
Daci: “What about green bananas as a safe starch? I really miss them since being on a lchf diet. I like them better than ripe ones. Always have. Any thoughts?”
Eat them! Bananas are a great food, green or yellow.
George: “Big fan of PHD and have been incorporating resistant starch particularly in the form of 4 Tbl of Bob’s Red Mill Unmodified Potato starch. Question: Give the nutritional breakdown of 4 Tbl of Potato Starch (160 calories/40 grams of carbohydrate): do does amounts contribute to the PHD minimum levels of starch 400-600 calories per day if this form of starch bypasses digestion in the stomach and small intestine and instead is largely digested by gut bacteria in the large intestine/colon? Or is it recommended to eat some starch that is not “resistant”? If so, how much of “resistant” and Non-resistant starch should be consumed or does it not matter?”
No, resistant starch does not count as a carbohydrate source. It is a short-chain fatty acid source providing about 1 to 1.5 calories fatty acids per gram. It doesn’t provide any carbohydrates. Of course, it is always accompanied by digestible starch in real foods. Those count as carbohydrates.
Yes, you should always combine resistant starch with digestible starch. In general, I think a natural whole foods approach is going to work out best in the end.
General guidelines, you want about 20-25% of calories as digestible starch from “safe starches,” about 10% of calories as sugars from fruits, beets, carrots, and the like, and about 2% of calories from maybe 30 grams of fiber per day, probably about half from resistant starch naturally formed in “safe starches” and half from a diverse array of fruits and vegetables.
Pam: “You have milk as a not to be consumed. But, what about raw milk? I have been drinking raw goat milk for about a year. And then there is the Milk Cure from the early 20th century. Your thoughts?”
Hi Pam, as we say in the book, milk is in many ways close to the ideal food, but our food production system does not inspire confidence in it. I would say you do need confidence in your dairy farmer, that he uses aseptic procedures to prevent contamination of the goat milk by goat dung (easy to occur, in nature the udders are often contaminated by stool as a means to pass maternal gut microbes to offspring) and keeps his goats healthy. There is a risk of infections such as brucellosis. Overall I am somewhat doubtful of the advantages of habitually drinking even well sourced milk, but I don’t have strong feelings about it. It can be curative for some conditions, though a good diet would also generally be curative of those conditions. Milk is simply an easy way to obtain a good diet.
Fight! (Just kidding)
The Internet is large, everyone’s got opinions, and we could waste a lot of time trading opinions. For that reason I think critics should generally be ignored, if all they have is opinions without any specific (which is to say, constructive) criticism.
However, once in a while it may be educational to see what authors think of their opinionated critics, so I thought I’d offer comments on a conversation between Harry and Tom. Harry in bold, Tom in italic, my commentary in regular font:
[Harry:] Paul’s central thesis (that toxins cause disease, and should therefore be minimised) is a leap of faith.
Paul: That is overstating our thesis. First, our diet is primarily focused on nutrient optimization, not toxin minimization. Toxin reduction is a secondary goal; the idea is that given two equally nourishing alternatives, say wheat or white rice, if there is evidence that one is significantly more toxic than the other (in this case, wheat more toxic than rice), we should avoid that one and get the nutrition from the safer source.
[Harry continues:] If toxins do in fact cause disease (that is, chronic consumption of low doses of toxins; we all know that consumption of high doses makes one very ill…or dead), then it simply does not follow that they should be minimised.
Hormesis in the body occurs in many systems, including the digestive/metabolic systems. It would certainly strike us as strange if we surmised that, since working to exhaustion causes death, then lying prone all day is the best way to avoid death. Similarly, it is strange (although understandable) that one might think that toxins should be avoided at all costs. Just like exposure to bacteria challenges and ultimately strengthens the immune system, so too it is possible that exposure to a certain level of dietary toxins is preferable to a completely ‘safe’ diet.
Paul: We discuss hormesis prominently in the book; see pages 192-193 at the beginning of Chapter 18, Food Toxins. The reason we aren’t concerned about the toxins in vegetables is that the doses are usually at hormetic or inconsequential levels.
[Harry:] The resolution to this question ultimately lies with controlled studies…but given the difficulty of assessing variables in the human diet, this may be a long time coming.
Paul: It is virtually impossible to do controlled studies of low-level toxicity. We are concerned about effects that may take a month or two off an 80 year life. To detect such effects would require an experiment lasting at least 80 years.
[Harry:] In the interim, how about we swear off alarmist diet gurus that demonise foods that have been eaten by humans for centuries…and instead just shoot for a balanced diet that is mostly unprocessed foods? Too boring?”
Paul: I object to the claim that we “demonize” any food. No, we weigh the evidence for each food’s merits and demerits, and find some foods wanting.
Harry’s main objection is to our eschewal of certain foods, such as wheat and soy, which have been eaten by humans for centuries. But is it really alarmist to point out that many people have noticed health improvements from removal of wheat, that the biomedical literature notes many cases of people harmed by wheat consumption, that research is exposing mechanisms by which wheat compounds do harm, that statistically countries that don’t eat much wheat tend to have longer lifespans (especially after correcting for income), and that there is no evidence for the presence of nutrients in wheat that cannot be obtained equally well from our “safe starches”?
In order to maximize the healthfulness of a diet – and finding the maximally healthful diet was the purpose of our book, thus the aspirational name “perfect health diet” – we have to weigh risks, such as the loss of sperm in men eating soy, and the cognitive impairment experienced by people eating tofu, against the benefits of eating a food, assessed in an “opportunity cost” sense against alternative food choices. Soy and wheat, in our judgment, do not pass this test.
[Tom Naughton:] A balanced diet of mostly unprocessed food is exactly what he recommends. As for toxins, he’s quite clear that it’s a matter of “the dose makes the poison.” He describes safe starches as low-toxin foods, not no-toxin foods. So I think you’re more in agreement than not.
Paul: Thank you Tom. Exactly right.
[Harry again:] Yes, of course the dose makes the poison. My point exactly.
Paul’s view is that the dose should always be as low as possible. This is where we are getting into pure hypothetical territory. There is a possibility (one that is reasonable given what we know about hormesis) that a dose of certain toxins somewhat higher than the lowest possible is superior in terms of promoting good health (just as exposure to some bacteria is far better for the immune system than living in a sterile environment).
Paul: Again, a mis-statement of our views. We discuss many cases of toxic foods that we recommend eating. For example, on page 195 we discuss the case of a woman who nearly died from eating raw bok choy. We recommend cooking vegetables to reduce toxicity and eating a variety of vegetables, not the same vegetable every day, to reduce toxin dosage. We don’t say, “eat the lowest possible dose of bok choy,” rather, “eat bok choy in moderation prepared in a way that reduces toxicity.”
[Harry:] As I said, it would be wickedly difficult to determine the optimal levels of dietary toxins using the scientific method, but it is just conjecture to argue that since a high dose of toxicity is bad for health, the lowest possible dose should be recommended. This is a classic case where ‘common sense’ (a priori reasoning and induction) does not necessarily yield the truth…hence the need for empirical testing.
Paul: The same straw man again, we don’t make that argument. More empirical testing is desirable, yes, but we have to make decisions about what to eat on the evidence available now. Harry appears to favor the decision rule, “eat everything until empirical testing convicts it beyond a shadow of doubt,” but we prefer our rule, “weigh the evidence and avoid foods that appear to deliver an excess of harm over help.”
[Harry:] I guess I’m just over people running a contestable notion up the flagpole and passing it off as truth. The history of dietary advice is replete with such ideas, which while superficially attractive, turned out to be fruitless.”
[Tom:] Well, I personally like the idea of running a contestable notion up the flagpole. The passing it off as truth part is a different matter.
Paul: Well said Tom.
Forming contestable hypotheses and evaluating evidence pro and con in order to come to judgments of their truth is science. Many judgments are tentative and subject to later correction. Harry here comes perilously close to rejecting science per se on the ground that scientific judgments might later turn out to be have been mistaken.
On the other hand, if it is only duplicitous judgments and foundationless claims that Harry objects to, his objection does not apply to us. We show our reasoning and cite the evidence that supports our conclusions.
However, Harry’s concern may apply to himself. Is he certain he is not spreading foundationless claims about diet book authors on the Internet?
Thank You!
Thank you, Tom, and Fat Head readers for the opportunity to answer your questions. It’s been my pleasure!

















Recent Comments