This is probably the most important and interesting podcast I’ve had the privilege of being part of: an expert panel on Recovering from Autoimmune and Neurodegenerative Diseases.
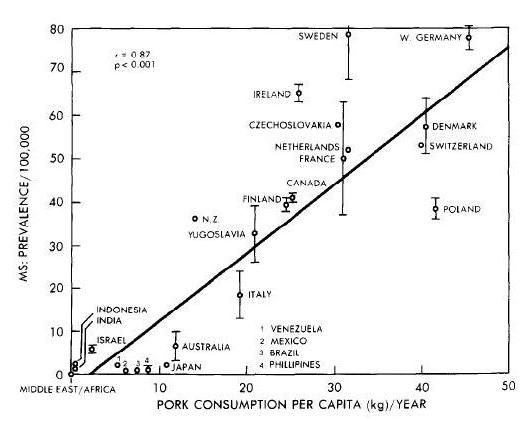
The panel was arranged by Whitney Ross Gray of Nutrisclerosis, who has recovered from Multiple Sclerosis with an ancestral diet rich in animal foods.
The expert panelists were:
- Terry Wahls, M.D., who has famously recovered from Multiple Sclerosis on an ancestral diet rich in plant foods, and is now leading a clinical trial studying ancestral diets as treatments for M.S.
- Sarah Ballantyne, Ph.D., who blogs at The Paleo Mom. Sarah suffered from an autoimmune disease, lichen planus, as well as other ailments, and healed them (and lost 120 pounds) with an ancestral diet.
- Paul Jaminet, Ph.D. I had a chronic disease with neurological symptoms that overlapped with M.S., but it turned out to be an infectious disease and cleared with antibiotics. However, this could not be diagnosed until after I’d made considerable progress addressing it through an ancestral diet, which became the Perfect Health Diet.
Questions were solicited beforehand from patients suffering from autoimmune and neurodegenerative diseases, and in an hour and forty minutes we covered many fascinating topics.
I think the combination of personal experience recovering from chronic diseases, and scientific and medical expertise, made for an exceptionally useful conversation. If you are interested in these diseases – or just in how to be healthy, since the methods that address these conditions are generally beneficial for anyone’s health – take a listen.
My thanks to Whitney for organizing the discussion, Carl for hosting it, and Terry and Sarah for making a great panel.













Recent Comments