I was going to write a single post about how to implement a therapeutic ketogenic (ketone-generating) diet.
But then I thought it was worth spelling out issues in some detail. There are various ways to make a diet ketogenic, and different ways are appropriate in different diseases. Also, different diseases may call for a different balance between three criteria:
1) Safety. Does the diet generate side effects?
2) Therapy. Is the diet as curative as it can be?
3) Pleasurability and practicality. Is the diet unnecessarily expensive, unpalatable, or boring?
I soon realized that with so many factors affecting diet design, it would be hard to fit everything into a single post. So I’m going to split up the discussion into parts. Today I’ll look at the various ways to make a diet ketogenic. On Tuesday I’ll look at how to design a diet for Kindy’s NBIA kids. We’ll look at what they’re eating now, and consider ways they might be able to improve their diets further – and, hopefully, get further improvements in health, longevity, and function.
Maybe we’ll look at some other diseases after that, or maybe I’ll just move on to the lemon juice series I’ve been planning. The lemon juice and acid-base balance issues will fit in nicely since kidney stones and acidosis are risks of ketogenic diets and lemon juice relieves those risks.
So: how can we make a diet ketogenic?
What Is a Ketone?
The liver is responsible for making sure that the body (but especially the brain and heart) have access to a sufficient supply of energy from the blood. To fulfill that responsibility, it manufactures two energy substrates – glucose and ketones – and exports them into the blood as needed.
The most important ketones are acetoacetic acid and beta-hydroxybutyric acid.
Ketones are water-soluble small molecules. They diffuse throughout the body into cells, and are taken up by mitochondria and oxidized for energy.
Ketones are especially important to neurons, which can only consume glucose or ketones. So if something is wrong with glucose metabolism, ketones can be the sole usable energy source of neurons. (Other cell types, but not neurons, burn fats.)
Manufacture of Glucose and Ketones During Starvation
While preparing this post, I was surprised at how long it took for doctors to appreciate that ketones are an acceptable alternative energy source for the brain. The realization that the brain doesn’t perpetually rely on glucose during starvation apparently didn’t sink in until 1967!
The use of prolonged starvation for the treatment of obesity has posed a fascinating problem; namely, that man is capable of fasting for periods of time beyond which he would have utilized all of his carbohydrate resources and all of his proteins for gluconeogenesis in order to provide adequate calories as glucose for the central nervous system.
This study was designed to clarify the apparent paradox, and it was found that beta-hydroxybutyrate and acetoacetate replace glucose as the brain’s primary fuel during starvation. [1]
This makes it a bit easier to understand why ketogenic diets have not yet become standard therapies for neurological diseases. Epileptics caught a lucky break – the ketogenic diet was already in use for epilepsy in the 1920s. The ketogenic diet’s therapeutic potential for other neurological disorders probably couldn’t have been appreciated until after 1967, and by then medicine had turned its back on dietary therapy.
But back to ketones. During starvation, glucose and ketones have to be manufactured from body parts. The body’s resources include:
- Glycogen – a storage form of glucose. However, glycogen supplies are minimal.
- “Complete” protein – a mix of amino acids similar to that found in animal meats.
- Long-chain fats – fatty acids 14-carbons or longer in length, attached to a glycerol backbone as either triglycerides or phospholipids.
During starvation, different raw materials end up as different energy substrates:
- Glycogen can be used to make glucose but not ketones. So glycogen converts 100% to glucose.
- Protein is broken down into its constituent amino acids. Some amino acids can become glucose but never ketones; some can become either; some can become ketones but glucose. “Complete” protein usually found in the body typically converts 46% to ketones, 54% to glucose. [UPDATE: Actually, this is incorrect. As Tony Mach points out in the comments, complete protein converts 20% to ketones, 80% to glucose. The 46-54 ratio is the contribution to Wilder’s ketogenic ratio, see below.]
- Triglycerides and phospholipids are broken up into their constituent parts. The fatty acids can make ketones but not glucose; the glycerol backbones can make glucose but not ketones. Typically, 10-12% of energy from a triglyceride is in the form of glycerol (which has the potential to become glucose) and 88-90% is in the form of fatty acids (which have the potential to become ketones).
As we note in the book, during starvation the body is cannibalizing tissues that are roughly 74% fat, 26% protein by calories. Due to the preponderance of fat, starvation is highly “ketogenic” (ketone generating). The 26% of calories that are protein generate roughly equal amounts of ketones and glucose, but the 74% of calories that are fat generate only ketones.
This doesn’t mean that during starvation ketones are 87% of energy and glucose 13% of energy. Most of the fats are burnt directly for energy without conversion to ketones. But a fair amount of fats are diverted into ketone production, and ketones are abundant during starvation.
A Ketogenic Diet Using “Body Part Foods”
If your diet could include only compounds found in the body – glucose, complete protein, and long-chain fats stored as triglycerides or phospholipids – then we can use the above numbers to estimate the “ketogenic potential” of the diet.
I have to credit commenter “Cathy” at the PaNu Forum for this next part. Kindy posted a question about the ketogenic diet for NBIA on the PaNu Forum in October 2010, and Cathy left an informative comment:
The ketogenic formula was originally developed by Wilder at the Mayo clinic in the 1920’s. By googling WILDER KETOGENIC FORMULA, I found a link to the book “The Ketogenic Diet: A Treatment for Epilepsy” published in 2000. Quite a bit of the book is available for reading online; here is the URL
.
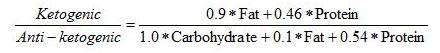
On page 36 of this book is Wilder’s formula for the ketogenic potential of a diet:
This formula basically treats all fats as triglycerides of long-chain fatty acids, and protein as “complete” protein with a typical mix of amino acids. It makes a ratio of the ketone precursors to the glucose precursors.
Wilder’s “ketogenic ratio” was used by Dr. Richard Bernstein in his Diabetes Solution to help people appraise the ketogenicity of a diet. A ratio below 1.5 signifies a minimally ketogenic diet; the higher the ratio goes above 1.5, the more ketones will be generated.
Other Dietary Ketone Precursors
If you’re not starving, you have the opportunity to eat foods that are not components of the body, and that are more ketogenic than “body part foods.”
Specifically, you can eat:
- Short-chain fats such as are found in coconut oil.
- A mix of amino acids that is not “complete,” but is biased toward the ketogenic amino acids.
If you do this then your diet will be more ketogenic than Wilder’s formula would suggest.
Eating these foods may be advantageous. For instance, suppose you want to eat enough carbs to avoid “zero-carb dangers” such as mucus deficiency. At the same time, you want to generate abundant ketones to nourish the brain. You can achieve both by eating carbs for glucose, but also eating short-chain fats and ketogenic amino acids to make ketones.
So let’s look at why these foods are so effective at producing ketones.
Amino Acids
The main metabolic process which converts one metabolic substrate into another is called the citric acid cycle, tricarboxylic acid (TCA) cycle, or Krebs cycle.
The TCA cycle looks like this (blue arrows):
The passage from succinyl CoA to fumarate is where ATP is made. The cycle can be fed in several ways:
- By pyruvate which is an intermediate produced in glucose metabolism;
- By acetyl CoA which is an intermediate produced by ketones or fatty acid oxidation;
- By amino acids which can enter the TCA cycle at various points.
The green boxes show glucogenic amino acids entering the cycle. The white boxes show ketogenic amino acids that are made into either acetyl CoA or acetoacetyl CoA and thence can either leave as ketones (via HMG-CoA) or enter the cycle by conversion of acetyl CoA to citrate.
The crucial takeaway, as far as this post is concerned, is the distribution of amino acids among green and white boxes:
- Leucine and lysine appear only in white boxes, not in green boxes. They are purely ketogenic.
- Isoleucine, tryptophan, phenylalanine, and tyrosine appear in both green and white boxes. They can be either ketogenic or glucogenic.
- The other amino acids appear only in green boxes and are purely glucogenic.
So if the diet is rich in leucine and lysine, but poor in glucogenic amino acids, then it will be highly ketogenic.
Short-Chain Fats
Fats are made into acetyl CoA. Acetyl CoA can either enter the TCA cycle or be converted to ketones. What decides which way it goes?
One important factor is whether the cell has enough ATP. If the cell has plenty of ATP then it won’t allow the TCA cycle to make any more, and the TCA cycle gets stuffed with succinyl CoA and then with all the other intermediates in the pipeline behind it.
Once the TCA cycle is full, acetyl CoA no longer enters the cycle and instead leaves as ketones.
Long-chain fats can follow this route, but not terribly easily. They have alternatives:
- Long-chain fats can serve as structural molecules in cell membranes throughout the body.
- Long-chain fats can be stored in adipose cells.
- Long-chain fats can be burned by cells throughout the body, and transported to cells that need them.
These factors mean that you have to eat a very large amount of long-chain fats before you produce substantial ketones.
Short-chain fats (12 carbons or less in length; often called medium-chain) are different. Short-chain fats do not appear in cell membranes and are not stored in adipose tissue (except for a little 12-carbon fatty acids). Rather than being transported throughout the body, they are shunted to the liver for disposal.
This means that if you eat a lot of coconut oil (which is 58% short-chain fats), you deliver a lot of fat to the liver for disposal. The disposal process for fat is conversion to acetyl CoA followed by either burning in the TCA cycle or conversion to ketones.
After a big cup of coconut oil is delivered to the liver, the liver’s ATP levels are quickly saturated. The TCA cycle is stuffed and the liver will dispose of the coconut oil by making ketones.
It will do this whether the rest of the body needs the ketones or not. The liver wants to get rid of the coconut oil, and it does it by making ketones whether the rest of the body wants them or not.
Summary
So we have three ways to make the diet ketogenic:
1) Make Wilder’s “ketogenic ratio” high by eating a lot of fat, very few carbs, and not too much protein.
2) Supplement with the ketogenic amino acids lysine and leucine.
3) Supplement with coconut oil or another source of short-chain fats.
If we do (2) or (3), then the diet can be ketogenic even if it has a fair number of carbs.
So now we have an arsenal of ways to generate ketones. We have to look at diseases and diet risks to figure out which way of making the diet ketogenic is optimal.
I’ll look at that next week.
References
[1] Owen OE et al. Brain metabolism during fasting. J Clin Invest. 1967 Oct;46(10):1589-95. http://pmid.us/6061736.











hi paul,
my sister has been dealing with epilepsy for years (she’s in her mid-30s). she’s had surgery to remove a brain lesion that was thought to be the culprit and has been on multiple meds. she’s at the point where she either has to accept continuing to have seizures or make friends with the side effects of her meds (mainly extreme dizziness and blurred vision). her seizures are “simple partial”, so she can function well despite them, but obviously not an ideal situation. she sees the implications of diet with her disease, as caffeine and chocolate trigger her seizures, but will not pursue a ketogenic diet as outlined by you. is there anything to suggest that your more traditional PHD would improves things–she may be more inclined to try something like that first. thanks for your thoughts.
Hi Steve,
Ketogenic diets are the gold standard for epilepsy and I’m sorry she’s not interested in our version as it’s a fairly easy ketogenic diet.
The traditional PHD is pretty close. How about traditional PHD with intermittent fasting? She could then try introducing a few tablespoons of MCT oil, which is tasteless, into the daily fast to enhance ketosis.
You don’t need very much ketosis to make a difference, so that might do it for her.
Best, Paul
Hi,
I would like to know if I can do a 21 day water fast with the supplement L-lysine? When I detox durring the fast I want to keep my immune system up so that I don’t get a cold sore while fasting. Does anyone know if its safe to do durring a fast?
Hi cris,
Personally, I would separate the two issues. I think using short-chain fatty acids is a safer way to generate ketosis. Any lysine you take as an anti-viral therapy you can take on the side. Lysine might have negative effects, every immunomodulatory substance helps against some infections but hurts against others. Also, arginine:lysine ratio can be important for some processes so unbalancing it may have side effects. I wouldn’t go overboard on the lysine.
Best, Paul
Hi Paul,
I read this post a while back and I’m reading through it again now. I’ve been wondering about the possibility of diabetics benefitting from having at least minimal amounts of ketones. Of course usually the concern for diabetics is ketoacidosis, if ketone levels were very high causing the pH of blood to go too low– apparently very dangerous. But recently I read that ketoacidosis would likely only happen if ketones were very high AND blood sugar was high. I don’t know much about that though. Anyway, back to what I meant to write about… so, I wasnt thinking actually about ketoacidosis, but rather, about the extreme blood sugar lows that diabetics sometimes experience. And of course, if their blood sugar goes severely low, they could have a seizure, then, if not tended to quickly, they could go into a coma, then possibly death. I have gone into a seizure one time, about 6 or 7 years ago but I thank God that a roommate found me and put some hard candy under my lip to absorb the sugar. In any case, I was wondering… if there had been ketones present, wouldn’t that have been enough fuel for the brain to prevent a seizure? Is it that simple (probably not…)? But if it were true, then it would seem to me that for diabetics, as long as their blood sugar is well controlled, having a small or moderate amount of ketones could be helpful in those rare cases of extremely low blood sugar. But, I’m sure there’s a lot more involved than just this… I just don’t know much of the mechanics of it all yet.
Oh- disclaimer for you- this is not me seeking any kind of diabetic advice. I’m just curious what knowledge you have about this and if you know of any studies done or if you’ve heard of anything like this before? Or… if you might be able to explain the mechanics of why my idea just wouldnt work (because of this thing blocking that thing or a lack of something in diabetics, etc.). Sorry, I really don’t know scientific jargon– I can sometimes just barely read these posts! But they’re great and I’m learning!
Thanks for your input,
KH
Hi KH,
Yes, ketones alleviate hypoglycemia and will prevent hypoglycemic seizures.
However, if you do get into a seizure, be sure to take a carb source, because ketones will be generated too slowly from (say) coconut oil. Glucose enters the bloodstream immediately.
I have gone back and forth on whether mild ketosis may be helpful for diabetics. I wouldn’t recommend it as a routine thing but it might be helpful intermittently, as in intermittent fasting with a bit of coconut oil.
A healthy, nourishing diet without a caloric excess or what I will call “useless macronutrients” in my obesity series is the key for diabetes. Ketones may have a place in helping manage glucose regulation, but I think there’s not enough data to tell yet.
Best, Paul
Thanks Paul,
I was actually thinking about long- term mild ketosis for the purpose of prevention of seizure (not as an immediate remedy to the seizure since I know that wouldn’t work), in other words, that the presence of ketones already in the body would prevent a seizure if blood glucose levels dropped severely low. And of course the hypoglycemia would still need to be dealt with immediately, but if I had to choose between severe hypoglycemia without ketones already present, resulting in a seizure (and hoping someone is around to give me something) OR severe hypoglycemia with ketones already present, and therefore no seizure (but rather, being conscious and getting myself some sugar or something) well of course I pick no seizure. But I don’t really know if this scenario would actually play out like that (don’t worry, I’m not going to try it!). And I know you guys said before to another poster that you have limited experience/ knowledge with diabetes, but I just wanted to get your thoughts on the theoretical idea.
As for my own personal experience (I’m type 1), I am trying to produce mild ketones for my brain, but according to the Ketostix, I haven’t been very successful. Only two times it showed up as “trace” ketones, the rest have all been negative. (However, I have been taking only a small amount of coconut oil, so maybe that’s why.) And I don’t know how accurate the ketostix are. But I do keep a close eye on myself and check blood sugar all day long, usually 8- 10 times a day. And I do always have glucose tablets with me which do work fast. So, I would and do definitely take those when I’m low.
Thanks for your quick response!
Very appreciated!
KH
Hi KH,
I think ketosis makes more sense for Type Is than for Type IIs.
But you don’t really want such a strong ketosis that you’re excreting a lot of ketones in urine. That’s an excess beyond what your body can use and it promotes infection and acidifies the body.
So you might have been doing just the right amount of ketosis, or too little. You might experiment with adding coconut oil until you see low levels of ketones in the urine consistently, and then cut back to the point where they disappear from the urine.
Best, Paul
Hi Paul,
During my last pregnancy I was eating a lot of carbs with some fat, not much protein. When I did the peeing on the stick to test for various things like hydration etc, it always showed that I was excreting ketones unless I ate within an hour of testing.
I figured this is because of a fast metabolism, not really understanding ketones at all. Since I was eating high carb, low fat, assuming I wasn’t in ketosis… is there another reason to be eliminating ketones out of the urine? Not sure if it makes sense to do a ketosis diet if my body is already excreting ketones.
Thanks
Ok, thanks Paul. I will keep researching it and see what I can come up with. Honestly, almost everything I find that includes ketosis and type 1 diabetic in the same sentence sounds horrible, but I’m trying to find some good unbiased sources if I can (versus the kind of sources that say that as a type 1 diabetic I should absolutely be on an ACE inhibitor, statins and who knows what else– I’m so tired of hearing that). No thank you!
So, I’ll let you know if I come to any great conclusion.
I had another random thought on the other side of the coin– I might stop coconut oil, reduce fat intake and up carbs and see if my dizziness goes away (it’s not spinning like vertigo, more like gently swaying, it’s been mild, but annoying, for a few months now). So, of course that would mean no ketosis. I’ll try it and see what happens. I really just want the dizziness to go away (by the way, it’s not hypoglycemic related– I can find no rhyme or reason to its occuring– everyday, random moments, actually almost all day long). The dizziness was one reason (at first) that I thought ketosis might help get rid of the dizziness (if it were a bacterial brain infection). That was my thinking. But, might as well try the opposite– totally eliminate possible ketosis– and see if I improve.
Sorry I’m all over the place here!
Thanks much!
KH
Hi KH,
Yes, you have to experiment. You can also try carbs and coconut oil at the same time, they’re not mutually exclusive.
Best, Paul
Hi,
This may not be the right thread thread to ask this but I saw a soup recipe to boil bones in “acidified water”. I did some finds and dont know what “acidified water” means. Never heard the term and did some searches to no luck. Does anyone know what it means?
Thanks
Hi John,
It means if you put some acid — lemon juice, vinegar, tomatoes, or red wine are the usual choices — in the water, then the acid will leach minerals from the bone and give you some extra nourishment and flavor.
Hi Paul,
I have been adding a fat (butter/olive/coconut oil),lemon/lime, vinegar to rice and butter/olive oil and vinegar to potatoes as you have suggested. Does taste great and seems to reduce inflammation after meals. I have been using balsamic vinegar typically, is this ok? Do you recommend a different type of vinegar?
Hi SC,
Balsamic vinegar is fine, any form of vinegar will do.
10-4, thx Paul
Doesn’t balsamic vinegar have a lot of sugar in it?
I was on a paleo diet but never saw any benefits from it.
I have a fatty liver and was told this diet would help it but I also have no gallbladder and was wondering if the diet would still help the fatty liver condition?
Thanks
Hi Cheryl,
Yes, our diet will help a fatty liver.
Keys are reducing polyunsaturated fat and fructose (alcohol too if excessive), and improving nutrient status.
Then fixing gut dysbiosis and infections.
Without a gallbladder you may benefit from increasing carbs and taking oxbile supplements with meals. But in general, you can still do well on this diet.
Best, Paul
Did you ever list risks etc and contiue with this? I cannot find anything else. Thanks S
Hi Sherie,
Check out our ketogenic category: http://perfecthealthdiet.com/category/diets/ketogenic_diet/
Most of our discussion of the risks of poorly designed ketogenic diets can be found in our “zero carb dangers” series: http://perfecthealthdiet.com/category/zero-carb-dangers/, go back to the older posts. A well designed ketogenic diet should include some starchy carbs and adequate protein.
Hi
What is your opinion of supplementing with acetyl-L-carnitine (ALC)? Can it be of benefit making ketones or is it of harm in this process? I´ve read on my MCT-oil bottle that if/when you have a great intake of the MCT oil, one should supplement with ALC
Well, vitamin C is an ALC precursor and eating a fat-rich diet promotes ALC generation, so I think everyone following our diet+supplements should have plenty of natural ALC. And the supplements are kind of expensive. I don’t think they’re necessary. But I don’t think they’re toxic either, so if you want to try them go ahead. But I doubt they’ll have any discernible effect.
Hi Paul,
I just wanted to clarify a couple of things in regards to making PHD ketogenic for treating depression.
How long should you do it for to see what the effects are on depression?
I will be consuming a normal ammount of PHD carbs (More on weight training days afer training) and want to maintain ketones – Will 12 tablespoons of Coconut oil do it?
Is timing of taking the coconut oil important throughout the day?
Along with the coconut oil consumption should I also consume lysine? leucine? BCaa’s? All of them? – How much of each per day and is timing important for those too?
Thanks Paul, I really want to get it right without it being detrimental to my training aspirations!
Hi MartB,
Effects should be very rapid if excitotoxicity or some genetic issue with glucose metabolism is the problem. A week should be a sufficient test.
Yes, 12 tbsp coconut oil or 8 tbsp MCT oil would be plenty. If the KD would have an effect, that would show it. Then if it does, reduce the dose to find the minimum effective intake of MCT oil/coconut oil.
It should be spread through the day, but take some during your overnight fast.
Leucine/BCAAs are helpful to combine with it. 5 g /day is good. No timing is not important, take them with food.
Hi Paul,
So would taking MCTs like coconut oil on a fast be of any effect or is it useless.
Ps. What’s your take on types of fats? Conventional advice given by the govt (a laugh, I know) favors polyunsaturated but I’m starting to feel that short or long; unsaturated or saturated doesn’t make so much of a difference as a balance of each.
So long as it isn’t hydrogenated.
I’ve seen people on an EVOO only diet and their skin isn’t any better than people who enjoy animal fat as well.
I have NBIA What diet would work for me
Hi Paul,
First, a big thank you for the wonderful work you and Shou-Ching are doing.
I started on the ketogenic version of PHD about 3 weeks ago since I have IBS, ADHD and experience anxiety.
I’m having a few issues and thought you could help me with them.
First, I experience extreme GI distress when I take the MCT oil. This doesn’t happen with coconut oil. I tried taking MCT oil during the 16-hour fast, but I can only tolerate it in small amounts with food. My aim is 4 tablespoons as you mention in your book.
How much coconut oil would I have to ingest to induce ketosis? I am eating only 200 calories of carbs a day.
Second issue is I’m gaining weight! I have about 15 lbs to lose, and I am post-menopausal. I work out according to the recommendations in your book,and presently I’m only eating 2 meals per day…I’m not hungry! Perhaps this weigh gainn will subside with time.
I look forward to your response,
Sherie
Hi Sherie,
I generally recommend eating the regular diet for a few months to get acclimated, before experimenting with the ketogenic diet. The ketogenic diet can make things better or worse, and it is good to do a controlled experiment to in which going into ketosis is the only thing you change.
It is hard to say how much coconut oil you would need because it depends on how much you are eating. Slight calorie restriction can make it very easy to enter ketosis. Some resistant starch can also help, but that may be counter-indicated due to your IBS. You should definitely do intermittent fasting, and considering lengthening the period of your fast. That will help reshape the gut flora. But 4-6 tablespoons coconut oil is usually enough.
The ketogenic diet does make you eat more calories, so it is easy to put on weight with it. That is another reason to delay it until you know that our regular diet won’t work by itself. Usually it does.
For some guidance on weight loss, search the blog for “Weight Loss Version.” Also, circadian rhythms are important; and take extra vitamin C, optimize vitamin D, and eat some liver for vitamin A.
Best, Paul
Dear Paul
Many thanks for your prompt reply! I did try the regular version of PHD but was having digestive difficulty with all the safe starches. I am taking your recommended supplements. I think I may hang in there with the ketogenic version now that I quit taking MCT oil.
I am feeling strong and clear-headed, and the fasts are easy for me. I appreciate all your help!
All the best,
Sherie
Hello Paul
Sorry for my ignorance but ref Ketogenic Diet in book
you state at least 200 carb calories.
I looked on NutritionalData website but am still confused.How many weight grammes in Potatoes does this calculate out to be is it 50 ?
Thankyou for all your hard work
Marcus
Hi Marcus,
That would be about 1/2 pound or 1/4 kg potatoes.
Leucine and lysine help you produce more keytones for therapeutic uses, but what about weight-loss? Are they effective in that regard?
Hi Laura,
No, I wouldn’t consider them valuable for weight loss, although leucine will help preserve muscle on calorie-restricted diets.
thank you so much for the reply! I’ve been wondering.
If you have any gallbladder symptoms, you should take a close look at what you eat everyday. For example, cholesterol is the prime culprit in gallbladder disease. Although a very small amount of cholesterol is necessary for good health, your liver naturally produces all the cholesterol you will ever need. However, other animals produce cholesterol too. When you eat meat and dairy foods, you take in their cholesterol which causes your cholesterol to skyrocket. And as explained above, eating cholesterol can and does lead to gallstones and disease.
I have just started reading your book and I can’t work out whether a therapeutic ketogenic diet for a neurological condition such as MS is something if it helps needs to be done long term/ongoing or only until symptoms improve? Many thanks
Hi Paul,
I have been on the PHD for around 4 months now since becoming very ill last year with severe fatigue, digestive issues, weight loss, liver pain, back pain, depression and anxiety. I have made a lot of progress, along with seeing a naturopath who has been helping me with supplementation and detoxification. However, I feel like I have plateaued and am still experience anxiety, fatigue and pain. I seem to go up and down and have noticed a pattern with regards to fructose. If I eat a banana, I feel sick and have increased fatigue and pain. I am toying now with implementing the ketogenic diet and since I stopped all fructose I have less pain and fatigue. Does this add up? And will I ever be able to have fructose again? Eg, would berries be okay to eat on a ketogenic diet? Also, are the branched aminio acids, you say in the book to supplement with, a must? Thank you so much for all your help thus far. Your book has been a god send for me!
Ali
Hi Paul,
Great thread and explanation of exactly how ketosis works. I’d love your opinion on something. I’m homozygous for the ApoE4 variant. Lots of research and experimentation reveals that my genotype tends to react to SFAs with a dramatic rise in LDL-C and LDL-P. Could I achieve even mild ketosis using primarily MUFAs?
As you know, my genotype puts me at very high risk of developing Alzheimer’s. My Neurologist indicates that a mildly ketogenic diet could be neuroprotective and may help me avoid dementia.
I’d live to hear your thoughts on using heavy MUFAs to achieve this goal.
Thanks in advance for your help-
Julie
Hi Paul,
I’m just starting out with the ketogenic diet and am astounded with how much fat I need to eat compared to how little protein. I did the Kenton calculator thing and it said I (165 lbs at 5’3) need 25 g carbs, 120 g protein, and 170 g fat!! So, basically, have a meat salad and then shovel coconut oil into my mouth for the rest of the day? Also, is there a way to buy this coconut oil for cheap?
Hi Paul,
I suffer from hypoglycemia eating the SAD. I suspected reactive hypoglycemia but got very confused when I went to the hospital. I even did a test there and found out I also have nocturnal hypoglycemia (the whole night I have levels in the 40’s) and also spend my whole having hypoglycemic levels after eating – also in the low 40’s. However I don’t have an insulinoma, and doctors didn’t detect high insulin levels. They are not familiar with the paleo diet and only know the standard medical advices. Since nobody could help me I started researching for my own and found out about the paleo diet.I follow the Perfect Health Diet now and my symptons improved alot, my hypoglycemia during the day no longer exists. Even though everything is better I would like to understand this… what happens now is that during the night from 2am to 3am I even have numbers in the 100. Every single night. And when I wake up in the morning now I have low fasting levels (65 to 70). Before this I never had low fasting levels, my hypoglycemia was only after eating and during the night. Do you have any idea why this happens? Please it would mean alot to me if you could help me I’m really confused
Hi Paul,
I was wondering about the amino acids. I am following a ketogenic diet often, but my protein shake has a large added amino acid complex, many of which are glucogenic.
My question is, considering that the shake is very low carbohydrate (3g), will consuming glucogenic amino acids hinder my ketosis state at all?
Thank you x
Hi Jamie,
Yes, they’ll tend to inhibit ketone production, but you need protein for nourishment as well. You don’t want to achieve ketosis through starvation, that will be harmful. That raises the question of why you are following a ketogenic diet, and whether you can notice whether you are in ketosis or not. If ketosis relieves headaches, for instance, you can adjust coconut oil or MCT oil dose to get rid of the headaches, and experiment to find how much you have to raise MCT oil dose when you raise protein and carbs. If you can’t tell whether you are in ketosis, then you probably shouldn’t be doing a ketogenic diet, as it probably won’t have benefits for you.
Hello,
I’ve heard differing opinions on whether keto is the best route for people with autoimmune disorders–particularly MS. What is your opinion?
I have both MS & RA and have been AIP for 2 yrs.
Many thanks
Hi Tracie,
I think it’s a poor place to start, but it’s not bad to try a controlled experiment after you’ve put in place all the things that are more reliably positive.
Keto is not curative for autoimmunity, but it might help against some infections (while hurting against others), and it also can help people with certain genetic defects. Often when people have “autoimmune disease” they also have chronic infections or gene mutations; “autoimmune” can be a diagnosis of ignorance. Depending on your situation, then there is a chance it could help, but it can also hurt, so you need to experiment in a careful way.
PHD, both diet and lifestyle, would be a good place to start before considering a test.
Best, Paul
Thanks for your prompt reply, Paul.
I appreciate your candidness and honesty. I see a functional medicine MD so am aware of all of my interesting genetic defects. 😛
They’ve never mentioned keto, but I’ll make sure and inquire after their opinion at my next appt.
I have been noticing many people pushing keto for autoimmunity in social media circles and thought I’d ask someone who recently addressed it (Robb Wolf podcast #233).
Thanks again for your most informative and useful work and information.
Most graciously,
Tracie
Hi my son is 11 and paralysed t1 .. Would this diet help him !? What qould you recomend ? Thank you . Emma
Hi Emma,
You are saying he is type I diabetic and already paralyzed? Our diet will help everyone, in type I diabetics a lower carb version is optimal, but it is very difficult to reverse paralysis. At least you can minimize the chance of further damage, and maybe get some healing of peripheral nerves over several years. Get him on a lower-carb version of our diet and control his blood glucose as best you can with the right doses of insulin. Supplement vitamin B12 to encourage nerve regrowth (methylcobalamin). Help him find daily exercises he can do — search on things like “paraplegic exercise”.
Best, Paul
I think she means T1 level or paralysis:
http://www.apparelyzed.com/support/functionality/t1-t4.html
Thank you Nick!
Hi Emma,
Sorry, I misunderstood. Injuries as high as the thoracic spinal cord are hard to heal. It is difficult to regenerate a severed nerve, much less a severed spinal cord, but several types of paralysis can be at least partially repaired, partly through replacement of dead nerve cells which is a ~2 year process involving migration of stem cells along the spinal cord and nerves, and partly through retraining of the brain (there is a phenomenon called learned paralysis which is often part of the problem in stroke).
Apart from possibly repairing part of the paralysis, the diet would help the rest of his body remain healthy. Because paralysis tends to lead to lack of activity, it is especially important to eat well and learn how to live in a proper way.
Best, Paul
Hi Paul
Before I ask my question, I would just like to say thank you for all the work you do replying to questions on this blog and for an excellent book. Now on to my question!
I notice here that you say supplementing with coconut oil can turn a diet ketogenic and as I understand it the consumption medium chain fatty acids in general encourages ketone production? However, in your book you mention eliminating fructose sources from the diet as fructose metabolism depletes the liver of ATP and reduces its production of ketones? We have been adding coconut oil to a smoothy that often has carrot and blueberries to help my father who has heart disease and neurological problems from strokes (and possibly statins(?) that he takes). So I’m wondering whether we can get away with smaller amounts of fructose or whether even the slightest amount may cause problems?
Many thanks.
Pete
I think some carrots and blueberries are OK. The more fructose, the more coconut oil you need for ketogenesis, but you don’t want to totally remove pleasure from your diet.
However, I don’t think heart disease and strokes indicate a ketogenic diet. I would just have your father do regular PHD.
Hi Paul
That is good news thank you, but it does leave me a little confused. I had the impression from your chapter on therapeutic ketogenic diets that it would be better because it mentions the heart’s hydraulic efficiency being better on ketones. Are you saying it is enough to supplement with the two table spoons a day to achieve that kind of benefit?
I really do appreciate the time you spend to answer these questions.
Looking forward to hearing from you.
Pete
Paul, in your August 1 reply to Emma, you mention a 2- year process involving migration of stem cells and replacement of dead nerve cells. Is this a natural physiological process of healing, or were you referring to stem cells replacement therapy?
Natural.
Hi Paul,
Thanks for all the work that you do. I have been following the PHD for quite some time. About one year ago I began a modified ketogenic diet to address neurodegenerative issues. I began to supplement with coconut oil (approximately 5 tablespoons per day), and I feel great. My neurological symptoms related to dystonia have substantially improved. However, a few months ago I developed persistent acne on my face. Could the increase in saturated fat from the coconut oil have caused this acne condition?
Thank you,
Rob
Yes. Supplement pantothenic acid 1 g per day, plus eat your liver weekly, 3 egg yolks daily, and supplement zinc and maybe phospholipids/lecithin. You need to provide micronutrients to dispose of the fat.
Hello Paul,
I’m interested in a ketogenic diet for my chronicle migraine. My problem is that I get palpitations whenever I consume coconut oil. Any suggestions or advice is highly appreciated. I’ve read about taking taurine & l-arginine to relieve palps but I get headaches when taking them, not sure if it’s caused by the combination or one of them. I’ve tried l-arginine a lone & it doesn’t seem to cause me headache on its own. I haven’t had the chance yet to try taurine alone as I’ve been having headaches a lot lately.
Hi Paul,
I’m thinking of trying the ketogenic diet outlined on page 158 as a shot in the dark to cure or help remove mental roadblocks which I feel I’ve had all my life. Maybe that seems strange, but right now I have the time and discipline to do it, so I’d like to try. I have some questions.
Cutting out all fructose – no fruit or sweet vegetables either?
Should my overall calories stay about the same?
I do a 30 min intense bicycle ride every other day – will that be dangerous?
Since this is an experiment, how much time do you think I should give it before I quit for lack of results?