I was going to write a single post about how to implement a therapeutic ketogenic (ketone-generating) diet.
But then I thought it was worth spelling out issues in some detail. There are various ways to make a diet ketogenic, and different ways are appropriate in different diseases. Also, different diseases may call for a different balance between three criteria:
1) Safety. Does the diet generate side effects?
2) Therapy. Is the diet as curative as it can be?
3) Pleasurability and practicality. Is the diet unnecessarily expensive, unpalatable, or boring?
I soon realized that with so many factors affecting diet design, it would be hard to fit everything into a single post. So I’m going to split up the discussion into parts. Today I’ll look at the various ways to make a diet ketogenic. On Tuesday I’ll look at how to design a diet for Kindy’s NBIA kids. We’ll look at what they’re eating now, and consider ways they might be able to improve their diets further – and, hopefully, get further improvements in health, longevity, and function.
Maybe we’ll look at some other diseases after that, or maybe I’ll just move on to the lemon juice series I’ve been planning. The lemon juice and acid-base balance issues will fit in nicely since kidney stones and acidosis are risks of ketogenic diets and lemon juice relieves those risks.
So: how can we make a diet ketogenic?
What Is a Ketone?
The liver is responsible for making sure that the body (but especially the brain and heart) have access to a sufficient supply of energy from the blood. To fulfill that responsibility, it manufactures two energy substrates – glucose and ketones – and exports them into the blood as needed.
The most important ketones are acetoacetic acid and beta-hydroxybutyric acid.
Ketones are water-soluble small molecules. They diffuse throughout the body into cells, and are taken up by mitochondria and oxidized for energy.
Ketones are especially important to neurons, which can only consume glucose or ketones. So if something is wrong with glucose metabolism, ketones can be the sole usable energy source of neurons. (Other cell types, but not neurons, burn fats.)
Manufacture of Glucose and Ketones During Starvation
While preparing this post, I was surprised at how long it took for doctors to appreciate that ketones are an acceptable alternative energy source for the brain. The realization that the brain doesn’t perpetually rely on glucose during starvation apparently didn’t sink in until 1967!
The use of prolonged starvation for the treatment of obesity has posed a fascinating problem; namely, that man is capable of fasting for periods of time beyond which he would have utilized all of his carbohydrate resources and all of his proteins for gluconeogenesis in order to provide adequate calories as glucose for the central nervous system.
This study was designed to clarify the apparent paradox, and it was found that beta-hydroxybutyrate and acetoacetate replace glucose as the brain’s primary fuel during starvation. [1]
This makes it a bit easier to understand why ketogenic diets have not yet become standard therapies for neurological diseases. Epileptics caught a lucky break – the ketogenic diet was already in use for epilepsy in the 1920s. The ketogenic diet’s therapeutic potential for other neurological disorders probably couldn’t have been appreciated until after 1967, and by then medicine had turned its back on dietary therapy.
But back to ketones. During starvation, glucose and ketones have to be manufactured from body parts. The body’s resources include:
- Glycogen – a storage form of glucose. However, glycogen supplies are minimal.
- “Complete” protein – a mix of amino acids similar to that found in animal meats.
- Long-chain fats – fatty acids 14-carbons or longer in length, attached to a glycerol backbone as either triglycerides or phospholipids.
During starvation, different raw materials end up as different energy substrates:
- Glycogen can be used to make glucose but not ketones. So glycogen converts 100% to glucose.
- Protein is broken down into its constituent amino acids. Some amino acids can become glucose but never ketones; some can become either; some can become ketones but glucose. “Complete” protein usually found in the body typically converts 46% to ketones, 54% to glucose. [UPDATE: Actually, this is incorrect. As Tony Mach points out in the comments, complete protein converts 20% to ketones, 80% to glucose. The 46-54 ratio is the contribution to Wilder’s ketogenic ratio, see below.]
- Triglycerides and phospholipids are broken up into their constituent parts. The fatty acids can make ketones but not glucose; the glycerol backbones can make glucose but not ketones. Typically, 10-12% of energy from a triglyceride is in the form of glycerol (which has the potential to become glucose) and 88-90% is in the form of fatty acids (which have the potential to become ketones).
As we note in the book, during starvation the body is cannibalizing tissues that are roughly 74% fat, 26% protein by calories. Due to the preponderance of fat, starvation is highly “ketogenic” (ketone generating). The 26% of calories that are protein generate roughly equal amounts of ketones and glucose, but the 74% of calories that are fat generate only ketones.
This doesn’t mean that during starvation ketones are 87% of energy and glucose 13% of energy. Most of the fats are burnt directly for energy without conversion to ketones. But a fair amount of fats are diverted into ketone production, and ketones are abundant during starvation.
A Ketogenic Diet Using “Body Part Foods”
If your diet could include only compounds found in the body – glucose, complete protein, and long-chain fats stored as triglycerides or phospholipids – then we can use the above numbers to estimate the “ketogenic potential” of the diet.
I have to credit commenter “Cathy” at the PaNu Forum for this next part. Kindy posted a question about the ketogenic diet for NBIA on the PaNu Forum in October 2010, and Cathy left an informative comment:
The ketogenic formula was originally developed by Wilder at the Mayo clinic in the 1920’s. By googling WILDER KETOGENIC FORMULA, I found a link to the book “The Ketogenic Diet: A Treatment for Epilepsy” published in 2000. Quite a bit of the book is available for reading online; here is the URL
.
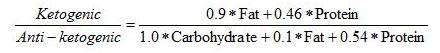
On page 36 of this book is Wilder’s formula for the ketogenic potential of a diet:
This formula basically treats all fats as triglycerides of long-chain fatty acids, and protein as “complete” protein with a typical mix of amino acids. It makes a ratio of the ketone precursors to the glucose precursors.
Wilder’s “ketogenic ratio” was used by Dr. Richard Bernstein in his Diabetes Solution to help people appraise the ketogenicity of a diet. A ratio below 1.5 signifies a minimally ketogenic diet; the higher the ratio goes above 1.5, the more ketones will be generated.
Other Dietary Ketone Precursors
If you’re not starving, you have the opportunity to eat foods that are not components of the body, and that are more ketogenic than “body part foods.”
Specifically, you can eat:
- Short-chain fats such as are found in coconut oil.
- A mix of amino acids that is not “complete,” but is biased toward the ketogenic amino acids.
If you do this then your diet will be more ketogenic than Wilder’s formula would suggest.
Eating these foods may be advantageous. For instance, suppose you want to eat enough carbs to avoid “zero-carb dangers” such as mucus deficiency. At the same time, you want to generate abundant ketones to nourish the brain. You can achieve both by eating carbs for glucose, but also eating short-chain fats and ketogenic amino acids to make ketones.
So let’s look at why these foods are so effective at producing ketones.
Amino Acids
The main metabolic process which converts one metabolic substrate into another is called the citric acid cycle, tricarboxylic acid (TCA) cycle, or Krebs cycle.
The TCA cycle looks like this (blue arrows):
The passage from succinyl CoA to fumarate is where ATP is made. The cycle can be fed in several ways:
- By pyruvate which is an intermediate produced in glucose metabolism;
- By acetyl CoA which is an intermediate produced by ketones or fatty acid oxidation;
- By amino acids which can enter the TCA cycle at various points.
The green boxes show glucogenic amino acids entering the cycle. The white boxes show ketogenic amino acids that are made into either acetyl CoA or acetoacetyl CoA and thence can either leave as ketones (via HMG-CoA) or enter the cycle by conversion of acetyl CoA to citrate.
The crucial takeaway, as far as this post is concerned, is the distribution of amino acids among green and white boxes:
- Leucine and lysine appear only in white boxes, not in green boxes. They are purely ketogenic.
- Isoleucine, tryptophan, phenylalanine, and tyrosine appear in both green and white boxes. They can be either ketogenic or glucogenic.
- The other amino acids appear only in green boxes and are purely glucogenic.
So if the diet is rich in leucine and lysine, but poor in glucogenic amino acids, then it will be highly ketogenic.
Short-Chain Fats
Fats are made into acetyl CoA. Acetyl CoA can either enter the TCA cycle or be converted to ketones. What decides which way it goes?
One important factor is whether the cell has enough ATP. If the cell has plenty of ATP then it won’t allow the TCA cycle to make any more, and the TCA cycle gets stuffed with succinyl CoA and then with all the other intermediates in the pipeline behind it.
Once the TCA cycle is full, acetyl CoA no longer enters the cycle and instead leaves as ketones.
Long-chain fats can follow this route, but not terribly easily. They have alternatives:
- Long-chain fats can serve as structural molecules in cell membranes throughout the body.
- Long-chain fats can be stored in adipose cells.
- Long-chain fats can be burned by cells throughout the body, and transported to cells that need them.
These factors mean that you have to eat a very large amount of long-chain fats before you produce substantial ketones.
Short-chain fats (12 carbons or less in length; often called medium-chain) are different. Short-chain fats do not appear in cell membranes and are not stored in adipose tissue (except for a little 12-carbon fatty acids). Rather than being transported throughout the body, they are shunted to the liver for disposal.
This means that if you eat a lot of coconut oil (which is 58% short-chain fats), you deliver a lot of fat to the liver for disposal. The disposal process for fat is conversion to acetyl CoA followed by either burning in the TCA cycle or conversion to ketones.
After a big cup of coconut oil is delivered to the liver, the liver’s ATP levels are quickly saturated. The TCA cycle is stuffed and the liver will dispose of the coconut oil by making ketones.
It will do this whether the rest of the body needs the ketones or not. The liver wants to get rid of the coconut oil, and it does it by making ketones whether the rest of the body wants them or not.
Summary
So we have three ways to make the diet ketogenic:
1) Make Wilder’s “ketogenic ratio” high by eating a lot of fat, very few carbs, and not too much protein.
2) Supplement with the ketogenic amino acids lysine and leucine.
3) Supplement with coconut oil or another source of short-chain fats.
If we do (2) or (3), then the diet can be ketogenic even if it has a fair number of carbs.
So now we have an arsenal of ways to generate ketones. We have to look at diseases and diet risks to figure out which way of making the diet ketogenic is optimal.
I’ll look at that next week.
References
[1] Owen OE et al. Brain metabolism during fasting. J Clin Invest. 1967 Oct;46(10):1589-95. http://pmid.us/6061736.











Paul,
Very interesting. Seems like eating a lot of coconut oil will cause the liver to do extra work. Does this present any concerns in your opinion?
Hi
I’m interested in the liver/coconut oil question too. I had some liver problems a few years back. Does everyone benefit from the process described, even if your liver is not functioning normally? My concern is excess weight around the middle. I have had successful weight loss everywhere except around the middle despite being low carb for over a year (50g a day or less).
Ketone production is only beneficial if the ketones are accessible to neurons. Do you know if neurons preferentially utilize ketones over glucose?
My first thoughts were concerning the liver as well.
What are things that are helpful for the liver?
I guess eating less toxins (that have to be metabolized by the liver) is a good idea with regards to the liver, e.g. less sugar/fructose, less alcohol.
Any other thoughts?
I keep reading about magnesium and how the body needs it to produce over 300 enzymes, I guess that includes liver enzymes? What are your thoughts on supplementing magnesium to its RDA with regards to the liver? Any other supplements you think are helpful for the liver and/or a ketogenic diet?
And of course eating liver (cow-, chicken- or pork-) once or twice a week is a excellent idea, from my point of view. It think it contain all the building blocks the human liver needs and I guess in a good ratio (but plus some carbs, so it might be more anti-ketogenic…).
As a side note, for the carbs, my favorite is plantains – have to try to fry them in coconut oil :-). They are mainly starch, no sugar, no fructose and if they are green no glucose. I hope the content of antinutriens is low, but I don’t know.
One more thought: The liver consumes ATP when metabolizing fructose AFAIK, so if you keep fructose/sacharose-suger intake low, you should keep ATP levels high in the liver and that should be helpful for a ketogenic diet. Am I right?
And a rough (back of an envelope / back of my head) calculation: Meat protein is around 16% ketogenic aminos (Lysine and Leucin), around 14% of ketogenic or glucogenic aminos. I couldn’t find numbers for all the pure glucogenic aminos, so I can only account for around 53% of the remaining 70%. (One has to probably make a weighted sum anyway…)
I’m not an expert in biochemistry, but my guess would be that meat protein is around 20% ketogenic aminos and around 80% glucogenic aminos (give or take some percent), but I might be wrong and might not know some important steps to do such a calculation…
Hi Todd,
I don’t think so – rather the opposite. Saturated fats are non-toxic and burn very cleanly. Any that are not burned are exported as ketones or new lipids (cholesterol, etc). Disposal of coconut oil actually generates ATP, so it’s totally different from fructose disposal. Coconut oil disposal raises HDL which is thought to be cardioprotective. So it should be beneficial.
Hi Jo,
Excess weight around the middle can be due to high cortisol levels or chronic bowel inflammation. So you might want to check those other possibilities out. You might find that a little more carbs may be helpful for gut health.
For liver health nutrition is more important. In addition to our regular recommendations, glutathione is important for the liver. Selenium, NAC and vitamin C are helpful for glutathione support.
Hi Poisonguy,
Yes, they do.
Hi Tony,
Yes, you’re quite right. Keeping toxins down, especially sugar, alcohol, and polyunsaturated fats, is key for the liver. Keeping nutrient levels high is also important, including antioxidants as noted above. We recommend magnesium supplementation of at least 200 mg/day but you can supplement at the RDA without any risk. Our recommended supplements page has our supplement recommendations: http://perfecthealthdiet.com/?page_id=1066.
And eating liver is nutritious as well.
Plantains are an excellent food! As far as I know they lack significant toxins when ripe or cooked.
Yes, that’s an important point, eating fructose depletes liver ATP and so short-chain fats would be burned to generate energy instead of converted to ketones. So don’t eat fructose if you want to be ketogenic!
Very good observations Tony!
Best, Paul
Hi Tony,
Thanks for calculating the ketogenic/glucogenic amino acid composition of meat. (UPDATE: I’ve updated the post with a correction. Thanks Tony!)
One thing to remember is that Wilder’s ratio is based on the ketogenic potential of dietary calories in. So fat calories and carb calories enter equally, even though all carb calories become glucose while not all fat calories become ketones.
So a Wilder’s ratio of 1, corresponding to a 50% fat 50% carb zero protein diet, is not ketogenic at all.
The protein weights have to fit into the carb-fat scale, so meat that is 20% ketogenic and 80% glucogenic may produce a Wilder’s ratio of 1 also, consistent with the weights in the formula.
I haven’t looked up how the formula was determined — I believe it was empirical, based on which diets produced an amount of ketones similar to the level produced in fasting.
Best, Paul
Hey Paul, would coconut milk provide the same benefits of coconut oil, in terms of producing a ketogenic state or do the benefits only arise from consuming the pure coconut oil? As a rule of thumb, is it possible to over consume any of these fats barring no desire to lose weight?
OT: I bit off topic, but reading some of Ray Peat’s articles got me thinking of iron overload and the role it plays in disease. Do you think iron overload is a problem, especially when consuming close to 30 miligrams a day. Could we potentially be consuming to much iron? Also one more thing, sorry for the randomness of my questions hahaha, there is a lot on my mind and I am constantly learning new things, but does it matter what kind of white rice we eat or is it all created equally?
Hi Robert,
Most of the calories in coconut milk are from coconut oil, so yes, it’s a ketogenic food.
Yes, you can overconsume these fats. The result would be weight gain.
I think the problem with iron is more how the rest of the diet affects its handling, than with how much there is. But it might not be bad to give blood from time to time … the body can replenish a deficiency more easily than it can excrete an excess.
All white rice is pretty similar in nutritional value, I think.
I’m a little confused by some terminology. I looked up short-chain fatty acids on Wikipedia, and the first one in the list is acetic acid, which, if I understand correctly, is essentially vinegar (i.e. vinegar is a solution of 5-20% acetic acid). Yet vinegar does not contain fat. Is there a change of terms I don’t know about, or is the amount of acetic acid in vinegar so small as to have negligible fat content, or something else?
Thank you!
Hi Amber,
Actually, CarbSane had a post about this yesterday: http://carbsanity.blogspot.com/2011/02/when-is-fat-fat.html
Acetic acid is basically the cleaved end of a fatty acid, but it behaves nothing like longer fats. So it might technically be considered a fatty acid, but biologically and practically it has nothing in common with fats.
I use “short-chain fats” in kind of a portmanteau way to cover all fatty acids that are too short to play a role in cell membranes. A cell membrane made of short-chain fats would disintegrate; the fats need to be long enough to maintain membrane integrity.
This is why there are no cells made of vinegar!
Hi Paul,
I saw that the coconut oil and the palm kernel oil are very similar in terms of fatty acid profile, MCT 57-60% for both of them. Is there any reason to use coconut oil over palm kernel oil? Why the coconut oil seem to be preferred while the palm kernel oil is not so recommended? Let’s presume that both of them are extra virgin and organic.
Hi Andrew,
Yes, they’re very similar, and equally healthy. Use whichever you prefer.
I mention coconut oil a lot because that’s what we use, and it’s widely available, but both are fine. Buyers should be aware that it’s palm KERNEL oil, not palm oil, that has the short-chain fats.
Best, Paul
On the subject of liver function. I did a Functional Liver Detoxification Profile last year that involved taking caffeine and paracetemol then collecting urine samples. The results showed my Phase 2 liver function (conjugation/excretion) below the reference ranges for glucuronidation (very low), glycination (just below ref ranges) and sulphation (high). My doctor informed me that it’s “the way I’m built” and that I most likely can’t do anything to improve it. I’m currently taking ‘Hepatic Detox’ supplements and have been told I should probably always take them. Try as I might, I can’t find any information online that helps me to understand this better. I hate taking unnecessary (and expensive) supplements if I know I can address something from a nutritional perspective. Do you have an opinion on this or even the validity of the test itself?
Hi GeeBee,
I thought this was a fairly good discussion of the science: http://en.wikipedia.org/wiki/Hepatotoxicity and this is a fairly good overview of potentially helpful supplements: http://www.diagnose-me.com/treat/T355489.html
I don’t know whether the test is valid. Do you have evidence of liver damage?
I assume you’re taking things like glutathione/NAC/glycine/choline/vitamin C/taurine/selenium supplements? Do you have any biomarker you are monitoring to see if supplements are having an effect, such as liver enzymes?
Best, Paul
“Do you have evidence of liver damage?”
No. The test was done along with hair tissue analysis as part of a workup trying to get to the bottom of some strange and minor health issues I’m experiencing (skin/face hypersensitivity, dry eyes and skin, mild rosacea and blepharitis, occasional vertigo and thinking I can smell ammonia). She said the ammonia thing could be related to toxins being released. The hair tissue analysis showed very high levels of copper which I’ve managed to bring down considerably supplementing with vit C and zinc. As mentioned I’m also taking the Hepatic Detox supplement as well as molybdenum, Methyl Max (B12, B6, Folic acid) and magnesium. My initial liver enzyme test was fine as have been all the previous ones I’ve ever had. The hair tissue analysis is the only ongoing test I’m having for monitoring purposes. I’m just not sure whether the hair tissue analysis is alt-med-woo (to paraphrase Dr Eades) or not….
On a side note, since starting the PHD six weeks ago (I’ve been a low-carber for the last eight years) my energy levels and sleep quality have improved beyond all expectations so I’m thrilled about that.
Hi GeeBee,
That’s great that you’re doing better!
I would definitely look at supplementing glutathione-related nutrients. If not glutathione itself, NAC, glycine, selenium, and C. Maybe those are in your Hepatic Detox supplement.
But since your liver enzymes are fine I wouldn’t worry.
There are many possible causes of skin problems; since there’s a lot of immune activity, any autoimmune condition, allergy or infection can trigger them. Food toxins and nutrient deficiencies or imbalances can lead to distortions in immune activity that are reflected in the skin.
Rosacea is mysterious, mine is much better but not completely gone. I think it’s due to a chronic infection. I developed it circa 1992 during a long course of antibiotics, and all my subsequent problems seemed to begin then.
Best, Paul
Yes, I’m concentrating on getting more nutrient dense foods into my diet. I’ve added calves liver, egg yolks, herring, salmon and mackerel a few times a week and drastically cut down on nut consumption. One of the things that hits you in the face when you start tracking nutrient levels is how the PUFAs add up from all the nuts and nut products (almond meal etc.) that low carbers tend to use. I’ve virtually eliminated all of them apart from a few Brazil nuts for the selenium and some macadamias.
I’ll definitely follow up on those nutrient recommendations. Thanks for your input!
Hi Paul,
I bought your book yesterday & basically haven’t put it down since, very informative.
I have a few questions/queries if i may;
1. The book mentions Low Body Temperature, but does not go in to detail (that i have found yet); What do i need to do to check?
2. Where you talk about ketogenic diets/fasts you recommend consuming short chain fats; i just want to confirm your definition, you are referring to saturated fats with 12 carbons or fewer…..is that correct? {only i have also seen Short chain referred to as less than 6 (six) carbons & Medium chain as 6 to 12 carbons}.
3. & lastly. It seems (from the book & the web) that iodine deficiency is common place in the modern populace & am wondering why this is, would our primal ancestors have had the same deficiency do you think?
Thanks for this great post. Your explanations are most illuminating. I’m really looking forward to the next installment in this series!
Hi Darrin,
1. Hypothyroidism is the most common cause of low temperature and we have a section on how to recover from that. In general, switching from a high-carb to low-carb diet and increasing saturated/monounsaturated fat consumption is helpful, but don’t go so low-carb as to create stress from a starvation response (glucose or protein deficiency). Being well-nourished and avoiding food toxins tends to fix low body temperature. I would say, follow the steps in the book and most likely body temperature will normalize. You’ll probably also notice a much broader temperature tolerance — both cold tolerance and heat tolerance.
2. Yes, short chain fats in our lingo encompasses the standard “short-chain” and “medium-chain” — 12 carbons or fewer. Since they’re handled similarly biologically, we thought it made more sense to use a descriptive term instead of technical jargon.
3. Probably our ancestors were commonly iodine deficient, unless they lived on the seashore. A lot of Paleolithic settlements were on the seashore, and shellfish and seaweed were probably a big part of the diet. The “Out of Africa” expansion proceeded by boat and this sea-living population was probably smarter than competing populations due to high iodine intake. Another factor is that vitamin C can substitute for iodine to some degree, so high fruit and vegetable consumption can mitigate iodine deficiency.
Kate – Thanks!
Thanks Paul for a great post. I’m directing everyone possible here to get an understanding of the keto diet. If you google it, you get all kinds of scary stuff that primarily say “DO NOT DO THIS UNLESS YOU ARE IN A HOSPITAL”.
Hmmm, we are doing this to AVOID being in the hospital!
I am keeping Mathias’ intake around the 80% fat, 15% protein, 5% carb level with less than 5% PUFA. I am trying to add coconut oil in every place I can think of but this is harder to do than one would think. I want him to take 4 – 6 tablespoons a day so I can up his carbs a bit (as he is at the point now where we are more or less forcing him to eat because the fat is making him not hungry and he doesn’t have enough carbs (even at the 30-50 gram level) to seem to make him want to eat.
I am trying ‘hot chocolate’: heavy whipping cream, coconut oil, cocoa-plain, drop of stevia. He likes it but will only take a few drinks before he is ‘full’.
I am cooking eggs (from our own chickens) in coconut oil – but again a few bites and he’s done. I’ve also tried to get him to just take it on a spoon – but that was a no-go.
Zach has an easier time because he is tube fed – and he doesn’t really care what is in the mixture. So he is getting a much higher level of coconut oil and also a higher level of carbs.
Zach’s parents will post here soon but I wanted to share that Zach has made another milestone. For the first time in years (5 or more?), he stood flat footed on his left foot yesterday. He cannot stand alone but with assistance, when he was placed in a standing position his foot was flat on the floor all by himself. Our kids both have feet and hands that are hyperflexed inwards (with the smaller muscle pulling upwards). So the fact that Mathias is pointing accurately with his fingers again and that Zach actually stood flat footed is nothing short of a miracle.
Thank you for all your great explanations. I have a feeling that many, many people with neurodegenerative conditions (or predispositions to these) are going to be greatly helped by all your research and your clear descriptions.
Great post – we are looking forward to the others!
Kindy
Hi Kindy,
I’ve been meaning to email you about this, I’m planning Tuesday’s post to cover benefits and risks of ketogenic diets, and then Thursday’s to put it all together with a practical diet design.
I think you have to expect that the high calorie consumption of these kids is due to the CoA deficiency and that as the ketogenic diet fixes that, their appetite will drop. That’s OK. It just means we have to be efficient in designing the diet to get the most ketones and nutrients per calorie that we can.
It’s so good to hear of more progress! I think that the ketogenic diet might do much more for these kids even than it does for epileptics. I’ll discuss why on Tuesday.
Best, Paul
Thanks for the response Kate, to follow up,
With the body temp, are we talking oral basal temperature & should this ideally be above 98F?
I own a basic digital thermometer, will that do the job okay.
I also have a couple of new queries for yourself/Paul/other PHD staffers;
I have read/heard that combining Fat & Carbs should be avoided, is this just a myth, or maybe it really means excessive carbs or certain types of carbs ie. Fructose.
Protein powders: I occasionally supplement with Pea Protein powder (made from Golden Peas), i prefer not to use dairy protein powders (such as Whey), do you have any views on (golden) pea protein powder, i think it meets all the PHD requirements.
Thanks again Darrin
Hi Darrin,
I don’t know that it’s necessary to measure temperature; unless you are evaluating hypothyroidism or some other disorder, you can just go by how you feel.
However, if you choose to track temperature, consistency in measurement is the most important consideration.
Info from http://en.wikipedia.org/wiki/Normal_human_body_temperature:
I think fat and carbs go great together. I think that meme got about as a hypothetical explanation for why diets of 40% carb and 40% fat most easily fatten lab animals. The reason is that sugar and omega-6 fats are a bad combination. But if you eat starch and saturated fats (e.g. potato and butter), you’ll be fine.
We’re not fans of protein powder – why not just eat meat? – and worry about legume toxins, but I guess I don’t have a strong objection to pea protein powder.
Finally ordered your book after reading your blog for a while. I have hypothyroidism and had a blocked tear duct in my right eye. My eye was constantly tearing and I would constantly be wiping it. Had surgery a few years back to create new tear duct. I had no issues after but tearing started up again. Do you think being too low carb for a lot of the time the cause.
So happy about the progress of the kids on the ketogenic diet. Best wishes for even more improvements.
Hi Sue,
Did the tearing restart soon after the surgery?
In addition to the blocked tear duct, tearing can happen because the tears lack mucin / mucus to help them adhere to the eye. This can be caused by being too low-carb.
But blocked tear ducts are usually not caused by low-carb. The most common cause of blocked tear ducts is inflammation, usually due to infection. There are many other possible causes which you can find on the Internet.
I don’t know what’s going on, but a good doctor/opthalmologist should be able to diagnose it. Our diet should be good against either situation, but infections should be checked out, as it may not be confined to the eye.
Best, Paul
Excellent post, brought up some biochemistry horror memories though 🙂
Paul, my right eye would constantly tear that I would have to have a tissue in my hand at all times. It would also build up with gunk near the tear duct. Sometimes the eye would be sticky all across and hard to open in the morning. They tried to unblock the tear duct but were unable to so said I had to have surgery to create new tear duct through the nose. After the surgery the constant tearing stopped. This was at least 5 years ago and started up again in the right eye. I woke up with both eyes swollen a few weeks back, not sure why.
I don’t know if it makes sense that tear ducts blocked but had excess tearing.
How do they confirm infection in eye – could be sinuses as have an issue with sinuses occasionally.
Hi Sue,
It does sound like an infection, the gunk might be dried pus or mucus created in the duct to expel the infection.
They can take a scraping and culture it, or just look at it and see if its inflamed and try antibiotics.
However, chronic infections are hard to deal with. Also, don’t exclude the possibility of a fungal infection. Malassezia yeasts are known to cause a seborrheic dermatitis which affects the eyes.
Very likely the sinus issue has the same cause.
I would try to figure out the cause this time and fix it.
Best, Paul
Hi Paul,
Another very informative post. When I read your remark about medium-chain fatty acids being too short for membranes, I immediately connected the dots on why these fatty acids can kill bacteria, viruses and fungi. Thank you for this insight.
I have 2 coconut related questions:
1) About coconut oil you said: Yes, you can overconsume these fats. The result would be weight gain. Given your remark that most medium-chain fatty acids cannot be stored in adipose tissue, how would that work? I know that in choline deficient rats coconut oil can lead to fatty liver [1] (which of course can lead to a whole cascade that may ultimately lead to weight gain). And very high ketone concentrations will lead to tissue insulin resistance [2]. But still, what would fatten the adipose tissue if there are mainly ketones in circulation?
2) Do you have any idea on the pathways of topically applied coconut oil? I’m just curious about where it would end up and how it got there.
By the way: while trying to answer some of my own questions, I came across two papers about raspberries. Apparently a polyphenolic compound in raspberries is a ketone. It seems to increase lipolysis and fatty acid oxidation [3], and it seems to be able to prevent/improve obesity and fatty liver [4] (in mice).
John
References:
[1] Masterjohn C. The Sweet Truth About Liver and Egg Yolks — Choline Matters More to Fatty Liver Than Sugar, Alcohol, or Fat. http://blog.cholesterol-and-health.com/2010/11/sweet-truth-about-liver-and-egg-yolks.html
[2] Sonksen P., Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth. 2000 Jul;85(1):69-79. http://pmid.us/10927996
[3] Park K.S. Raspberry ketone increases both lipolysis and fatty acid oxidation in 3T3-L1 adipocytes. Planta Med. 2010 Oct;76(15):1654-8. http://pmid.us/20425690
[4] Morimoto C., et al. Anti-obese action of raspberry ketone. Life Sci. 2005 May 27;77(2):194-204. http://pmid.us/15862604
Hi John,
1) Coconut oil delivers calories. The shorter-chain fats themselves are disposed of in the liver, but the liver can export calories to the body in several ways. Ketones, of course, substitute for other energy sources and so they conserve body fat and glucose. Short-chain fats can also be lengthened into palmitate and other longer fats that can be stored in adipose cells or membranes. If the coconut oil is eaten in combination with lots of carbs, so that glucose has to be disposed of via conversion to acetyl CoA, this pathway is especially likely.
Also coconut oil is 42% long-chain fats by weight, and these can go straight into adipose tissue.
2) I’m afraid I’m not sure what happens to topically applied coconut oil. I’m sure it’s safe though.
Raspberries – thanks! I’m not sure I should add raspberries to my 3 ways to make a diet ketogenic, but wouldn’t it be cool if raspberries did!
Best, Paul
Thanks Paul,
1) Agreed, if there are other energy sources, these can be stored as fat. And I forgot about the long-chain fatty acids in coconut oil. I didn’t know about the elongation to palmitate.
2) No problem, I also think that putting coconut oil on your skin is safe. I was just curious about what happens to it.
About the raspberry ketone: according to its Wikipedia page, it causes the specific raspberry fragrance, and it’s not very abundant (it costs around $20,000 per kg).
So indeed it doesn’t seem like a practical option to make a diet ketogenic.
Using vinegar would probably be a more practical option. Peter Dobromylskyj mentioned its ketogenic potential as well.
Apple cider vinegar is supposedly this cure-all potion (weight loss, lowering cholesterol, etc.). I wonder to what extent ketones are responsible for its effect.
John
Thanks, John, for the links. I had forgotten that thread at Peter’s and interesting that raspberry ketones suppress appetite in mice.
Is it possible to use coconut butter or coconut milk in a ketogenic fast?
I don’t think I could actually down quite that much straight coconut oil, much as I like it. Is it possible to use Artisana coconut butter or coconut milk or even avocado to replace some of the coconut oil or would the small amounts of carbs and protein keep this out of the ketogenic fast range?
Hi Karen,
Yes and yes.
Avocado – it depends on the purpose. You’ll have less of a fast but it would still be ketogenic.
Hi Paul,
Where in Dr. Bernstein’s [i]Diabetes Solution[i/] is the info on the “ketogenic ratio” to be found? I am quite familiar with his books, and I can only can place this topic as having been discussed by members of the website forum (introduced IIRC by a long-time member, Georgette). Thanks, I’d like to know Bernstein’s thoughts on the subject.
Second, wasn’t sure where to post this; I’ll throw it in here. Following much of your recommendations re: normalizing thyroid function (i.e., correcting hypothyroid) I’ve managed to lower my TSH to <1 (.685 to be exact) after many years of that value hovering around 3.
However! My free t3 continues to fall. This is the first time I've tested out-of-range low at 1.6pg/mL (RR 2.0 – 4.4). I've used the same lab every time, and under the same (fasted) conditions. Oh, t4 is low-normal: 0.91ng/dL (RR 0.82 – 1.77). No antibodies.
A.M. oral temp upon waking is usually 96.x (with x <= 6). This morn it was -ahem- 95.8. Temp rises to "normal" range mid-afternoon, pattern is consistent day-to-day.
Now, if I didn't *know* these test values and their interpretation, I would never think I had any kind of thyroid problem. I've no symptoms but the low temp, of which I'm aware.
I'm taking your recommended supps, inc. Iosol (one drop) or Iodoral (1/2) daily, selenium 200mcg Se-Methyl-Selenocysteine + 1 (3-4g) Brazil nut.
Any input/suggestions much appreciated!
Kindy's story with the boys and Ketogenic diet serves as a wonderful reminder of just how very much can be accomplished when one addresses challenges with loving intent and purpose, coupled with active willingness and determination. My best wishes to all involved.
Best,
KKC
Hi KKC,
It may be that it was on the forum only. I was paraphrasing Cathy on the PaNu forum and may have misunderstood.
I think it’s good that the TSH came down; I saw a study not long ago that TSH was better correlated with health outcomes than T4 or T3 levels. I should look for that and check whether the circumstances seem relevant to your case.
How is your cold and heat tolerance? In my personal experience that’s a better indicator than temperature. Can your body adapt properly to different thermal environments?
Let me think about your situation and get back to you. At the moment I’m not sure how to interpret your numbers.
Best, Paul
Hi Paul,
I think it was in the forum only, discussed among members, thanks.
As to my cold and heat tolerance, I think it’s fine, although I do dislike *extremes* either way. As I wrote, I consider myself to be asypmtomatic. (Although I did go through early menopause,? as did my late Mom who was later diagnosed hypo-t and put on Synthroid.) Dunno. I’ll keep monitoring, along with my 25(OH)D levels which I”m bringing down slowly from a high of 82+ (July, 2010 – now, 78).
Thanks again, I am so very glad I found this place and your work!
And for anyone who might be interested: DirectLabs.com (no affiliation) is offering the 25(OH)D test for $39 in the month of March. The test is good for 6(six) months from date of order. They use LabCorp.
Be well,
KKC
How much leucine and lysine would you recommend? Is there a formula based on weight, percentage of protein intake or other factors?
Hi Karen,
That’s addressed in the next post in this series: http://perfecthealthdiet.com/?p=2638.
There’s no formula, but the experiences of epileptic children (and some rat studies) do give some guidelines about safe level of intake.
Hi Paul,
In the comment section of Chris Masterjohn’s “New Fatty Liver Study Shows that Carbohydrate Restriction Causes Statistical Anomalies”, I speculated about a possible mechanism of the protective effect of coconut oil on fatty liver, in response to an anonymous commenter. The starting point of my small investigation was your ketone post, so I think it’s appropriate to share my findings here as well.
When I re-read your post, one thing didn’t quite add up for me: why would the acetyl-CoA excess due to MCTs be turned into ketones, while in other cases (e.g., fructose excess) it would be turned into fat? (Of course, turning fat back into fat doesn’t seem efficient, but I guess the same can be said for the futile triglyceride cycle.)
So I flipped through my brand new Lehninger Principles of Biochemistry (I’m trying to build a more solid foundation for my health related speculations, so biochem basics seem appropriate), and I think I found something. Perhaps I’m stating the obvious here, and you just left it out of this post for readability. If not, it’s great that I can give something back (hopefully useful).
It appears that medium-chain fatty acids need to go through ω-oxidation before they can go through β-oxidation. There is a Wikipedia page on ω-oxidation, which is based on the text in Lehninger PoB. Step one in the process, hydroxylation, requires NADPH. But fatty acid synthesis also requires NADPH.
So my speculation is that the ω-oxidation of MCTs might deplete NADPH, making acetyl-CoA conversion to fat impossible. In that case, the liver would convert acetyl-CoA into ketones.
Could this be a realistic explanation for the ketogenic potential of MCTs, or am I missing something?
John
John, great contribution, thank you. I’ve puzzled over that same point myself. I’ll have to think your idea over a bit.
There is a preciser, but more complicated formula for calculating the ketogenic properties of a diet:
“The formula doesn’t take into account the antiketogenic properties of some amino acids but gives an approximate result to the Woodyat equation.
A paper published by I.A. Cohen adressed the issue brought by these equations: they only apply to isocaloric conditions because they fail to take into account the utilization of energy stores in a hypocaloric diet, underestimating the degree of ketosis of a given diet.”
http://www.ketotic.org/2011/05/total-ketogenic-ratio-tkr.html
Thanks, Tony. Good information.