In the earlier two posts of this series (HDL and Immunity, April 12; HDL: Higher is Good, But is Highest Best?, April 14), we established that HDL is central to the immunity and toxin clearance, and that it’s probably desirable to have more of it than our body’s natural levels, since we are in a more pathogen-and-toxin-rich environment than the Paleolithic and evolution hasn’t caught up to the situation.
The question is: how?
Disease Can Upregulate HDL
Chris Kresser left two great comments (here and here):
I tend to view HDL >85 or 90 in the presence of other inflammatory or immunological markers as a potential sign of infection or immune dysregulation.
I don’t have the reference handy, but I came across a study associating elevated HDL and CRP (occurring together) with INCREASED risk of heart disease….
I frequently see HDL >100 in patients with several other markers of inflammation, such as elevated CRP, ferritin, WBC, monocytes, etc.
Yes, indeed; as one review of HDL and heart attacks states, “many patients who experience a clinical event have normal, or even high, levels of HDL cholesterol.” [1]
Heart attacks result from a high burden of infected atherosclerotic lesions. When the body is fighting infections, it upregulates its defense mechanisms, including HDL.
Mario added a great comment along this line:
This could explain why runners have higher levels of HDL: to fight infections that abound among them!
And, the fact that pathogen-fighting HDL particles do not go back to the liver can explain why the half-life of HDL in runners is much higher than in sedentaries http://www.ncbi.nlm.nih.gov/pubmed/6748208.
These facts lead us toward one possible strategy for raising HDL: swallow a lot of pathogens!
Our Strategy: Benign Hormetic Stress
But this isn’t likely be desirable. Higher HDL may do some good, but the pathogens are likely to do a lot more harm.
So we have to look at tactics for raising HDL that do more good than harm. I think it’s useful to classify tactics in three groups:
- Beneficial Methods. These methods have no known toxicity, but cause the body to increase HDL levels – perhaps because of an association with danger in our evolutionary past.
- Mildly Toxic, Plausibly Beneficial Methods. These methods have some toxicity, but there is a plausible case to be made that the toxicity is innocuous or insignificant, so that the benefits of higher HDL will outweigh the harms.
- Damaging Methods. Intentionally swallowing HDL-increasing pathogens or toxins is probably a bad strategy most of the time, and should be avoided.
I’ll look at tactics one by one.
Coconut Oil-Induced Ketosis
One of the most powerful, and probably also benign, ways to raise HDL is intermittent fasting or ketogenic dieting, with ketosis enhanced by the use of coconut oil or MCT (medium-chain triglyceride) oil.
Ketosis stimulates the ketone receptor GPR109A, which strongly induces HDL synthesis. GPR109A is better known as the receptor on which niacin acts to raise HDL, but its physiological ligand was not known until recently when it was found to be the ketone beta-hydroxy-butyrate. [2] It looks like any time a human goes into ketosis, HDL is upregulated.
Why we evolved a mechanism to increase HDL during ketosis is not known. However, it’s easy to imagine plausible stories. Ketosis would have been a frequent event in the Paleolithic, since most hunter-gatherers probably ate low-carb diets. However, ketosis would have been associated with times of stress:
- Ketosis occurs during fasting, and involuntary fasting is a threat to health that forces eating of marginal foods from which infection risks are high.
- Ketosis can also be induced by a lack of carb-containing plant foods; this would naturally lead to a shortage of animal foods, and famine, soon after. Famine depresses immunity and increases risk of infection.
- Drought was probably a common cause of both lack of carb-rich foods and famine. Drought would tend to force reliance on marginal, polluted or infected water sources.
In the modern world, we control our food intake and can generate ketosis safely without ever reaching a famine state that significantly depresses immunity. There are safe ways to activate GPR109A via intermittent ketogenic dieting with minimal risk of ill effects.
I believe the chief risks from ketogenic dieting are:
1. Promotion of protozoal and fungal infections. While ketogenic dieting is helpful against bacterial and viral infections, fungi and protozoa are eukaryotes who can metabolize ketones in their mitochondria. In fact, because ketones are water-soluble small molecules and diffuse into pathogen mitochondria, while glucose and fatty acids are chaperoned through the human body by transport molecules, ketones are a uniquely available energy substrate for parasitic fungi and protozoa. Moreover, glucose is a major resource for the immune defense against these pathogens, and induction of ketosis by carb restriction can diminish immunity against protozoa and fungi. Since protozoal infections such as Toxoplasma gondii and fungal infections such as Candida are now common, each afflicting perhaps 30% of the population or more, this is a major concern.
2. Ketosis induced through severe carb and protein restriction may trigger the dangers of zero-carb dieting. I’ve done a series on this (it started here).
The solution is to achieve ketosis intermittently, through tactics like daily intermittent fasting, and to induce it positively through the consumption of short-chain fats such as are found in coconut oil or MCTs, or through leucine supplementation. A healthy diet, ketogenic or not, should meet our recommendations of at least 200 carb calories from starches and at least 600 calories from carbs plus protein.
Physical Activity
Exercise is another method for raising HDL that seems entirely healthful.
In the evolutionary environment, continuous exertion probably signaled danger: either a difficult hunt or, more likely, some form of warfare with other humans. In either case, injury and a need for wound repair was a likely prospect. Breaching of the skin barrier by wounds mean infections. Since HDL plays a role in wound repair and infection resistance, it would make sense to upregulate HDL production during exertion.
In one 12-week trial, HDL was raised by 24.8% on a moderate-intensity walking program and by 20.9% on a high-intensity walking program. [3]
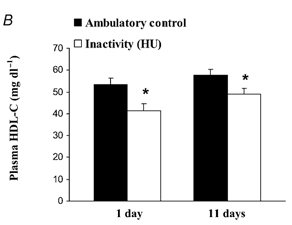
In the evolutionary milieu, sitting for 16 hours a day would have indicated a lack of danger and little need for HDL. It turns out that daily sitting time strong predicts low HDL – and it only takes a day for HDL levels to adjust. In rats, 16 hours of daily inactivity caused a 20-25% drop in HDL levels by the end of the first day [4]:
The same phenomenon occurs in humans: 20 days of bed rest leads to a 20% reduction in HDL [5].
Resistance training also helps, but perhaps not as much as reduced sitting time. Obese sedentary women raised HDL by 15% following a 9-week, 3 times per week resistance training protocol. [6]
Overall, the most effective way to raise is HDL through activity is simply to reduce the daily time spent sitting and increase the time spent standing or walking.
Sitting is also a major risk factor for obesity, diabetes, and cardiovascular disease. [7] So it looks like high activity levels are strongly health-improving.
Until recently I was sitting or sleeping about 23 hours a day, which can’t be healthful. To repair that I recently built a standing desk. Now I stand, kneel (on a padded bench), or half-kneel half-stand throughout my working hours. I strongly recommend a standing desk as an effective way to increase HDL.
High-Fat Diets and Dairy Fat Consumption
When long-chain fats are eaten, they are transported from the intestine by particles called chylomicrons. Researchers injected radiolabeled chylomicrons into rats to determine the fate of the components. They found that chylomicrons frequently turn into HDL:
Catabolism of chylomicrons is associated with a rapid transfer of phospholipid, apoA-I, and possibly apoA-IV into HDL. Chylomicron phospholipid appears to give rise to vesicles which are probably incorporated into preexisting HDL. Chylomicron surface components may be an important source of plasma HDL. [8] (Hat tip CarbSane.)
Which long-chain fats are best? A case can be made for dairy fats.
There is a clear association between eating dairy fats and having high HDL. Blood levels of trans-palmitoleic acid, an omega-7 trans-fat obtainable only by eating milk products from ruminants, is strongly associated in prospective cohort studies with higher HDL. [9b] Feeding experiments in guinea pigs confirm that butter oil increases HDL. [9]
Seth Roberts cut his coronary artery calcification score by 24% by eating a half-stick of butter per day; perhaps butter’s HDL-raising property deserves the credit. High dairy fat consumption is associated with improved health in prospective cohort studies, for instance much lower rates of diabetes and lower CRP levels. [9b]
The reason dairy fats work is uncertain. The mechanism could be via chylomicron breakdown, and other fats might work nearly as well. People who eat the most dairy fats probably eat high-fat diets that are low in omega-6 fats, and omega-6 fats reduce HDL; so the dairy fats could just be a marker for high-fat low-omega-6 diets. However, it’s possible that the ruminant trans-fat CLA is especially beneficial. It might not hurt to copy Seth, and eat a lot of butter.
Alcohol
Interestingly, drinking alcohol may be a healthful way to raise HDL. We’ve previously discussed epidemiological evidence for health benefits from drinking and the matter of how to drink safely (Is It Smart to Drink?, Sep 9, 2010), but didn’t discuss alcohol’s effect on HDL.
Well, it’s significant. Alcohol increases HDL-C level, with higher doses of ethanol leading to higher HDL levels and lower rates of coronary artery disease. This works as long as there is no liver damage. Once liver damage begins, alcohol lowers HDL. [10]
This is good news because alcohol alone does not damage the liver – only the combination of alcohol with polyunsaturated fats – either omega-6 or omega-3 will do. As long as alcohol is consumed only with saturated fats, it is likely to be beneficial to health.
Here’s some numbers relating alcohol dose to HDL increase:
- One beer per day raised HDL by 4.4% without affecting other lipid parameters. [11]
- A half-bottle of wine per day (containing 39 g ethanol) raised HDL by 17% without affecting other lipid parameters. [12]
It is possible that red wine is particularly beneficial for HDL due to certain plant compounds that accompany the alcohol. [13]
In an analysis of the MRFIT trial, alcohol’s HDL-raising effect was found to be responsible for half of its benefits for mortality from coronary heart disease. [14] It appears that alcohol’s other health benefits, from its glucose-lowering effect to its stress-relieving effect, are less important for health than its HDL-raising effect.
Niacin
Niacin supplementation is the most common doctor-prescribed way to raise HDL. Dr. William Davis of Track Your Plaque fame is an ardent advocate of niacin, as are many other cardiologists.
Niacin increases HDL the same way ketones do, by activating the ketone receptor GPR109A. Gram doses of niacin are roughly equally effective with tablespoon doses of coconut oil in raising HDL. For instance, four grams of niacin per day for 6 weeks raised HDL levels by 50%. [15]
However, there are two key differences:
1. Niacin is toxic whereas ketones are not.
2. Ketones diffuse throughout the body whereas niacin binds certain cells, notably fat cells, preferentially and this concentrates its toxicity.
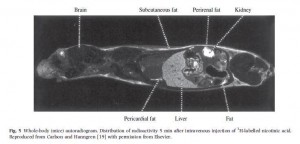
The localization of niacin to fatty tissues is clear in this radiogram taken 5 minutes after injection of radioactive-labeled niacin to a mouse [16]:
Major sites of niacin binding are the skin, the liver, and the fat surrounding the kidney. This is why these are sites of niacin toxicity: the toxins from niacin conversion are localized here.
Skin flushing is the most obvious sign of niacin toxicity, but organs can also be damaged. As one review states, “Unfortunately, when used as a pharmaceutical, niacin has more than its share of drug toxicities, including hepatotoxicity, gastric toxicity, glucotoxicity, and, most commonly, skin toxicity.” [17]
Niacin toxicity results from the manner in which it is converted to the active forms of vitamin B3, NAD and NADP. Niacinamide, an alternative form of vitamin B3, is converted to NAD and NADP without toxicity, but does not stimulate the GPR109A receptor and does not raise HDL levels.
Time-release niacin is especially prone to poisoning the liver. [18] The liver’s main niacin disposal pathway can only metabolize a small amount of niacin at a time. Time-release niacin causes more niacin to pass through this high-toxicity liver pathway.
Another issue with niacin is that NAD is the rate-limiting vitamin for bacterial metabolism. Excess vitamin B3 intake, therefore, promotes bacterial infections.
In general, I consider niacin to be an alternative to coconut oil-driven ketosis rather than a complement to it. Both niacin and ketones act on the same receptor, and the HDL increases from coconut oil alone are so large (commonly to 120 mg/dl or higher) that adding niacin on top would be gilding the lily.
Since benefits from niacin against atherosclerosis probably come either from HDL increases or from other effects of activating GPR109A [19], it is likely that coconut oil delivers all or nearly all the benefits of niacin.
In most cases, due to its lack of toxicity, coconut oil should be preferred. The exception would be people who have significant protozoal or fungal infections but not bacterial infections. Since ketones feed the former while niacin feeds the latter, such people may benefit from niacin instead of coconut oil.
Some other HDL-raising factors
In general, good nutritional status supports high HDL levels. In some populations, multivitamin and multimineral supplements have been shown to raise HDL. [20]
Micronutrients that are beneficial may include vitamin C, taurine, and glycine. Bile acids are made from cholesterol using vitamin C and are then conjugated with taurine and glycine. Bile duct blockage tends to lower HDL and providing bile-supporting nutrients like vitamin C [21] and taurine [22, 23] can under some circumstances raise HDL. Glycine is richly present in gelatin (cooked collagen), and taurine in uncooked or rare meats.
Plant fiber and polyphenols have been reported to raise HDL. For instance, a polyphenol-rich carob fiber was found to raise HDL by 7% while lowering LDL [24], and psyllium has been reported to raise HDL [25]. It is unclear to me whether this is a beneficial pathway or not. On the one hand, butyrate and other volatile fatty acids from gut flora may stimulate the ketone receptor. On the other hand, many of these polyphenols are directly toxic, and fiber increases gut bacterial populations and endotoxin flux into the body. HDL may be upregulated because it has more toxins to clear.
Higher potassium excretion is associated with higher HDL, suggesting that high intake of potassium-rich foods like potatoes, bananas, and vegetables might raise HDL. [26] Since potassium-rich foods are also usually fiber-rich, this association may be mediated by short-chain fats from fermentation of fiber by gut bacteria. But potassium is a nutrient low-carb dieters can easily become deficient in, so it may be worth tending to.
Some Things to Avoid
Dietary components that promote lipid peroxidation, including fructose, omega-6 fats, and trans-fats, lower HDL levels. Smoking also lowers HDL. [27]
A Japanese study found that “Concerning dietary habits, total cholesterol was lower by a mean of 13 mg/dl (0.34 mmol/L), triglycerides lower by 40 mg/dl (0.45 mmol/L), and HDL-cholesterol higher by 5 mg/dl (0.13 mmol/L) in the group who ate 7 or more Japanese-style meals in the 9 meals during 3 days than in the group who ate 3 or less Japanese-style meals in the 9 meals.” [27]
Japanese-style meals are low-toxicity and essentially Perfect Health Diet compliant. The alternative is probably western style food high in wheat, vegetable oils, and sugar.
Conclusion
HDL can be raised in destructive ways – such as ingestion of toxins or pathogens – but there are healthy ways to raise HDL.
I believe the following four ways are healthiest, and are sufficient to optimize HDL levels:
- Eat a nourishing diet rich in saturated and monounsaturated fat, especially dairy fat, but low in omega-6 fats, fructose, and other toxins. In short: eat the Perfect Health Diet.
- Be physically active. Be on your feet as much as possible; favor a standing desk over sitting. Do resistance exercise or other intense exercise occasionally.
- Engage in intermittent fasting, and consume a lot of coconut oil, coconut milk, or MCTs to stimulate the ketone receptor.
- Drink alcoholic beverages – but only when consuming meals low in polyunsaturated fats. Drink up when you eat beef, but be cautious when the entrée is salmon.
Niacin, the most effective pharmaceutical for raising HDL, has some toxicity and is probably inferior to coconut oil and intermittent fasting except in people with protozoal or fungal infections.
Our best wishes for high HDL!
Related posts:
- HDL and Immunity, April 12, 2011
- HDL: Higher is Good, But is Highest Best?, April 14, 2011
References
[1] Navab M et al. HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol. 2011 Apr;8(4):222-32. http://pmid.us/21304474.
[2] Ahmed K et al. GPR109A, GPR109B and GPR81, a family of hydroxy-carboxylic acid receptors. Trends Pharmacol Sci. 2009 Nov;30(11):557-62. http://pmid.us/19837462.
[3] Spate-Douglas T, Keyser RE. Exercise intensity: its effect on the high-density lipoprotein profile. Arch Phys Med Rehabil. 1999 Jun;80(6):691-5. http://pmid.us/10378497.
[4] Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003 Sep 1;551(Pt 2):673-82. http://pmid.us/12815182.
[5] Yanagibori R et al. The effects of 20 days bed rest on serum lipids and lipoprotein concentrations in healthy young subjects. J Gravit Physiol. 1997 Jan;4(1):S82-90. http://pmid.us/11541183.
[6] Costa RR et al. Effects of resistance training on the lipid profile in obese women. J Sports Med Phys Fitness. 2011 Mar;51(1):169-77. http://pmid.us/21297577.
[7] Hamilton MT et al. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007 Nov;56(11):2655-67. http://pmid.us/17827399.
[8] Tall AR et al. Metabolic fate of chylomicron phospholipids and apoproteins in the rat. J Clin Invest. 1979 Oct;64(4):977-89. http://pmid.us/225354.
[9] Rice BH et al. Ruminant-produced trans-fatty acids raise plasma total and small HDL particle concentrations in male Hartley guinea pigs. J Nutr. 2010 Dec;140(12):2173-9. http://pmid.us/20980644.
[9b] Mozaffarian D et al. Trans-palmitoleic acid, metabolic risk factors, and new-onset diabetes in U.S. adults: a cohort study. Ann Intern Med. 2010 Dec 21;153(12):790-9. http://pmid.us/21173413.
[10] Lakshman R et al. Is alcohol beneficial or harmful for cardioprotection? Genes Nutr. [Epub ahead of print] http://pmid.us/20012900.
[11] Thornton J et al. Moderate alcohol intake reduces bile cholesterol saturation and raises HDL cholesterol. Lancet. 1983 Oct 8;2(8354):819-22. http://pmid.us/6137650.
[12] McConnell MV et al. Effects of a single, daily alcoholic beverage on lipid and hemostatic markers of cardiovascular risk. Am J Cardiol. 1997 Nov 1;80(9):1226-8. http://pmid.us/9359559.
[13] Brien SE et al. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011 Feb 22;342:d636. http://pmid.us/21343206.
[14] Suh I et al. Alcohol use and mortality from coronary heart disease: the role of high-density lipoprotein cholesterol. The Multiple Risk Factor Intervention Trial Research Group. Ann Intern Med. 1992 Jun 1;116(11):881-7. http://pmid.us/1580443.
[15] Carlson LA, Hamsten A, Asplund A. Pronounced lowering of serum levels of lipoprotein Lp(a) in hyperlipidaemic subjects treated with nicotinic acid. J Intern Med 1989; 226: 271–6.
[16] Carlson LA. Nicotinic acid: the broad-spectrum lipid drug. A 50th anniversary review. J Intern Med. 2005 Aug;258(2):94-114. http://pmid.us/16018787.
[17] Dunbar RL, Gelfand JM. Seeing red: flushing out instigators of niacin-associated skin toxicity. J Clin Invest. 2010 Aug 2;120(8):2651-5. http://pmid.us/20664168.
[18] Bassan M. A case for immediate-release niacin. Heart Lung. 2011 Mar 15. [Epub ahead of print] http://pmid.us/21414665.
[19] Lukasova M et al. Nicotinic acid inhibits progression of atherosclerosis in mice through its receptor GPR109A expressed by immune cells. J Clin Invest. 2011 Mar 1;121(3):1163-73. http://pmid.us/21317532.
[20] Li Y et al. Effects of multivitamin and mineral supplementation on adiposity, energy expenditure and lipid profiles in obese Chinese women. Int J Obes (Lond). 2010 Jun;34(6):1070-7. http://pmid.us/20142823.
[21] Yanai H, Morimoto M. Effect of ascorbate on serum lipids and urate metabolism during exhaustive training. Clin Sci (Lond). 2004 Jan;106(1):107-9. http://pmid.us/12927020.
[22] Choi MJ. Effects of dietary taurine supplementation on plasma and liver lipids in OVX rats fed calcium-deficient diet. Nutr Res Pract. 2008 Spring;2(1):13-6. http://pmid.us/20126359.
[23] Elvevoll EO et al. Seafood diets: hypolipidemic and antiatherogenic effects of taurine and n-3 fatty acids. Atherosclerosis. 2008 Oct;200(2):396-402. http://pmid.us/18242615.
[24] Ruiz-Roso B et al. Insoluble carob fiber rich in polyphenols lowers total and LDL cholesterol in hypercholesterolemic sujects. Plant Foods Hum Nutr. 2010 Mar;65(1):50-6. http://pmid.us/20094802.
[25] Giacosa A, Rondanelli M. The right fiber for the right disease: an update on the psyllium seed husk and the metabolic syndrome. J Clin Gastroenterol. 2010 Sep;44 Suppl 1:S58-60. http://pmid.us/20616745.
[26] Ishikawa M et al. Taurine’s health influence on Japanese high school girls. J Biomed Sci. 2010 Aug 24;17 Suppl 1:S47. http://pmid.us/20804624.
[27] Hata Y, Nakajima K. Life-style and serum lipids and lipoproteins. J Atheroscler Thromb. 2000;7(4):177-97. http://pmid.us/11521681.











Great stuff Paul.
If I’m reading this right, you think that it’s ok to have very high HDL (~120) as long as CRP is very low (<.1). I'm thinking lots of exercise and coconut oil are why it's so high now.
Tyler
Hi Tyler,
Yes, I think that’s fine. Exercise and coconut oil are the way to go! And a little wine with dinner. 🙂
Paul:
Given that a substantial proportion of the adult population suffer with toe nail fungus, of which i do, would this qualify as a fungus that would fit your recommendation of coconut oil avoidance?
Regarding a high plaque load, there are many out there have it and have no issues. The key is for the plaque to remain stable which PFD should help in maintaing.
Do you have some research you can cite regarding coconut oil affecting the GPR109A receptor the way statins do? Thanks.
Paul,
I’m battling candida right now and am following your recommendations including eating ~400 calories of safe starches daily. Question for you: How often should I be eating to stay out of ketosis? I typically stop eating for the day at 6 pm and have breakfast the next morning at 8 AM.
Thanks!
Jess
Hi Steve,
I don’t think I would diverge from the regular diet much because of a toenail infection. If you get systemic symptoms, like gut bloating, oral thrush, rosacea, those kind of things, then I’d worry a bit more.
References for coconut oil causing ketosis are in this post: http://perfecthealthdiet.com/?p=2479. Then ketosis causes higher HDL by activating GPR109A.
Hi Jess,
I think you may want to experiment. I personally do intermittent fasting, 16-hour fast and 8-hour eating, and eat plenty of starches in the feeding window. So I have a bit of ketosis, but only for maybe 6 hours a day.
Your strategy sounds great, I don’t think you’ll have a lot of ketosis. A little is OK. You could experiment with 600 calories of starches, see if you notice any difference.
Best, Paul
Thanks Paul: The only issues i have are coronary plaque and i am a long sufferer of atopic dermatitis(eczema) that gets better as the climate becomes more humid. Would be great to reduce the plaque as i am the ony male in my family not to have a heart attack. At age 60, i hope to keep it that way by following PHD and keeping wheat sugar, bad oils out of the diet; should keep plaque stable, i hope!
The book is quite good and i hope that the starch level recommended will not adversely affect small LDL. My recent NMR (although i take Zetia and Crestor which i have temporarily stopped) were less than 90, HDL of 64 and total LDL particles of 640. ONly with the addition of sat fat have i been able to shift to pattern A, and have small LDL this low.
Thanks again for your input.
Don’t you think that all saturated fats raise HDL?
I have done everything you have listed to raise your HDL. My HDL went from 54 to 76 and my CRP fell to .36
Obviously, My HDL is the healthy kind.
Hey Paul I would really like to increase my butter consumption but it usually gives me horrendous gas and diarrhea. Most of my fat usually comes from coconut oil, though the last week I have been experimenting with tallow which gave me the exact same reaction as butter. Do you think this is some sort of bile insufficiency or a reaction to dairy? I find it weird that tallow would give me the exact same symptoms as butter.
Hi Paul,
Would blood donation raise HDL? What are the effects of blood donation on pathogens / chronic infections? Do you believe blood donation could play a role in maintaining optimal health?
Thanks.
Hi Paul,
Thank you again for these great posts on HDL. I have learned a lot from them.
As you wrote in your post, HDL can be raised by many ways such as fasting, ketosis, and low carb diets.
If my understanding is correct, HDL is involved in transporting lipids from cells such as adipocytes to the liver. If one is participating in one of the three events listed above, then the body will be heavily relying on fat as a energy source. As a consequence, the body needs to be able to easily mobilize fat to the liver so that ketones and gluconeogenesis needs are met. This would require the body to make more HDL to help shuttle lipids to the liver.
Could a high HDL concentration be a reflection of lipid mobilization to the liver? A person on a high carb diet of course would not need as much HDL since the liver needs would be easily met from dietary carbohydates. And with high insulin levels, the liver would be in lipogenesis mode and the excess carbs would be converted to fat and then exported out via LDL.
Perhaps HDL and LDL levels are a reflection of how fat is mobilized in the body?
Thank you for your time.
Erik
http://findarticles.com/p/articles/mi_m0887/is_n7-8_v15/ai_18602515/
“Coronary heart disease death rates decreased with increasing concentration of HDL cholesterol throughout most of the range of HDL cholesterol values. Above an HDL cholesterol level of 1.75 mmol/L, however, the coronary death rate increased. This effect was associated with alcohol consumption but was not associated with the amount of alcohol intake.”
HDL of 1.75 mmol/L is equal to 68 mg/dL.
@Robert,
what about ghee?
I would try that.
Hi Paul,
I plan on doing a CR-keto diet as a test with low protein (~60 g) and about ~70 g of net carbs from vegetables.
With fibers counting up to 60 grams a day and supplementing fermented kefir dairy/coconut milk, would I still be prone to the infections that you mention?
“Now I stand, kneel (on a padded bench), or half-kneel half-stand throughout my working hours.”
Would very much like more information about your new desk. I think we need something like that around here.
Thanks so much for such a great book and blog.
Hi steve,
Plaque stability is probably closely related to infectious burden in the atherosclerotic lesion. Intermittent fasting should help, and HDL raising. You might also try antibiotics for plaque regression. Their effect has been unclear in clinical trials but I think on a good diet would be much more likely to help. In general, on bad diets antibiotics are ineffective against chronic infections, but can work very well on a good diet.
Modest starch intake should be fine. Key is to keep the omega-6 low to stop conversion to oxLDL!
Hi Jake,
Yes, all saturated and monounsaturated fats should raise HDL, but there may be differences among the individual fatty acids, and dairy fats seem to have an outsize effect.
Hi Robert,
Odd. The beef tallow experiment seems to refute the dairy sensitivity theory, which you can further test by trying Franco’s idea to clarify the butter (removing sugars and proteins which cause dairy reactions) and see if that helps. Also, what about olive oil? (Unpalatable by itself I know.)
If it’s the oil then it seems like a digestive issue, probably bile, possibly pancreatic enzymes. You could supplement oxbile with the butter to see if that helps; if so take vitamin C, taurine, and glycine (bile supports) and see if that fixes the problem. If it is a bile problem you might have your doctor look into gallbladder issues – a gallstone could be a possibility.
There are also lipase supplements, but I would thoroughly test for bile issues before trying that. Take lipase only with the fat.
Best, Paul
Hi David,
There is a bit of evidence for blood donation raising HDL, and benefits from iron reduction would be consistent with lipid profiles generally worsening in women after menopause. See e.g. http://www.ncbi.nlm.nih.gov/pubmed/21263413.
This makes some biochemical sense too, since iron excess increases ROS production and it’s the highly oxidative stress that diminishes HDL levels.
Since iron is beneficial to pathogens and iron transport systems are conserved from bacteria through humans, low iron status should generally be helpful against chronic infections. So blood donation should be beneficial for the donor.
Yes, I do think blood donation is beneficial, and I’ve begun doing it regularly myself.
Hi Erik,
Yes, fat and cholesterol transport is one function of HDL and affects HDL production. But exactly how significant it is is unclear. Most researchers think of fat and cholesterol transport (search “reverse cholesterol transport” on Pubmed) as the primary functions of HDL and would expect them to dominate HDL synthesis and destruction. I tend to think the immune and toxin clearance functions are more important.
Hi Kratos,
Excellent find! Thanks. Full text of the article is here: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2350977/
Look at Table 1: Lowest mortality was in the 2nd highest HDL group, but the highest HDL group had the 2nd lowest mortality of the 6 groups. Higher mortality at highest HDL is consistent with HDL being upregulated in severe infections.
In table 2, we see that 2-5 drinks per day produced lowest mortality and >5 drinks was most harmful. This could be either because alcohol was poisoning the liver or because very sick people are more likely to become heavy drinkers.
Note this: “There were few non-drinkers in the two upper categories of concentration of high density lipoprotein cholesterol, and no coronary deaths occurred in these categories (table 3).”
It looks like alcohol is protective, but you have to avoid liver damage.
Hi Lars,
That seems awfully low in protein and carbs to me. You should check out our zero-carb dangers series. As a temporary type of fasting that’s fine, but as a long-term diet it’s deficient in carb+protein and will lead to muscle loss and starvation-stress.
Check out posts 2, 3, and 4 in the zero-carb dangers series, links starting here: http://perfecthealthdiet.com/?p=1032.
I’m in the group that believes that intermittent fasting is better than CR, and that ketogenic diets are best with moderate ketosis and a fair amount of carb consumption.
Hi Ellen,
Perhaps I can get a post out of the standup desk.
Paul,
What about vitamin D? Dr. Davis, who has many of his patients taking significant amounts vit D, has noticed and reported on very large increases in HDL that he feels are attributable to the vitamin D. The published evidence is scant right now (because the trials are all used much lower amounts of D). That said, if true, vit D may represent one of the best ways to raise HDL (in that there doesn’t seem to be an offset requiring greater use of the HDL – like infections).
good post! I will have to keep an eye on those inflammatory markers you mention.
Hi Dan,
Yes, vitamin D would have been the next thing I would have considered, if the post had been less long and I had had more time.
I didn’t bother because I think the evidence supports optimizing 25OHD around 40 ng/ml for whites, lower for blacks. I don’t think the huge vitamin D doses that Dr. Davis recommends are prudent, even if they raise HDL. But that is a topic that deserves fuller consideration.
Best, Paul
Paul:
On your recommendation of possible antibiotic to treat plaque what would your recommendation be for type of antibiotic, and frequency/duration of use per year?
Regarding Oxy LDL, i assume that what you say about Omega 6 applies to excess Omega 3 as well? My consumption of Omega 6 is hopefully limited: no wheat, or high 6 oils. Only consume Olive in salad and butter and coconut oil is rest. Do get some Omega 6 from eggs, chicken, turkey(infrequent and small consumption)eggs and avocado’s. thanks again for input.
I do not think D influences HDL, at least for me in a major fashion. My HDL has ranged from 54 to 64 and increased level with lower level of D3 consumption- 4,000 units. During summer will go to zero, but tough to get sun being in office all day.
Potato is about the only starch i consume; infrequent user of rice. Generally consume 1 sweet or baked potato a day with butter and or coco oil. Eat dark chocolate daily. Hopefully, enough starch per PHD suggestions
OK, OK, as of last night I discontinued 1.5g/day of SloNiacin, and as of this morning I cooked my eggs in coconut oil rather than bacon grease.
I looked at every instance of “coconut oil” in the digital version of the PHD book without success so I ask here: what is a good procedure for liquefying coconut oil for use as a salad dressing base? Feel free to include a complete dressing recipe 🙂
New comment for change of subject… Paul, you mentioned that you do 16hr/8hr fast/eat cycle. For 2+ years I’ve been doing an Alternate Day Diet, influenced by Johnson’s book of that name. On alternate days I consume close to 700 kcal starting around 11AM-1PM, and on the other days I eat ad libitum starting with a big breakfast in the early AM. On all days my last food is eaten 8-9PM.
Originally I thought this might increase longevity via expression of SIRT1, etc., but the real reason I’ve stayed with it is that it seems to be a psychologically easy way to keep my weight stable. The occasional mild hunger is “only until tomorrow morning” and on the tomorrows I can eat whatever I like (within the PHD/archevore guidelines) without guilt.
A daily regimen like yours would be a lot more convenient socially w/r dinner engagements. Do you have any thoughts on the comparative health effects of the two schedules?
Thanks…
You write: “A healthy diet, ketogenic or not, should meet our recommendations of at least 200 carb calories from starches and at least 600 calories from carbs plus protein.”
Some day (in your copious spare time 😉 I’d love to see you comment on optimal strategies for essentially carb cycling on the PHD. Where I am right now (priority on weight loss), staying on the lower end seems most useful the majority of the time. But unlike Mike Eades or other hard-core LCers, I’m not interested in staying there permanently.
That said, I’m not interested in Tim Ferriss’ cheat day concept either. But it seems to me that there might be a way to plan for holidays, travel etc, that gives you the flexibility of increasing carb intake without dealing with the uber-high postprandrial blood glucose levels seen by LCers doing an OGTT.
Maybe, a la the LC OGTT recommendation, that’s just ramping up carbs in advance of a holiday/travel? But maybe there are other strategies? I.e., if you were tolerating carbs, how frequently would you need to have a higher carb meal to stay that way? Once a day? Every other day?
I realize this makes me sound like the junkie I probably am, but I’d welcome your thoughts even if they are “you’re a junkie … get over it” ;).
Hi Steve,
Those are questions for which there are no confident answers; a wide variety of pathogens are found in atherosclerotic lesions (e.g. http://www.ncbi.nlm.nih.gov/pubmed/21366733) but which are causal is in dispute. However, Chlamydophila pneumoniae is a likely agent of the disease.
Good antibiotics for C pn are doxycycline and macrolides such as azithromycin.
Dosage and length of time is another matter in dispute. I took a typical dose for acute infections, 200 mg doxy, for 3 months. Some favor low-dose antibiotics maintained for a very long time.
Sounds like you’re doing good on the omega-6!
Best, Paul
Hi Steve B,
I could have saved you the trouble – it’s not in the print book either.
Well, you can microwave the coconut oil to warm it past 76 F, or you can use MCT oil which is liquid. I’m not aware of tricks to lower the melting point of coconut oil, but coconut milk is ~80% coconut oil and is a liquid. You could try a coconut milk with vinegar and herb dressing.
I think the Alternate Day Diet and daily intermittent fasting are probably extremely similar in their health effects. I don’t see much to choose between them.
Hi Beth,
I don’t think you’re a junkie! Glucose is a nutrient up to 600 calories a day, so nothing to be ashamed of. The people who refuse to eat it may be in more trouble.
I think eating some every day is good practice, to exercise the insulin pathways and maintain sensitivity. It may also serve as a sort of circadian therapy for glucose regulation problems.
But there’s very little science to guide us on this. Experimenting, listening to your body, and deciding what to do based on personal experience is probably best.
Best, Paul
Hi Paul,
Yes, I am aware of that series and I’ve started jotting down notes from it of which precautions to take.
It is low protein but it seems necessary to keep IGF-1 levels at a minimum. Actually, I want to do a keto version of the diet to maintain muscle. Lyle McDonald, who’s work is wrapped around the idea of a ketogenic diet, proposes that muscle maintenance is possible on as low as 50 g on a ketogenic diet. It seems to have some mystical protein sparing effect.
You are aware that I’m talking about 70 grams of carbs plus 60 grams of fiber? I’m not sure if fiber makes any difference in the low carb danger game (which was actually my hidden question in the first comment), nevertheless it’s still higher than many VLCers and I expect to do some experimenting and stay just on the limit of ketosis. I’ll expect my keto carb tolerance to be slightly higher than most, given my low protein intake.
Intermittent fasting is what I’m doing right now. Unfortunately I’m not even near convinced this will yield the same longevity benefits.
Hi Lars,
Fiber should help as MCTs/coconut oil/ketones do, the resulting short-chain fats substitute for glucose and conserve protein.
I know that you can conserve muscle on low protein intakes – I mentioned the ability to achieve nitrogen balance at very low protein intakes in our “Protein for Athletes” post, http://perfecthealthdiet.com/?p=2712. I just don’t know how to quantify the protein intake you need to avoid negative consequences. In order to achieve nitrogen balance at low intakes, the body invokes a lot of starvation responses that may not be optimal for health if continued long-term.
You might look into the influence of individual amino acids on IGF-1. I haven’t done this yet but intend to. If leucine and branched-chain amino acids lack an IGF-1 response, or glycine/gelatin, you can help promote muscle synthesis while avoiding the IGF-1 that concerns you.
Well, it sounds like an interesting experiment. Let me know how things go.
Best, Paul
Great post Paul, BUT (I hate this word, especially when I’m using it like this)
These type of articles will wind people to raise their HDL no matter what. You know as well as I do, how people that know what HDL is, have the tendency to be maniacal regarding their supplementation and diet…
And to no surprise, people increase their Niacin consumption just to make a nicer lipid panel results…
Oh well… Ironic, while people know that Cholesterol value has no correlation with HD and has been as a marketing for Statins & friends, STILL TRY TO GET “ACCEPTABLE” cholesterol levels…
Do I have a better Idea? Not really thou… but ranting is free 🙂
Peace!
Hi Mike,
Well, overdoing these things is a concern. In case it wasn’t clear let me reiterate:
We recommend AGAINST niacin supplementation.
We recommend MODERATE not high alcohol consumption.
We recommend MODERATE not high induction of ketosis via techniques like intermittent fasting and coconut oil consumption … and carbs should NOT be severely restricted.
We recommend physical activity and occasional intense exercise but not stressful intense exercise such as marathoning (from which Grete Waitz just died at 57).
Higher HDL is good, but only if the things that raise it are not themselves damaging. Since most things that raise HDL are or can be damaging, prudence is needed.
Best, Paul
Paul, you said “… marathoning (from which Grete Waitz just died at 57)”
Gee. The news said cancer. How confident are you that she died “from” running marathons?
Thanks for your reply, Paul.
Out of curiosity, what would you consider a healthy HDL level stimulated by coconut oil? I keep seeing levels of 100 or above mentioned in some people. How long does it take to reach those levels. Is this the norm for people consuming lots of coconut oil? Do pacific islanders who consume a lot of coconut have high levels of HDL?
The last several months I have been following the PHD. I have been consuming a lot of dairy fats and coconut oil. I would say easily 50-80% of my daily calories are from fat sources. I have drastically cut out omega 6 oils and fructose consumption. I am curious to see how my lipid profile has changed from a year ago. I was on a standard USDA and AHA recommended diet. I never touched butter for years and avoided red meat.
Thanks!
Erik
Paul,
Let me apologize in advance if this post is too long.
I am a 44 year old female with clinical MS (presenting as optic neuritis) and pre-diabetes. I am of normal weight. When diagnosed I gave up gluten, dairy, sugar (except on occasion) legumes and followed a low fat diet (MS Recovery Diet).
Since going on PHD I have lost the fatigue that I’ve had in my legs. Thank you! I have been very healthy with no relapses since diagnoses. I do not take any MS drugs but I do take LDN (Since 10/10). I saw immediate improvement when giving up gluten and same with dairy. I have tried lately to re-introduce dairy but I still react to it. I can eat small amounts. Butter and ghee do not bother me. I feel very healthy on the PHD. However, I have developed a rash on the back of my neck that the doctor says is fungal. After reading your post I assume it’s from the coconut oil? Also, to be fair before receiving your book I did start the diet w/o fully understanding it and went too low carb which resulted in muscle and bone aches (and slight fever).
Question#1 Do I need to avoid coconut oil altogether(eating and cooking)and does this include coconut milk or meat?
Question #2 How does someone that cannot consume dairy get the needed fats?
Question#3 How many carbs should a person who has MS and is prediabetic get a day?
Also Q#4 What addt’l supplements beyond your those on your regular supp. list would you recommend?
My vit D level is 42.
Thank you for writing your book-I feel that it is the missing link that I have been looking for. I plan on buying one for all of my 8 siblings! I know you are a busy guy-please answer in your leisure!
Hi Steve,
An attempt at humor. No, I’m not at all confident. Still, I doubt marathoning is healthful.
Hi Erik,
I really couldn’t name a number. It probably varies with each person, depending on their health, physical activity, diet, and infection status. But I think eating coconut oil is a healthful practice, whatever the HDL number ends up being.
When you find out your new lipid profile, let us know! I’ll publish mine when I get it.
Best, Paul
Well, Grete Weitz died from cancer… Claims of overtraing and relation to cancer still have to be proven… backed up somehow. I see a connection but it’s quite a long shot. We are still having hard times opening people eyes on more direct stuff.
Regarding Niacin, I know people taking that as a supplement, and paying alot for a “time release” variety in order to make their lipid panel “better”
Personally, I dont think any form of ethylic alcohol ingestion can have ANY health benefits, other than the “feel good” effect people like. And regarding ketosis… I strongly believe that’s our normal state… I more believe in the “carb rush” induction. Ketones are our normal fuel… glucose is something that works too, with problems thou…
Peace and Cheers
Mike from the Paleo Village 🙂
Hi Sara,
Long questions are fine! These are important issues.
I am very glad you are trying our diet. I believe MS is curable and that our diet and antibiotics are the best chance. I hope that you can be cured and give us a case study.
My symptoms overlapped with those of MS and turned out to be due to a bacterial infection of the brain, which is fortunate; viral infections can also cause MS and are harder to treat.
I like the LDN, good choice. It helps against all likely MS pathogens.
Fungal infections are definitely a risk factor on very low-carb diets. I don’t know how much is glucose scarcity to the immune system and how much ketones to the fungus, but my fungal infection flares if I ever go zero-carb or do long fasts.
Questions:
1) No, I would continue to eat coconut oil and milk. Ketosis is actually good for your MS, and helpful against bacterial and viral infections. The mind and nerves are very important, so I would optimize for MS rather than for the fungal infection. There are other ways to address that which I’ll be posting about.
2) Well, dairy is not needed, strictly speaking, but it sure is nice! The best way is to eat clarified butter (ghee). Since you tolerate regular butter, you can do an easy 3/4-clarification by melting butter with water in the microwave, and after it separates keeping the yellow fatty part and throwing away the white watery part.
3) I would recommend around 200 carb calories from starches a day. This should be enough to avoid zero-carb dangers, if you get adequate protein, but still keep you in mild ketosis which will be good for MS. If the fungal infection persists at this intake, you could try more starches and see if that helps. It’s really experimental at this level of refinement – you have to try to judge what works best for you. But 200 would be a reasonable starting point.
4) NAC or glutathione are very important for MS. They are antimicrobial as well as key antioxidants for immunity. I would take all the essential supplements with extra C – maybe 4 g/day. Potassium is very important for fungal infections (and who knows maybe MS too). If you don’t eat a lot of vegetables you might want to supplement that.
I also recommend melatonin, but your need may differ – judge by the quality of your sleep. The brain’s immune response to bacterial and viral infections leads to a melatonin deficiency. Melatonin is antimicrobial and beneficial for recovery as well as sleep.
Vitamins B6 and B12 can benefit nerve repair. I wouldn’t go overboard with the B12, but 500 mcg is a good dose. Maybe 50 mg B6. B1 (thiamin, 100 mg), B2 (riboflavin, 100 mg), B5 (pantothenic acid, 500 mg) and biotin (5 mg once/wk) might be helpful and can’t hurt. I would avoid niacin and folic acid. I wouldn’t take vitamin A supplements, but carotenoid rich foods like egg yolks are great.
For additional ideas, you might want to visit David Wheldon’s site, http://www.davidwheldon.co.uk/ms-treatment.html, and follow link #7 to his supplement list. In terms of antioxidants, which he emphasizes, I think C, selenium, NAC or glutathione, zinc, and copper are most important. If you take extra zinc, beyond a multivitamin, don’t go too overboard – average less than 20 mg/day beyond the multivitamin.
I’m not sure the other antioxidants he suggests are necessary, but I might go for alpha lipoic acid or CoQ10 first.
I disagree with evening primrose oil. Omega-3 fats I would get from food only (e.g. salmon, sardines). Bioflavonoids I would get from food only, but flavonoid rich foods are probably healthful. Vitamin E I would get from food only or from food-derived mixed tocopherol and tocotrienol formulations in low doses. Carnitine I don’t think is necessary if you get adequate vitamin C.
When you take antibiotics you may have to deal with “die-off” symptoms such as porphyria and some supplements can help with that.
More supplement ideas can be found at http://cpnhelp.org. Their suggestions will be most helpful if your MS proves to be bacterial in origin.
I hope this gives you a good starting point, and feel free to ask more questions any time.
Best, Paul
Paul,
Thanks so much!
I do take melatonin so that I can sleep while taking the LDN and I have always had sleeping problems (excess pm. energy).
I have gone on the cpn site an am very interested but here in Louisville KY it will take me awhile to find a doctor willing to prescribe the antibiotics (I will however mine that site and Dave Wheldon’s for info like you suggest). My neurologist is angry with me because I won’t take an MS drug but I’ve been doing great with no changes in my MRI’s. He says diet will get me nowhere and he’ll try to keep from saying “He told me so”!
Oh well! I know how much changing my diet has done for me.
Thanks again! You’ve given me more advice than I’ve ever gotten from any of my doctors and I truly appreciate it. So glad that I don’t have to give up the coconut oil.
Sara, hopefully we will be the ones saying “I told you so!”
I do think you’ll need antimicrobial drugs as well as diet to be cured, but diet is essential. You have my prayers.
Paul, what are your thoughts on the flouride content of green tea?
I quit caffiene in Feb 2010, and have been doing just fine without it… but I do miss some green tea sometimes. I quit caffiene mainly because I found that coffee flared my folliculitis, and I found an article that stated caffiene kills gut flora? Then there are of course all the scares about flouride in tea and the thyroid… so naturally I just quit all caffienated substances all together.
I check your blog daily for what I consider the best health and diet information ever, anywhere. I am striving to follow your diet carefully. After several years of paleo I am almost able to see my abs again. Actually I feel great all the time. At 63 years old I have no health problems at all, that I am aware of. I hope to live a remaining healthy and very long life.
Two questions:
1) Since I’m surely infected with the regular “bugs” like everyone else, would it be a good idea for a healthy person to take a more aggressive approach on rare occasion, like antibiotics etc? Maybe during a longer fast? (I have no idea which ones they might be.) Or just stay with the standard dietary advise you have given?
2) How often do you suggest a man give blood? Does it depend on iron numbers?
Thanks, I’ll keep you updated once I reach that point. There’s still some insecurity, as you’ve might have noticed as I was hoping the 280 starch/glucose calories would keep me out the low carb dangers.
I might even decide that it’s to risky before I even get started.
About the amino acids, yes leucine seems to be a major signal for IGF-1 to rise together with methionine. I would therefore expect the same thing of BCAA.
It’s nice to see that you take time to answer all of the comments.
Hi Bill,
I think this might have come up on the green tea thread, http://perfecthealthdiet.com/?p=2101.
Fluoride and other contaminants are a concern. Our response is to buy very high-quality teas from unpolluted growing regions – basically, Taiwanese High Mountain teas and high-quality Japanese teas. We don’t much trust tea from China. No doubt that’s unfair to many fine Chinese teas, but it’s one of the most polluted countries on earth.
Hi James,
Thanks!
It’s a very good question and like many good questions, it’s hard to say what the right answer is.
Personally, I wouldn’t take any substantial amount of antibiotics without symptoms, but I would consider taking a few days of doxycycline (200 mg/day) for diagnostic purposes. Basically, doxy and many other antibiotics are protein synthesis inhibitors which will inhibit bacterial activity while you take them. So if you notice a slight immediate improvement while on doxy and then a return to previous after you stop, this would indicate some kind of bacterial infection. (Severe infections can produce a negative response, from toxins released during bacterial die-off; this would strongly indicate a need for antibiotics.) If you don’t notice any effect, then you don’t need antibiotics.
The antibiotics will be most effective at killing bacteria during fasts, but it’s not necessary to link the antibiotic timing to your diet.
The Red Cross allows you to give blood every 2 months. Since we eat red meat and beef liver (or should), the body can easily replenish iron enough to avoid a deficiency, so there’s no reason not to give regularly. You can test your serum ferritin numbers if you’re concerned.
Hi Lars,
If the 280 glucose calories are from starch, then I’d feel a lot better. You could argue that 520 carb+protein calories are barely adequate with ketosis. The trouble with counting vegetables is the intestine consumes a lot of glucose digesting them. Also, you don’t know exactly how much of their glucose is intercepted by gut bacteria, so their contribution can vary among persons.
You might check out the amino acid mix of gelatin for its IGF-1 capacity. That might be a good way to get protein without IGF-1 stimulation. You don’t need much ketosis, so it’s not necessary to take ketogenic amino acids.
Best, Paul
Paul: Your link to a citation when pressed came through with nothing: (e.g. http://www.ncbi.nlm.nih.gov/pubmed/21366733). Perhaps you have the wrong number?
1. i am in the alcohol not really needed camp, and note that all studies of its benefits are with those on bad diets, not PHD like diets. I believe this to be an issue with many studies that show a benefit from one variable,ie alcohol or fish oils; maybe these are not needed if the bad stuff-sugar bad oils, wheat, etc are not in the diet.
2. Would not using antibiotics to attack coronary plaque, adversely affect the gut flora,and is it really worth the trade-off and experimentation when low to no fructose intake,Omega 6,etc maybe be just as good?
3. I am not really good at measuring and ask if one sweet potato or baked potato eaten per day is sufficient starch intake per PHD recommendations?
I generally skip breakfast(sometimes just tea, sometimes hot cocoa with coconut oil added) and first meal when i do is around noon which is mostly a large salad with some meat or fish and olive oil for dressing. Starch is with dinner meal and starch has coconut oil added and or butter.
Thanks
Hi steve,
I chose that paper to demonstrate the wide range of microbes found in atherosclerotic lesions. C. pneumoniae and cytomegalovirus are almost universal, but this study found some others that usually aren’t reported:
“We recovered 872 isolates of limited number of species, including Propionibacterium acnes, Staphylococcus epidermidis and Streptococcus infantis and the fastidious anaerobe Porphyromonas gingivalis, and confirmed its presence in tissue using double immunofluorescence imaging.”
Species are important because different antibiotics work against different microbes.
1. I would agree in principle, but mechanistically I think the HDL-raising effect should work on our diet too. So if HDL is beneficial, it’s plausible that alcohol would still be beneficial. In fact, on our diet most of the harm alcohol does will be gone, so the calculus could swing the other way, toward more alcohol consumption.
2. That’s the risk. I don’t see antibiotics as a substitute for a good diet – on a bad diet the antibiotics won’t work – but they can add additional value to a good diet. I think in a healthy gut on a good diet, the flora can recover fairly quickly. A bad diet leads to infections pretty quickly once the beneficial flora are depleted. There’s a real lack of evidence to guide us on the pros and cons of antibiotics for atherosclerosis.
3. One pound of sweet potato or baked potato would be about our recommended starch intake. So it depends on how big your potatoes are!
That sounds great – skipping breakfast, meat or fish salad, starch with dinner.
Best, Paul
I enjoyed this series. I am certain I will be referring back to these post every so often. 🙂
Thank you for all the hard work.
I wonder if you have thoughts on, or know of WobenzymN?
It was recommended to me by a Naturopathic Doctor.
I took it for a few months a couple years ago. It
helps with inflammation. I quit taking it because
it disrupted sound sleep. I was taking one tablet
twice a day. It was recommended to take it first thing in the morning on an empty stomach. (wait one hour before eating) Then at night at least two hours after dinner.
I purchased another bottle this evening and have taken one. I have been battling chronic fluid in my ears, sinuses, and wake with puffy eyes. I know this will help all of that. My problem will be interrupted sleep after a few days of consuming this product.
Any thoughts on why it would interrupt sleep? I want to take this for all the good I get out of it.
timely article, i just got some test results back last week. So thought i may as well post them up, plus results from 2 yrs ago. The results were in mmol/l, but i have converted to mg/dl in this post.
APR2009 APR2011 (45 y/o male)
Cholesterol: 189.48 235.86
Triglyceride: 35.43 35.43
HDL Cholesterol: 73.47 100.54
Chol/HDL-C Ratio: 2.6 2.3
VLDL Cholesterol: 7.73 7.73
LDL Cholesterol: 108.28 127.61
CRP was not tested.
I must admit, i don’t know what any of it means. The doctor said that Total Cholesterol was high, or she may have said ‘a bit high’ but did not require any attention (something to keep an eye may have been said).
Hi Betty,
I am kind of agnostic to negative on the value of those plant protease enzymes. Maybe they can help, but I haven’t seen convincing evidence of it. They can do harm too. If you try it, listen to your body.
Why might it disrupt sleep? Proteases do funny things – they can split human proteins in two which stops them from working. Sometimes the pieces have weird activity. No one really understands the implications of taking these.
Hi Darrin,
Looks good! Everything’s great, except the LDL is slightly higher than it should be, which can be explained by your hypothyroidism or a copper or other micronutrient deficiency. I know you’re working on fixing those.