In the earlier two posts of this series (HDL and Immunity, April 12; HDL: Higher is Good, But is Highest Best?, April 14), we established that HDL is central to the immunity and toxin clearance, and that it’s probably desirable to have more of it than our body’s natural levels, since we are in a more pathogen-and-toxin-rich environment than the Paleolithic and evolution hasn’t caught up to the situation.
The question is: how?
Disease Can Upregulate HDL
Chris Kresser left two great comments (here and here):
I tend to view HDL >85 or 90 in the presence of other inflammatory or immunological markers as a potential sign of infection or immune dysregulation.
I don’t have the reference handy, but I came across a study associating elevated HDL and CRP (occurring together) with INCREASED risk of heart disease….
I frequently see HDL >100 in patients with several other markers of inflammation, such as elevated CRP, ferritin, WBC, monocytes, etc.
Yes, indeed; as one review of HDL and heart attacks states, “many patients who experience a clinical event have normal, or even high, levels of HDL cholesterol.” [1]
Heart attacks result from a high burden of infected atherosclerotic lesions. When the body is fighting infections, it upregulates its defense mechanisms, including HDL.
Mario added a great comment along this line:
This could explain why runners have higher levels of HDL: to fight infections that abound among them!
And, the fact that pathogen-fighting HDL particles do not go back to the liver can explain why the half-life of HDL in runners is much higher than in sedentaries http://www.ncbi.nlm.nih.gov/pubmed/6748208.
These facts lead us toward one possible strategy for raising HDL: swallow a lot of pathogens!
Our Strategy: Benign Hormetic Stress
But this isn’t likely be desirable. Higher HDL may do some good, but the pathogens are likely to do a lot more harm.
So we have to look at tactics for raising HDL that do more good than harm. I think it’s useful to classify tactics in three groups:
- Beneficial Methods. These methods have no known toxicity, but cause the body to increase HDL levels – perhaps because of an association with danger in our evolutionary past.
- Mildly Toxic, Plausibly Beneficial Methods. These methods have some toxicity, but there is a plausible case to be made that the toxicity is innocuous or insignificant, so that the benefits of higher HDL will outweigh the harms.
- Damaging Methods. Intentionally swallowing HDL-increasing pathogens or toxins is probably a bad strategy most of the time, and should be avoided.
I’ll look at tactics one by one.
Coconut Oil-Induced Ketosis
One of the most powerful, and probably also benign, ways to raise HDL is intermittent fasting or ketogenic dieting, with ketosis enhanced by the use of coconut oil or MCT (medium-chain triglyceride) oil.
Ketosis stimulates the ketone receptor GPR109A, which strongly induces HDL synthesis. GPR109A is better known as the receptor on which niacin acts to raise HDL, but its physiological ligand was not known until recently when it was found to be the ketone beta-hydroxy-butyrate. [2] It looks like any time a human goes into ketosis, HDL is upregulated.
Why we evolved a mechanism to increase HDL during ketosis is not known. However, it’s easy to imagine plausible stories. Ketosis would have been a frequent event in the Paleolithic, since most hunter-gatherers probably ate low-carb diets. However, ketosis would have been associated with times of stress:
- Ketosis occurs during fasting, and involuntary fasting is a threat to health that forces eating of marginal foods from which infection risks are high.
- Ketosis can also be induced by a lack of carb-containing plant foods; this would naturally lead to a shortage of animal foods, and famine, soon after. Famine depresses immunity and increases risk of infection.
- Drought was probably a common cause of both lack of carb-rich foods and famine. Drought would tend to force reliance on marginal, polluted or infected water sources.
In the modern world, we control our food intake and can generate ketosis safely without ever reaching a famine state that significantly depresses immunity. There are safe ways to activate GPR109A via intermittent ketogenic dieting with minimal risk of ill effects.
I believe the chief risks from ketogenic dieting are:
1. Promotion of protozoal and fungal infections. While ketogenic dieting is helpful against bacterial and viral infections, fungi and protozoa are eukaryotes who can metabolize ketones in their mitochondria. In fact, because ketones are water-soluble small molecules and diffuse into pathogen mitochondria, while glucose and fatty acids are chaperoned through the human body by transport molecules, ketones are a uniquely available energy substrate for parasitic fungi and protozoa. Moreover, glucose is a major resource for the immune defense against these pathogens, and induction of ketosis by carb restriction can diminish immunity against protozoa and fungi. Since protozoal infections such as Toxoplasma gondii and fungal infections such as Candida are now common, each afflicting perhaps 30% of the population or more, this is a major concern.
2. Ketosis induced through severe carb and protein restriction may trigger the dangers of zero-carb dieting. I’ve done a series on this (it started here).
The solution is to achieve ketosis intermittently, through tactics like daily intermittent fasting, and to induce it positively through the consumption of short-chain fats such as are found in coconut oil or MCTs, or through leucine supplementation. A healthy diet, ketogenic or not, should meet our recommendations of at least 200 carb calories from starches and at least 600 calories from carbs plus protein.
Physical Activity
Exercise is another method for raising HDL that seems entirely healthful.
In the evolutionary environment, continuous exertion probably signaled danger: either a difficult hunt or, more likely, some form of warfare with other humans. In either case, injury and a need for wound repair was a likely prospect. Breaching of the skin barrier by wounds mean infections. Since HDL plays a role in wound repair and infection resistance, it would make sense to upregulate HDL production during exertion.
In one 12-week trial, HDL was raised by 24.8% on a moderate-intensity walking program and by 20.9% on a high-intensity walking program. [3]
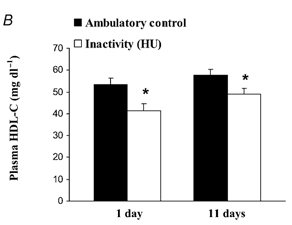
In the evolutionary milieu, sitting for 16 hours a day would have indicated a lack of danger and little need for HDL. It turns out that daily sitting time strong predicts low HDL – and it only takes a day for HDL levels to adjust. In rats, 16 hours of daily inactivity caused a 20-25% drop in HDL levels by the end of the first day [4]:
The same phenomenon occurs in humans: 20 days of bed rest leads to a 20% reduction in HDL [5].
Resistance training also helps, but perhaps not as much as reduced sitting time. Obese sedentary women raised HDL by 15% following a 9-week, 3 times per week resistance training protocol. [6]
Overall, the most effective way to raise is HDL through activity is simply to reduce the daily time spent sitting and increase the time spent standing or walking.
Sitting is also a major risk factor for obesity, diabetes, and cardiovascular disease. [7] So it looks like high activity levels are strongly health-improving.
Until recently I was sitting or sleeping about 23 hours a day, which can’t be healthful. To repair that I recently built a standing desk. Now I stand, kneel (on a padded bench), or half-kneel half-stand throughout my working hours. I strongly recommend a standing desk as an effective way to increase HDL.
High-Fat Diets and Dairy Fat Consumption
When long-chain fats are eaten, they are transported from the intestine by particles called chylomicrons. Researchers injected radiolabeled chylomicrons into rats to determine the fate of the components. They found that chylomicrons frequently turn into HDL:
Catabolism of chylomicrons is associated with a rapid transfer of phospholipid, apoA-I, and possibly apoA-IV into HDL. Chylomicron phospholipid appears to give rise to vesicles which are probably incorporated into preexisting HDL. Chylomicron surface components may be an important source of plasma HDL. [8] (Hat tip CarbSane.)
Which long-chain fats are best? A case can be made for dairy fats.
There is a clear association between eating dairy fats and having high HDL. Blood levels of trans-palmitoleic acid, an omega-7 trans-fat obtainable only by eating milk products from ruminants, is strongly associated in prospective cohort studies with higher HDL. [9b] Feeding experiments in guinea pigs confirm that butter oil increases HDL. [9]
Seth Roberts cut his coronary artery calcification score by 24% by eating a half-stick of butter per day; perhaps butter’s HDL-raising property deserves the credit. High dairy fat consumption is associated with improved health in prospective cohort studies, for instance much lower rates of diabetes and lower CRP levels. [9b]
The reason dairy fats work is uncertain. The mechanism could be via chylomicron breakdown, and other fats might work nearly as well. People who eat the most dairy fats probably eat high-fat diets that are low in omega-6 fats, and omega-6 fats reduce HDL; so the dairy fats could just be a marker for high-fat low-omega-6 diets. However, it’s possible that the ruminant trans-fat CLA is especially beneficial. It might not hurt to copy Seth, and eat a lot of butter.
Alcohol
Interestingly, drinking alcohol may be a healthful way to raise HDL. We’ve previously discussed epidemiological evidence for health benefits from drinking and the matter of how to drink safely (Is It Smart to Drink?, Sep 9, 2010), but didn’t discuss alcohol’s effect on HDL.
Well, it’s significant. Alcohol increases HDL-C level, with higher doses of ethanol leading to higher HDL levels and lower rates of coronary artery disease. This works as long as there is no liver damage. Once liver damage begins, alcohol lowers HDL. [10]
This is good news because alcohol alone does not damage the liver – only the combination of alcohol with polyunsaturated fats – either omega-6 or omega-3 will do. As long as alcohol is consumed only with saturated fats, it is likely to be beneficial to health.
Here’s some numbers relating alcohol dose to HDL increase:
- One beer per day raised HDL by 4.4% without affecting other lipid parameters. [11]
- A half-bottle of wine per day (containing 39 g ethanol) raised HDL by 17% without affecting other lipid parameters. [12]
It is possible that red wine is particularly beneficial for HDL due to certain plant compounds that accompany the alcohol. [13]
In an analysis of the MRFIT trial, alcohol’s HDL-raising effect was found to be responsible for half of its benefits for mortality from coronary heart disease. [14] It appears that alcohol’s other health benefits, from its glucose-lowering effect to its stress-relieving effect, are less important for health than its HDL-raising effect.
Niacin
Niacin supplementation is the most common doctor-prescribed way to raise HDL. Dr. William Davis of Track Your Plaque fame is an ardent advocate of niacin, as are many other cardiologists.
Niacin increases HDL the same way ketones do, by activating the ketone receptor GPR109A. Gram doses of niacin are roughly equally effective with tablespoon doses of coconut oil in raising HDL. For instance, four grams of niacin per day for 6 weeks raised HDL levels by 50%. [15]
However, there are two key differences:
1. Niacin is toxic whereas ketones are not.
2. Ketones diffuse throughout the body whereas niacin binds certain cells, notably fat cells, preferentially and this concentrates its toxicity.
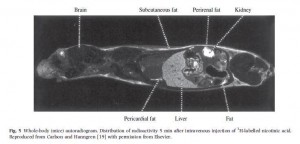
The localization of niacin to fatty tissues is clear in this radiogram taken 5 minutes after injection of radioactive-labeled niacin to a mouse [16]:
Major sites of niacin binding are the skin, the liver, and the fat surrounding the kidney. This is why these are sites of niacin toxicity: the toxins from niacin conversion are localized here.
Skin flushing is the most obvious sign of niacin toxicity, but organs can also be damaged. As one review states, “Unfortunately, when used as a pharmaceutical, niacin has more than its share of drug toxicities, including hepatotoxicity, gastric toxicity, glucotoxicity, and, most commonly, skin toxicity.” [17]
Niacin toxicity results from the manner in which it is converted to the active forms of vitamin B3, NAD and NADP. Niacinamide, an alternative form of vitamin B3, is converted to NAD and NADP without toxicity, but does not stimulate the GPR109A receptor and does not raise HDL levels.
Time-release niacin is especially prone to poisoning the liver. [18] The liver’s main niacin disposal pathway can only metabolize a small amount of niacin at a time. Time-release niacin causes more niacin to pass through this high-toxicity liver pathway.
Another issue with niacin is that NAD is the rate-limiting vitamin for bacterial metabolism. Excess vitamin B3 intake, therefore, promotes bacterial infections.
In general, I consider niacin to be an alternative to coconut oil-driven ketosis rather than a complement to it. Both niacin and ketones act on the same receptor, and the HDL increases from coconut oil alone are so large (commonly to 120 mg/dl or higher) that adding niacin on top would be gilding the lily.
Since benefits from niacin against atherosclerosis probably come either from HDL increases or from other effects of activating GPR109A [19], it is likely that coconut oil delivers all or nearly all the benefits of niacin.
In most cases, due to its lack of toxicity, coconut oil should be preferred. The exception would be people who have significant protozoal or fungal infections but not bacterial infections. Since ketones feed the former while niacin feeds the latter, such people may benefit from niacin instead of coconut oil.
Some other HDL-raising factors
In general, good nutritional status supports high HDL levels. In some populations, multivitamin and multimineral supplements have been shown to raise HDL. [20]
Micronutrients that are beneficial may include vitamin C, taurine, and glycine. Bile acids are made from cholesterol using vitamin C and are then conjugated with taurine and glycine. Bile duct blockage tends to lower HDL and providing bile-supporting nutrients like vitamin C [21] and taurine [22, 23] can under some circumstances raise HDL. Glycine is richly present in gelatin (cooked collagen), and taurine in uncooked or rare meats.
Plant fiber and polyphenols have been reported to raise HDL. For instance, a polyphenol-rich carob fiber was found to raise HDL by 7% while lowering LDL [24], and psyllium has been reported to raise HDL [25]. It is unclear to me whether this is a beneficial pathway or not. On the one hand, butyrate and other volatile fatty acids from gut flora may stimulate the ketone receptor. On the other hand, many of these polyphenols are directly toxic, and fiber increases gut bacterial populations and endotoxin flux into the body. HDL may be upregulated because it has more toxins to clear.
Higher potassium excretion is associated with higher HDL, suggesting that high intake of potassium-rich foods like potatoes, bananas, and vegetables might raise HDL. [26] Since potassium-rich foods are also usually fiber-rich, this association may be mediated by short-chain fats from fermentation of fiber by gut bacteria. But potassium is a nutrient low-carb dieters can easily become deficient in, so it may be worth tending to.
Some Things to Avoid
Dietary components that promote lipid peroxidation, including fructose, omega-6 fats, and trans-fats, lower HDL levels. Smoking also lowers HDL. [27]
A Japanese study found that “Concerning dietary habits, total cholesterol was lower by a mean of 13 mg/dl (0.34 mmol/L), triglycerides lower by 40 mg/dl (0.45 mmol/L), and HDL-cholesterol higher by 5 mg/dl (0.13 mmol/L) in the group who ate 7 or more Japanese-style meals in the 9 meals during 3 days than in the group who ate 3 or less Japanese-style meals in the 9 meals.” [27]
Japanese-style meals are low-toxicity and essentially Perfect Health Diet compliant. The alternative is probably western style food high in wheat, vegetable oils, and sugar.
Conclusion
HDL can be raised in destructive ways – such as ingestion of toxins or pathogens – but there are healthy ways to raise HDL.
I believe the following four ways are healthiest, and are sufficient to optimize HDL levels:
- Eat a nourishing diet rich in saturated and monounsaturated fat, especially dairy fat, but low in omega-6 fats, fructose, and other toxins. In short: eat the Perfect Health Diet.
- Be physically active. Be on your feet as much as possible; favor a standing desk over sitting. Do resistance exercise or other intense exercise occasionally.
- Engage in intermittent fasting, and consume a lot of coconut oil, coconut milk, or MCTs to stimulate the ketone receptor.
- Drink alcoholic beverages – but only when consuming meals low in polyunsaturated fats. Drink up when you eat beef, but be cautious when the entrée is salmon.
Niacin, the most effective pharmaceutical for raising HDL, has some toxicity and is probably inferior to coconut oil and intermittent fasting except in people with protozoal or fungal infections.
Our best wishes for high HDL!
Related posts:
- HDL and Immunity, April 12, 2011
- HDL: Higher is Good, But is Highest Best?, April 14, 2011
References
[1] Navab M et al. HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol. 2011 Apr;8(4):222-32. http://pmid.us/21304474.
[2] Ahmed K et al. GPR109A, GPR109B and GPR81, a family of hydroxy-carboxylic acid receptors. Trends Pharmacol Sci. 2009 Nov;30(11):557-62. http://pmid.us/19837462.
[3] Spate-Douglas T, Keyser RE. Exercise intensity: its effect on the high-density lipoprotein profile. Arch Phys Med Rehabil. 1999 Jun;80(6):691-5. http://pmid.us/10378497.
[4] Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003 Sep 1;551(Pt 2):673-82. http://pmid.us/12815182.
[5] Yanagibori R et al. The effects of 20 days bed rest on serum lipids and lipoprotein concentrations in healthy young subjects. J Gravit Physiol. 1997 Jan;4(1):S82-90. http://pmid.us/11541183.
[6] Costa RR et al. Effects of resistance training on the lipid profile in obese women. J Sports Med Phys Fitness. 2011 Mar;51(1):169-77. http://pmid.us/21297577.
[7] Hamilton MT et al. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007 Nov;56(11):2655-67. http://pmid.us/17827399.
[8] Tall AR et al. Metabolic fate of chylomicron phospholipids and apoproteins in the rat. J Clin Invest. 1979 Oct;64(4):977-89. http://pmid.us/225354.
[9] Rice BH et al. Ruminant-produced trans-fatty acids raise plasma total and small HDL particle concentrations in male Hartley guinea pigs. J Nutr. 2010 Dec;140(12):2173-9. http://pmid.us/20980644.
[9b] Mozaffarian D et al. Trans-palmitoleic acid, metabolic risk factors, and new-onset diabetes in U.S. adults: a cohort study. Ann Intern Med. 2010 Dec 21;153(12):790-9. http://pmid.us/21173413.
[10] Lakshman R et al. Is alcohol beneficial or harmful for cardioprotection? Genes Nutr. [Epub ahead of print] http://pmid.us/20012900.
[11] Thornton J et al. Moderate alcohol intake reduces bile cholesterol saturation and raises HDL cholesterol. Lancet. 1983 Oct 8;2(8354):819-22. http://pmid.us/6137650.
[12] McConnell MV et al. Effects of a single, daily alcoholic beverage on lipid and hemostatic markers of cardiovascular risk. Am J Cardiol. 1997 Nov 1;80(9):1226-8. http://pmid.us/9359559.
[13] Brien SE et al. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011 Feb 22;342:d636. http://pmid.us/21343206.
[14] Suh I et al. Alcohol use and mortality from coronary heart disease: the role of high-density lipoprotein cholesterol. The Multiple Risk Factor Intervention Trial Research Group. Ann Intern Med. 1992 Jun 1;116(11):881-7. http://pmid.us/1580443.
[15] Carlson LA, Hamsten A, Asplund A. Pronounced lowering of serum levels of lipoprotein Lp(a) in hyperlipidaemic subjects treated with nicotinic acid. J Intern Med 1989; 226: 271–6.
[16] Carlson LA. Nicotinic acid: the broad-spectrum lipid drug. A 50th anniversary review. J Intern Med. 2005 Aug;258(2):94-114. http://pmid.us/16018787.
[17] Dunbar RL, Gelfand JM. Seeing red: flushing out instigators of niacin-associated skin toxicity. J Clin Invest. 2010 Aug 2;120(8):2651-5. http://pmid.us/20664168.
[18] Bassan M. A case for immediate-release niacin. Heart Lung. 2011 Mar 15. [Epub ahead of print] http://pmid.us/21414665.
[19] Lukasova M et al. Nicotinic acid inhibits progression of atherosclerosis in mice through its receptor GPR109A expressed by immune cells. J Clin Invest. 2011 Mar 1;121(3):1163-73. http://pmid.us/21317532.
[20] Li Y et al. Effects of multivitamin and mineral supplementation on adiposity, energy expenditure and lipid profiles in obese Chinese women. Int J Obes (Lond). 2010 Jun;34(6):1070-7. http://pmid.us/20142823.
[21] Yanai H, Morimoto M. Effect of ascorbate on serum lipids and urate metabolism during exhaustive training. Clin Sci (Lond). 2004 Jan;106(1):107-9. http://pmid.us/12927020.
[22] Choi MJ. Effects of dietary taurine supplementation on plasma and liver lipids in OVX rats fed calcium-deficient diet. Nutr Res Pract. 2008 Spring;2(1):13-6. http://pmid.us/20126359.
[23] Elvevoll EO et al. Seafood diets: hypolipidemic and antiatherogenic effects of taurine and n-3 fatty acids. Atherosclerosis. 2008 Oct;200(2):396-402. http://pmid.us/18242615.
[24] Ruiz-Roso B et al. Insoluble carob fiber rich in polyphenols lowers total and LDL cholesterol in hypercholesterolemic sujects. Plant Foods Hum Nutr. 2010 Mar;65(1):50-6. http://pmid.us/20094802.
[25] Giacosa A, Rondanelli M. The right fiber for the right disease: an update on the psyllium seed husk and the metabolic syndrome. J Clin Gastroenterol. 2010 Sep;44 Suppl 1:S58-60. http://pmid.us/20616745.
[26] Ishikawa M et al. Taurine’s health influence on Japanese high school girls. J Biomed Sci. 2010 Aug 24;17 Suppl 1:S47. http://pmid.us/20804624.
[27] Hata Y, Nakajima K. Life-style and serum lipids and lipoproteins. J Atheroscler Thromb. 2000;7(4):177-97. http://pmid.us/11521681.











Paul, Nice post as usual. I have been following the diet in PHD for 6 months now. When I started, my HDL was low (40) and I have not tested yet. The problem for me now is sometimes during the day, I get EXTREMELY hungry with headaches and just feeling mentally “tired.” The way I deal with it is I eat some (grass fed) beef jerkey, almonds and brazil nuts and sometimes carrots and I drink a lot of water. Am I missing something? The other day I got a bit scared since I felt a bit dizzy too and a slight loss of focus.
I take a multivitamin but nothing else. I did loose about 10 pounds the first 3 months on the PHD but I have stopped losing weight now. I have also noticed that I am getting to bed a lot earlier than usual (but I am working hard so…).
Thanks
Elie
Hey Paul!
Thanks for the always quick and eloquent response. I had another question, I saw on another post that you don’t recommend things that have been fermented with yeast, so I was wondering what you thought of yogurt and kefir, since they contain yeast species as well as bacteria. For example, I have been fermenting kefir with raw milk (although in the past two weeks, have gotten lazy and pretty sure my grains are dead) Is it better to drink raw milk with just the bacterial species or ferment it in kefir?
Tried to go high carb for testosterone and while I noticed a libido increase… I also came down with a fever, sore throat, and once I beat that by toughing it out… my on and off onset insomnia came back with full force… so it’s back to PHD ratios for athletes… I felt much better on that. I am sure with time, some muscle gain an d a mastering of sleep and my T will be good again. I am thinking of doing perhaps one high carb, low fat day just in case there is some starvation response I still need to get out of.. and of course upping the calories every day.
As always, your writings, research, kindness and promptness blow my mind.
Hi Ellie,
Something is wrong and we should definitely track it down. Please keep me posted so that I can learn with you.
First, let me double-check that you are really following our diet. You’re not too low-carb, or still afraid of fats? You’re taking the essential supplements?
My best guesses for missing micronutrients would be potassium and choline. So I would focus on eating 3 egg yolks a day (for choline) plus getting at least 2 g potassium a day from vegetables and high-potassium carb sources like potatoes and bananas. 400 calories from carbs is over a pound of potatoes or bananas a day … add in some vegetables and potassium will be OK.
Let me know how it goes … if that doesn’t work I’ll come up with more ideas.
Hi Bill,
I think PHD for Athletes should be enough to optimize testosterone and libido … I don’t think high carb low fat dieting is necessary, even for “cheat days.” Of course, they’re not likely to do much harm either, although insomnia is a symptom that the carbs may be feeding some infection.
On the kefir question, to be honest I don’t know which is better … the answer might be different for different persons. I would suggest listening to your body. You might do one month one way, the next month the other, and see if you notice a difference.
Best, Paul
Paul,
Thanks for the reply! How would I test for a chronic infection? The one thing that comes to mind is maybe H. Pylori, because I was burping quite a bit on the high carb stint, although I stuck to potatoes, yams, and some white rice for all of it. My dandruff finally left 100% on the high carb stint, which is perhaps the one positive of it. Anyway, last I tested my CRP, HDL, ferritin, monocytes, and white blood cells they were all normal/perfect. Although, my monocytes were slightly higher when tested in January… I was drinking a gallon of raw milk a day though back then, not sure if that effects the numbers. I don’t really have any other markers of immune dysfunction or inflammation besides the folliculitis which cleared up when I stopped uses any kind of product like soap or lotion on my skin. My low T for my age and slightly sluggish thyroid (TSH of 1.27, but good T3 and T4 numbers, no antibodies) can all be explained by my severe overtraining and undereating for 1 year + and my zero carbish stint from January to August last year. I am have a history of serious underfuelling without realizing it. Thanks to the starch additions of PHD, this is no longer an issue and I once again have an appetite.
The only thing I can think of is the fact that my partner has HIV and HPV and had EBV as well. I have tested negative for all 3, but I have not tested in the last few months. Am I really putting myself at risk here? Is a good diet and protection enough?
I tested positive for Hep B in January.. but I have had the vaccine and my liver numbers are perfect so that has to be a fluke.
Excuse the fact that my posts are always all over the place. Thank you.
Just want to add that I am 21… so I would love to get any sort of infection treated now and when I am young and stronger… plus I have another year of college and it would be wicked to be able to step out onto the job market without any health woes!
Just another thought… I have had a loss if smell in the last 5 years. Not completely, but things must be very strong or close for me to smell them. I did have a blow to my nose in 10th grade and it broke but was “fixed” in minutes by a friend if mine ( I got in a fight). I seem to always have a tad bit of congestion too. Nothing that prevents me from breathing well. This could be linked to my raw milk consumption.
Is there a resource where I can find a doctor in my area who specializes in testing and figuring out this infection stuff? I got pretty tired of being the one educating my doctor….
Hi Bill,
Based on what you’ve said, I would try to follow a good diet and nutrition for 6 months and see if everything clears up.
The dandruff was due to a Malassezia (fungal) infection which higher-carb diets help against. But if you just get a reasonable amount of carbs, say 400 calories/day, you should do fine.
It sounds like your overtraining and poor eating might explain everything.
Re your partner’s infections, I would suggest Googling proper hygiene. I haven’t investigated how to minimize transmission risk. I wouldn’t count on diet alone for protection, it would be better not to get the viruses in the first place.
Best, Paul
Hi Betty, Paul:
Here are some thoughts on enzyme supplementation.
First, I’ve successfully kept a bad SI joint at bay using Wobenzym N. Last time I hurt it I was in Austria without established healthcare. Doc prescribed nsaids so I took it – messed up my stomach and small bowel within a few days (in the states I had access to holistic treatments). Switched to Wobenzym N and it was the quickest recovery I’ve had (hurt it every 18 months or so).
Second, (@Paul) I perhaps misinterpreted your disinterest in Wobenzym, given that you’ve promoted enzyme supplementation in your biofilm posts? Nattokinase helped me greatly when a holistic MD diagnosed me with intestinal biofilm last year. Protocol was roughly like: http://www.autismpedia.org/wiki/index.php?title=Protocols/Usman. Simply commenting because fibrinolytics also don’t have a lot of ‘evidence’ for health benefit in their corner, and also can inflict harm…
Thanks for all the awesome work – your diet protocol has helped me maintain gut health (after I flushed the intestinal biofilm) for the longest period of time yet…
Hi Paul.
I have a friend with fibromyalgia– she gave up gluten and wheat a couple years ago, eats relatively well (could be improved I think) -but she refuses to give up her daily latte that is 1/2 dairy. I’ve recommended that she try to give up the dairy and see if she improves. She can’t/won’t. She gets these insane flares which leaves her almost disabled and unable to walk because the wide spread tingling/pain. Would you recommend antibiotics in this case? Do you think dairy is contributing to her condition? I do think she has a chronic fungal infection because she gets very bloated with some foods and belches like a sailor on leave.
Thanks!
Ellen,
LDN is one good option for fibromyalgia. Here is a small trial on low dose naltrexone for fibro done at Stanford:
http://www.ncbi.nlm.nih.gov/pubmed/19453963
Thanks for the info Mario– will check it out. LDN is primarily being used for pain relief in this trial, no?
Hi Ellen,
Let your friend know about Ladybug’s successful cure of fibromyalgia: http://perfecthealthdiet.com/?p=76.
My impression is that fibromyalgia is usually due to multiple infections – say, a virus like Epstein-Barr with a bacterium – and antibiotics are often but not always helpful. In Ladybug’s case they led to a cure.
I don’t know whether dairy is contributing. She could try restricting herself to clarified butter and goat or sheep’s milk products for a while, that would give her some dairy and take out likely problematic proteins.
Fungal infections tend to happen when other infections weaken immune function. Since C pneumoniae does that, that would add to the potential for antibiotics to help her.
LDN enhances immunity and should be curative, not just pain relieving.
Our best wishes to your friend!
Best, Paul
Paul– thank you! She wanted me to relay to you that she often wakes up burping and burps even if she’s not eating anything– and this happens more often during allergy season. Do you see any correlation there?
Hi Ellen,
Well, lots of different kinds of gut dysbiosis can cause gas. Belching rather than farting suggests trouble in the small intestine rather than the colon. Allergens often get swallowed and will trigger inflammation in the digestive tract as well as the sinuses, so it’s no surprise they would aggravate the situation.
It’s not possible to make a specific diagnosis from afar but she should definitely work at fixing her problems! They are curable, I believe, and in general if things aren’t getting better, they’re probably getting worse. So best to tend to them now rather than later.
Something to keep in mind is that even if there are several problems with different causes, infections and pathologies tend to reinforce one another. So any health concern that she finds tractable is worth addressing – it may help her other conditions.
Best, Paul
Thanks so much for your feedback Paul– I’ll pass all this on to her. I’m dedicated to helping her fix her issues- and PHD is at the top of the list to accomplish that.
Hi
Great site, just got your book, halfway through, great read!
My cholesterol numbers a month ago were;
Total 344
HDL 96
LDL 228
TRIGS 77
Dont know if they checked the CRP.
Since the test I have been supplementing with copper, 2g/day, eating raw garlic, turmeric, cinnamo, raw milk, coconut oil etc.
Trying to keep PUFA’s low, eating plenty of beef, lamb eggs.
I weight train teice a week, sprints on bike or running once a wewk, plus walking 2-3 times a week for 30mins.
Any other suggestions to help my numbers? my LDL seems way high to me!
Also reading above regarding Niacin, you say excess causes skin flushing. I dont take niacin, but I regularly get skin flushing, mainly face, neck and sometimes arms, in the morning after eating breakfast, and it happens when I eat differant things, but I mainly have leftover meat or fish with veg, avocado or cheese, with some greek yoghurt and a plum.
Could this flushing be niacin flushing?
Thanks, and sorry for the long post!
Hi Dave,
Now that I’m done with HDL, I’m going to continue the LDL series, those upcoming posts will offer a few more tips.
Re the flushing, another possibility to consider is histamine intolerance. Jamie Scott had a nice discussion of that here: http://thatpaleoguy.blogspot.com/2011/04/histamine-intolerance.html
Best, Paul
PS – I hope the copper is 2 mg/day, not 2 g!
Hi Paul
Thanks for quick reply, yes I meant 2/mg/day!
Thanks also for the link, maybe it’s the fish causing the flushing, I do regularly have fish leftover from the night before, and, according to the article, fish goes rancid pretty quick and the histamine levels go up. Interesting stuff.
Look forward to the LDL series.
Dave
I’m curious about how the unique metabolism of the short chain fatty acids in coconut oil affects the way that the body handles glucose when coconut is consumed in a meal along with carbs.
After such a meal the blood stream will contain both short chain fats and elevated glucose and insulin. In this situation is the liver able to absorb glucose and replenish its glycogen stores, or is this suppressed while the liver is processing the short chain fats?
What happens if fructose is also present? Does the presence of the short chain fats in the blood delay processing of fructose by the liver?
Similarly, when the liver starts putting ketones into the blood stream does this interfere with the absorption of glucose by the muscles to replenish glycogen stores? Does the presence of ketones in the blood interfere with the normal response by the muscles to elevated blood glucose and insulin?
Thanks for all the great information you provide. I’m eagerly awaiting the Kindle version of your book.
Hi Jim,
Glucose production and insulin levels are reduced when coconut oil is consumed. E.g., http://www.ncbi.nlm.nih.gov/pubmed/19300863.
I don’t think I’ve ever seen a test of fructose and coconut oil together. But I think small doses, like a banana with coconut oil, shouldn’t be any problem at all.
Ketones won’t stop elevated glucose and insulin from causing glycogen replenishment. However it may be tricky to get ketosis, elevated glucose, and insulin simultaneously.
Best, Paul
Paul,
I’m a very healthy natural bodybuilder but don’t compete. I am 43 years old and just had a blood profile test. Here’s the numbers:
total chol. 280
hdl 75
ldl 190
vldl 13
trig 104
alt and ast in 30’s.
I follow a low carb diet, hardly any starches, cook with coc oil and butter. I do drink lots of beer, 8-10 per day. I am never sick with the exception of 2-3 times a year sinus infections.
Why is my ldl so high?
Mark
Hi Mark,
I started an LDL series not long ago, see http://perfecthealthdiet.com/?p=2536 and http://perfecthealthdiet.com/?p=2547. The second post, and the comments to the two posts, may give you some ideas.
I’m going to continue that series soon with a deeper exploration of LDL functions and why it may become elevated on Paleo diets.
Best, Paul
Paul,
I have been including coconut oil in my diet for about 8 weeks now. I have a blood panel done every 3 mos. My HDL has been at 54 for about 2 years now but went to the doctor this week to get the results of my latest panel and my HDL is now at 82! My LDL did climb also from 120 to 138 and my trigs just 3 points (not a big deal is it?). I am working on getting the right protein/fat ratio. We talked about how to include fats when dairy free about a week ago and I am working on that. My doctor was pleased and doesn’t want to see me again for 6 mos. My CRP was 2.26 (which has ranged from 2.8 to 5.36) the highest during an MS flare up.
I am working on getting my diet (and supplements) as close to PHD as possible and will report back on my next panel.
Any thoughts on doing a post on spinal stenosis? Unfortunately, during an MRI of my neck they found stenosis. I’m sure due to years of an undiagnosed dairy allergy and chronic acidity. I am just now starting to have trouble with my hand. Would the bone broth be beneficial or is it too late once it’s detected?
Hi Sara,
Sounds good! Except for the spinal stenosis.
I don’t believe it’s ever too late. The body is constantly breaking itself down and reconstructing itself.
Richard Nikoley had that recently, see http://freetheanimal.com/2011/02/this-is-one-big-ass-pain-in-the-neck.html. Possibly his experience can give you some tips.
I would expect that bone supplements like vitamin K2, C, D, magnesium, and vitamin A might be helpful to you. Vitamin A is necessary to break down / destroy bone, so if you have too much bone pressing on the spinal cord then a little extra A might be in order. The others can follow our regular recommendations, maybe a bit more C and K2.
I think bone broth should be beneficial too. I’m not sure about the acidity part, but lemon juice and minerals would help.
Best, Paul
http://www.ncbi.nlm.nih.gov/pubmed/20412290
Inflammation reduces HDL protection against primary cardiac risk.
BACKGROUND:
We recently reported high high-density lipoprotein (HDL) cholesterol as a predictor of recurrent risk in a subgroup of postinfarction patients defined by hypercholesterolemia and high C-reactive protein (CRP) levels. We investigated whether a similar high-risk subgroup might exist for incident cardiovascular disease.
MATERIAL AND METHODS:
A graphical exploratory data analysis tool was used to identify high-risk subgroups in a male population-based cohort (n = 3405) from the prevention of renal and vascular end-stage disease study by generating 3-dimensional mappings of risk over the HDL-cholesterol/CRP domain with subsequent use of Kaplan-Meier analysis to verify high-risk. Within-subgroup risk was assessed using Cox proportional hazards regression and Kaplan-Meier analysis.
RESULTS:
Mappings revealed two high-risk subgroups: a low HDL-cholesterol/high CRP subgroup and a high HDL-cholesterol/high CRP subgroup. The low HDL-cholesterol subgroup demonstrated a pattern of metabolic syndrome dyslipidemia contrasted with a predominantly unremarkable biomarker pattern for the high HDL-cholesterol subgroup. However, in the high HDL-cholesterol subgroup, CRP levels were higher than the low HDL-cholesterol subgroup; and within the high HDL-cholesterol subgroup, CRP predicted risk. Moreover, in the high HDL-cholesterol subgroup, risk was associated with lower triglyceride levels in conjunction with presumptively larger HDL particles.
CONCLUSIONS:
High HDL-cholesterol and high CRP levels define a subgroup of men at high-risk for incident cardiovascular disease. High HDL cholesterol-associated risk likely relates to impaired HDL particle remodelling in the setting of inflammation. This approach may facilitate identification of additional inflammation-related mechanisms underlying high HDL cholesterol-associated risk; and potentially influence management of such patients.
Hi Kratos,
That’s a great paper, thank you!
I would interpret the high-HDL high-CRP group as people with infections, the low-HDL high-CRP group as people with metabolic syndrome and diet-induced inflammation.
Interesting information of Niacin and bacteria, thanks! Not sure if this was brought up but any insight on Niacinamide being effective against candida? Currently dealing with a fungal infection and was going to give it a shot, but am likely also dealing with bacterial issues. Not sure if I want to worsen one to better the other.
Apologies if this has already been addressed. Here is the study:
http://www.ncbi.nlm.nih.gov/pubmed/20601951
What worries me is that, if I read correctly, it causes mutations in the DNA. I’d hate to breed a super-mutant fungus in my gut. Currently on Diflucan after trying Nystatin, both have given some success, but I am eager to explore other strategies (already tried the standard natural anti-microbials).
Hi Yves,
That’s an interesting paper. I will have to read the whole thing, and look at what doses were required, and check if anything similar has been observed in human cells.
Niacinamide is considered to be fairly harmless to humans up to gram doses, so long as you don’t have a bacterial infection. It can also have antiviral effects.
Listen closely to your body if you try it.
Paul, thank you for the reply. I stumbled across the full paper (searching google with the title of the paper). It states that they gave the rats 500 mg per kg body weight. I’m not sure how this would extrapolate to humans since that dosing would be clearly toxic. I’m a non-scientist so reading the paper was a little difficult. It seemed to be saying that some strains were made more susceptible to echinocandin drugs, but not diflucan (fluconazole). I may go ahead and try it anyway, or at least wait back on a lab result that should tell me the strain that I have and what agents it is resistant against.
Cheers!
p.s. I don’t think the email notification of new comments works for me. I checked my spam and it was not there either.
Hi Yves,
I’ll see if I can test the email notification feature. Thanks for letting me know.
Paul
Hi Paul,
I’d just like to point out that – at least in my case – your method to raise HDL appears to work!
I eat lots of coconut oil/milk and butter and heavy cream. Regular IF and probably average 400 cal of startches most days; daily medium intensitity excercise and some calisthenics 3-4 times a week. I’ve basically been following the PHD closely for at least 6 months, and most suppliments except iodine. And I do not drink very often.
29 y/o male:
Total – 261
HDL – 115
LDL – 136
Tri – 49
TC/HDL ratio – 2.3
Though the lab didn’t get into LDL particle size, but with the Tri/HDL ratio I can imagine that it’s mostly the light, fluffy kind.
And I get the point regarding high HDL as a sign of possible infection, but I don’t think I’ve got any. I feel great, if that’s any measure. However, is there something I should look for? Because it seems my HDL is higher than most…
Thanks, Paul!
Hi Robert,
That’s great! Those are awesome lipids!
I wouldn’t worry about infections, some infections lower HDL. Everyone’s a little different where their HDL ends up on a good diet and lifestyle. Possibly the LDL number is slightly higher than it could be, but it’s well within the normal range (unless you’re a drug salesman).
Best, Paul
Thanks for the feedback, Paul. Much appreciated. And I thought the LDL was a little high too, but my doctor didn’t mention it. So no salesmen coming my way…yet. 😉
Unfortunately no details on the particle size, which would likely help to interpret those numbers. Either way, I’ll focus on your LDL lowering posts and see what happens in the next six months or so.
Thanks again!
I’m going to do more LDL posts soon. LDL is an interesting topic — HDL is a bit simpler so I did that first.
Hi Robert,
A couple things to consider that may put your mind a bit more at ease … it does for me! 🙂
1. This article from the Center for Preventive Medicine indicates:
“Individuals with TG below 70 do not have small, dense LDL. It would not be necessary to measure LDL particle size in these individuals.”
http://www.centerforpreventivemedicine.com/04114med_messenger.pdf
2. LDL is typically calculated (Friedewald equation) and not directly measured. There’s a belief that low fasting triglycerides can distort calculated LDL.
Using the Iranian equation, your LDL is 103.
http://healthcorrelator.blogspot.com/2010/04/friedewald-and-iranian-equations.html
http://homepages.slingshot.co.nz/~geoff36/LDL_mg.htm
Cheers!
Mark
P.S. Paul, I’m looking forward to your follow-up LDL posts!
Thanks for that info, Mark. I didn’t know lower triglycerides could skew total cholesterol numbers. I like my Iranian equation number a little better!
Hi Paul,
I saw this in the news today. Looks like the Niacin drug called Niaspin was ineffective at preventing heart attacks.
Here is the link to the news:
http://www.npr.org/blogs/health/2011/05/26/136678665/study-boosting-good-cholesterol-with-niacin-did-not-cut-heart-risks?ft=1&f=1001
Stroke risk also increased in the Niaspin group. I am amazed how the drug companies keep pushing the low cholesterol dogma. It is pure insanity.
Erik
Hi Erik,
Very interesting. This is why we don’t recommend high-dose niacin: strokes, I believe, are commonly caused by infections and niacin can promote bacterial infections.
That said, I think higher HDL is beneficial regardless of how it is raised, so the niacin does have some benefits.
I just think coconut oil delivers the same benefits, but more safely.
When I do my LDL series I’ll look into the question of whether HDL needs LDL around to deliver its benefits. It’s possible the statins might have undermined the niacin benefits.
Best, Paul
Insofar as getting more coconut oil into the diet, I have a hard time using it as a cooking oil because it alters the flavor of everything. I’ve searched but can’t find any evidence of risks associated with using refined / deodorized coconut oils, but the “paleosphere” always seems to suggest using the extra-virgin stuff. Might a refined product be detrimental or should it be considered safe?
Hi Jeff,
Refined is fine. The extra virgin is closer to the original coconut and has more coconut fiber/stuff in it. That gives flavor but also makes it less desirable as a cooking oil, and not everyone likes the flavor. Refined has less stuff, just the oils, so it’s a better cooking oil.
I don’t know how they refine it, I’m assuming there are no toxic chemicals introduced. As coconut oil is not easily denatured, it should be easy to refine it using safe physical methods.
“Seth Roberts cut his coronary artery calcification score by 24% by eating a half-stick of butter per day;perhaps butter’s HDL-raising property deserves the credit”
Its far more likely its about Vitamin K2 from the butter.
Hi Paul,
I wanted to share my recent lab tests. Here is my background information. My previous blood work was done in June of 2010. Back then, I was on a standard low fat USDA dietary guideline diet. I avoided whole milk, cream, red meat, eggs and butter. Up to that point, I never kept butter in the fridge for years except to make deserts during the holidays. I tried to keep saturated fat low and consumed a lot of whole grains and legumes. I ate Irish style oatmeal for breakfast every morning religiously. I have never had a craving for sweets and don’t consume cookies, cakes or candies. I would say my diet was mostly whole foods. It was rich in whole grains, fruits, nuts, veggies and legumes. I would eat salmon and chicken as my source of meats.
When I had my blood work done in June of 2010, I was shocked that my cholesterol was so “high” and that my HDL was somewhat on the low range. I really thought that I was doing everything right. I wasn’t overweight, had normal blood pressure, exercised daily and didn’t smoke. Things didn’t add up and that is when I decided to research more about the relationships of cholesterol and heart disease. Heart disease has always been on the back of my mind since my father, paternal grandfather and paternal uncles had bypass surgeries and heart attacks in their early 50’s. My dad had his first surgery at 48 and a second bypass three years later. So heart health is an important topic for me since I have a family history of it.
I started reading the scientific literature using the PUBMED search engine and realized that blood cholesterol and health wasn’t as clear cut as the USDA, AHA and AMA make it out to be. I also came across your work, Chris Masterjohn, Chris Kesser, and Stephan Guyenet last summer and my view of cholesterol and health changed drastically. I especially loved your writing from your blog and I ended up buying your book and following the PHD. Your book and writings have totally changed the way I think about my diet, nutrition and health. So in the past year, I have minimized grains, cut out processed food, do not eat sweets and avoid omega-6 rich cooking oils like the plague. I have increased my intake of saturated fat by several fold and use butter and coconut oil as my cooking oils. I eat eggs for breakfast and add cream/coconut milk to my coffee. I eat sardines and salmon weekly. I get plenty of sunshine and exercise several times a week. I eat just as much fruits and vegetables as I did in the past. I do however consume more sweet potatoes and potatoes. I use to avoid the “evil” potato as well! I do have to say that I do not take any supplements. I eat whole fat yogurt daily with berries and do consume a variety of nuts too. I basically do not calorie count and eat to what I feel. I have actually lost weight and my skin has become healthier as well. My lips do not become chapped like they use to in the past. I always had chapped lips for most of my life.
Here is the blood work data from June of 2010 and this month.
6/2010 9/2011 %Difference
Total Cholesterol 221 279 26%
HDL Cholesterol 42 55 31%
LDL Cholesterol Calc 159 214 35%
Total Cholest:HDL Ratio 5.3 5.1 -4%
Triglycerides levels 100 50 -50%
NON-HDL Cholesterol 179 224 25%
Lp(a) 7 nmol/L
Homocysteine
serum CRP 1.1
Hba1c 5.5%
Glucose 84 94 12%
Albumin 4.6 4.3 -7%
Alkaline Phosphatase 49 39 -20%
Aspartate Transaminase 19 25 32%
Bilirubin 1.1 0.8 -27%
Alanine Transferase 19 34 79%
So my cholesterol did go up quite a bit. I was happy to see that my HDL went up by 30% and my triglycerides dropped by 50%. So my ratio of HDL to TGs is really good. I asked my doctor to order other heart disease risk markers. Unfortunately, I don’t have them from the first visit. However, the good news is that my Lp(a) is very low and CRP as well. I haven’t received the homocysteine results yet. So it looks like my risk factors are low. My doctor wants me to schedule a follow up with him regarding the high LDL. That was the only thing he mentioned that was of concern in his opinion. I will not take statins.
Any thoughts on the high LDL level? Should I be concerned?
I have read that people on low carb diets tend to have higher LDL levels due to the way the number is calculated. My LDL is likely to be the light fluffy LDL which is less harmful indicated by the HDL/TG ratio. How should I approach my doctor in terms of addressing the high LDL? Are there other tests that you recommend? I plan to keep following the PHD.
Many thanks for your time and help.
Much appreciated,
Erik
Re: Erik
My experience is similar after going from low-fat vegetarian to something reasonably resembling PHD, except that my HDL is also quite high (always was, but much more now):
Total: 382
HDL: 157
LDL (calculated): 217
Triglycerides: 39
My doc is predictably alarmed by the LDL and wants four months of lower fat, a retest, and then, I’m sure, comes the statin pitch (he didn’t have much luck with the PSA pitch or the colonoscopy pitch, but God bless him, he keeps trying!)
I’m very nearly at the point of following the estimable Dr. Nortin Hadler’s example of refusing to let anyone ever again test my cholesterol, PSA, blood sugar, peer and slice into my colon, etc., etc. It’s not clear to me that anyone reliably knows what to do with the results of such analytical expeditions, the main consequences of which seem to be anxiety and looming threats of iatrogenesis. My primary care doc, already mildly annoyed, would not be at all amused.
Now, back to stewing over the meaning of those high cholesterol panel values…………
Re: Bill
Thanks for sharing your experience. It is interesting that not all low carb/paleo dieters experience an increase in cholesterol. Why some people see increases and others don’t is complicated. It may be due to nutrient deficiencies such as cooper or choline as Paul pointed out in his past blog:
http://perfecthealthdiet.com/?p=2547
You may of already read his LDL/HDL topics in the blog. They are quite informative. I think the difficulty is that each person has their own unique metabolism. The lipid profile could be looked as a finger print of what the body is doing. It could be a reflection of liver health, nutrient deficiencies, infections, and possibly a macronutrient composition.
I don’t know why my cholesterol responded the way it did. Perhaps, my metabolism is sensitive to long chain saturated fatty acids and it produces more LDL. I may also be deficient in some nutrients. I wonder too whether low carb diets are more prone to some nutrient deficiencies where you wouldn’t see it in a standard USDA like one. Although, the USDA diet will cause a different set of problems or deficiencies.
I don’t take supplements such as copper, iodine, or a general supplement. So I may try to see if that helps. I have read that APOe4 allele may also explain some of the responsiveness to saturated fat intake. I am thinking of asking my doctor to see if I can test for what allele I have. If that is the case, perhaps laying off saturated fat may lower it. However, that opens another question of whether that is necessary. Is higher LDL in the context of a nutrient rich and low toxic diet a problem? I don’t know.
Erik
Hi Erik,
Be sure to read this post on how low-carb can raise LDL via reductions in T3 thyroid hormone: http://perfecthealthdiet.com/?p=4457
I don’t think you should be overly concerned about the high LDL, but I would try eating more carbs and supplementing our recommended micronutrients. If you eat 1/4 lb beef liver per week, copper is not necessary. Antioxidant minerals are important, as are vitamins C, D, and K2.
You certainly should not take statins.
Calculated LDL levels are overestimated when triglycerides are low. Your numbers are high but not terribly scary, especially on a good diet.
I’m glad you’re doing well otherwise!
Best, Paul
Hi Paul,
Thanks for your reply and link. I was wondering if I had low T3 levels. I plan to ask my doctor to test for thyroid levels and a vitamin d test. I plan to try your suggestions and retest my lipids in 4-6 months. I look forward to eating more liver. My parents used to make it for me as a kid and I liked it. I use to love chicken livers too.
I have been well overall. The phd is working great for me. Also, my son’s gastrointestinal issues have been improving from the addition of probiotics and better nutrition. He is also starting to say a lot more words this summer. He is asking for things with words for the first time. I can’t say what helped him since there are so many variables interplaying but I am happy to see improvements in language. Our pediatrician was shocked and excited about his improvements. I think his probiotics, gluten free diet, vitamin supplements and intensive ABA therapy have helped a lot. My son’s autism has been a very good learning experience. I feel very lucky to have you as a fantastic resource of information.
Many thanks again for your help and kindness!
Erik