On Tuesday (Omega-3 Fats, Angiogenesis, and Cancer: Part I, April 26, 2011) I introduced the issue of possible relationships between omega-3 fatty acids, their lipid peroxidation products, and diseases of angiogenesis such as cancer, and promised to discuss a possible mechanism today.
It may be well, however, to start by saying a little bit more about the Brasky paper [1] linking prostate cancer to DHA.
Denise Minger’s Commentary on the Brasky Paper
Denise Minger wrote a commentary on this paper for Mark’s Daily Apple, which is excellent. Her conclusion – “given the oxidation-prone nature of all polyunsaturated fats, a massive intake of omega-3’s – despite their brilliance in moderation – could potentially do more harm than good” – is the proper one.
A few of Denise’s observations, however, could stand elaboration.
The study measured the fraction of serum phospholipid fatty acids in various polyunsaturated and trans-fat species, not dietary intake. This is the right parameter to measure, as fatty acid profiles can be measured precisely while dietary intakes assessed through questionnaires are notoriously unreliable. Also, phospholipids are the fats in cell membranes, and these are the ones involved in the inflammatory signaling pathways long thought to drive cancer risk. So cell membrane lipid measurements have the best chance to demonstrate a link to cancer risk.
Denise makes the important point, however, that the connection between dietary fish oil intake and serum fatty acid profile is not simple. Higher DHA intake raises phospholipid DHA levels, but lower intake of non-omega-3 fats also raises the DHA fraction. She points to a study [2] comparing a low-fat diet (20% fat, 6.7% PUFA, n-6:n-3 ratio 11.1) to a high-fat diet (45% fat, 15% PUFA, n-6:n-3 ratio 12.3). The low-fat diet had more of its fat in the form of long-chain omega-3s, but the specific DHA intake on the diets was not reported. Membrane DHA ended up 28% higher on the low-fat diet.
So if DHA is dangerous, low-fat dieters will be in the most trouble. Another reason to eat a high-fat diet!
Does this affect our interpretation of the Brasky study? I don’t think it affects it much, because study participants were healthy at the start of the study with no history of cancer and macronutrient intakes don’t vary a lot among the general public. Americans vary surprisingly little from the median of about 50% carbs, 15% protein, and 35% fat – so it’s likely that the quartile with high tissue DHA levels were also high fish oil consumers.
However, study participants were followed for 7 years, at which point their prostate cancer status was assessed. Incidence of low-grade prostate cancers had no association with start-of-the-study DHA intake, but incidence of high-grade prostate cancers was strongly associated.
Here are a couple of possible explanations for this pattern:
- DHA is bad: DHA doesn’t drive early cancer development but does drive late-stage cancer growth – i.e. the transition from low-grade to high-grade cancer. So the DHA consumers got the high-grade cancers. Angiogenesis does, in fact, drive the shift from low-grade to high-grade cancer, so a DHA-angiogenesis association would be consistent with this explanation.
- Hospital diet advice is bad: DHA was a marker at the start of the study for conscientious, educated, disciplined persons who followed health advice and ate fish oil. When these people were diagnosed with low-grade cancer, they followed the dietary advice of their cancer dietitian. The dietitian’s advice? Eat lots of wheat, whole grains, legumes, and vegetable oils. It could be the conscientious folks who followed bad diet advice from the hospital dietitian who got the high-grade cancers.
So there is a possible confounding effect.
Another of Denise’s assertions is that there is an “otherwise consistent train of research showing that DHA seems protective at best (and neutral at worst).” Now it is true that there are more studies showing DHA to have benefits against cancer than harm. But this trend is hardly consistent, and the vast majority of studies have failed to detect a relationship.
In the comments to Tuesday’s post, eric linked to a 2005 meta-review of studies on omega-3 fats and cancer. [3] The reviewers looked at 1,210 journal articles and found a mixed bag of mostly insignificant evidence:
Significant associations between omega-3 consumption and cancer risk were reported for lung cancer in two studies; for breast cancer in one; for prostate cancer in one; and for skin cancer in one. However, for lung cancer, one of the significant associations was for increased cancer risk and the other was for decreased risk (four other risk ratios were not significant for lung cancer). For breast cancer, five other estimates did not show a significant association. Only one study assessed skin cancer risk. No effects were reported for cancers of the aerodigestive tract, bladder cancer, colorectal cancer, lymphoma, ovarian cancer, pancreatic cancer, or stomach cancer. Thus, omega-3 fatty acids do not appear to decrease overall cancer risk.
Data were insufficient to permit assessment of a temporal or dose-response relationship. [3]
So the score was 4 studies finding that DHA is associated with less cancer, 1 that it is associated with more, and a boatload that it had no association.
Now there are two ways of interpreting this general insignificance of DHA against cancer. One is to note that there are slightly more studies showing DHA to have benefits than harm, and therefore to judge that DHA might be helpful against cancer.
But another, equally plausible, interpretation is this. Most Americans eat far too much omega-6, and their omega-6 to omega-3 tissue ratio is too high, which is pro-inflammatory via the COX-2 pathway. Eating omega-3s including DHA reduces inflammation by downregulating the COX-2 pathway. This accounts for the well-attested benefits of DHA against cardiovascular disease. Now, cancer is promoted by COX-2 pathway inflammation, which is why COX-2 inhibitors such as aspirin and ibuprofen are protective against cancer. [4] DHA’s action to downregulate this pathway must generate an anti-cancer effect. But, unlike aspirin and ibuprofen, DHA has no observable effect on overall cancer risk. This suggests that DHA has other effects, unrelated to its anti-inflammatory activity, that are cancer promoting. These counterbalance the benefits from its anti-inflammatory effect. If DHA has pro-angiogenic effects that are independent of COX-2 mediated inflammation, then this could account for the observations.
One reason an association of DHA with high-grade cancer may have been missed is that it would be detected only in large studies able to segregate cancers by grade. Brasky et al note:
In the European Prospective Investigation into Cancer and Nutrition (EPIC) (12), the highest quintile of percent DHA was associated with elevated risks of both low-grade (relative risk (RR) = 1.53, 95% CI: 0.96, 2.44) and high-grade (RR = 1.41, 95% CI: 0.76, 2.62) prostate cancer. They also reported significant positive associations of the percent EPA with high-grade prostate cancer (RR = 2.00, 95% CI: 1.07, 3.76). Given that the Prostate Cancer Prevention Trial and the European Prospective Investigation into Cancer and Nutrition, the 2 largest studies of blood levels of phospholipid fatty acids, reported increased risks of high-grade prostate cancer with high levels of ω-3 fatty acids, it remains a possibility that these fatty acids promote tumorigenesis. [1]
If there were no other evidence linking DHA to angiogenesis, the Brasky and EPIC study associations would be interesting, but unlikely to change anyone’s mind. Denise points out the need for other evidence – especially, mechanistic evidence – to make the connection more plausible:
We haven’t sleuthed out any mechanism that could explain why DHA (but not other polyunsaturated fats) promotes rapid tumor growth.
And this is where today’s post comes in. In fact, there is a known mechanism by which DHA but not other polyunsaturated fats can promote rapid tumor growth. Shou-Ching told me about it a few months ago.
DHA and Angiogenesis in Macular Degeneration
Let’s start by going back to 2003 and a paper on the role of a compound called carboxyethylpyrrole (CEP) in age-related macular degeneration (AMD). [5] AMD is an eye disease caused by improper angiogenesis. Basically, malformed blood vessels overgrow the eye, causing retinal detachment and blindness. It afflicts 35% of those over age 75, and is the leading cause of blindness in developed countries. CEP? Well, the paper explains:
Free radical-induced oxidation of docosahexaenoate (DHA)-containing lipids generates ω-(2-carboxyethyl)pyrrole (CEP) protein adducts that are more abundant in ocular tissues from AMD than normal human donors…. The CEP adduct uniquely indicates oxidative modification from DHA derivatives because CEP protein modifications cannot arise from any other common polyunsaturated fatty acid. [5]
CEP is uniquely produced by oxidation of DHA, not other PUFAs. Its abundance depends on DHA abundance, availability of retinyl proteins, and the level of oxidative stress.
CEP is elevated in AMD. The correlation is strong: a person in whom the immune system is trying but failing to clear elevated CEP levels almost invariably has macular degeneration (AMD):
Of individuals (n = 13) exhibiting both antigen and autoantibody levels above the mean for non-AMD controls, 92% had AMD. [5]
So CEP is a great marker for AMD. Is it causal?
Well, first it’s worth noting that the retina is uniquely vulnerable to DHA oxidation:
Although rare in most human tissues, DHA is present in ~80 mol % of the polyunsaturated lipids in photoreceptor outer segments (13). The abundance of DHA in photoreceptors, the high photooxidative stress in retina, and the fact that DHA is the most oxidizable fatty acid in humans (13) suggests that DHA oxidation products may have possible utility as biomarkers for AMD susceptibility. [5]
Oxidation is linked to AMD, and antioxidants slow AMD progression:
Oxidative damage appears to contribute to the pathogenesis of AMD (4) based on epidemiological studies showing that smoking significantly increases the risk of AMD (1, 24). The molecular mechanism for how smoking enhances the risk for AMD is not known. We speculate that reactive oxygen and nitrogen species derived from tobacco smoke in the lungs leads to oxidative protein modifications in the blood that contribute to drusen formation and choroidal neovascularization. Results from a recent clinical trial (5) also demonstrate that the progression of AMD can be slowed in some individuals by high daily doses of antioxidant vitamins and zinc. Direct evidence of oxidative damage in AMD donor eye tissues include elevated levels of CEP adducts uniquely derived from the oxidative fragmentation of DHA (6). [5]
This is where things stood in 2003. By 2010 this group, led by Case Western Reserve University chemist Robert G. Salomon, had established that administering CEP to mice can cause AMD:
To test the hypothesis that this hapten is causally involved in initiating an inflammatory response in AMD, we immunized C57BL/6J mice with mouse serum albumin (MSA) adducted with CEP. Immunized mice develop antibodies to CEP, fix complement component-3 in Bruch’s membrane, accumulate drusen below the retinal pigment epithelium during aging, show decreased a- and b-wave amplitudes in response to light, and develop lesions in the retinal pigment epithelium mimicking geographic atrophy, the blinding end-stage condition characteristic of the dry form of AMD. Inflammatory cells are present in the region of lesions and may be actively involved in the pathology observed. [6]
This constitutes the first really good animal model for AMD. [6]
How does this relate to cancer? That leads us to a Nature paper from October 2010 [7], from the group of Tatiana Byzova at the Cleveland Clinic.
DHA, Immunity, and Angiogenesis
This is a rich paper. Briefly, CEP has a physiological function: it is transiently elevated in wounds and recruits immune cells from bone marrow to the site of the wound. These immune cells further increase oxidative stress and promote angiogenesis; CEP levels are highest at the time of peak angiogenesis. CEP is highly elevated in cancers. Unlike in wounds, where CEP is elevated for a few days, in cancers CEP elevation is chronic.
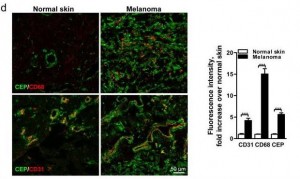
Here’s a staining comparing CEP in normal skin and in melanoma:
The CEP is co-localized with CD68, a glycoprotein which binds to LDL and is found on macrophages, and with CD31, a membrane marker of neutrophils, macrophages, and endothelial cells. CEP is marking endothelial cells and white blood cells in angiogenic vessels, and possibly LDL.
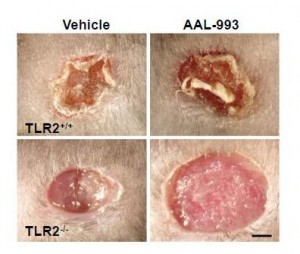
It turns out that CEP drives angiogenesis by attaching to an immune receptor, Toll-like receptor 2 (TLR2). There are two major pathways for angiogenesis: one driven by vascular endothelial growth factor (VEGF), which is dominant in conditions of hypoxia (oxygen starvation), and one by TLR2. Of these, the TLR2 pathway may in some contexts be more important. Here are pictures of wound healing in mice:
On the upper left is a normal mouse. On the upper right is a similar wound treated with the VEGF inhibitor AAL-993. This wound is rather like a cancer treated with the VEGF inhibitor Avastin. Wound healing is slightly impaired, but still works.
On the lower left is a similar wound with no VEGF inhibition, but the TLR2 pathway blocked by TLR2 knockout. The wound can’t scab and doesn’t heal successfully. If TLR2 is knocked out and VEGF inhibited, there is no wound healing at all (lower right).
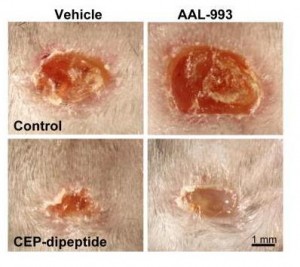
You can accelerate angiogenesis and wound healing by adding CEP to the wound.
In the bottom row, CEP has been added. Left is without VEGF inhibition, right with.
If you administer CEP-neutralizing antibodies to a normal wound, wound healing takes more than twice as long. This confirms that angiogenesis driven specifically by CEP (and therefore by DHA oxidation) is part of healthy wound healing.
Tumors use these same pathways to generate vessels and feed their growth. As the paper notes:
[T]umors implanted in TLR2-/- mice exhibited dramatically decreased vascularization and increased areas of necrosis. [7]
Here’s the paper’s conclusion:
Altogether our results establish a novel mechanism of angiogenesis that is independent of hypoxia-triggered VEGF expression. The products of lipid oxidation are generated as a consequence of oxidative stress and are recognized by TLR2, possibly in a complex with TLR1 on ECs, and promote angiogenesis in vivo, thereby contributing to accelerated wound healing and tissue recovery. If high levels of CEP and its analogs accumulate in tissues, it may lead to excessive vascularization, e.g. in tumors. Contribution of the CEP/TLR2 axis to angiogenesis varies in different physiological settings possibly depending on the extent of oxidative stress. CEP-driven angiogenesis may be an attractive therapeutic target, especially in cancers resistant to anti-VEGF therapy. Inflammation and oxidation-driven angiogenesis may occur in other pathologies, for example atherosclerosis, where arterial thickening can depend on its microvasculature. In these settings, there is an extensive generation of oxidative products which might promote atherogenesis via TLR2. Indeed, it was shown that TLR2?/? mice are protected from atherosclerosis, and this effect could be mediated by cells other than bone marrow-derived29. Thus, along with pathogen- and danger-associated molecular patterns, TLR2 recognizes an oxidation-associated molecular pattern. This new function of TLR2 as a sensor of oxidative stress reveals the shortcut link between innate immunity, oxidation and angiogenesis. [7]
Connection to Vitamin A
DHA is oxidized to a compound called HOHA which then combines with a protein, generally a retinyl (vitamin A-derived) protein to form CEP.
Cancers generate lots of CEP from DHA, and perhaps one way they do that is by generating lots of retinyl proteins. Cancers are known to have disturbed vitamin A biology with lots of retinyl:
Disturbance in vitamin A metabolism seems to be an important attribute of cancer cells. Retinoids, particularly retinoic acid, have critical regulatory functions and appear to modulate tumor development and progression. The key step of vitamin A metabolism is the esterification of all-trans retinol, catalyzed by lecithin/retinol acyltransferase. In this work we show that malignant melanoma cells are able to esterify all-trans retinol and subsequently isomerise all-trans retinyl esters into 11-cis retinol, whereas their benign counterparts – melanocytes are not able to catalyze these reactions. Besides, melanoma cell lines express lecithin/retinol acyltranseferase both at the mRNA and protein levels. In contrast, melanocytes do not express this enzyme … [8]
I haven’t looked much into this literature but it may speak to higher cancer risk with excessive vitamin A intake. Thus high-vitamin A cod liver oil may be a double risk for cancer patients.
Conclusion
It looks like we have a recipe for angiogenesis:
This recipe is invoked normally and properly during wound healing. But it is also invoked excessively in pathological contexts – notably in cancers and age-related macular degeneration, probably also in other angiogenesis-associated diseases such as arthritis, rosacea, obesity, psoriasis, endometriosis, dementia, and multiple sclerosis.
In the case of cancer, DHA oxidation to CEP might transform miniscule, harmless cancers to high-grade, life-threatening cancers.
Should this possibility affect our dietary omega-3 recommendations? Well, we need to know the relative importance of the three ingredients on the left side of the above equation in producing angiogenesis. Chris Kresser wondered in the comments Tuesday whether oxidation may be the key factor:
I question whether DHA supplementation would truly play a causative role in the absence of a *pro-oxidative environment*.
In other words, perhaps in someone eating a SAD, not exercising, under a lot of stress, etc. DHA is more easily oxidized and thus potentially carcinogenic.
But in someone that is keeping all other oxidative risk factors low (i.e. they’re avoiding n-6, exercising, managing stress, reducing exposure to chemical toxins, etc.) I tend to doubt that supplementing with DHA could cause significant harm.
That’s the last piece of the puzzle: how do we minimize the level of oxidized DHA?
As I replied to Chris in the comments, low-carb Paleo dieters are not out of the woods in regard to oxidative stress. Oxidative stress is generated normally during metabolism, immune function – and by cancers. If anti-oxidant minerals like zinc, copper, and selenium and vitamins like vitamin C are deficient, then oxidative stress can be very high on a low-carb Paleo diet.
At the moment, I think it’s prudent to eat no more than 1 pound of salmon or similar cold-water fish per week, to avoid further EPA/DHA supplements, and to avoid low-fat diets which tend to elevate membrane DHA levels. Moderate omega-3 consumption is especially important for those suffering from diseases of pathological angiogenesis – especially cancer. DHA is essential for good health – but in excess, it is probably dangerous.
References
[1] Brasky TM et al. Serum Phospholipid Fatty Acids and Prostate Cancer Risk: Results From the Prostate Cancer Prevention Trial. Am. J. Epidemiol. April 24, 2011 DOI: 10.1093/aje/kwr027 (Will be at http://pmid.us/21518693.)
[2] Raatz SK et al. Total fat intake modifies plasma fatty acid composition in humans. J Nutr. 2001 Feb;131(2):231-4. http://pmid.us/11160538.
[3] MacLean CH, Newberry SJ, Mojica WA, et al. Effects of Omega-3 Fatty Acids on Cancer. Summary, Evidence Report/Technology Assessment: Number 113. AHRQ Publication Number 05-E010-1, February 2005. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/clinic/epcsums/o3cansum.htm.
[4] Harris RE. Cyclooxygenase-2 (cox-2) and the inflammogenesis of cancer. Subcell Biochem. 2007;42:93-126. http://pmid.us/17612047.
[5] Gu X et al. Carboxyethylpyrrole protein adducts and autoantibodies, biomarkers for age-related macular degeneration. J Biol Chem. 2003 Oct 24;278(43):42027-35. http://pmid.us/12923198.
[6] Hollyfield JG et al. A hapten generated from an oxidation fragment of docosahexaenoic acid is sufficient to initiate age-related macular degeneration. Mol Neurobiol. 2010 Jun;41(2-3):290-8. http://pmid.us/20221855.
[7] West XZ et al. Oxidative stress induces angiogenesis by activating TLR2 with novel endogenous ligands. Nature. 2010 Oct 21;467(7318):972-6. http://pmid.us/20927103.
[8] Amann PM et al. Vitamin A metabolism in benign and malignant melanocytic skin cells: Importance of lecithin/retinol acyltransferase and RPE65. J Cell Physiol. 2011 Apr 4. doi: 10.1002/jcp.22779. [Epub ahead of print] http://pmid.us/21465477.











Paul, I may be your only low-brow reader, so this comment is probably an anomaly, but what I get from reading this post and others like it (not to over-simplify too much) is the PHD + suggested supplements + sensible exercise should be all we need to maintain and/or regain optimal health and weight.
I hope I’m right because it’s way too late for me get a doctorate in biology, medicine, pharmacology, nutrition and related fields that would be required for me to follow your work.
Hi erp,
I’m sorry it’s so science-rich. Unfortunately some topics are hard to address without getting technical.
I realize that few readers will want to follow such a post. Still, writing it helps me understand the literature, so helpfully I can make good recommendations at the end.
Yes, I do think your formula PHD + suggested supplements + sensible exericse is best!
Fascinating, as always. There’s also been some work done that indicates that an evolutionary balance of n6/n3 fats lowers the risk of AMD.
Could this be because as, as Chris implied, the excess n-6 is leading to n-3 oxidation?
I put up a post a while ago with three studies on this topic:
http://yelling-stop.blogspot.com/2011/02/linoleic-acid-and-blindness.html
Erp, I love the level of technical jargon in the Jaminets’ work. Along with the easy writing style, the articles are informative and practical. Too much else out there is simplistic fluff, sales pitches. If it’s too much, skip to the conclusion where the take home point is clear.
Good topic! Anthony Colpo – fish oil caps, Shane Ellison – no fish oil, WAPF – cod liver oil, PHD – eat fish. This issue needed more exploration. What a valuable website article to follow up the book’s recommendations! I have more confidence in following the guidelines and will not drop it when I read another health book.
Thanks Paul for the post. Denise Minger’s post on MDA was much more of a knee jerk take on the study re DHA and cancer, and your analysis was far more substantiated and persuasive even to a former liberal arts major, like myself.
I also appreciated your pointing out the research review on the equivocal evidence regarding fish oil and cancer, generally.
Unfortunately ocean fisheries are being wiped out as companies go for these small fish species. The fact that this is being done to provide consumers with (1) a supplement of dubious benefit and (2) supplemnts of generally low quality, processed and oxidized, is just sad.
Makes sense to me. Of course I had to be skeptical because whatever reduces inflammation always seems to prevent cancer, and DHA reduces inflammation but then again not necessarily if there is just so gosh-darn much linoleic acid hanging around in the body from soy oil. Indeed it may not be in issue in causing cancer if inflammation and insulin levels are low like they would be on a paleo diet, but give the DHA to someone who is less healthy and not even benefiting from it in the first place and your mechanism makes sense. Whatever the case, the Perfect Health Diet fish consumption recommendation is the most reasonable.
And what makes you think Denise will turn me down!? Heh, thanks for the concern, though.
Hi Jay,
I’m glad you like it! Often I write in order to learn, and just have to hope I don’t chase away too many readers in the process.
Hi Mike,
I don’t know what can be done about the overfishing problem. Too many people, too little ocean.
That’s one reason we don’t push for wild-caught salmon over farmed salmon, even though they’re healthier. If people are going to be able to eat salmon without driving them to extinction, we’ll have to be able to farm them.
Denise didn’t seem to be aware of the evidence tying DHA to angiogenesis, and she argued only for one side, but she did make a good point about the relation between diet and serum DHA.
Hi Stabby,
If she’s into fur, I think you have a shot!
Paul, thanks for putting my mind at ease. I’m in awe of the level of erudition, not only of our host, but of the others who comment here.
erp I am his other low-brow reader, constantly stunned by the level of discourse that goes on the comments here (with the exception of my own).
I arrived at the same conclusion, though I do have a question for Paul: what of “omega-3” eggs (from flaxseed-fed hens). I eat ones with “double the DHA” — http://www.egglandsbest.com/nutrition/nutrition-facts.aspx — probably 4-6 yolks a day.
I do not eat fish ever as I can’t teach myself to like it. I have fish oil spoons irregularly, maybe 2x/month.
I suspect this puts me well within “moderate” range but curious if it’s even worth opting for the omega-3 eggs any more…
I’d just like to add another fan’s voice Jaybird’s. It’s great fun that you speculate in this informed, detailed and careful but accessible manner. It inspires a lot of confidence. I do hope you continue in this vein. (If you are worried about turning away non-technical readers, an appropriate summary appended might be a a much better compromise, than simplifying the text.)
Hi John,
Those are fine. DHA levels are very low. You’re getting double of miniscule instead of miniscule.
I would recommend the omega-3 rich eggs, they should be better than the others. The chickens will be healthier with some omega-3 in their feed, they have a very omega-6 rich feed.
“I haven’t looked much into this literature but it may speak to higher cancer risk with excessive vitamin A intake.”
Gah! I’ve been specifically taking fish oil when I eat liver so that there’ll be plenty of vitamin A around to hopefully stop the fish oil oxidising…
This definitely needs more looking into. Much like with omega-3, lots of research seems to suggest that vitamin A reduces cancers (and angiogenesis in the case of vitamin A http://www.jpedsurg.org/article/S0022-3468%2879%2970118-7/abstract), so will be interesting to see what the factors that produce differing results are.
Hi David,
Vitamin A is an antioxidant and it will reduce the oxidative stress … hard to say which counts more, increased retinyl or decreased oxidation. Needs more looking into as you say!
Hi Paul,
I have to agree with Jaybird and donat. Your educational content in this blog is what made me buy the book. I have a background in nutritional science and I truly appreciate your evidence based approach to your writing.
That was very interesting how you tied DHA to CEP. I think eating fish in moderation as you suggest is a safe approach. Besides, fish contain many other nutrients besides DHA such as selenium, carotenoids, B12, etc.
I also recall reading a post from the Healthy Skeptic blog that DHA has a higher absorbtion rate from fish than supplements. That suggests that on a gram per gram basis, fish is far better than pills in terms of getting DHA and would reduce the amount of total PUFA exposure needed. Here is the link:
http://thehealthyskeptic.org/the-fish-vs-fish-oil-smackdown
Hope all is well.
Erik
Are omega-3 enriched eggs really healthy? These hens are partly fed on flaxseed meal and/or fish processing byproducts – both certain to be at least partially rancid.
Wouldn’t these rancid oils end up in the eggs?
“At the moment, I think it’s prudent to eat no more than 1 pound of salmon or similar cold-water fish per week,”
And no less?
“to avoid further EPA/DHA supplements,”
Sorry, but… further than what? I am assuming that salmon or similar cold-water fish is not a supplement.
“and to avoid low-fat diets which tend to elevate membrane DHA levels.”
Which low-fat diets are those?
Hi Peter,
Well, rancid oils are bad. We have to compare two bad diets – the bad diet that doesn’t have omega-3 and the bad diet that does. As long as the flaxseed is not too rancid, the one with omega-3 should be better.
Every animal has toxin clearing mechanisms, so rancid oils will tend to go to the liver and be cleared. Some might go to the eggs, but the bigger danger is poisoning the hen and then changes in the egg from a sick hen.
Hi Steve,
“less” – Well, that’s what I’m re-considering is whether less might be better!
We really relied on cardiovascular disease risk to estimate optimal omega-3 intake … now if omega-3s promote other diseases we have to scale back our recommendations.
However, still working on piecing together the evidence.
“further” – I meant beyond the fish recommendation.
“low-fat diets” – Say, Dean Ornish’s. I assume no one listening to our advice is on that, but maybe we get some low-fat readers through google, or maybe some of readers have relatives on low-fat diets!
Celebrex and the like increase cardiac risk while being anti-inflammatory and likely anti-cancer. Many things increase cancer risk and decrease cardiac risk (I’ve had a long day at a conference so I’m blanking on other specific examples but I used to take note of that in medical school and thought of it as a bit of a general rule) I don’t think it is all due to the old adage “you’ve gotta die of something” and since heart disease and cancer are one and two, if one doesn’t get you, the other will.
Just musing. Fascinating post. What is the cancer incidence among the Inuit, I wonder?
Sorry, for example, estrogen increases cancer risk but seems to decrease cardiac risk (at least in the context of a woman’s own natural estrogen – HRT increased both. Birth control maybe lowers cancer risk in nulliparous women, probably increases it otherwise.
Oh, and alcohol lowers cardiac risk and increases cancer risk.
(I’ll stop now)
“What is the cancer incidence among the Inuit, I wonder?”
It was nearly non-existant, until they adopted the Modern American Diet. Like all the rest of us.
Fascinating stuff! I definitely wasn’t aware of the angiogenesis connection — I just linked to your last two articles from my blog so readers can take a look at this perspective as well.
Regarding the EPIC study: although there was an association between phospholipid DHA and prostate cancer, the study failed to find a link with actual intake of fish fat: http://www.ajcn.org/content/87/5/1405.full.pdf (PDF). It could be argued that the nonassociation was due to shabby food questionnaires, though.
One other interesting thing about the Brasky study was the rate of diabetes among men with high-grade (but not low-grade) prostate cancer. It seems to corroborate other studies showing T2 diabetes is linked to aggressive prostate tumor growth (ie, http://www.nature.com/pcan/journal/v14/n1/full/pcan201041a.html). I’ve been trying to figure out if diabetes could play a role in altering the phospholipid fatty acid profile and tie in with this at all, but I haven’t found anything conclusive.
Anyway, excellent post! I think we’re mostly in agreement with all this. 🙂
““and to avoid low-fat diets which tend to elevate membrane DHA levels.””
“Which low-fat diets are those?”
This study found a membrane DHA increase using a diet with 20% versus 45% fat:
http://jn.nutrition.org/content/131/2/231.full
I’ve done a back of the envelope calculation that says that losing two pounds of fat in a week is equivalent to around 15g of dietary omega 6 PUFA per day (I actually confirmed this conceptually via email to Bill Lands) … and my old joints seem to concur.
I don’t like the idea of lots of fish oil, but have recently reintroduced it to see if it would help. It seems as if it is, tho perhaps that’s a placebo effect.
Great post – I really appreciate Paul adding balance to the DHA discussion.
In my opinion the solution to the overfished oceans is to allow property rights to be established. As long as no one owns the ocean’s resources, everyone has an incentive to grab as much as they can. As long as the open oceans are in a free-for-all state, the only reason to stop fishing is that all the fish are gone.
As (I believe) Larry Summers said, no one washes a rental car.
Hi Emily,
I think you’re right, that they benefit from opposite foods. A plant-toxin-rich diet seems more helpful with cancer, plant-toxin-poor and animal-food-rich diet with heart disease.
There’s other correlations too that are hard to account for. If you look at the specific foods that work best against cancer, they are also the best foods against fungal infections. Most anti-fungal compounds produced by plants work against cancer. I think it is not a coincidence, but I don’t know the mechanism.
Hi Denise,
Welcome! Thanks for the link.
Hi Beth,
Congrats on the weight loss!
Hi Peter,
I agree. Thanks.
Great discussion. My take away, for now, is to approach possible heart disease as a longer term, slower pathological process where fighting it or protecting against it means doing things mostly right most of the time but never to obsessively, i.e., eat whole foods in natriaul stste without doing anything weird like limiting sat fat or eating alot of PUFA’s.
On the other side is cancer with a profile more of a discrete on off state that is either dealt with or not by the body in a short or shorter time frame when compared to the more process driven pathology of long term arterial plague buildup. Did the body get the cancer cells before angiogenesis got the cells off to tumor level or didn’t it? Did it miss the threshold for success by some small fraction of normal cell biology determined maybe by a month of bad eating or 6 weeks of high stress level?
Cancer prevention may end up being nothing more than weekly house cleaning with a more intensive yearly spring cleaning. Fasting may be the key along with a periodic anti-angiogenesis hack proposed by doctor Li. Autophagy, cyclic protein restriction, occasional ketosis, and then a big angiogenesis cut off to any budding cancer cells rounding out the protocol.
erp, if it’s any comfort to you, I invariably skip to the end for the conclusions. 🙂
Question for Paul: It is my understanding that grass-fed beef has a good supply of Omega-3 — and might be a reasonable substitute for fish. Have you read anything that compares the two in that regard?
Thanks for your posts!
Marilyn, I usually read the whole post to make sure I don’t miss anything, but I am grateful when I get to the conclusion. :-]
Marilyn, I know you asked Paul, but while there are lots of good reasons to eat grass-fed beef, a source of omega 3 isn’t one of them (what little PUFA there is in beef has a better 3/6 ratio than in grain fed beef, but there’s just not a lot there).
The WAPF folks have more on this here: http://westonaprice.org/farm-a-ranch/448-splendor-from-the-grass (see the omega 3 fats sidebar).
Hi Perry – I think there’s a lot of sense in that.
Beth, thanks for answering Marilyn’s question. Yes, beef is low in PUFA of either kind, which makes it healthy, but not a substitute for fish.
Thanks, Beth and Paul. I do eat plenty of fish. The question was just out of curiosity. Thanks for the info!
Thank you so much for reviewing this issue- I just found your web site through the Minger site —
Just a tiny clarification, AMD doesn’t usually cause retinal detachments nor total blindness. The leakage and bleeding from the choroidal neovascularization will destroy the macula, but you will maintain peripheral vision. Glaucoma, on the other hand, can cause total blindness.
Thanks, Tamara.
Dear Paul
My husband has been diagnosed with Parkinson’s, and rather than just wait to see what happens we have searched the internet and came upon the Perfect Health Diet. I have read your book about four times now, and have been trying to find out what exactly he should try and do and what extra vitamins or minerals would be good in his case. Of course, we have immediately started a ketogenic diet, (and like it a lot-not difficult to stick to!),but I am not sure we are doing the optimal thing for his case. Can you give us some extra suggestions? Thanking you in advance. Cornelia
Hi Cornelia,
I’ve been meaning to look into Parkinson’s — I am collecting papers but haven’t had time to read them yet.
It’s characterized by the loss of mitochondria from the axons of neurons, which leads to loss of neuronal function.
A ketogenic diet should help, also supplements that support mitochondria. Acetylation pathways are important in Parkinson’s and can be influenced by diet, but I haven’t researched that sufficiently yet.
I believe that infections will turn out to play a major role in Parkinson’s. High immune activity in the brain leading to inflammation is characteristic of the disease. However, pathogens that cause the activity are unknown. Here’s a review: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1241555/?tool=pubmed
Your husband might want to experiment briefly with an antibiotic like doxycycline that penetrates the brain and acts as a broad-spectrum protein-synthesis inhibitor. It’s possible he might notice immediate changes in mood or cognitive abilities due to inhibition of bacterial activity. If so he should continue with antibiotics.
I would adopt and be well adapted to the diet and supplements before testing antibiotics, so that his condition is stable and it is easier to detect antibiotic effects.
Melatonin may be helpful, as the brain’s immune response downregulates its synthesis by hiding tryptophan from bacteria.
I’ll try to work on Parkinson’s when I get a chance, but the key is to get close to the optimal diet and nutrition and lifestyle (intermittent fasting, sound sleep, etc) and then experiment with possible therapies.
Best, Paul
I just bought big box of Omega-3 only to read that DHA can increase prostate cancer :/ Each pill of my fish oil have 330 Epa and 220 Dha. Product label says that I should take 2 sofgels daily, so that would give me 660 EPA and 440 dha [I guess that is 1,1 gram of EFA’s]. Is that a safe dose? I decided to take the pills because I don’t eat a lot of fish. As for others fats, I only use butter. Any advices guys?
Hi Jason,
That’s a good dose. We recommend about 1 g/day, equivalent to your 2 pills, but from fish rather than fish oil capsules: http://perfecthealthdiet.com/?p=55.
Best, Paul
Obviously everything that is fresh should be better, but I’ve heard that nowadays “fresh fish” contains a lot of dioxins, PCB and other contaminants. While fish oil capsules made by top brands are “purified” [molecularly distilled].
Yes, it’s hard to find commercial foods that can be recommended without any reservations. You have to use your judgment about which have the lowest risks.
“The relationship of dietary omega-3 long-chain polyunsaturated fatty acid intake with incident age-related macular degeneration: AREDS report no. 23.”
http://www.ncbi.nlm.nih.gov/pubmed/18779490?ordinalpos=1&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_DefaultReportPanel.Pubmed_RVDocSum
Also came across this link about the original study:
http://blog.straightchiro.com/2011/05/31/a-cancer-causing-substance-does-fish-oil-cause-prostate-cancer/
Hi Jeff,
Thanks. It looks like the benefits of fish oil dominate up to a certain point that is above where nearly everyone is. Probably 99% of the population eats too little fish oil or too much omega-6.
But it seems that artificially raising tissue DHA levels by drugs leads to trouble, and this calls into question whether huge dietary fish oil intakes may be counterproductive. Where is the bottom of the J-curve for fish oil?
Thanks for the AMD evidence.
Best, Paul