In my reply to Jimmy Moore’s safe starches symposium (see Jimmy Moore’s seminar on “safe starches”: My reply, Oct 12), I didn’t quite have time to fully address the issue of hyperglycemic toxicity.
As J Stanton commented, it would have been good to note that we recommend consuming “safe starches” as parts of meals, not as isolated snacks, and to discuss how meal design mitigates risk of hyperglycemic toxicity:
I’ve written entire articles on the fact that fat content is the primary driver of glycemic index. It’s silly to demonize white potatoes due to high GI when a couple pats of butter – or simply consuming it as part of a PHD-compliant high-fat meal – will drop it far more than substituting a sweet potato.
I thought I’d delve into the factors affecting blood glucose response to meals, and how to minimize the rise in blood sugar. It’s a topic of general interest, since hyperglycemia might have a mild detrimental health effect in nearly everyone; but of special importance to diabetics, since controlling blood sugar is so crucial to their health.
Glycemic Index of Safe Starches
The glycemic index (GI) is “defined as the area under the two hour blood glucose response curve (AUC) following the ingestion of a fixed portion of carbohydrate (usually 50 g).” Pure glucose in water is used as the reference and defines a GI of 100.
Our recommended “safe starches” are significantly lower in GI than glucose.
White rice is typically listed with a GI of 70 or 72, but it varies by strain: Bangladeshi rice has a GI of 37, American brown rice of 50, Japonica (a white short-grained rice) of 48, Basmati rice of 58, Chinese vermicelli of 58, American long-grain rice of 61, risotto rice of 69, American white rice is 72, short-grain white rice is 83, and jasmine rice 89 (source).
Potatoes are a high-GI food but again the GI is highly variable. Baked white potatoes with the skin have a GI of 69, peeled their GI is 98. Yams have GI of 35 to 77 depending on how they are prepared, sweet potatoes of 44 to 94 (source).
With some foods the GI varies strongly with ripeness. Plaintains when unripe have a GI of 40 but when ripe the GI can reach 90 (source).
Taro has a GI of 48 to 56. That’s similar to many fruits, such as bananas which have a GI of 47 to 62. Tapioca has a GI of 70 if steamed, but can exceed 80 if boiled (source).
Gentle Cooking Lowers the Glycemic Index
As a rule, gentle cooking of starchy plants leads to a lower glycemic index and high cooking temperatures lead to a higher glycemic index.
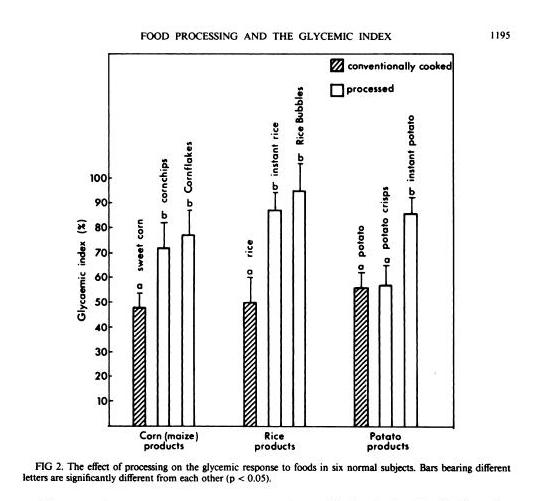
In general, industrially processed foods, which are often processed at very high temperatures to speed them through factories, have high GIs. A study in the American Journal of Clinical Nutrition [1] compared home-cooked corn, rice, and potato with processed foods based on them (instant rice, Rice Bubbles, corn chips, Cornflakes, instant potato, and potato crisps), and the processed foods had consistently higher GIs:
Another study in the British Journal of Nutrition [2] looked at 14 starchy plants prepared in different ways and found that roasting and baking raised the GI:
GI value of some of the roasted and baked foods were significantly higher than foods boiled or fried (P<0.05). The results indicate that foods processed by roasting or baking may result in higher GI. Conversely, boiling of foods may contribute to a lower GI diet.
Perhaps cooking methods that dry out the plant increase the GI.
Meals Have Lower GI
GI is calculated by eating a single food and only that food.
But what happens when you eat a meal? You’re no longer eating one food, but a mixture of foods. The baked potato may come with meat and vegetables, and with butter on top.
You might think that a weighted average of the GI of the various foods might give a good indication of the GI of the meal. Then, since fat, meat, and vegetables have a low GI, you’d expect GI of the meal to be much lower.
It turns out that the GI of meals is low – in fact, it is even lower than the average GI of the foods composing the meal.
That is the result of a new study in the American Journal of Clinical Nutrition [3]. Three meals were prepared combining a starch (potato, rice, or spaghetti) that digested to 50 g (200 calories) glucose with vegetables, sauce, and pan-fried chicken. The GIs of the meals were consistently lower than the values predicted using a weighted average of GIs of the meal components:
| Meal | Actual GI | Predicted GI |
| Potato | 53 | 63 |
| Rice | 38 | 51 |
| Spaghetti | 38 | 54 |
So eating a starch as part of a meal reduces GI to the range 38 to 53 – below the levels of many fruits and berries.
Fat Reduces GI
J Stanton has noted that adding a little fat to a starch is very effective in lowering its GI. In a post titled “Fat and Glycemic Index: The Myth of Complex Carbohydrates,” JS states that:
- Flour tortillas have a GI of 30, compared to a GI of 72 for wheat bread, because tortillas are made with lard.
- Butter reduces the glycemic index of French bread from 95 to 65.
- A Pizza Hut Super Supreme Pizza has a GI of 30, whereas a Vegetarian Supreme has a GI of 49.
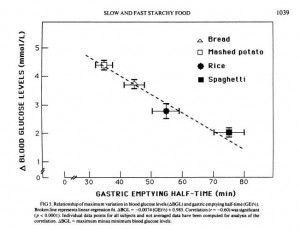
JS suggests that the reason fat does this is that it lowers the gastric emptying rate, and cites a study which showed that adding fat to starches could increase the gastric emptying time – the time for food to leave the stomach – by 50%. [4]
What’s interesting to me here is that what we really care about is not the glycemic index, but the peak blood glucose level attained after a meal. It is blood glucose levels above 140 mg/dl only that are harmful, and the harm is proportional to how high blood glucose levels rise above 140 mg/dl. So it’s the spikes we want to avoid.
But another paper shows that gastric emptying rate is even more closely tied to peak blood glucose level than it is to glycemic index. From [5]:
So combining a starch with fat may reduce peak blood glucose levels even more than it reduces the glycemic index; which is a good thing.
Dairy reduces GI
Dairy is effective at reducing GI:
[D]airy products significantly reduced the GI of white rice when consumed together, prior to or after a carbohydrate meal. [6]
It is not likely that dairy fat alone was responsible, because whole milk worked better than butter. However, low-fat milk only reduced the GI of rice by 16%, while whole milk reduced it by 41%. So clearly dairy fats are part of the recipe, but not the whole story; whey protein may also matter.
Fiber Reduces GI
Fiber is another meal element that reduces the rise in blood sugar after eating.
Removing fiber from starchy foods increases their glycemic index [7]; adding fiber decreases it. For instance, adding a polysaccharide fiber to cornstarch reduced its GI from 83 to 58; to rice reduced its GI from 82 to 45; to yogurt from 44 to 38. [8]
So it’s good to eat starches with vegetables – the foods richest in fiber.
Acids, Especially Vinegar, Reduce GI
Traditional cuisines usually make sauces by combining a fat with an acid. Frequently used sauce acids are vinegars and citric acid from lemons, limes, or other citrus fruits.
It turns that sauce acids can substantially reduce the GI of meals. The best attested is vinegar. From a study in the European Journal of Clinical Nutrition [6]:
In the current study, the addition of vinegar and vinegared foods to white rice reduced the GI of white rice. The acetic acid in vinegar was thought to be responsible for the antihyperglycemic effect. The amount of acetic acid to be effective could be as low as that found in sushi (estimated to be about 0.2–1.5 g/100 g). The antihyperglycemic effect of vinegar is consistent with other studies performed earlier (Brighenti et al, 1995; Liljeberg & Bjorck, 1998). Although vinegar could lower GI vales, the mechanism has rarely been reported. Most studies accounted the mechanism to be due to a delay in gastric emptying. In animal studies, Fushimi (Fushimi et al, 2001) showed that acetic acid could activate gluconeogenesis and induce glycogenesis in the liver after a fasting state. It could also inhibit glycolysis in muscles. [6]
Other acids also work. Pickled foods, which are sour due to lactic acid released by bacteria, reduce the glycemic index of rice by 27% if eaten before the rice and by 25% if eaten alongside the rice [6].
Wines, especially red wines, are somewhat acidic. I haven’t seen a study of how drinking wine with a meal affects glycemic index, but it is known observationally that wine drinkers have better glycemic control and, often, long lives. [9]
So What’s the Healthiest Way to Eat “Safe Starches”?
One way to limit the likelihood of reaching dangerous blood sugar levels after a meal is by eating a relatively “low carb” diet. We recommend that sedentary people eat about 400 to 600 carb calories per day. This limits the amount eaten at any one sitting to about 200 calories / 50 g, which is the amount of a typical glucose tolerance test. It is an amount the body is well able to handle.
But the manner in which carbs are eaten may be just as important as the amount.
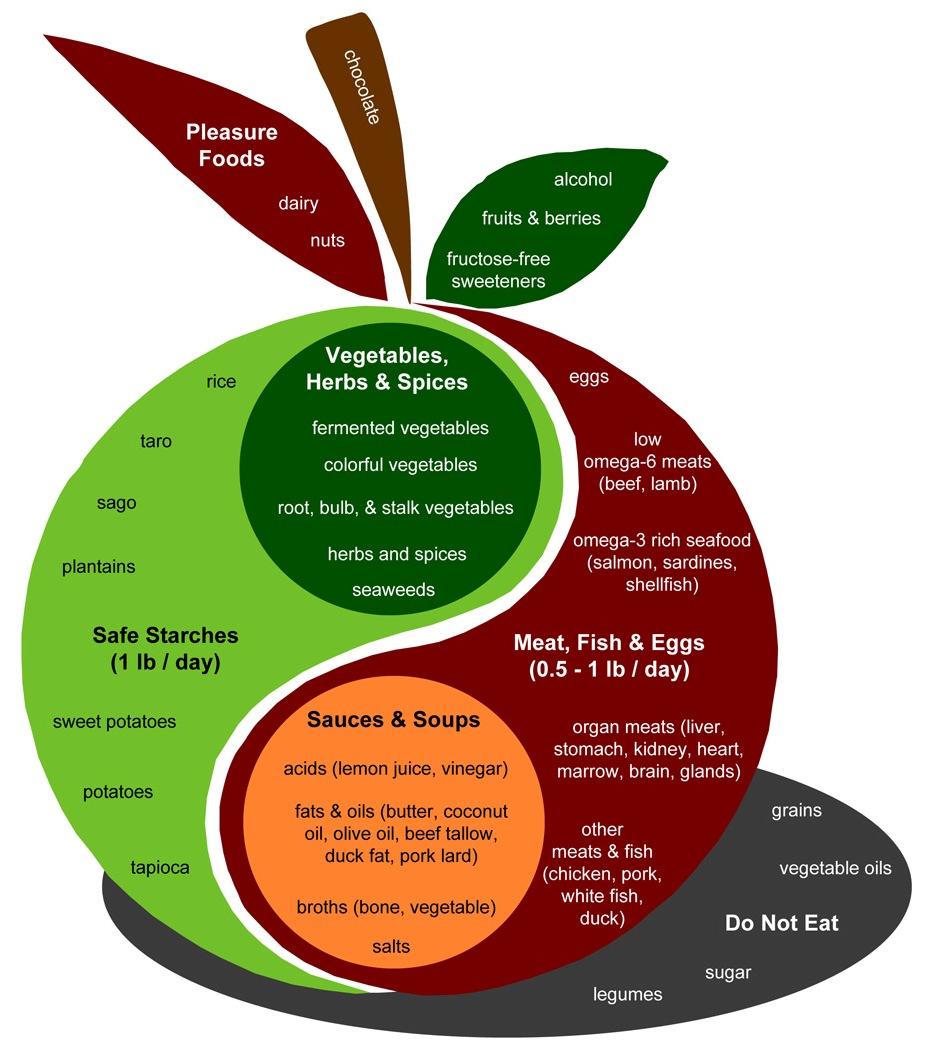
Let’s look again at the Perfect Health Diet Food Plate:
The design of a PHD meal is found in the body of the apple. Assuming two meals a day, the recipe is to combine:
- A safe starch (roughly ½ pound, which translates to 150 to 300 carb calories);
- A meat, fish, or egg (¼ to ½ pound);
- A sauce made up of fats and acids such as lemon juice or vinegar;
- Vegetables, preferably including fermented vegetables with their healthy acids;
- (Optionally) some dairy or a glass of wine.
This is precisely the recipe which science has found minimizes the elevation of blood glucose after meals.
It seems reasonable to expect that a meal designed in this fashion will have a glycemic index around 30. The odds of 200 carb calories with a glycemic index of 30 generating blood sugar levels that are dangerous – 140 mg/dl or higher – in healthy people is very low. Even in diabetics, it may be uncommon.
So, yes, Virginia. There is a Santa Claus, and you can eat safe starches and avoid hyperglycemia too!
References
[1] Brand JC et al. Food processing and the glycemic index. Am J Clin Nutr. 1985 Dec;42(6):1192-6. http://pmid.us/4072954.
[2] Bahado-Singh PS et al. Food processing methods influence the glycaemic indices of some commonly eaten West Indian carbohydrate-rich foods. Br J Nutr. 2006 Sep;96(3):476-81. http://pmid.us/16925852.
[3] Dodd H et al. Calculating meal glycemic index by using measured and published food values compared with directly measured meal glycemic index. Am J Clin Nutr. 2011 Oct;94(4):992-6. http://pmid.us/21831990.
[4] Thouvenot P et al. Fat and starch gastric emptying rate in humans: a reproducibility study of a double-isotopic technique. Am J Clin Nutr 1994;59(suppl):781S.
[5] Mourot J et al. Relationship between the rate of gastric emptying and glucose and insulin responses to starchy foods in young healthy adults. Am J Clin Nutr. 1988 Oct;48(4):1035-40. http://pmid.us/3048076.
[6] Sugiyama M et al. Glycemic index of single and mixed meal foods among common Japanese foods with white rice as a reference food. Eur J Clin Nutr. 2003 Jun;57(6):743-52. http://pmid.us/12792658. Full text: http://www.nature.com/ejcn/journal/v57/n6/full/1601606a.html.
[7] Benini L et al. Gastric emptying of a solid meal is accelerated by the removal of dietary fibre naturally present in food. Gut. 1995 Jun;36(6):825-30. http://pmid.us/7615267.
[8] Jenkins AL et al. Effect of adding the novel fiber, PGX®, to commonly consumed foods on glycemic response, glycemic index and GRIP: a simple and effective strategy for reducing post prandial blood glucose levels–a randomized, controlled trial. Nutr J. 2010 Nov 22;9:58. http://pmid.us/21092221.
[9] Perissinotto E et al. Alcohol consumption and cardiovascular risk factors in older lifelong wine drinkers: the Italian Longitudinal Study on Aging. Nutr Metab Cardiovasc Dis. 2010 Nov;20(9):647-55. http://pmid.us/19695851.











What do you think about the area under the curve (AUC) with respect to postprandial blood glucose? Is it an important factor to consider? By that I mean, the relative good or bad results from remaining at a lower absolute BG reading but over a longer period of time. As an example, hitting (only) 120 and remaining there for 3 hrs compared to a spike up to 140 at 1 hr but drops to ~100 by 2 hrs.
This is a wonderful article! Thank you for pulling together so many facts.
Another concept to consider is that eating meat increases stomach acidity and slows gastric emptying. So, if adding exogenous acid to a meal can slow gastric emptying and reduce GI, it seems like endogenous acid production should do the same.
Once again, a complete, PHD-compliant meal wins!
Finally, I think it’s important to note that GI is a very approximate number – determined empirically by making a few people eat food, testing their blood glucose, and averaging the results. Obviously the results will depend on the glycemic control of the test subjects, as well as the food itself.
In the giant list of GI values I link in my article, the values obtained for a single food vary dramatically, depending on the source. So I try to compare values taken from the same source (e.g. the meat vs. vegetarian pizza example), and when that’s not possible, I only treat large differences as significant.
The takeaway here is clear: we don’t need to worry about “complex carbohydrates” when we’re eating them as part of a nutritious, high-fat meal. I suspect we could accompany an otherwise PHD-compliant dish with 150 calories of powdered dextrose and still not suffer hyperglycemia.
JS
Another important component of PHD is that it is health-promoting and will improve insulin sensitivity through nutrition and elimination of harmful foods. Do carbohydrates cause high blood glucose? Not necessarily, insulin sensitivity and glucose transporter activity are more important.
And on that note, I remember reading about how when we sit for a long time glucose clearance becomes impaired. Not really a problem if it is hours after a meal and everything has calmed down, but what about right after a meal? Wouldn’t a walk after dinner upregulate the glucose transporters and improve glucose clearance?
And how about building some muscle? That improves the ability to clear glucose from the bloodstream as well. Some things to consider, especially for those who have previously subscribed to the strategy of not exercising and consuming little to no carbohydrate as the only dietary intervention.
Hi Lisa,
I think it’s really “area under the curve above 140 mg/dl” that we need to be concerned about. And so spending 3 hours at 130 is better than spending 30 minutes at 150.
Hi JS,
Great points. Yes, I think pure glucose should be fine too; or rice syrup.
Hi Stabby,
Great point about insulin sensitivity and glucose transporter activity. Nutrition is important for glucose transport.
And another great point about exercise and activity. I’m not sure walking immediately after a meal is helpful, but high daily activity levels certainly are. A standing desk is a good idea, and adding muscle as you say.
Best, Paul
I would think yet an additional factor is the glucose / insulin tolerance of the person eating the meal. A VLCer who eats suddenly eats a meal with a significant carb component might experience a high GI response.
I mention this with Jimmy Moore in mind specifically: when he gives the PHD a test run in November, I hope he precedes the test with a few days of easing into it so that his immediate response and results are not adversely affected by his own carb intolerance resulting purely from his historical VLC tendencies. (I also hope he tries the PHD for more than one week, which seems to be too short a time period to fairly judge the effect of it.)
Thank you for your article.
How does the microwaving affect food?
Hi Remnant,
Unfortunately, Jimmy will not be trying PHD in November. We may invite his readers to try it in December.
But I think a week should be enough for significant adaptation.
Hi Galina,
You might want to read this post: http://perfecthealthdiet.com/?p=1315.
It doesn’t affect food much.
Paul,
you make too much sense! 😉
Stabby,
interestingly Ellington Darden prescriped a 30 minute walk after dinner to aid weightloss as early as ~30 years ago. And that from a guy who is very much against all aerobic/endurance exercise.
Owning a dog may help for motivation in that regard.
Thank you Paul! That exactly answers what I was asking myself for some time: If/how the glycemic index matters. I realized that my reaction to starchy food is very different depending on the starch (I am not diabetic or otherwise affected). I tested my reaction to breakfast for I feel I can best judge if food is eaten on an empty stomach: I combined a safe starch with coconut milk, yoghurt and very little protein and observed how long they kept me full, if hunger increased gradually or if I suddenly felt weak and ravenous: Plantains are perfect, I ate them cooked and fried (not deep fried). Potatoes are fine as well, as are sweet potatoes, but I cannot imagine them as part of my breakfast on a regular basis. Fruit doesn`t keep me satisfied for a long time. The worst food for me (on an empty stomach) is rice. I feel an immense drop in my blood sugar about two hours after finishing my breakfast…Paul, as I love your recipes, I am desparately needing some ideas for breakfast: A banana and yoghurt (as mentioned in your book) makes me hungry too early but I still prefer my breakfast to be the lightest meal of the day (calorie-wise). Maybe you have a good idea apart from the typical scrambled eggs that Paleo eaters usually recommend? I work out 6-7 times a week (weight lifting, running, interval training) for 40-70 minutes. Do I qualify as someone who needs more than 600 kcal from carbs or is it fine if I stick to the higher end (150 g)? Thank you very much!
Another thing I would like to ask your opinion is a bread I have just discovered and come to like: It is made with (white) rice flour, potatoe starch, plantain flour (other ingredients are egg white and lactose) and it tastes fine, like real bread. I like it a lot and it is a possible source for starchy carbs for my daughter who eats neither rice nor rice noodles and very small amounts of potatoes. Is it fine to eat it or is it highly processed food that doesn´t have its place in a Paleo diet? Thank you?
Hello Paul,
What are your thoughts on the following article from Stephan Guyenet (2 years old min you) on the uselessness of Glycemic Index –
http://wholehealthsource.blogspot.com/2009/03/its-time-to-let-go-of-glycemic-index.html
Note there are some linked/follow-on posts referenced but I didn’t reference those above.
Warm regards,
Aravind
Your bottom line recommendations looks suspiciously like the old “Schwarzbein Square” to me! (“quality proteins, healthy fats, nonstarchy veggies, real carbohydrates”). I always try to set up my plate this way. great article, this exploration of safe starches has been fascinating.
Dan
Hi Iris,
We usually don’t eat breakfast (or we eat a banana and boiled eggs, or leftovers), so we haven’t been coming up with breakfast recipes. Luckily breakfast has been a hot topic on the Recipes thread: http://perfecthealthdiet.com/?p=1346#comment-10423, http://perfecthealthdiet.com/?p=1346#comment-10502, http://perfecthealthdiet.com/?p=1346#comment-10521, http://perfecthealthdiet.com/?p=1346#comment-15526, http://perfecthealthdiet.com/?p=1346#comment-17266, http://perfecthealthdiet.com/?p=1346#comment-17449, http://perfecthealthdiet.com/?p=1346#comment-20964, http://perfecthealthdiet.com/?p=1346#comment-22290, http://perfecthealthdiet.com/?p=1346#comment-24178,
http://perfecthealthdiet.com/?p=1346#comment-27088 and following comments, http://perfecthealthdiet.com/?p=1346#comment-27165, http://perfecthealthdiet.com/?p=1346#comment-30831, http://perfecthealthdiet.com/?p=1346#comment-30839, http://perfecthealthdiet.com/?p=1346#comment-31022.
In Asia, soups are commonly eaten for breakfast. Have a soup of beef brone broth, vegetables, with some rice and egg mixed in.
I think 600 carb calories is probably sufficient for you but 700 or 800 might not be amiss, especially on running/interval training days.
The bread sounds fine. Rice flour, potato starch, and plantain flour are all “safe starches” and ingredients we endorse. Manufacturing might increase the glycemic index a bit but it shouldn’t add toxins.
Hi Aravind,
Thanks for the link to Stephan’s piece. I agree with Stephan’s conclusions. The manner in which you eat is more important than the glycemic index of the ingredients, and glycemic index is of little practical import for weight loss or, in healthy people, for glycemic control. This is one reason why glycemic index doesn’t figure in calculating the “safeness” of a starch.
I do think glycemic index has some value for diabetics, especially those tracking their own glucose levels in response to food. But it seemed to be excessively important to many participants in Jimmy Moore’s forum.
With regard to whole dairy affecting blood sugar, a young man of my acquaintance who had become diabetic, found that eating cheese with his meals helped him achieve normal blood sugar levels. I tried it and it made no difference. I suspect that I was already eating more fat than he had been, but that is just a guess.
Hi Paul, I used to follow the higher end of carbs (150 g) and usually peak at 138 1hr pp, now I upped my carb intake at almost 350-400 grs a day and my glucose tolerance increased tremendously. After I ate 3 cups of basmati rice my 1h pp reached 110, and after almost 800 gr of baked potatoes my 1h pp peak at 112. I know that glucose clearence can improve by adding carbs on regular basis, but is it normal to rarely reach 120 1 h pp after a really high carb meal?.
Best,
Marc
Hi Dan,
The “Schwarzbein Square” was new to me, but it does look very much like our recommendations! Congrats to Diane Schwarzbein.
Hi Ellen,
It may be that the kind of cheese is important. If it’s dairy fats plus whey, then soft cheeses with milk or cream added may be needed.
Hi Marc,
Yes, it’s normal. That’s what’s commonly observed in Asia. The downside is that fasting glucose levels get lower too, and it can be tougher to tolerate long fasts. And you’ll have higher levels of glucose utilization which may not be optimal for longevity. But there are benefits to high carb consumption in glucose tolerance, that is for sure.
These last 2 articles on starches and now the glycemic index have been great! I remember reading the PHD book and thinking the one area I wished the book had covered more was the glycemic index. Covering it is only necessary because so many like you noted in the VLC paleo and higher carb paleo (Colpo – glycemic load emphasis) as well as diets outside of paleo make an issue of it. The effect of fat on the glycemic effect of starches was mentioned I believe in Fallon and Enig’s Eat Fat, Lose Fat book. They mentioned it in passing and haven’t read much since on it. Glad you followed up on that idea and clarified an issue in the back of mind for quite a while. I think the fructose not effecting glycemic index like glucose does has really skewed the diet world’s understanding of an optimal diet too.
Nice!
One problem I have with the notion of “covering” carbs with fat to reduce BG response, however, it that it is the fat + carb combos that really can pack on the pounds.
Also here’s one area I agree with the “damaged folks” in that the GI has little predictive value for the insulin resistant. Too much fat with carbs will lead to delayed glucose clearance. Many IR and type II do respond favorably to VHC, VLF diets.
Six of one, half a dozen of the other as Mom likes to say!
Ev
I have read from DrDavis “Not everybody should slow gastric emptying. Diabetics with a condition called diabetic gastroparesis should not use these methods, as they can further slow the abnormal gastric emptying that develops as part of their disease, making a bad situation worse.”
http://www.trackyourplaque.com/blog/2010/02/gastric-emptying-when-slower-is-better.html
Hi Jay,
Sooner or later, we’ll cover everything. That’s the great aspect of blogging!
Hi CarbSane,
Yes … there’s no perfect macronutrient mix for diabetics. I’m not sure it’s quite as balanced as six of one and half dozen of the other though.
Hi Lance,
That’s a great point by Dr Davis, thanks for finding it.
Your suggestion of soup as a PHD compliant meal exactly described the lunch I just finished–broth, meat, veggies, rice and an egg. Do you have suggestions on how to incorporate an acidic sauce into a soup?
Also, it seems that you favor beef broth vs. chicken broth. Is it because of Omega 3/6 ratios?
Your shared insights have encouraged my family to start incorporating more safe starches into our diet. My husband the former carb addict is thrilled!
Hi Elyse,
Your soup sounds great. Just twist a bit of lemon or lime into it, a la Pho: http://perfecthealthdiet.com/?p=2517.
Omega-6 is one reason to favor beef broth, another is that it’s easier to get thicker (more viscous) broths that we assume are more nutritious – having a lot of collagen, minerals, marrow. Also beef bone broths are less work, it’s easy to pull the bones out after long cooking.
Hi Paul
I really enjoy your blog. Ordering your book!
Is there a weight loss benefit to eating safe starches only with dinner/last meal of day?
Would doing so keep your blood sugar more stable during the day? I understand that is the thinking according to Peter at hyperlipid-optimal dieter.
I was VERY strict VLC for about 6 months. After reading your blog and archevore, I decided to add safe starches. I did so mainly because of my poor energy level, hair loss, increasing anxiety, and bad mood. Each of those symptoms developed later in the diet. Also, had very low/no sex drive, symptom my husband hated most. I added safe starches back to my diet. I am the all or nothing type, always have been. After almost three weeks one would think my rice and potato pleasures would come to an end. Moderation is hard for me. Once I add a potato then the inevitable seems to be 4 or 5 more potatoes. I do better eliminating starches than moderating them. Overeating then leads to bad anxiety and guilt feelings.
I was thinking about trying rice syrup as an alternative to starches. I still fear that rice syrup may lead to over indulging of something I had eliminated in my “paleo” diet.
My goal is to lose fat, specifically around the midsection. At the moment I feel removing safe starches is safest for me. I just can’t seem to eat a normal serving of rice. I do eat all grass fed beef, lamb, pork. I also practice a 12-15 IF daily
Actually this man was VERY specific about the type of cheese he ate: it had to be 1) raw and 2) goat or sheep and 3) mold ripened as in blue, or bloomy ( as in camembert or brie) or washed rind. The bloomy cheeses are pretty soft, but only when ripe and I don’t think any of them have extra cream or milk added
I had to mail order them to meet the requirements. They were delish. I savored them regularly for six months. But didn’t change my blood sugar one bit and were the cause of my fungal infection becoming a rash ( A big puzzle, which you helped me to figure out)
Regarding being all nor nothing with the starches, I think that this is where Stephan’s food reward ideas may help some of us.
I was not overeating to any great degree. Certainly nothing like I used to eat years ago when I ate conventional crap and junk food and would often binge. Really, it seemed to me like I have been eating very moderately for years now.
Nevertheless, reading Kessler’s book THE End of Overeating, and experimenting with some of Stephan’s ideas I am much more easily satisfied with my half cup of rice or potato when I eat them plain. My meals are becoming smaller i seem to have a better sense of how much food I really need. I didn’t realize it, but simply adding butter and salt to my rice or potatoes was increasing my desire for more starch AND more everything else. I wasn’t out of control, but I think I was overconsuming.
So it wasn’t the starch per se, but the combination, It was not even paleo junk food. It seems I am just hyper sensitive to those stimulting combinations. Possibly because I did eat a lot of junk food for many years. Or maybe just my genes.
This experiment has been less than two weeks, so it is hard to know if I will continue to lose weight or be able to continue eating so simply. Or, indeed, if I will need to be quite so pure after doing this for a while. But it has been eye opening.
At this point I do believe that some of us are just very easily stimulated by the combination of salt, fat and sugar/ starch.
Because I do have blood sugar issues and want to slow down my response to the starch, I eat butter by itself at the start of the meal if I feel that the meat will not provide enough fat. I salt my meat, but only lightly.
I have no problem with a safe starch. Makes sense… subsets of humans have adapted to eat these foods for a long time.
But what is the benefit of adding safe starches, as opposed to getting up to 100g of carbohydrates from vegetables, green leafies, etc? Is there some sort of vitamin deficiency if you stick with tons of colorful veggies instead of using rice or sweet potato?
How would someone who consumes close to 400 grams of carbohydrates from safe starches approach this? I know it’s not optimal but my sport is highly glycogen depleting.
Hi kang-yung,
I think blood glucose stays more stable if you distribute the starches through the day.
Some studies have shown a weight loss benefit to distributing carbs evenly over the day (eg http://www.ncbi.nlm.nih.gov/pubmed/18694791).
I am not sure how to interpret your desire to eat 4-5 potatoes. If these are small potatoes, that’s not very much; it could be that you are still glucose deficient and that is driving your hunger.
You shouldn’t feel anxiety or guilt over eating potatoes. Remember the guy who ate the all-potato diet (eating 6 pounds of potatoes a day or something) and lost weight. The same would probably happen to you on an all potato diet.
Another possibility is that you have glucose regulation issues leading to hypoglycemia and hunger. If so the hunger would appear hours after the carb eating, not immediately.
If the cravings are immediate, I would suggest gratifying them for a while. They’ll probably go away in time.
Hi Ellen,
Ah, well those of us with fungal infections had best stay away from moldy cheeses. I don’t know from that story whether the fungi were getting rid of a bacterial or parasite infection that caused his glucose regulation issue, or whether it was something in the cheese. Probably the former.
Your food reward comments are very interesting. It does seem like the starch – fat – salt combination is significant for a lot of people.
PS – Looking forward to seeing you at Wise Traditions!
Hi Ed,
It’s hard to get useful glucose from vegetables, they have so little and you lose nearly as much in digestion as you obtain.
Hi Robert,
If you’re a very active athlete, it’s possible that 400 g of carbs is helpful. Certainly Michael Phelps with his 12,000 calorie a day swimming protocol would have needed quite a bit more than that.
I think the approach is similar, you just eat more carbs. The macronutrient ratios might migrate toward 30-40% carbs (since exercise uses about that glucose fraction), more just before competitions. Mixing the carbs with some fat, fiber, acids will reduce the peak glucose levels which is what you want.
Best, Paul
Hi Paul
I wonder if eating the starches separately and then finishing the meal with fat might or might not decrease blood sugar without being high reward for those who have this issue?
Something completely different. Most people on Jimmy Moore’s forum are worried about your minimum carb recommendation. This is a question about the approx maximum you advise for healthy people.
Thinking of KGH’s multifuel stove analogy, Chris M’s comment about individual variability, the Kitavan-Okinavan type legacy, or even the difference between the diet-heart and the lipid-heart hypotheses.
Looking again at your book most of the carb arguments are about hyperglycemia and high insulin. But only two studies to show that high dietary carbs are the/a problem, neither of them of course looking at safe carb consumption.
You say “But the manner in which carbs are eaten may be just as important as the amount.” If only safe starches are eaten in the right manner are there any arguments that the maximum you suggest holds? Or is your current view more like: this amount is the safest bet, but we really don’t know if more is any worse (to the extent that one is metabolically healthy)?
Hi Paul,
How interesting to know that the fungus might have that benefit for us humans. But now that I think about it, why not in us since they do it in the soil?
So would you say that, even those of us with fungal issues don’t want to wipe out all fungus, just bring them into balance?
Unfortunately, I won’t be in Dallas for Wise Traditions. But do look for Harvey (he has one of his chicken books with your name on it)
I am intrigued by what you said about “fasting glucose getting low” in a high carb diet while glucose tolerance increases and that longer fasts are more difficult to tolerate. Are fasting glucose levels higher on a lower carb diet? Or did I get this wrong?
Hi donat,
That’s a great idea. I would think on Stephan’s theory eating them separately should reduce reward, while keeping the same macronutrient ratio. Might be a great way to test food reward in a controlled experiment — eat the same ingredients, just mixed or separate!
The question of what is the safe or optimal upper limit for carbs is an open issue. We have very little data because most evidence for harm from high-carb diets is confounded by the low quality / toxicity of the carb sources, esp wheat and sugar.
Asians eat low toxicity carbs, eg rice, but they have the longest lifespans, and we don’t have a lower-carb rice eating population to compare them with.
So the evidence for low-carb is mainly (a) evolutionary – eg breast milk composition, mammalian diets – and (b) based on estimates of body utilization of the nutrients, and the idea that you don’t want to force the body to convert one macronutrient into another.
This is admittedly weak evidence. Even if you buy that these show that low to moderate carb is optimal (ie evolutionarily selected), they don’t tell us whether high carb is only very slightly worse or much worse.
Hi Ellen,
It’s like the little old lady who swallowed the fly. You just hope the thing you swallow to eat the thing you swallowed earlier leaves you better off …
I think the best gut flora is probably all bacterial, but some of the worst are also, and fungal-bacterial mixes are inbetween. So taking fungi can improve some of the worst cases but harm some of the best cases.
I’ll look forward to meeting Harvey. Sorry to miss you! Shou-Ching won’t be there either, so it will be a guys weekend I guess.
Hi Iris,
Yes, low-carb diets tend to flatten blood glucose levels, lower after meals but higher after fasts.
It’s not uncommon for VLC dieters to have fasting blood glucose over 100 mg/dl. I had that and so did Peter at Hyperlipid.
Paul,
About over eating starches, I think there are two separate issues:
1) blood sugar regulation that would cause you to be hungry in an hour or so after eating.
2) over stimulation of the kind of pathway Stephan and Kessler discuss that causes you just to keep eating. That stimulation happens with the first bite of foods that are hyperpalatable for you and seems to cause compulsive eating. Being out of control cab certainly cause anxiety as Kang-Yung experienced.
In the case of 1) eating more fat with the starch itself would help. In the case of 2) it would hurt.
Most people do put butter on the potatoes or rice (as well as salt). Plus the only possible cause for overeating carbs they have considered is the carbs themselves. So unless they experiment with having the fat separately they won’t be able to tell what is going on.
A good experiment to help sort if out might be to try all three variations below and observe hunger after the meal and compulsion to eat more than you know you should.
1)no fat in the meal at all,
2)fat eaten at the same meal, but not mixed into the starch (and also with no salt on the starch)
3) as normal, with lots of butter and salt cooked into or stirred into the starch.
Ha! glad to see that you suggested the same kind of experiment while I was writing the previous comment. Makes me feel smart!!.
I might add that it would also be a good thing to check post meal blood sugars at one, two and three hours.
Hi Paul-
Would coconut oil lower the GI as well as butter?As I understand,Coconut oil requires very little digestion.
Hi Paul,
Thank you so much for your book and blog. It has helped me tremendously and I am so grateful for your and your wife’s work!!! 🙂
I feel for kang-yung. I have the same problem with her re: the all or nothing and moderation being hard. If I have some safe starches, I want more, like sweet potatoes. I feel like I could eat sweet potatoes all day long and nothing else! I have the same problem with dairy – like cheese and plain Greek yogurt. Maybe I should try eating those all day and see how long it lasts! For now, staying away from those foods seems to be the easiest thing. I do believe that the cravings are easier to manage when I eat some fat, like butter and coconut oil. Also, I believe they were worse because I wasn’t getting enough Omega 3 and too much Omega 6. (I was eating 2 chicken thighs w/ the skin every day and not eating enough salmon/seafood & red meat and organ meats.) Also, my cravings are more difficult to manage once a month probably due to hormones. And now I’m following the PHD supplement recommendations, so I think that has helped my cravings too.
Thanks again!
-Connie
Hi Ellen,
Great minds think alike! Great advice.
Hi John,
There haven’t been any experiments comparing coconut oil to butter that I’m aware of. In general coconut oil leads to lower blood sugar levels, as ketones serve as glucose substitutes, but that might take a bit of adaptation.
Hi Connie,
Thanks for sharing your experiences. I do think cravings are connected to malnutrition, so fixing an omega-3 deficiency and taking supplements should help. Also not being too low carb!
Best, Paul
To be more clear,I was referring to coconut oil lowering the GI of carbs when consumed together,not just a separate entity compared to butter.
Thanks Paul
Do you have any particular perspective on Apo E4? I’ve been diagnosed as E4/E4.
Apologies if you have written about it before, as I just can’t seem to find any refernece to it.
Many thanks!
S.
Hi John,
Yes, I understood.
Hi Stratus,
Apo E4 is the ancestral allele, everybody had it in the Paleolithic, so you should do well on a Paleo diet. Maybe not so well on a Neolithic diet.
While this isn´t related directly to the GI, I would like to ask about the thermogenetic effect of food: Carbohydrate seems to be thermogenetic and consumes some energy while being processed by the body (while fat doesn`t). Thus it seems at first glance that carb is less fattening but I do not know if this thermogenetic effect is compensated by some other factors. Also, overfeeding experiments show that only 77% of excess carbcalories are stored as fat while it is 97% for fat. Given that those studies aren`t flawed it seems that control of energy intake is more important on a high fat diet (and more difficult as it is easier to measure a potatoe than some added fat…). Is this true or did I oversimplify a process that is way more complex?
Hi Iris,
Great question … it will be the topic of upcoming blog posts! I am going to argue that paradoxically, the more thermogenic a macronutrient is, the more fattening it is.
I am looking forward to reading about the issue!
Hello Paul, I love your site… I really need to read the whole book sometime.
For some reason I thought the consensus was drifting towards the combination of fat and carb together as being more the problem. At what point does added fat to a meal become counter-productive, i.e. cause supposed insulin resistance or does it even work this way?
Despite being an extremely active 25 yr old (healthy?) male, I seem to have negative symptoms (cravings, acne lesions) from eating even a moderate amount of starch, even after say a strenuous workout or long day of work. I have three theories:
1. I eat too much fat before/during carb consumption
2. Gut issues…?
3. Omega 6 in my tissues making carb inflammatory (not sure, I go in and out of almond eating phases)
What do you think of the efficacy of eating a starch-only diet for a while (a la Chris Voigt potato diet)to sort of re-vamp my carb metabolism? As this would also clear out excess tissue PUFA? Not really sure if I have any of this right.
Your thoughts are greatly appreciated.
Hi Paul
So I eliminated safe starches for about 4 days straight. My desire for eating bowls of rice and potatoes went away once I eliminated them. Last night with my dinner, I ate about 2 cups of mashed sweet potatoes with sea salt, raw cream and butter. I usually start my meal with a normal size serving, but then sometimes go back for seconds or so. Shortly after, I also ate about 3 cups of Japanese short grain rice with raw butter and coarse sea salt. I am also believing that salt and fat do make safe starches more desirable to some people. I did want to try to give my body a chance to “regulate” itself on the carb aspect, so I do try to include them. I do think when you go from VLC to moderate carb your body is depleted and that drives up your natural senses to eat carbs/starchy foods.
Sometimes I feel like I don’t know how to eat safe starches. When eating them, I do feel more sluggish and heavy. I also experienced a bit of joint aches. For me, intermittent fasting is a bit easier on just green veggies. I still continue to fast, but I get intense hunger pains. Perhaps, these are things that will clear themselves up once safe starches are part of my diet on a more regular, normal basis.
One last thing, have you made homemade ice cream with rice syrup? I see you mention ice cream as being occasionally acceptable in some of the previous posts, what kind/brand do you prefer?
Thanks again.
“Hi Stratus,
Apo E4 is the ancestral allele, everybody had it in the Paleolithic, so you should do well on a Paleo diet. Maybe not so well on a Neolithic diet.”
Hmmm….not so sure about that!
My LDL rocketed during Paleo, as did sLDL and VLDL.
Now on low fat, mainly fish and my LDL is reducing (126). Weight down from 72kg to 64kg (6’1″)
I think a lot more careful attention should be paid to Apo E4, since it seems to account for about 40% of CVD and 50% Alzheimers disease. Paleo (in various forms) will probably do mare harm than good ,as E4’s seem to hyper-absorb dietary cholesterol.
Kind regards,
S.
Stratus,
It’s been 6 years after you posted, and a lot has been written about apoE4 since then.
I don’t know if this site touched on the topic again or not in the intervening years, but I have found that some “healthy” food and supplement recommendations for the general public are actually not so great, or are even contraindicated for people with one or two apoE4 alleles.
For example, fish and fish oil does not seem to help their brains like it does for non-apoE4 people, and it might even be a bit harmful (if I recall correctly).
There are a couple of other things too, but I forget them at the moment (probably due to my apoE4 allele, ha ha ha).
You wrote that you have 2 copies of the allele, which is more rare than having 1 copy of apoE4 and 1 copy of one of the other apo alleles, and I believe that I have read that it is much more likely that someone with 2 copies of the E4 allele will get Alzheimers than someone who has no E4 — it’s about 9 to 19 times more likely with two e4 alleles, I think, as compared to 4 to 9 times more likely with one E4 allele.
(Plus, being a woman and/or being a descendant of people from Northern Europe and having apoE4 makes Alzheimers a bit more likely than if one has apoE4 but is male and/or is not descended from Northern European peoples.)
I’ve read that if one finds out that he/she has 2 apoE4 alleles, as you did, he/she probably should see a neurologist right away, just to sort of get checked out and maybe to schedule follow-up visits and possible future interventions.
Also, if one has an apoE4 allele, it’s recommended that close relatives get tested to learn their status on it.
I asked my neurosurgeon (whom I see for a different issue) if I should see a neurologist for my one apoE4 allele
(my Alzheimers risk with the one E4 allele is a bit higher because I’m a female, 99% of my genes are from 3 countries of Northern Europe according to 23andMe, and I am rapidly approaching menopause, which apparently is a significant time of undesired dementia-related brain changes for women with apoE4),
and the answer was that with one allele, I shouldn’t specifically consult a neurologist about it, unless/until I started to have some pretty Alzheimer-ish symptoms.
I am not sure about that – it might be prudent to see one, maybe in a few years after more is known about ApoE4 – but my first point of action this year, as menopause is seemingly approaching, is to talk to my endocrinologist about the bioidentical hormone therapies that have been shown to help apoE4 women reduce their risk of developing Alzheimers (if they start those therapies at the beginning of menopause, not several years after it began.)
Stanford University is doing quite a bit of research on apoE4, and there’s quite a bit of stuff in reputable general-audience publications and on PubMed. Apparently one or two years ago, the US Govt started a 30 million dollar research study or something into apoE4. I don’t know where that stands at the moment.
I was unhappily surprised last year when,
except for the neurosurgeon (and I’m actually not 100% sure that the topic was ringing a lot of bells with that person either),
ALL of my allopathic doctors (my GP and a handful of different types of specialists), even some younger MDs in their mid-30s, told me they had never heard of apoE4, they didn’t know anything about it, and they were not interested in discussing my apoE4 allele since they had not trained on the subject. They were not interested in my PubMed information, my compiled statistics / genetic info about the different apoE alleles, or my questions about starting hormone replacement for it in order to lower my 4 to 9 times risk of getting Alzheimers. That was disheartening. It’s not a fringe / crank kind of topic!
However, due to a change in my health insurance coverage, I must find all new doctors this year (indeed, immediately, since the new year is already 1 month old), so I hope that I can find some that are still taking new patients (not easy to find in my area), are moderately decent at their job, and would be open enough to their patients’ solid, serious, scientifically-based medical issues that they would be willing to learn a little about the topics even if they had not been taught about them in medical school and had not come across the issues in their continuing education.
I noticed a few weeks ago that the ThePaleoMom site has a blogpost/article about apoE4 — though the article is a few years old now, and most of the publication references provided at the bottom of the page were even a couple of years older — which chimed with what I had learned about it in my brief research last summer.
People who have done a genetic test like 23andMe should check to see what apoE alleles they have, and if they have one or two E4s, do some reading on it and learn about the latest nutritional and lifestyle advice that is especially for E4 folks.
Hi Stratus,
I am very interested in the ApoE4 issue too. Have you read dr. BG’s relevant articles, dr. Davis’s comments related to people who have smLDL while on low carb high fat? I think dr. Kruse had an interesting comment somewhere, maybe on his blog or on paleohacks. I wonder is there any correlation with sensitivity to food reward.
Paleo doesn’t mean very low carb, high fat. If you feel better on low fat, and fish, that’s great, it is still paleo if you exclude neolithic foods (wheat, seed oils, refined sugar)
I saw a documentary on the Hadza and they were eating tubers, berries, honey and small animals, rarely zebras or bigger game. There isn’t a lot of fat in there, and the hunts are not very successful, overall meat is not that available. (The Origins of Us on BBC)
Hi Simona,
Yes, I’m aware of Dr Davis work and read some of Dr Kruse own blog on Apo E4 (although I’m still not entirely sure what he recommends us to do!).
The various iterations of Paleo can be confusing (at least for me!) abd I don’t feel better (or worse) on low fat and fish….it’s just the only thing that seems to have brought my lipids down.
My Apo B/Apo A1 ratio was absolutely horrendous (and I really mean HORRENDOUS) when eating meat and fat, however I felt fine, as I do now. The only difference is I now have a BMI of about 18.5 and everyone is saying I look much too thin (and I’m in Europe!).
S.
Hi Danny,
The cravings and acne lesions when eating starch mean you have gut dysbiosis.
Sometimes this can have simple cures. I just got an email from someone who fixed theirs simply by taking salt and betaine hydrochloride. They had a chloride deficiency / lack of stomach acid and fixing that fixed the dysbiosis.
Acne lesions may be due to circulating gut toxins or due to a small intestinal dysbiosis or oral dysbiosis. Try good oral hygiene, the salt therapy, probiotics and fermented vegetables and yogurt, and detox aids like bentonite clay, charcoal, and chlorella.
There are other things to do, like micronutrients, especially collagen support. But this can get you started.
I would eat just enough starch to test how you’re doing and be able to tell whether you’re improving or getting worse.