In my reply to Jimmy Moore’s safe starches symposium (see Jimmy Moore’s seminar on “safe starches”: My reply, Oct 12), I didn’t quite have time to fully address the issue of hyperglycemic toxicity.
As J Stanton commented, it would have been good to note that we recommend consuming “safe starches” as parts of meals, not as isolated snacks, and to discuss how meal design mitigates risk of hyperglycemic toxicity:
I’ve written entire articles on the fact that fat content is the primary driver of glycemic index. It’s silly to demonize white potatoes due to high GI when a couple pats of butter – or simply consuming it as part of a PHD-compliant high-fat meal – will drop it far more than substituting a sweet potato.
I thought I’d delve into the factors affecting blood glucose response to meals, and how to minimize the rise in blood sugar. It’s a topic of general interest, since hyperglycemia might have a mild detrimental health effect in nearly everyone; but of special importance to diabetics, since controlling blood sugar is so crucial to their health.
Glycemic Index of Safe Starches
The glycemic index (GI) is “defined as the area under the two hour blood glucose response curve (AUC) following the ingestion of a fixed portion of carbohydrate (usually 50 g).” Pure glucose in water is used as the reference and defines a GI of 100.
Our recommended “safe starches” are significantly lower in GI than glucose.
White rice is typically listed with a GI of 70 or 72, but it varies by strain: Bangladeshi rice has a GI of 37, American brown rice of 50, Japonica (a white short-grained rice) of 48, Basmati rice of 58, Chinese vermicelli of 58, American long-grain rice of 61, risotto rice of 69, American white rice is 72, short-grain white rice is 83, and jasmine rice 89 (source).
Potatoes are a high-GI food but again the GI is highly variable. Baked white potatoes with the skin have a GI of 69, peeled their GI is 98. Yams have GI of 35 to 77 depending on how they are prepared, sweet potatoes of 44 to 94 (source).
With some foods the GI varies strongly with ripeness. Plaintains when unripe have a GI of 40 but when ripe the GI can reach 90 (source).
Taro has a GI of 48 to 56. That’s similar to many fruits, such as bananas which have a GI of 47 to 62. Tapioca has a GI of 70 if steamed, but can exceed 80 if boiled (source).
Gentle Cooking Lowers the Glycemic Index
As a rule, gentle cooking of starchy plants leads to a lower glycemic index and high cooking temperatures lead to a higher glycemic index.
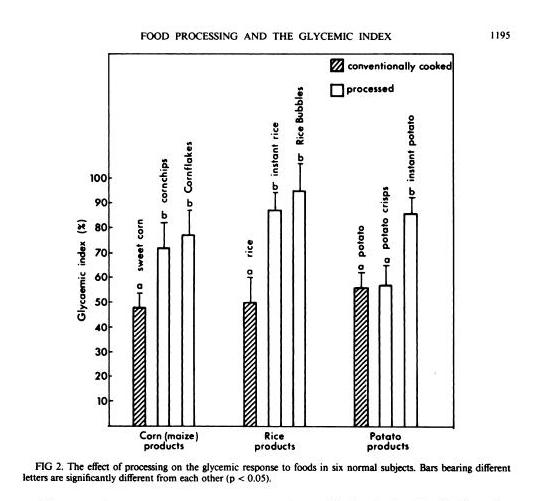
In general, industrially processed foods, which are often processed at very high temperatures to speed them through factories, have high GIs. A study in the American Journal of Clinical Nutrition [1] compared home-cooked corn, rice, and potato with processed foods based on them (instant rice, Rice Bubbles, corn chips, Cornflakes, instant potato, and potato crisps), and the processed foods had consistently higher GIs:
Another study in the British Journal of Nutrition [2] looked at 14 starchy plants prepared in different ways and found that roasting and baking raised the GI:
GI value of some of the roasted and baked foods were significantly higher than foods boiled or fried (P<0.05). The results indicate that foods processed by roasting or baking may result in higher GI. Conversely, boiling of foods may contribute to a lower GI diet.
Perhaps cooking methods that dry out the plant increase the GI.
Meals Have Lower GI
GI is calculated by eating a single food and only that food.
But what happens when you eat a meal? You’re no longer eating one food, but a mixture of foods. The baked potato may come with meat and vegetables, and with butter on top.
You might think that a weighted average of the GI of the various foods might give a good indication of the GI of the meal. Then, since fat, meat, and vegetables have a low GI, you’d expect GI of the meal to be much lower.
It turns out that the GI of meals is low – in fact, it is even lower than the average GI of the foods composing the meal.
That is the result of a new study in the American Journal of Clinical Nutrition [3]. Three meals were prepared combining a starch (potato, rice, or spaghetti) that digested to 50 g (200 calories) glucose with vegetables, sauce, and pan-fried chicken. The GIs of the meals were consistently lower than the values predicted using a weighted average of GIs of the meal components:
| Meal | Actual GI | Predicted GI |
| Potato | 53 | 63 |
| Rice | 38 | 51 |
| Spaghetti | 38 | 54 |
So eating a starch as part of a meal reduces GI to the range 38 to 53 – below the levels of many fruits and berries.
Fat Reduces GI
J Stanton has noted that adding a little fat to a starch is very effective in lowering its GI. In a post titled “Fat and Glycemic Index: The Myth of Complex Carbohydrates,” JS states that:
- Flour tortillas have a GI of 30, compared to a GI of 72 for wheat bread, because tortillas are made with lard.
- Butter reduces the glycemic index of French bread from 95 to 65.
- A Pizza Hut Super Supreme Pizza has a GI of 30, whereas a Vegetarian Supreme has a GI of 49.
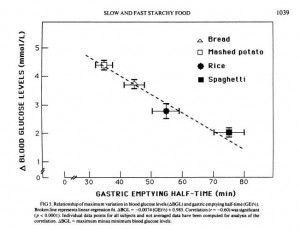
JS suggests that the reason fat does this is that it lowers the gastric emptying rate, and cites a study which showed that adding fat to starches could increase the gastric emptying time – the time for food to leave the stomach – by 50%. [4]
What’s interesting to me here is that what we really care about is not the glycemic index, but the peak blood glucose level attained after a meal. It is blood glucose levels above 140 mg/dl only that are harmful, and the harm is proportional to how high blood glucose levels rise above 140 mg/dl. So it’s the spikes we want to avoid.
But another paper shows that gastric emptying rate is even more closely tied to peak blood glucose level than it is to glycemic index. From [5]:
So combining a starch with fat may reduce peak blood glucose levels even more than it reduces the glycemic index; which is a good thing.
Dairy reduces GI
Dairy is effective at reducing GI:
[D]airy products significantly reduced the GI of white rice when consumed together, prior to or after a carbohydrate meal. [6]
It is not likely that dairy fat alone was responsible, because whole milk worked better than butter. However, low-fat milk only reduced the GI of rice by 16%, while whole milk reduced it by 41%. So clearly dairy fats are part of the recipe, but not the whole story; whey protein may also matter.
Fiber Reduces GI
Fiber is another meal element that reduces the rise in blood sugar after eating.
Removing fiber from starchy foods increases their glycemic index [7]; adding fiber decreases it. For instance, adding a polysaccharide fiber to cornstarch reduced its GI from 83 to 58; to rice reduced its GI from 82 to 45; to yogurt from 44 to 38. [8]
So it’s good to eat starches with vegetables – the foods richest in fiber.
Acids, Especially Vinegar, Reduce GI
Traditional cuisines usually make sauces by combining a fat with an acid. Frequently used sauce acids are vinegars and citric acid from lemons, limes, or other citrus fruits.
It turns that sauce acids can substantially reduce the GI of meals. The best attested is vinegar. From a study in the European Journal of Clinical Nutrition [6]:
In the current study, the addition of vinegar and vinegared foods to white rice reduced the GI of white rice. The acetic acid in vinegar was thought to be responsible for the antihyperglycemic effect. The amount of acetic acid to be effective could be as low as that found in sushi (estimated to be about 0.2–1.5 g/100 g). The antihyperglycemic effect of vinegar is consistent with other studies performed earlier (Brighenti et al, 1995; Liljeberg & Bjorck, 1998). Although vinegar could lower GI vales, the mechanism has rarely been reported. Most studies accounted the mechanism to be due to a delay in gastric emptying. In animal studies, Fushimi (Fushimi et al, 2001) showed that acetic acid could activate gluconeogenesis and induce glycogenesis in the liver after a fasting state. It could also inhibit glycolysis in muscles. [6]
Other acids also work. Pickled foods, which are sour due to lactic acid released by bacteria, reduce the glycemic index of rice by 27% if eaten before the rice and by 25% if eaten alongside the rice [6].
Wines, especially red wines, are somewhat acidic. I haven’t seen a study of how drinking wine with a meal affects glycemic index, but it is known observationally that wine drinkers have better glycemic control and, often, long lives. [9]
So What’s the Healthiest Way to Eat “Safe Starches”?
One way to limit the likelihood of reaching dangerous blood sugar levels after a meal is by eating a relatively “low carb” diet. We recommend that sedentary people eat about 400 to 600 carb calories per day. This limits the amount eaten at any one sitting to about 200 calories / 50 g, which is the amount of a typical glucose tolerance test. It is an amount the body is well able to handle.
But the manner in which carbs are eaten may be just as important as the amount.
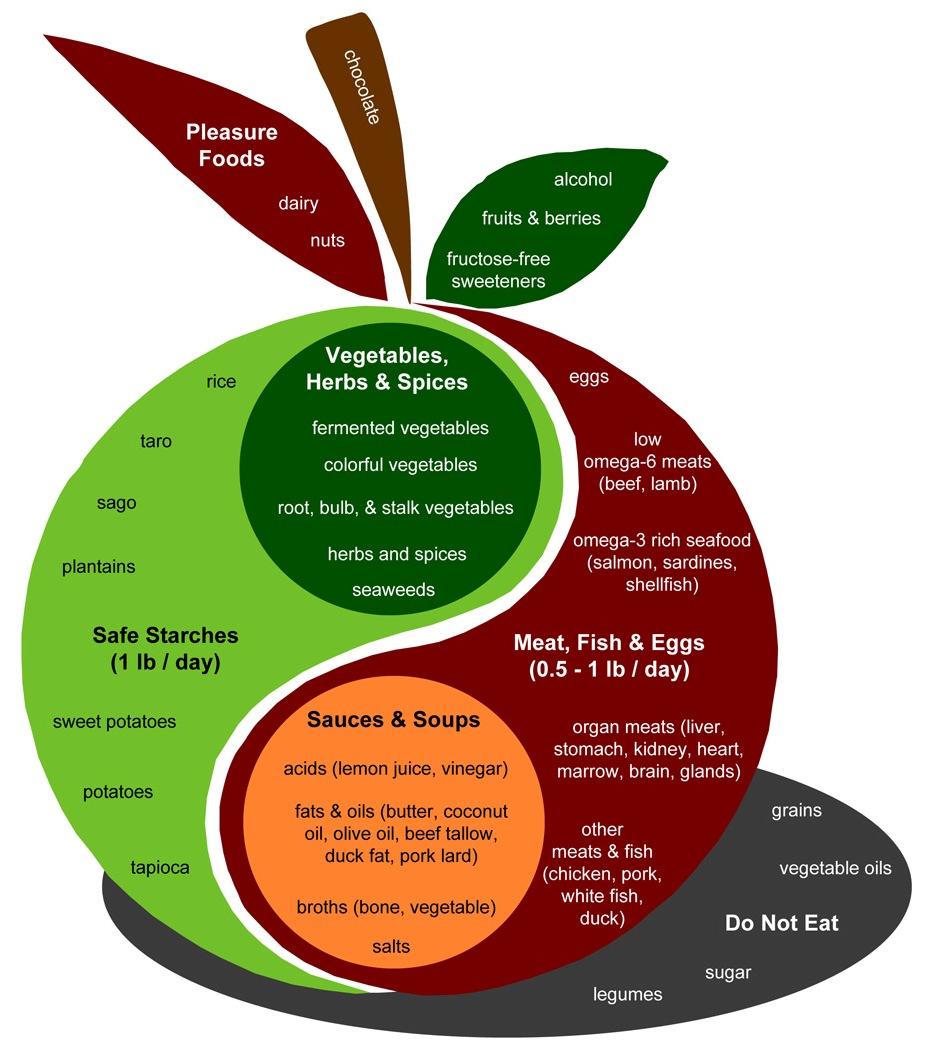
Let’s look again at the Perfect Health Diet Food Plate:
The design of a PHD meal is found in the body of the apple. Assuming two meals a day, the recipe is to combine:
- A safe starch (roughly ½ pound, which translates to 150 to 300 carb calories);
- A meat, fish, or egg (¼ to ½ pound);
- A sauce made up of fats and acids such as lemon juice or vinegar;
- Vegetables, preferably including fermented vegetables with their healthy acids;
- (Optionally) some dairy or a glass of wine.
This is precisely the recipe which science has found minimizes the elevation of blood glucose after meals.
It seems reasonable to expect that a meal designed in this fashion will have a glycemic index around 30. The odds of 200 carb calories with a glycemic index of 30 generating blood sugar levels that are dangerous – 140 mg/dl or higher – in healthy people is very low. Even in diabetics, it may be uncommon.
So, yes, Virginia. There is a Santa Claus, and you can eat safe starches and avoid hyperglycemia too!
References
[1] Brand JC et al. Food processing and the glycemic index. Am J Clin Nutr. 1985 Dec;42(6):1192-6. http://pmid.us/4072954.
[2] Bahado-Singh PS et al. Food processing methods influence the glycaemic indices of some commonly eaten West Indian carbohydrate-rich foods. Br J Nutr. 2006 Sep;96(3):476-81. http://pmid.us/16925852.
[3] Dodd H et al. Calculating meal glycemic index by using measured and published food values compared with directly measured meal glycemic index. Am J Clin Nutr. 2011 Oct;94(4):992-6. http://pmid.us/21831990.
[4] Thouvenot P et al. Fat and starch gastric emptying rate in humans: a reproducibility study of a double-isotopic technique. Am J Clin Nutr 1994;59(suppl):781S.
[5] Mourot J et al. Relationship between the rate of gastric emptying and glucose and insulin responses to starchy foods in young healthy adults. Am J Clin Nutr. 1988 Oct;48(4):1035-40. http://pmid.us/3048076.
[6] Sugiyama M et al. Glycemic index of single and mixed meal foods among common Japanese foods with white rice as a reference food. Eur J Clin Nutr. 2003 Jun;57(6):743-52. http://pmid.us/12792658. Full text: http://www.nature.com/ejcn/journal/v57/n6/full/1601606a.html.
[7] Benini L et al. Gastric emptying of a solid meal is accelerated by the removal of dietary fibre naturally present in food. Gut. 1995 Jun;36(6):825-30. http://pmid.us/7615267.
[8] Jenkins AL et al. Effect of adding the novel fiber, PGX®, to commonly consumed foods on glycemic response, glycemic index and GRIP: a simple and effective strategy for reducing post prandial blood glucose levels–a randomized, controlled trial. Nutr J. 2010 Nov 22;9:58. http://pmid.us/21092221.
[9] Perissinotto E et al. Alcohol consumption and cardiovascular risk factors in older lifelong wine drinkers: the Italian Longitudinal Study on Aging. Nutr Metab Cardiovasc Dis. 2010 Nov;20(9):647-55. http://pmid.us/19695851.











Hi Kang-yung,
I do think regular small doses of starches will help.
We do make our own ice cream with rice syrup. See http://perfecthealthdiet.com/?p=2408.
Hi Stratus,
I’ll have to read up on ApoE4. I don’t know why that happened to you.
Re: “Fat Reduces GI”
What about this ‘physiological insulin resistance’?
“Back in mid summer 2007 there was this thread on the Bernstein forum. Mark, posting as iwilsmar, asked about his gradual yet progressively rising fasting blood glucose (FBG) level over a 10 year period of paleolithic LC eating. Always eating less than 30g carbohydrate per day. Initially on LC his blood glucose was 83mg/dl but it has crept up, year by year, until now his FBG is up to 115mg/dl. Post prandial values are normal.
…
However, while muscles are in “refusal mode” for glucose the least input, from food or gluconeogenesis, will rapidly spike blood glucose out of all proportion. This is fine if you stick to LC in your eating. It also means that if you take an oral glucose tolerance test you will fail and be labelled diabetic. In fact, even a single high fat meal can do this, extending insulin resistance in to the next day. Here’s a reference for this.”
http://high-fat-nutrition.blogspot.com/2007/10/physiological-insulin-resistance.html
–
From comments section:
“I’ve noticed that since I’ve reduced my carb intake, eating a high-carb meal kicks my butt. I feel like… my blood glucose is through the roof and all my proteins are being glycated!! Seriously, I feel warm all over and tired as if I were having a systemic inflammatory response. Although it may just be my overactive imagination.”
http://www.lowcarbconversations.com/344/22-barbara-rose-dean-dwyer-paleo-guy-weston-price-gal-discuss-body-image-more/#comment-306963040
Hi Lance,
Funny, I quote that precise passage in my reply to Dr. Rosedale which will go up on Tuesday.
Eating more carbs improves glycemic control; eating carbs with fat reduces glycemic index of that meal, ie for a given level of glycemic control it reduces the rise in blood glucose. These are competing factors determining the influence of fat intake on blood glucose levels.
Hi Paul,
I’m uncertain how to classify winter squash, since it is not on your “apple guide” (unless it is considered to be a colorful vegetable). It doesn’t seem to be quite a starch, but it’s a little higher in carbs than other veggies (except maybe spaghetti squash). According to Nutrition Data, it is higher in Omega 3’s than 6’s. Yay! I love the stuff.
Also, what about parsnips? They are about as high in carbs as sweet potatoes.
It appears that mustard seed is slightly higher in Omega 3’s than 6’s. Also very tasty in many dishes.
Hi Cathryn,
Those are great foods. They are sugary, but sufficiently low in calories (below carrots, above spinach) that it really doesn’t matter. Eat as much as you like.
Interesting about mustard seed. I hadn’t thought of them as a food.
Actually Mustard is a very important food in North India. We have a whole festival dedicated to it. It also features prominently in our marriages and other customs.
We use the oil from Mustard, which is used for cooking. It is highly pungent, but people love the flavor. It does have a good amount of ALA. We also use the oil raw. It is pretty difficult for people not used to it.
Another awesome article. Thank you Paul !
Do you have any data how spices effect GI ? I remember reading something about cinnamon in Tim Ferris’s book but I’m not sure if he cites a source.
Hi Mitja,
Cinnamon is known for increasing insulin sensitivity. Many herbs have effects, and generally speaking the traditional herbs will be beneficial.
Hi, I really didn’t understand why do not eat legumes? Thank you.
Kudos.
don’t know why so many people (paleo or low carb or mainstream) make such a big deal of GI!
i wonder that’s why Japanese add vinegar to rice (sushi).
regards,
Oxalates, taro and milk AKA how things changed when part of a meal.
http://www.sciencedirect.com/science/article/pii/S0889157508001397
I didn’t know where to put, hope here is OK.
Thanks, Mik. I wonder why milk or coconut milk reduced the oxalate content.
Paul,
it’s my understanding that it’s due to calcium although I don’t know the mechanism.
Bioavailability of soluble oxalate from spinach eaten with and without milk products.
http://www.ncbi.nlm.nih.gov/pubmed/12810415
The bioavailability of oxalate from Oca (Oxalis tuberosa)
http://www.jurology.com/article/S0022-5347%2805%2965956-3/abstract
Composition and bioavailability of oxalates in baked taro (Colocasia esculenta var. Schott) leaves eaten with cows milk and cows milk and coconut milk
http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2621.2008.01855.x/abstract
I’m somewhat confused about the glycemic issues
of eating safe starches alone or with a bit of fat.
Does that cause a spike in glucose/insulin or is it
not a problem. I do understand that having safe
staches as part of a meal does not spike glucose/
insulin. I’m interested in the lower protein diet
approach to losing weight and, therefore, consuming
some safe starches with a bit of fat….
Is that a good approach to weight loss, as you
posit???
Thanks…
Linda
Hi Linda,
In general low-protein is not a good approach to weight loss, but normal protein (300-400 calories per day) can be. It’s not necessary to eat high protein as in many popular diets.
See this post for our recommendations for weight loss: http://perfecthealthdiet.com/?p=2145.
Best, Paul
Hi Paul,
Quick question regarding food combining (you are literally advocating a meat and potatoes diet here 😉 ) – what about the theory that we need to secrete different enzymes & acid at different times in differing quantities to digest different types of food (ptyalin needed for carbs is deactivated in the presence of acidic fruit, proteins shouldn’t be combined with starchy carbs, fats and fruits inhibit protein digestion, etc.). What is your take on potential putrefaction in the gut associated with bad food combining?
Thanks!
-Marc
Hi Marc,
I think the body is quite able to digest combinations of food. There may be pathologies in which separating food types is beneficial, but I don’t think normal people need to worry about how food is combined.
Best, Paul
Have you discussed your diet with Gary Taubes???
I am so interested in what his thoughts might be about the PHD….
I think he’s done a lot of solid research on the subject and I wonder what he thinks about the
starch component of recommended carb grams of the
PHD???
Linda
Hi Linda,
He knows of me, he’s emailed and we’ve met, but I haven’t asked him for an opinion of our diet and as far as I know he hasn’t expressed one. I gave him a copy of our book but I don’t know if he’s read it.
Best, Paul
I believe he once said he was thinking about eating sweet potatoes instead of wheat:
http://www.latestinpaleo.com/paleo-podcast/2011/8/29/latest-in-paleo-episode-30-gary-taubes.html and has said later
http://www.facebook.com/permalink.php?story_fbid=231431113593102&id=666889531 “I find it fascinating that some people can add starches back to their diet when they’ve plateaued and go back to losing weight. I’ll buy that that happens because one of the commenters on the blog described it. Although he doesn’t know if his weight loss would have happened anyway without the starches. That’s always possible, unlikely as it seems, and that’s why researchers do randomized controlled trials to assess the value of interventions. So I’d like to see this documented in something other than anecdotal reports. What you might consider doing, if you haven’t already, is compiling the data on these patients and posting it. Then we can get a real feel for the strength of this evidence and what to make of it.
Amusingly enough, after I first went very low carb I added back toasted pumpernickel and other low GI breads to my diet. My problem was postural hypotension and the added carbs took care of that immediately. My weight is stable also. But not with starches; with low GI wheat. “
Hi Lance,
I remember that second one, I even quoted it on the blog (in part for the disjunction between low GI wheat and starches).
My own view is that when other things are optimized, weight loss will tend to be maximized for many people with carb consumption of 400-500 calories and that many people trying VLC would lose weight faster if they added carbs.
Best, Paul
Paul:
You are wonderful for answering seemingly any and all
questions…
I know others have commented on this fact, but I am
very touched that you care so much about health that
you take the time to respond to each person and each
question.
Thank you so very much for offering so much in
personal terms. It inspires one to stay on the path…
Linda Seidman
Thank you, Linda.
Excellent post, thank you.
Do you know if after a strength training session, since the glycogen stores are partly depleted, it’s still wise to lower the GI of a meal that much? Won’t the body automatically regulate its blood glucose level below the dangerous limit by replenishing the glycogen stores?
In other words, how would you advise a bodybuilder to eat for his post workout meal?
Hi Florent,
Unless you need to recover quickly for an event or another arduous training session, I don’t think GI matters. It doesn’t change the amount of carbs coming in, just whether they’re distributed in 2 hours or 4 hours. Slower might be better.
Several people have explored the concept of “physiological insulin resistance” in response to low-carb/high-fat dieting. This is potentially dangerous, because in a person with a high degree of physiological IR, even moderate-carb foods that could ordinarily be safely handled produce wildly disproportionate spikes in blood sugar. But what is the decisive factor in producing this phenomenon? Is it the restriction in carbs, or the large quantities of fat?
In other words, what happens if you eat a moderately high amount of carbs (say 150-200 grams) with an equally high fat intake? Would this produce dangerous blood sugar levels?
It is common to see recommendations for high-carb dieting with little fat (most mainstream/vegan advice, and even some Paleo people), or high-fat dieting with few carbs (conventional Paleo advice). People like Danny Roddy advocate a high carb-to-fat ratio, and Stephan Guyenet has commented that his glucose handling improved when he switched to a high-carb, low-fat diet.
Both fat restriction (in favor of carbs) and carb restriction (in favor of fat) seem to have problems that make them sub-optimal. So what about moderately high amounts of both, especially if you are active with high energy needs? Why does this seem so rare? Are there problems with this approach as well?
Hi Jeremy,
Well, the middle ground, with a slight bias toward fat, is what we advocate.
I guess time will have to tell who is right!
I cannot imagine being able to digest 8 oz (that’s a half a pound!) of meat all in one meal. Are your stomachs made of cast iron? That much meat all in one sitting feels like a rock in my stomach.
Hi Mary,
For most women, 8 oz is an appropriate amount for one day.
I think if you ate one meal a day, you could manage 8 oz of meat.
If you have difficulty digesting protein, you might try eating extra salt and/or testing with betaine hydrochloride (to see if you lack stomach acid) or digestive enzymes (to see if you lack proteases/trypsin).
Making sure the GI of a meal is low makes everything better for me, from sleep to fasting to general energy level to immunity.
Great!
I’m wondering how you weigh white rice, cooked or raw, when figuring how much ‘safe starch’ to incorporate. Thank you!
In your book you cite a study showing eating carbs in the evening might be more beneficial. But it seems to avoid a carb overload, you would need to as you suggest in this post – breaking them up between lunch and dinner. So should carbs be just for dinner or split between lunch and dinner? Thank you
Hi Diane,
I favor splitting them between lunch and dinner.
Hi.
What about some rules making recommendations about specific combinations? Starches with protein = bad mix; acidic fruits with vegetables or starches = bad mix.
Thank you;
Eduardo
Hi Paul,
I used to be hypoglycemic and eating the PHD improved my symptoms. I used to have nocturnal hypoglycemia eating the SAD, like 40 the whole night.
Now I’ve been checking at every single night I have numbers like 100 at 2am. Every single night. When I wake up it’s always 70 or in the low 70’s.
It seems like there is a dysregulation but I don’t know why or what can I do to improve it. Can you help me and give me your opinion on why this happens?
Thank you very much and keep up the good work.
Hi Maria,
It’s usually an infection of the small intestine which has spread to the pancreas. Try getting vitamin A from liver 1/4 lb/week plus spinach, carrots, sweet potatoes; vitamin D from sun or supplements; vitamin C to about half bowel tolerance; zinc and iodine per our recommendations. Work on circadian rhythm entrainment (see chap 42) and do intermittent fasting. You want to improve immune function.
Best, Paul
Hi, Paul! So, can we mix fruits with starches and proteins and fats? Or should we eat fruits separately? What about melons?
Hi Paul,
What is the best dose-response to adding:
FAT / FRUCTOSE in minimizing the insulin response of a meal?
I know total calories increases insulin response, almost as important as high GI carb, etc.
And of course fructose is healthy in small amounts. I’ve heard you recommend 100 calories form fructose per day. I still must ask what is the least amount of fructose with greatest potential in blunting the insulin response of meals?
Henry
Hi Henry,
PHD ratios, a small amount of sweet (vegetables and maybe a bit of fruit/beets), starches, fat to taste, meat. Least amount of fructose – about 9% of the carb calories in the meal. That could be obtained with vegetables only.
Paul, What kind of rice do you usually eat? Do you avoid jasmine rice because of its high glycemic index relative to basmati? I’ve tried both the basmati and the jasmine from Lundberg in California, but I think if I eat the jasmine with vinegar and fat and with vegetables (fiber) it should be extremely blunted and safe? Thanks.
Hi Eric,
I think they’re all fine if you eat them properly.
Paul, pero si se tiene el colesterol y triglicéridos altos, se puede hacer esa mezcla de almidón con “grasa” (ejemplo:carnes) en las comidas?
Gracias
Yes. Eat our supplemental foods including liver.
I’m not sure if this is the correct place in which to ask this question, but I would like to know if cooked white rice can be a cause of (specifically, joint) inflammation? On-line information I’ve found so far has been somewhat confusing. Thank you!
Hi Paul!
A couple of studies suggesting other strategies for blood sugar regulation that haven’t been discussed in your post:
On eating rate
http://www.ncbi.nlm.nih.gov/pubmed/25484351
On viscosity
http://www.ncbi.nlm.nih.gov/pubmed/19114406
Speaking of toxicity, do you still plan blog about hyperlipidemia and excess dietary lipids in general (on your to-do list sometime ago)?
Wish you a great day..
Nice addition Gustavo, thanks!
I’ve done a lot of blog posts on hyperlipidemia. I have material for a few more but I don’t consider it a high priority. High LDL causes heart disease because it is inflammatory and because after modification of LDL it can only be taken up by white blood cells and excess of fat in white blood cells turns them to foam cells, causing atherosclerosis. This process has been discussed in our past LDL blog posts. High triglycerides is maybe a little more interesting, I haven’t blogged about that.
Thank you for the reply, Paul.
Regarding the viscosity that I mentioned before, it might be relevant in a context of starch retrogradation. I’ve been reading some studies comparing the ratio of amylose/amylopectin in starches and their postprandial effects. Some of them mentioned that while they were preparing the meals for the test, they had to add moisture to the meals to make them more palatable in those that contained significantly more amylose than amylopectin: they had become very viscous and unpalatable! They were also the ones that kept the measured markers more stable, which might indicate a good point in favour of the diet that you propose.
I second this question Paul, looking forward to this blog post.
Hi Paul,
Does ginger also work to reduce GI? How about berries and fruits? Is sourness of taste a good indicator for acidity and thus GI reducing effect?