Jimmy Moore is graciously continuing the conversation about safe starches with a post from Dr Ron Rosedale. For those trying to keep track, here’s how the discussion has gone:
- Jimmy’s original seminar on safe starches, featuring Paleo and low-carb luminaries.
- My main reply appeared both here and at Jimmy’s. I also wrote further on how to minimize hyperglycemic toxicity, and offered an appreciation of Dr Kurt Harris.
- Now, Dr Ron Rosedale has replied to my reply.
Today, I’ll reply to Dr Rosedale.
Dr Rosedale argues that glucose is toxic, so we should want to have less of it in our bodies; and that low-carb diets deliver less of it. He cites a lot of papers on the relationship between blood glucose levels and health, and uses blood glucose levels as a proxy for the level of glucose in the body.
Two basic matters are at issue: (1) What blood glucose level is best for health? (2) Which diet will generate those optimal blood glucose levels?
Let’s look at what the evidence shows.
What Blood Glucose Level is Best for Health?
In my main reply, I had written:
What is a dangerous level of blood glucose?
In diabetics, there seems to be no detectable health risk from glucose levels up to 140 mg/dl, but higher levels have risks. Neurons seem to be the most sensitive cells to high glucose levels, and the severity of neuropathy in diabetes is correlated with how high blood glucose rises above 140 mg/dl in response to a glucose tolerance test. [1] In people not diagnosed with diabetes, there is also some evidence for risks above 140 mg/dl. [2]
Dr Rosedale seemed to feel that this was the weakest point in my argument, and directed his fire here. My statement was a description of what the scientific literature shows, and the adjective “detectable” carries a lot of weight here. To refute my statement, you would have to find study subjects whose blood glucose never goes above 140 mg/dl, and yet show health impairments attributable to glucose.
Dr Rosedale argues there is no threshold separating safe from harmful levels of glucose, because glucose acts as a toxin at all concentrations:
I will spend a fair amount of time and show a fair number of studies to show that there is no threshold. Very simply, the higher the blood sugar rise, the more damage is done in some linear upward slope.
I emailed Ron to make sure that he really did mean there was no threshold, so that glycemic toxicity begins at 0 mg/dl. He replied:
I mean the former; that glucose will cause some damage when above 0 mg/dl … obviously a moot point and theoretical when glucose very low and incompatible with life and likely a minute amount of damage when that low. At any level of glucose compatible with life some more meaningful degree of glycation, hormonal response and genetic expression will take place. We will always want/need to repair the damage done to stay alive, but with age the repair mechanisms become damaged also. Eventually damage outdoes repair and we “age”, acquire chronic disease, and die.
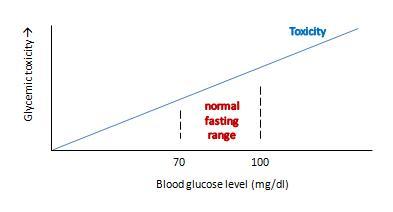
Ron’s view can be graphed like this:
This view makes sense as a matter of molecular chemistry: the number of glycation reactions may be proportional to the concentration of glucose, and if glycation products are health damaging toxins then toxicity may be proportional to glucose levels.
The trouble with this is that it doesn’t really get at what we want to know: what blood glucose level optimizes human health?
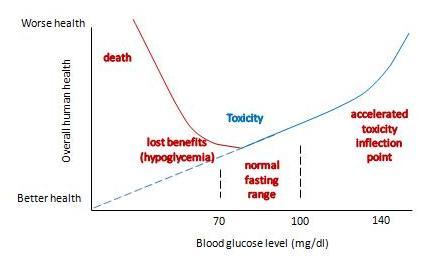
If we change the y-axis so that it doesn’t measure glycemic toxicity, but rather overall health of the human organism, then the shape of the curve is going to change in two major ways:
- First, in translating toxicity to its impact on health, we have to account for Paracelsus’s rule: “the dose makes the poison.” The body can readily repair small doses of a toxin with no ill effect – possibly even a hormetic benefit – but large doses of a toxin multiply damage exponentially and can prove fatal. So the impact of a toxin on health will not rise linearly, but non-linearly with a steeper slope as one moves to the right.
- Second, we have to account for the fact that glucose has a role as a nutrient. As Ron himself says, having too little blood glucose is “incompatible with life.” So low blood glucose – depriving us of the benefits of normal levels of this nutrient – is a catastrophic negative for health. This means that the left side of the curve needs radical adjustment.
With these two changes, our graph becomes something like this:
It now has a U-shape. I’ve drawn the inflection point where toxicity starts rising rapidly at around 140 mg/dl, and the inflection point on the other side where hypoglycemia causes substantial health damage at around 60 mg/dl. But the precise numbers don’t matter much; the point is that there is a U-shape, and somewhere in that U is a bottom where health is optimized.
What do we know about the precise shape of that U, and the location of the bottom?
We can’t intuit the shape of the bottom of the U using theoretical speculations. Theory doesn’t allow us to balance risks of hypoglycemia against toxicity on such a fine scale. The bottom of the U could be very flat, and it might not matter much whether blood glucose levels are 80 or 100 mg/dl. Or the bottom of the U could be tilted, so that the optimum is either at the low end, near 80 mg/dl, or the high end, near 100 mg/dl.
Empirical evidence is limited. Most studies relating blood glucose levels to health have been done on diabetics eating high-carb diets. There are few studies on healthy people, very few testing low-carb diets, and most are insufficiently powered to determine the precise shape of the bottom of the U.
Dr. Rosedale cites a good selection of studies in his response, and let’s review a representative subset. I was familiar with most of the studies; indeed some were cited in our book’s discussion of the dangers of hyperglycemia.
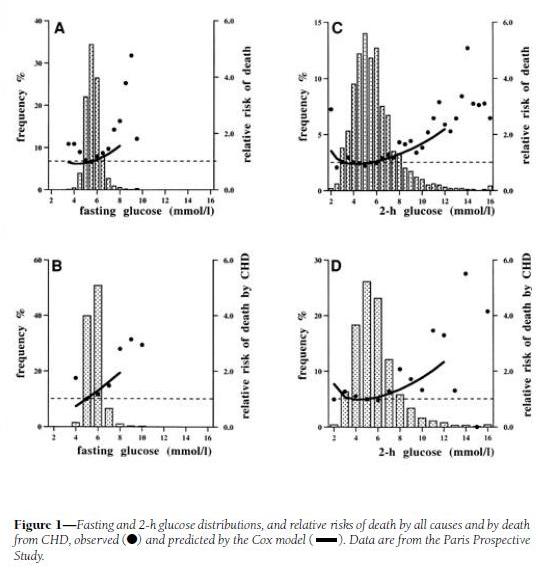
His first cite is “Is there a glycemic threshold for mortality risk?” from Diabetes Care, May 1999, http://pmid.us/10332668. Here is their data:
Look at the black dots, which are the actual data, not the fitted curves which are model-dependent; and at panels A and C, which treat all-cause mortality, not B and D, which are specific for coronary heart disease.
For both fasting and 2-h postprandial blood glucose, the black dots are lowest between about 4.5 and 6.0 mmol/l, which translates to 81 to 108 mg/dl. However, note that there is very little rise in mortality – only about 10% higher relative risk – in 2-h glucose levels of 7 mmol/l, which is 126 mg/dl. Since the postprandial peak is rarely at 2-h (45 min is a common peak), most of these people may well have been experiencing peak levels above 140 mg/dl.
My interpretation: I would say that this study demonstrates that mortality is a U-shaped function of blood glucose levels, but it doesn’t tell us the shape of the bottom of the U. It is consistent with the idea that significant health impairment occurs only with excursions of blood glucose above 140 mg/dl or below 60 mg/dl.
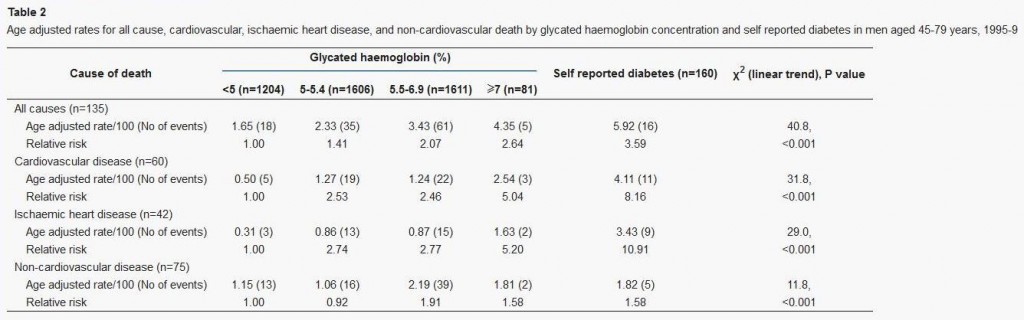
Dr Rosedale’s second cite is actually to a commentary: “‘Normal’ blood glucose and coronary risk” in the British Medical Journal, http://pmid.us/11141131, commenting on a paper by Khaw et al, “Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of european prospective investigation of cancer and nutrition (EPIC-Norfolk),” http://pmid.us/11141143.
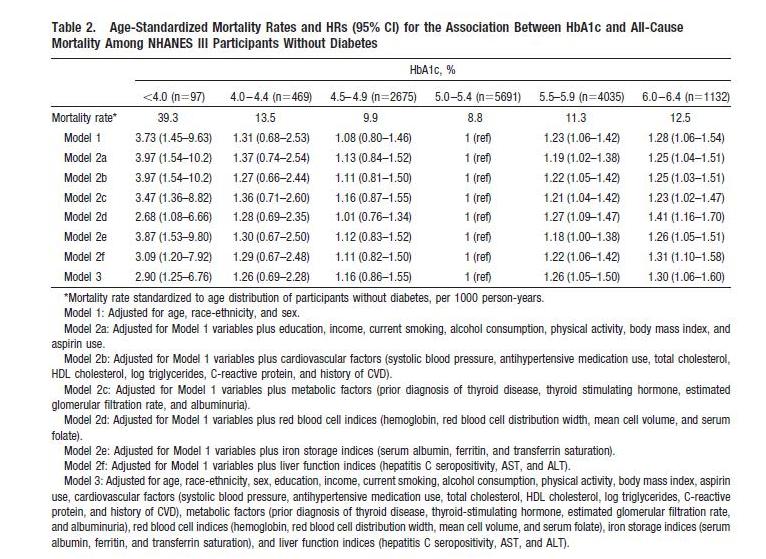
This study used glycated hemoglobin, HbA1c, which can serve as a measure of average blood glucose over the preceding ~3 weeks. Here is the data:
This supports the “blood sugar should be as low as possible” thesis, since lower HbA1c levels were associated with lower mortality. However, this study has a few flaws:
- It includes diabetics. Diabetics have poor glycemic control, and episodes of hypoglycemia as well as hyperglycemia, so HbA1c levels (which represent average blood sugar levels) may be a poor proxy for the levels of glycemic toxicity. Also, diabetics are usually on blood-glucose lowering medication, which may distort the blood sugar – mortality relationship.
- It lumps the population together in very large cohorts. Effectively there were only three cohorts, since the highest HbA1c cohort had only 2% of the sample; the other three cohorts contained 27%, 36%, and 36% of the study population respectively.
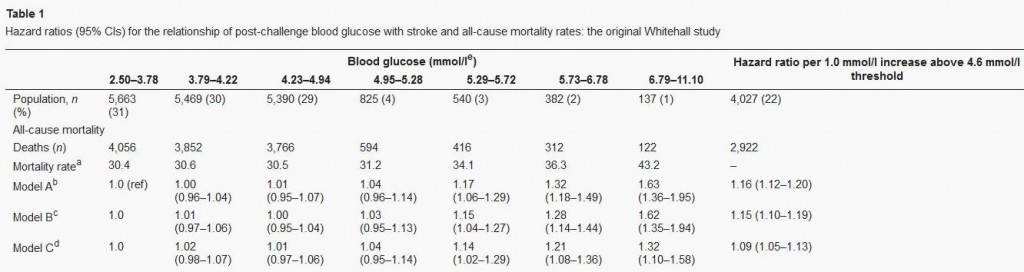
We can get a finer grip on what happens by looking at studies that lack these flaws. Here’s one: “Low hemoglobin A1c and risk of all-cause mortality among US adults without diabetes,” Circulation, 2010, http://pmid.us/20923991.
This study is an an analysis of NHANES III; it excludes diabetics and has 3 cohorts, not 1, with HbA1c below 5%. Here’s their data:
The U-shaped mortality curve is very clear. In raw data and all models, the lowest mortality is with HbA1c between 5.0 and 5.4. Mortality increases with every step down in HbA1c: in Model 1, mortality is 8% higher with HbA1c between 4.5 and 4.9, 31% higher between 4.0 and 4.4, and 273% higher below 4.0.
Via Ned Kock of Health Correlator comes a formula for translating HbA1c to average blood glucose levels:
Average blood glucose (mg/dl) = 28.7 × HbA1c – 46.7
Average blood glucose (mmol/l) = 1.59 × HbA1c – 2.59
So the minimum mortality HbA1c range of 5.0 to 5.4 translates to an average blood glucose level of 96.8 to 108.3 mg/dl (5.36 to 6.00 mmol/l).
This result is almost identical to the finding in Dr Rosedale’s first cite, from which Dr Rosedale quoted: “the lowest observed death rates were in the intervals centered on 5.5 mmol/l [99mg/dl] for fasting glucose.”
My interpretation: Once again, we find that there is a U-shaped mortality curve, and minimum mortality occurs with average or fasting blood glucose in the middle of the normal range – in the vicinity of 100 mg/dl or 5.5 mmol/l.
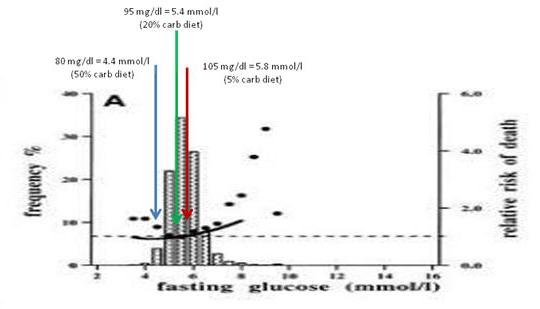
Let’s finish our examination of this issue with a quick look at Dr Rosedale’s third cite. That paper, “Post-challenge blood glucose concentration and stroke mortality rates in non-diabetic men in London: 38-year follow-up of the original Whitehall prospective cohort study,” Diabetologia, http://pmid.us/18438641, is a familiar one; it was cited in our book (p 36, fn 35).
This study looked at blood glucose levels 2 hours after swallowing 50 grams of glucose, and then followed the men for 38 years to observe mortality rates. CarbSane makes an important observation: this study used whole blood rather than plasma to assay blood glucose. Whole blood has more volume (due to inclusion of cells) but the same glucose, and so less glucose per deciliter. According to this paper, standard (plasma) values are about 25 mg/dl higher, so 95 mg/dl in whole blood actually corresponds to a plasma value of about 120 mg/dl.
Here is the data:
There is no significant difference in mortality among any group with post-challenge whole blood glucose up to 5.29 mmol/l (95 mg/dl), corresponding to 120 mg/dl or 6.7 mmol/l in standard measurements.
The study was designed to look at high blood glucose levels: there were 4 cohorts in the top 10% of blood glucose levels, but the bottom cohort in blood glucose had fully 31% of the sample. This cohort consisted of everyone with 2-hr whole blood glucose levels below 68 mg/dl, or plasma glucose below about 90 mg/dl. Mortality in this large group was indistinguishable from that in the next two groups, who had plasma glucose between 90 and 120 mg/dl.
My interpretation: This study wasn’t designed to observe the lower end of the U. At the higher end, it is consistent with the other studies: mortality rises with 2-hr plasma glucose above 120 mg/dl.
Summary: Optimal Blood Glucose Levels
All of the papers cited by Dr Rosedale are consistent with this story:
- Mortality and health have a U-shaped relationship with blood glucose.
- Optimum health occurs at blood glucose levels around 100 mg/dl – at normal levels, not exceptionally low levels.
- The impaired health seen with fasting or 2-hr blood glucose levels of 110 or 120 mg/dl may be largely attributable to the portion of the day in which those people experience blood glucose levels over 140 mg/dl.
I should note that Dr Rosedale acknowledges that high-normal blood glucose is better than low blood glucose for some aspects of health, like fertility:
Safe starch proponents say that raising blood glucose and raising insulin is a very natural phenomenon and needn’t be avoided. However, if we evolved in a certain way and with certain physiologic responses to the way we eat, it was not for a long, healthy, post-reproductive lifespan. It was for reproductive success. The two are not at all synonymous, in fact often antagonistic.
He’s saying that higher blood glucose favors “reproductive success,” while lower blood glucose favors “post-reproductive lifespan.” I guess one has to choose one’s priorities. Not everyone will choose maximum lifespan.
But suppose Dr Rosedale is right, and that low blood glucose levels are most desirable for at least some persons. I’m willing to stipulate, for the sake of argument, that optimal health for some persons may occur at below-normal blood glucose levels – say, 80 mg/dl. That brings us to the second issue: which diet will produce these low blood glucose levels?
Which Diet Minimizes Blood Glucose Levels?
If the key to health is achieving below-normal blood glucose levels, then low-carb diets are in trouble.
In general, very low-carb diets tend to raise fasting blood glucose and 2-hr glucose levels in response to an oral glucose tolerance test.
This is a well-known phenomenon in the low-carb community. When I ate a very low-carb diet, my fasting blood glucose was typically 104 mg/dl. Peter Dobromylskyj of Hyperlipid has reported the same effect: his fasting blood glucose is over 100 mg/dl. From one of Peter’s posts:
Back in mid summer 2007 there was this thread on the Bernstein forum. Mark, posting as iwilsmar, asked about his gradual yet progressively rising fasting blood glucose (FBG) level over a 10 year period of paleolithic LC eating. Always eating less than 30g carbohydrate per day. Initially on LC his blood glucose was 83mg/dl but it has crept up, year by year, until now his FBG is up to 115mg/dl….
I’ve been thinking about this for some time as my own FBG is usually five point something mmol/l whole blood. Converting my whole blood values to Mark’s USA plasma values, this works out at about 100-120mg/dl.
Peter notes that low-carb dieters will generally perform poorly on glucose tolerance tests, but that increasing carb intake to about 30% of calories is sufficient to produce a normal response to a glucose challenge:
The general opinion in LC circles is that you need 150g of carbohydrate per day for three days before an oral glucose tolerance test.
This is at the high end of the 20% to 30% of energy (400 to 600 calories on a 2000 calorie diet) that is the Perfect Health Diet recommendation for carbs.
The Kitavans eat more than 60% of calories as carbohydrate, mostly from starches. Their fasting blood glucose averages 3.7 mmol/l (67 mg/dl) (http://pmid.us/12817903).
Studies confirm that high-carb diets tend to lower fasting glucose and to lower the blood glucose response to a glucose challenge. CarbSane forwarded me some illustrative studies:
- “High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults,” http://pmid.us/2168124. Switching healthy adults to a higher carb diet reduced fasting blood glucose from 5.3 to 5.1 mmol/L (95.5 to 91.9 mg/dl) and reduced fasting insulin from 66 to 49.5 pmol/l.
- “Effect of high glucose and high sucrose diets on glucose tolerance of normal men,” http://pmid.us/4707966. On diets with glucose as the only carb source, 2-hr plasma glucose after a glucose challenge was 184 mg/dl on a 20% carb diet, 183 mg/dl on a 40% carb diet, 127 mg/dl on a 60% carb diet, and 116 mg/dl on an 80% carb diet. The 80% carb diet was the only one on which blood glucose never went above 140 mg/dl.
This last study did not report fasting glucose, but did track blood glucose for 4 hours after the glucose challenge. If we take the 4-hr blood glucose reading as representative of fasting glucose, we find that dieters eating 60% or 80% carb diets had fasting glucose of 76 and 68 mg/dl, respectively.
My interpretation of the evidence from multiple sources: A plausible conclusion is that a high-carb diet produces a low fasting glucose (let’s say, 80 mg/dl), a PHD type 20% carb diet an intermediate fasting glucose (95 mg/dl), and a very low-carb diet a high fasting glucose (say, 105 mg/dl).
Just for fun, I decided to see where these fasting glucose levels show up on the mortality plot from Balkau et al:
The 20% carb diet lines up pretty well with the mortality minimum, and both high-carb and very low-carb diets wind up at bins with slightly elevated mortality.
Now, I don’t believe we can infer from data on high-carb dieters what the relationship between blood glucose levels and mortality will be in low-carb dieters. It was Dr Rosedale, not me, who introduced this study into evidence.
But if we believe that lowest mortality really does occur with 2-hr post-challenge blood glucose around 100 mg/dl and fasting blood glucose below 100 mg/dl, as argued by the studies Dr Rosedale cited, and that this result applies to low-carb dieters, then I think the evidence is clear. One must eat some carbohydrates – at least 20-30% of energy.
This is the standard Perfect Health Diet recommendation. It seems that Dr Rosedale is supporting my diet, not his!
What About Diabetics?
Perhaps the boldest passage in Dr Rosedale’s reply was this:
We are all metabolically damaged to some extent. None of us has perfect insulin and leptin sensitivity…. It is for that reason that I say that we all have diabetes, some more than others, and should all be treated as such.
Well, if we all have diabetes, more or less, then I guess I have to consider whether our regular diet – which recommends about 20% of energy (400 calories) as carbs – is healthy for diabetics.
Now, before I begin this discussion, let me say that I don’t claim that this is optimal for diabetics. I think it is still an open question what the optimal diet for diabetics is, and different diabetics may experience a different optimum. I have often said that diabetics may benefit from going lower carb (and possibly higher protein) than our regular dietary recommendations. However, Dr Rosedale is here saying that even a healthy non-diabetic should eat a diet that is appropriate for diabetics. I want to see whether our regular diet meets that standard.
How do diabetics do on a 20% carb diet? Here’s some data that I found in a post by Stephan Guyenet at Whole Health Source. It’s from a 2004 study by Gannon & Nuttall (http://pmid.us/15331548) and the graph is from a later paper by Volek & Feinman (http://pmid.us/16288655/). Over a 24 hour period, blood glucose levels were tracked in Type II diabetics on their usual diets (blue and grey triangles) and after 5 weeks on a 55% carb – 15% protein – 30% fat (yellow circles) or 20% carb – 30% protein – 50% fat diet (blue circles):
The low-carb diet was a little higher in protein and lower in fat than we would recommend, but very close overall to our recommendations and spot-on in carbs.
What happened to blood glucose? It came close to non-diabetic levels. Fasting blood glucose dropped to 7 mmol/l (126 mg/dl), roughly the level at which diabetes is diagnosed. Postprandial blood glucose elevations were modest – peaking below 160 mg/dl which is about 20 mg/dl higher than in normal persons. Average daily blood glucose looks to be around 125 mg/dl.
What would have happened on a zero-carb diet? Fasting blood glucose probably would still have been elevated, near 126 mg/dl; this is common in diabetics because the loss of pancreatic beta cells creates a glucagon/insulin imbalance that leads to elevated fasting blood glucose. This blood glucose level would have been maintained throughout most of the day, with the postprandial peaks and troughs flattening. Average daily blood glucose level would have been similar to that on the 20% carb diet.
So the big benefit, in terms of glycemic control for diabetics, comes from reducing carbs from 55% to 20%. Further reductions in carb intake do not reduce average 24 hour blood glucose levels, but may reduce postprandial glucose spikes.
In fact, we have some Type II diabetics eating Perfect Health Diet style. Newell Wright reports good results:
I am a type II diabetic and a Perfect Health Diet follower, so I want to chime in with my experience….
I switched from the Atkins Induction diet to the Perfect Health Diet. I have been eating rice, potatoes, bananas, and other safe starches ever since, as well as fermented dairy products, such as plain, whole milk yogurt. I have also slowly lost another seven pounds. I enthusiastically recommend the book, Perfect Health Diet by Paul and Shou-Ching Jaminet.
Today, my fasting blood glucose reading was 105. Note that since following the Perfect Health Diet, my fasting blood glucose reading has gone down. Previously, I was suffering from the “dawn phenomenon.” My blood glucose levels overall were well below 140 one hour after a meal and 120 two hours after a meal. Only my fasting BG reading was out of whack, usually between 120 and 130, first thing in the morning.
For dinner tonight, I had a fatty pork rib, green beans, and a small baked potato with butter and sour cream. For dessert, I had a half cup of vanilla ice cream. One hour after eating, my blood glucose level was 128 and two hours after, it was 112.
So not only am I losing weight on the Perfect Health Diet, my blood glucose levels have actually improved, thanks to the increased carbs counteracting the dawn phenomenon, just as Dr. Kurt Harris (another proponent of safe starches) said it would.
So for me, as a type II diabetic, this “safe starches” exclusion is pointless…. [D]espite the type II diabetes, I am doing just fine on the Perfect Health Diet, thank you. I reject the diabetic exclusion of safe starches.
Note that Newell’s fasting blood glucose went down from 125 to 105 mg/dl when he raised his carb intake from Atkins Induction to Perfect Health Diet levels, and postprandial glucose levels on PHD were no higher than his fasting levels on Atkins Induction. It looks like he reduced blood glucose levels by adding starches to his diet.
To repeat: I’m not claiming that our regular diet, providing 20% of energy from “safe starches,” is optimal for diabetics. I don’t know what the optimal diabetes diet is, and it may be different for different diabetics. But I think there is plentiful evidence that even for diabetics, our “regular” diet is not a bad diet. And for some, it might be optimal.
Summary: Putting It All Together
It looks like 20% of energy is a sort of magic number for carbs. It:
- Averts glucose deficiency symptoms while achieving normal insulin sensitivity and glycemic control on oral glucose tolerance tests;
- Avoids significant hyperglycemic toxicity even in diabetics.
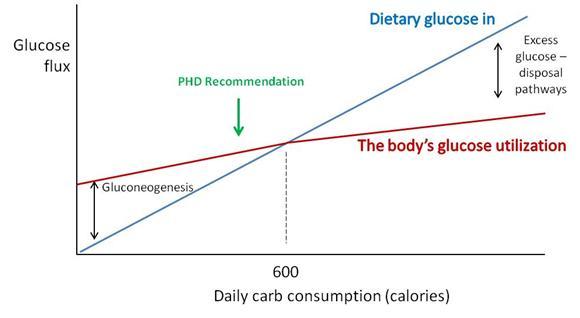
Why does this magic number, which happens to be the Perfect Health Diet recommendation for carb intake, do so well?
Perhaps a chart will make the science a little clearer.
“Dietary glucose in” (blue) represents the amount of carbs obtained from diet. “The body’s glucose utilization” (maroon) is how much glucose will be put to useful purposes at a given daily carb consumption. Glucose utilization does not vary as strongly as glucose intake; at low intakes a deficit is made up by gluconeogenesis (manufacture of glucose from protein) and at high intakes an excess of glucose is destroyed by thermogenesis or conversion of glucose to fat.
Where the blue and maroon lines cross, dietary glucose in matches the body’s glucose utilization. For most sedentary adults, this level will be around 600 carb calories per day. We recommend eating close to or slightly below this point (“PHD Recommendation”).
There are dangers in straying too far from this intersection point:
- Eating too few carbs creates a risk of health impairment due to insufficient glucose or protein.
- Eating too many carbs results in unnecessary exercise of glucose disposal pathways, and possible unhealthy fluctuations in blood glucose levels if those disposal pathways fail.
Hitting just below the intersection is a safe, low-stress point which will work well for most people.
For diabetics, the excess glucose disposal pathways are broken. However, this is not a major problem if you have no excess glucose to dispose of. Eating up to 20% of calories from carbs doesn’t require the use of disposal pathways – glucose can be stored as glycogen and then released as needed, so the effect of dietary glucose is primarily to reduce the amount of gluconeogenesis. Suppressing gluconeogenesis requires some residual insulin secretion ability, so Type I diabetics cannot achieve this, but most Type IIs can.
The upshot: A 20% carb diet meets the body’s glucose needs without much risk of hyperglycemic toxicity even in diabetics.
The Issue of Thyroid Hormones and Anti-Aging
The most distinctive element of Dr. Rosedale’s diet is its emphasis on longevity as the supreme measure of health, and its emphasis on calorie restriction (especially, carb and protein restriction) and metabolic suppression as the means to long life.
Our book, Perfect Health Diet, relied strongly on evidence from evolutionary selection to guide us toward the optimal diet.
Dr. Rosedale rejects evolutionary selection as a helpful criterion, since evolution did not necessarily select for longevity:
[I]f we evolved in a certain way and with certain physiologic responses to the way we eat, it was not for a long, healthy, post-reproductive lifespan. It was for reproductive success. The two are not at all synonymous, in fact often antagonistic. We have no footsteps to follow as far as the best way to eat for long healthy post reproductive life. We can only use the best science pertaining to the biology of aging and apply it to proper nutrition. That is what I feel I am doing.
We actually share much of Dr Rosedale’s perspective on what influences longevity; it is for longevity that we recommend slightly under-eating carb and protein compared to what evolution selects for. However, we don’t go as far in that direction as Dr Rosedale does.
We have written of the suppression of T3 thyroid hormone levels which is part of the body’s strategy for conserving glucose in times of scarcity, and how this is a risk factor for “euthyroid sick syndrome.” See Carbohydrates and the Thyroid, Aug 24, 2011.
Dr Rosedale acknowledges this and believes it to be beneficial:
I believe that Jaminet and most others misunderstand the physiologic response to low glucose, and the true meaning of low thyroid. Glucose scarcity (deficiency may be a misnomer) elicits an evolutionary response to perceived low fuel availability. This results in a shift in genetic expression to allow that organism to better survive the perceived famine…. As part of this genetic expression, and as part and parcel of nature’s mechanism to allow the maintenance of health and actually reduce the rate of aging, certain events will take place as seen in caloric restricted animals. These include a reduction in serum glucose, insulin, leptin, and free T3.
The reduction in free T3 is of great benefit, reducing temperature, metabolic damage and decreasing catabolism…. We are not talking about a hypothyroid condition. It is a purposeful reduction in thyroid activity to elicit health. Yes, reverse T3 is increased, as this is a normal, healthy, physiologic mechanism to reduce thyroid activity.
Note that Dr Rosedale acknowledges that his glucose-scarce diet reduces body temperature. Many Rosedale dieters have had this experience. Darrin didn’t like it:
This comment from Rosedale support may be of interest to you;
“The best place to measure is under the tongue. Ideal basal temperature is what you have when you first wake up in the morning, and on the Rosedale diet should be upper 96’s lower 97’s. We have found that when someone starts our diet, their basal temperature will go down about 1-2 degrees Fahrenheit which is a great improvement”.
Personally, i did not feel good on a lower body temp when i was low carb (sub 50g) & have been working hard (following phd diet & supps) to get my body temp back up. i would say my basal/morning oral temp is now around the 97.5F on average (up from around 96.5F average pre PHD).
Low body temperatures are associated with a variety of negative health outcomes. For instance, low body temperature is immunosuppressive, leads to poor outcomes in infections, and is a significant independent predictor for death in medical patients. Fever is curative for most infections, low body temperature is a risk factor for infections. Readers of our book know that we think infections are a major factor in aging and premature death. Whether a diet so restricted in carbs that it significantly lowers body temperature is really optimal for longevity is, I think, open to question.
There is a plausible case to be made for the Rosedale diet as a diet that sacrifices certain aspects of current health in the hope of extending lifespan. It cannot however claim to be the optimal diet for everyone. It is certainly not optimized for fertility, athleticism, or immunity against infections.
Conclusion
I am sympathetic to the broad perspective that underlies Dr Rosedale’s diet. Both our diets are low-carb, low-protein, and high-fat, and studies of longevity are the biggest factor motivating the recommendation to eat a fat-rich diet.
However, Dr Rosedale takes low-carb and low-protein dieting to an extreme that I think is not well supported by the evidence.
Dr Rosedale’s direct attempt at refuting our diet consists mainly of two claims:
- Lower blood glucose is better than higher blood glucose.
- The way to lower blood glucose is by eating fewer carbs.
Neither claim is supported. Mortality is a U-shaped function of blood glucose and blood glucose levels around 90 to 100 mg/dl are healthiest, not low blood glucose levels. Moreover, the diet that delivers the lowest blood glucose levels is a high-carb, insulin-sensitizing diet, such as the Kitavans eat, not a low-carb diet.
If I truly believed Dr Rosedale’s argument for lower blood glucose, he would have persuaded me to eat a high-carb Kitavan-style diet. However, I am not persuaded.
I believe that:
- Optimal blood glucose levels are in the 90 to 100 mg/dl range. High-carb diets cause below-optimal levels of blood glucose, especially during fasts. (Indeed, high-carb dieters routinely experience hunger and irritability during long fasts.) Very low-carb diets cause elevated blood glucose due to the body’s efforts to conserve glucose by suppressing utilization. Excessive suppression of glucose utilization is unhealthy.
- A 20% carb diet, while not optimal for every single person, is healthy for nearly everyone. Twenty percent may be the best single prediction of the optimal carb intake for the population as a whole. Even diabetics can do well eating 20% carbs.
And that is why we recommend moderate consumption of safe starches.












Wow. Well done!
Thank you for a great article, Paul.
If Ron Rosedale wants to take away my safe starches, he’s going to have to pry them out of my cold, dead hands — which, based on your discussion of the two diets’ effects on the thyroid, may well be warmer than his live ones. 😉
It’s interesting to contrast the views of Rosedale and Ray Peat on the question of whether high or low metabolism is best for longevity. If I recall correctly, Peat thinks that high metabolism, not low, promotes longevity.
Sincerely,
Vincent
Paul:
Any sense of where small LDL particle levels are at 400 starch calories? For me CAD is an issue and carbs affect small LDL expression for me and perhaps for others.
I think a natural lowish carb diet is best and depending upon one’s genetics they need to find out what carb level best works for them to minimize negative gene expression. One size, PHD, or Rosedale does not fit everyone.
Also, i think that perhaps when we are young with better working machinery, carb tolerance is better and can be higher; as one ages it needs to be reduced and i do not think any studies differentiate for the aging human animal. Perhaps when one gets to be late 50’s, early 60’s starch per PHD minimum level of 200 calories per day may be more in order than 400 calories since most in that age group have been on the SAD diet for a long time.
Nice presentation, and keep thinking!
A great and well argued post. Thanks
Great post Paul.
Consumption of a certain (but not high) amount of carbs is more likely to have been the norm during our evolutionary past than no or extremely low carb. The relevance of the evolutionary of view is demonstrated by the results in the studies you cite.
Take care
Miki
My brother recently got a 100 mg/dl on his test. It was flagged as too high and out of range. Now it makes sense if high carb data is the goal by his doctor. He still needs to transition more to PHD, but I’m working on him. 🙂
Thanks for so much work on these too high and now too low starches articles of late Paul. You should just print and bind your articles and sell as another book!
As South Park’s Mr. Mackay would probably say here, “Extremes are bad…mmkay.”
Paul,
Awesome post, thanks for taking the time to respond in detail.
I think it’s an interesting question whether there is a tradeoff between longevity and feeling your best at any one point. Perhaps life is like a battle where you have only limited resources to fight against the forces of aging and infection. If so, then there is some logic in dialing down the thyroid and body temp to conserve resources and extend the length of the battle.
However, there may be times in the battle where you need to step up and fight hard with everything you have to prevent an immediate loss or permanent damage. I think that many people in the heat of battle do not have the luxury to put the thyroid on low and hope for the best in the long run.
Now many people live longer and are sicker. That is why medical industry is so strong. Yet there are some really long living people that are generally free of modern diseases. What is their diet? LC?
Thanks Paul,
A really useful post. Much apreciated
You had me at glucose flux. As a EE who specialized in electromagnetics, it took me a hell of a long time to wrap my head around fluxes and gradients. That graph is definitely worth a thousand words.
Anyway, a very cogent response.
“Optimal blood glucose levels are in the 90 to 100 mg/dl range”…so basically im fked?
my fasting bs today > 57 mg/dl ( 10 hrs after eating, usually im 60 -70 mg/dl) i feel great btw, pure energy, never hungry, never tired… this doing one meal per day (it includes some carbs like 1L whole milk, lots of chocolate, lots of red meat, yolks, cheeses, and taste…)
body comp, ( barely any training at all)
http://img15.imagevenue.com/img.php?image=183410777_P1010010_122_496lo.jpg
meh, i think need to start moving my arse a bit again, in def loosing some muscle mass 🙁
(lol care not)
Thank you very much, Paul, for participating in this discussion. However, there are so many incomplete and/or false interpretations and conclusions drawn, that it will take me more time than I have right now to point them out. As soon as I can find the time, I will be happy to explain them. This will be too long for a simple comment, so can it be a post on your blog?
Hi Ron,
Yes, you’re more than welcome to do a guest post on the blog.
Best, Paul
Paul,
when you got into that starch debate I feared you would be pulled into the “arguing on the internet”-type of responses. Instead you managed to give two bright examples of reasoned discourse that respects the other parties, curiously explores the arguments in opposition of your view, very clearly spells out your reasoning and is helpful to the general public, all at the same time.
Thanks for the amazing work! I’m especially looking forward to the next version of your book.
Another Tour de Force. Well done.
I agree with Jaybird on publishing. My idea would be to compose a PHD annual including recipes. Can I help publish it? As far as both arguments are concerned, I believe both have merit. I tend to side with Peat regarding his thoughts on high metabolism and body temperature. It would seem to be that bolstering your immunity with an uninviting body temperature is the better option given that most western disease may have roots in microbial insult. Also, I believe most of Rosedale’s ill effects from glucose can easily be mitigated by a Sisson-style approach to exercise. Rosedale’s approach would not allow one to thrive, it seems “monkish”. I for one do not want to live an ascetic lifestyle. It is better, as with many things, to qualify longevity than to quantify it, as many do not get the choice if you get my drift.
Great post. I will leave the science to the scientists but I thought I would raise one “smell test” level observation from the perspective of an educated (at the risk of flattering myself) layperson.
We evolved from apes. Apes ate fruit and tubers in abundance. As we evolved away from that, was it either evolutionarily advantageous or necessary that we lose our ape-ancestor ability to handle starch / glucose? Until the Ice Age, I find it hard to believe that it was either. And even with the Ice Age, was there enough time to develop / evolve a metabolism that treated glucose entirely as a toxin? Also, even with the Ice Age, if starch became unavailable would we necessarily have continued to evolve to treat it as a toxin in all circumstances? My “smell test” gut instinct is that the answer to all of these questions is “No”.
Further, from an observational perspective, when we look at pre-modern-civilization Pacific Islanders / Hawaians who ate high starch diets, we see lean, healthy and (largely) disease-free people. Were these people actually poisoning themselves on cassava, and were they all potential Methuselahs who would have been even healthier and long-lived had they just stuck to protein and fat? Again, my gut instinct says “no”.
I realize that I am offering conjecture and broad deductions, not science. But I thought it might be worth throwing out there just for a bigger picture perspective.
Hi Paul,
This is a very fascinating topic. In my own experience, I use to consume a whole foods grain heavy low-fat USDA diet and my fasting blood glucose was 82.
In the past year being on the PHD diet, my fasting blood glucose went up to 94. I consumed far less carbs and my blood glucose increased. I also found it interesting that my HBa1c was 5.7. My doctor was concerned that the HBa1c was on the high side of normal.
Can we expect more glycation of hemoglobin on a low carb diet given that fasting blood glucose levels are higher?
I also recall during the summer getting cramps in my calves and triceps when I didn’t consume enough carbohydrates. It was very easy to under consume carbs when you cut out grains and legumes. The cramping went away when I added in sweet potatos, rice and yams. Now, I make an effort to get more carbs in my diet. I also noticed that my body odor would be stronger on days that I consumed less than 100 calories of carbs. For me, I have found that very low carbing doesn’t work well and there are side effects.
Hope all is well.
Erik
Great response Paul!
You still make the most sense (in scientific and real life experience terms) in paleo-land.
Albeit, I’m also partial to Peat in regards to protein percentage and metabolism.
Anyways, Rosedales reasoning to seperate optimal diets for fertility and longevity is flawed too. I think we discussed this here before that for humans (and even other big apes) grandparenting is a very successful strategy for survival of the genus. Besides fathering a child in old age, let’s say up to a man’s 80-90ies is not unheared of! So, for a man at least it seems fertility and longevity go hand in hand.
For women it might be interesting to know if age of menopause is diet/blood sugar dependant, I have no info about that.
Btw, do you remember I told you in summer my hunger for starch was on the decline and I was craving more fruits? Now with falling leaves and temperatures that reversed and it’s back to enjoying potatoes and rice – not much fruit on my mind(except my obligatory banana).
The low body temperature is immunosuppressive probably a good idea for those with over-active immune systems – eg auto-immune diseases.
At low body temperatures (as well as very high) enzymes don’t work as well.
I’m glad to have starches back in my diet.
Thank you, Paul, for taking so much time to discuss those arguments and make your stance clear! You have intensively discussed macro-nutrient-ratios as to how they affect health and have done an excellent job in doing so! I am also interested in if there is really a metabolic advantage in low/moderate carb intake when compared to high carb intake. Most low carbers believe in that lowering carb intake helps to lose fat independend (to some degree) of total energy intake. A different opinion is that carb intake speeds up metabolism for it takes energy processing them. It would be great if you sometime adressed this issue (macronutrient intake and how it affects weight/metabolism)!
Hi Paul,
Awesome work. I hope I can buy another of your books to help reward you one day! 🙂
Meanwhile, one minor quibble – I have heard several people propose over the years evolutionary theories for Grandparents and their role in our species success. As social animals the theory goes, even past reproductive age, grandparents help the society (childcare, knowledge, work, etc) this conveys an advantage to those still of reproductive age. Hence, by having genes for longevity (and other good grandparent traits) in a family, your family gets extra support through life – and therefore more successful genes. This has always seemed plausible to me!
A discussion of it was featured in Scientific American recently, but it pops up from time-to-time.
http://www.dailymail.co.uk/sciencetech/article-2018191/Granny-power-Why-grandparents-ensured-human-survival.html
http://www.guardian.co.uk/science/2011/jul/24/prehistoric-man-helped-as-elderly-survived
More discussion of such theories:
http://en.wikipedia.org/wiki/Patriarch_hypothesis
http://en.wikipedia.org/wiki/Grandmother_hypothesis
So don’t discount the fact that evolution has helped set us up just fine already for long life 🙂
–Q
Thanks for this Paul – very helpful. I have noticed my temperature has increased since starting PHD – I used to be always cold and being warmer feels much, much better – being constantly cold is a miserable way to live.
Great post! Thank you Paul. I am learning so much just from reading your posts and comments in this blog. In my experience, VLC didn’t work too well for me . . . back in March of this year I tried VLC to shed some some fat off after a fertility treatment and after 5 weeks of 10% carb diet, I had UTI and the DR told me it’s because I wasn’t eating enough carbs. Though I was losing weight (lost 1 lb every week with VLC plus cardio/weight training 4x/week so lost a total of 5 lbs in 5 weeks), I immediately stopped doing VLC diet. (btw, I adopted Tom Venuto’s principles on losing the fat and took his sample menu as a base when I did VLC). Well, during the summer months I did put that 5 lb weight back on, I still continued to read health/nutrition books trying to figure out the best way I could lose the fat without going on VLC. 5 weeks ago I found PHD website and ordered the book. I am now on my 4th week of PHD and doing pretty well eating 20% carbs. I also am taking the supplements Paul had recommended after I emailed him to ask what I can add to the one I was taking. One of the things I immediately noticed after doing PHD is that it improved the quality of my sleep (used to keep waking up several times at night and that is now a thing of the past because I now sleep uninterrupted for 7-8 hours); and no more cramps in my calves (that used to happen occasionally after a heavy work out); no more menstrual cramps as well. Also, today is the first time i had my monthly period that i didn’t get a pimple in my face. I usually get a big, really deep and hard to get rid of pimple just before or during my monthly period and my husband or a dermatologist would actually help me get it out especially if I had an important function to attend to. I was thinking that may be IF and the removal of wheat in my diet did greatly help me in seeing immediate improvement in my sleep. So yes at least in my experience, a great improvement in my over all health since I incorporated the principles that I learned from the PHD book. And btw, I have a very sensitive skin (Atopic skin type or atopic/atopy syndrome – a hereditary component, as my doctor calls it because my mo and grandma had it too) and I usually get itchy and/or red spots in my skin all the time but in the last 4 weeks the anti-itching cream which I carry everywhere has never been used even once. And to top it all off, I lost 3 lbs in the last 4 weeks (losing the 15 lb excess weight is not even on top of my list because I am trying to get pregnant). I don’t have any health problems and hardly get sick. I simply want to eat healthy and trying to figure out what diet works best for me. And I found it! Thanks to PHD. Thanks to the Jaminets! At 42, 5’6″ height, 125 lbs weight, and doing PHD on 20% carbs, I feel great! And yes, I am sticking with PHD for the rest of my life. Btw, I plan on adding more carbs next week may be at 30% as i’d like to experiment how my body would respond to a higher carb intake.
when it comes to temp. I side with Dr.Peat. The closer to 98 I get the better I am Feeling. I know a man with severe typeII, his basal temp is 95.5, enough said.
For us amateurs who fall for simplistic reasonings especially in the diet world, the kitavans have been used in the blood glucose debate alot. As you mention, the Kitavans have low blood glucose and since kitavans equal healthy then so it goes one should eat high carb. How would you respond Paul since they seem to defy the U shape curve and the other studies you discussed?
Hi Vincent,
Ray Peat is certainly in favor of high metabolism, but I don’t recall his writing on longevity. Would be interested in his thoughts.
Hi steve,
I don’t have any clinical experience like Dr Davis, and I’m not aware of studies showing the relationship of sdLDL levels to carb intake on low-carb diets. I also don’t know that it’s guaranteed that zero sdLDL is optimal. It might be good to have a distribution of LDL particle sizes. So I would be more inclined to say that whatever sdLDL distribution you get with 400 starch calories is optimal, than to say that we can infer optimal carb intake from sdLDL data.
There are definitely changes in glucose handling with age; older people are less able to handle extreme diets. Whether that changes the optimal diet is another question.
Hi Jay,
Shou-Ching also supports the idea of a “best of the blog” collection … we’ll see.
Hi Todd,
Great point, we might want to manipulate the thyroid to deal with circumstances like infections. However, that’s a level of sophistication that will take some time to develop.
Hi Stan,
I’ve written about that in the book and in a few posts: http://perfecthealthdiet.com/?cat=52
Hi lolo,
You look great and feel great, so I’d guess you’re healthy!
Protein is somewhat metabolically similar to carbs, it stimulates an insulin response for instance, so perhaps high protein intake explains your low blood glucose. Or you may be taking ketogenic oils like coconut oil, or ketogenic amino acids like BCAAs. Ketones will lower blood glucose.
Hi Gabriel,
A PHD annual sounds like a great idea.
Hi Remnant,
I agree.
Hi Erik,
Thanks for sharing your experience – another data point in low-carb raises blood glucose.
HbA1c of 5.0 to 5.4 is probably optimal in the general population, but optimal might be higher in low-carb dieters. Mine was measured only once, a year and a half ago, and was 5.4. But there is noise in this number, it depends on red blood cell turnover too, which does vary among persons. Stephan Guyenet’s was 5.8, if I recall correctly. I wouldn’t worry about 5.7.
Cramps are a common problem on vlc, and eating more carbs usually fixes it. I haven’t seen any papers that give clues to the mechanism.
Hi Franco,
Thanks!
Very interesting the summertime fructose desire and winter starch desire. Sort of a Ray Peat to PHD seasonal transition?
Hi Sue,
Interesting idea about autoimmune disorders. Though I’m not sure suppressing immunity is really a good idea in those diseases.
I like being warm too!
Hi Iris,
As far as “metabolic advantage” I’m going to be getting into closely related topics shortly as I develop a theory of obesity. I think in general macronutrients that have a metabolic advantage tend to be obesity-promoting.
However, I think it’s the disposal pathways that have the metabolic advantage, so carbs don’t really become obesity promoting until you get above the intersection point in my diagram.
Hi Quarrel,
Thanks for the links! Yes, there’s a lot of evidence for the grandparent hypothesis. I think as cultural transmission of knowledge became important, longevity became an advantage as well.
Hi Agatha,
Wonderful!
Hi Els,
That’s great! Let me know how your 30% carb experiment goes. The extra carbs may help you get pregnant, so I think it’s a good idea.
Hi Kevin,
I agree, body temperature should be normal. There’s a reason evolution chose that temperature, and everything should work its best around that point.
Hi Jay,
The Kitavans are healthy, but perhaps not optimally healthy. They have a high rate of malaria for instance.
Since I consider the Kitavan diet extremely healthy — just like ours only with more starch — I’m not surprised they’re healthy by international standards. Their diet is far healthier than the American diet.
Carb intake is not the only factor that determines health. So I wouldn’t say there’s any reason to think they defy the U.
Best, Paul
I think one aspect not given enough importance in this argument is activity level. Most of what is being discussed applies to sedentary samples. The Kitavans may enjoy greater health due to their lifestyle with diet being 1 mere aspect of it. CHOs are not nearly as harmful when you are moving frequently and doing manual work/play that requires strength and stamina. Your thoughts?
It’s true … but I don’t think their diet would be harmful to a sedentary person either, if he was in good health to start with.
Activity helps, strength helps, sun exposure helps, many aspects of the Paleo lifestyle help.
im confused…
_high protein intake explains your low blood glucose_
why? > high insulin? > gluconeogenesis? MAYBE is the timing of my daily sucrose @ milk breakfast + fasting combo?…. i mean _ it should_ go straight to my _depleted_ liver and muscles.
(if i workout… ) also the fructose is less insulogenic…. high protein releases both insulin and glucagon , and thought the pancreas stops secreting insulin when glucose levels drop below 83 mg/dL ? so my insulin levels should be… low?
_ you may be taking ketogenic oils like coconut oil or ketogenic amino acids like BCAAs. Ketones will lower blood glucose_
i take no pills and no BCAAs ( lots of animos in my 7 yolks) also 0% oil or any kind of coconut concoction , just regular butter ( and cacao butter…)
thanks!
Hi lolo,
Yes, your fasting insulin should be low. (Although elevated fasting insulin would explain your low fasting glucose.) The question is whether postprandial insulin contributes to a low fasting glucose.
Looks like ketogenic foods aren’t the answer. Alright, I don’t know why your blood glucose is low!
In answering what you believe is the glucose level best for health, it seems that you are really referring to what fasting glucose level you believe is best for health. Is this correct? I want to make sure I am understanding correctly what you have written above.
If I’ve understood you correctly, and fasting glucose in your view is optimal at 100ish, then wouldn’t postprandial blood sugar necessarily become higher than if fasting glucose was lower? Since A1C test may be impacted by blood cell size or anemia etc, do you think post-prandial testing should be done routinely on your plan to see if the postprandial glucose rises higher than the 140 threshhold? While some seem to feel better adding what you deem safe starch to their previously vlc diets, there have been postings where ldl and/or triglycerides have increased. Not sure what to make of this.
Anyway, thank you again for your posts and I’m looking forward to hearing Dr. Rosedale’s response. You are both real gentlemen and nice to read passionate debates that are civil and so informative.
Paul wrote: “Interesting idea about autoimmune disorders. Though I’m not sure suppressing immunity is really a good idea in those diseases.” I with you there, Paul. Further, I’m convinced that lumping all these quite varied diseases into one category — “autoimmune” — creates a huge barrier to further understanding of any of them.
Wish I could find it again. Somewhere, I read that the Kitavan study is flawed, and probably shouldn’t be taken as seriously as it often is.
Paul, could I have a refresher on what happens to blood glucose when you have an infection — does it typically drop? Maybe that is why paradoxically some lower carb adherents have lower than usual blood glucose than the typical range (for low carbers).
Hi Alexandra,
There are many measures of blood glucose – these papers used fasting and 2-hr after OGTT, but peak after OGTT and AUC after OGTT are also used.
Personally I don’t think blood glucose level is a very sensitive indicator of health. However, in most people I think 90-100 mg/dl is healthy.
Yes, postprandial blood sugar is generally higher than fasting.
I don’t think blood glucose testing is necessary except in diabetics or those who have hypoglycemic / glycemic dysregulation symptoms and are testing for diagnostic purposes. I did get a blood glucose meter for curiosity purposes, but pricking fingers gets old and I haven’t tested myself in quite a long time.
However, if you’re concerned about the safety of safe starches, I think it would be educational to get a meter and track your own adaptation to different diets.
Hi Marilyn,
Agreed. If you run across the Kitavan study critique, let me know.
Hi Aaron,
That would be a good topic for a blog post (or series). It’s a rather complex issue.
Hi Paul,
I see you recommend a general guideline of 20% (not too runaway with this idea) but I am a petite female who is sedentary at the moment due to some health problems and I have been eating around your recommended 100g of starch a day. Total carbs from veggies gets me between 120-140. Anyways, calories come to about 1100-1300 on a typical day. Breakdown looks more like 35%CHO 25%pro and 40%fat (duck at the moment). This seems to contradict the 20% guideline. How can 100g of starch be the same level for me a 112lb inactive female as to you? Don’t feel hungry, I literally use two plates to fit all the veggies I eat per meal (squash, white potato, rutabagga, water chestnuts).
Hi AC,
It’s more a calories guideline, then a % energy guideline, so you’re doing great. I think your current intake is perfect.
Thanks Paul. Sorry if I wasn’t clear. I understand postprandials are generally higher than fasting but what I meant to ask was wouldn’t a person starting with a higher pre-breakfast glucose level –say 100 — necessarily mean a higher post prandial than that that same person would get eating the very same breakfast if his or her starting glucose was 80? Anyway, I guess a little diagnostic testing would be the only way to find out as results would be highly individual in terms of how high a spike occurs and how long it takes to return back to the safe zone. I think people should test beyond 2 hours though because depending upon my meal composition, my peak can come at hour 3. This is especially true after a large meal or one that has lots of fiber or slower digesting foods like nuts. Since you are not diabetic and feel great, but haven’t tested in a long time, it might be interesting to see what if any chances have occurred in your tolerance to the safe starches over time. Glucose aside, beneficial changes or not with respect to HDL, LDL and Triglycerides might be interesting as well. Anyway, thank you again for the terrific blog and your book which I’ve recommended even to happy vlcers like myself because there is tons of useful info in it suitable for everyone.
Hi Paul,
I came to believe that it doesn’t matter that much (for me at least) where your carbs come from (fruits or safe starch) in the context of IF. Even macro percentage doesn’t seem to matter much (if protein is sufficient) when you eat “once per day” in a 4 h window. I think I read somewhere that also the Kitava-diet must be seen in the context of 1-2 meals per day.
If you’re snacking on fruit through all the day on top of 3 meals (like many “health conscious” folks do) the effects are very different.
Paul: The PHD has helped me in several important respects, but it has not yet fixed my awful memory. 🙂 Hopefully you or others will correct me if I am incorrectly attributing ideas to Ray Peat.
I vaguely recall an interview in which Peat criticized animal studies purporting to show that calorie restriction — and, by extension, low metabolism — promotes longevity. I think Peat said something to the effect that in the calorie restriction studies he had seen, researchers underfed animals from birth, creating undersized runts with above-average ratios of metabolic rate to size, who then outlived their larger peers. (I believe that elsewhere, he has also attributed the longevity of the underfed animals in some calorie restriction studies to lower loads of food toxins.) He did not believe one could infer from such studies that reducing metabolism in adulthood would promote longevity, and indeed, he expected the opposite.
My apologies if I am misstating Ray Peat’s views.
Sincerely,
Vincent
PS: The following article by Peat suggests one possible relationship between metabolic rate and longevity:
http://raypeat.com/articles/articles/co2.shtml
This article includes a more direct statement of Peat’s views on the relationship between metabolism and longevity:
http://raypeat.com/articles/articles/salt.shtml
Sincerely,
Vincent
I would also like to ask, like one of the commentors above, about recommendations for females. As I weight less than the average male and are interested in maintaining my weight I find this much more difficult when making sure to make room for 400 kcal from starches. When eating only veggies, meat, fish, eggs etc, even with plenty added fat, I found it impossible to eat too many calories. Now I find myself limiting my fat intake considerably because carbs + added fats easily leads to too many calories. But carbs without fat (rice, potatoes) are not at all appealing so I end up forcing them down…Maybe you could consider giving some recommendations to people who better not consume 2000 kcal or more per day (at least on non-exercise days) and still would like to keep their meals attractive?
Here Rosendal shows us a very big problem with LC fanatics : they are glucose-centric. Rosendal says that any BG level is toxic and hence we should be avoiding glucose. What he seems to forget or maybe not be aware of? is that ALL macros are ”toxic” in the post-prandial phase, causing inflammation and some damage to varying degree, and that’s one of the things that calorie restriction is based on; it’s based on the fact that food is ”slowly killing us” and that we should reduce it. It’s also aiming to reduce anabolism into the body. We should remember that there are also lipoxidation-end products, just as there is glycation end products and that neither are a good things.
Carbs restriction has never been shown to be longevity-productive. Calorie restriction is the only way so far that seems to work. If you have calorie restriction but don’t have carbs restriction, you’ll be perfectly fine, just look at the Okinawan which diet was vastly based on potatoes.
Why would fat and protein be free of any accusations? Why would only glucose be the ”ennemy”? It seems rather strange knowing what we know regarding lipoxidation end product and amino acids signaling on mTOR and others aging pathways.
Regarding caloric restriction, I once had a short correspondence with Dr Speakman, a well-known caloric restriction researcher at Aberdeen university and one of the authors of this and this.
I was asking if there was any way to measure the overall well-being of calorically restricted rats, as one of the main considerations when extending lifespan is whether it is possible to extend the quality of life as well, or if the result instead would only be a “thin” extension of existence “like too little butter scraped on too much bread” (Bilbo in Lord of the Rings).
I also asked if there were lessons to be drawn from the Ancel Keys starvation studies, which showed that caloric restriction in humans led to constant hunger, cold, lack of energy or libido, and total fixation on food and other mental and physical health derangements.
This was his fascinating (and faultlessly generous to an unsolicited query) reply:
His last point is in reference to his own finding that lab rats who commence caloric restriction in adulthood gain only small increments in lifespan.
@Scotlyn
Yes, it’s not really yet clear how many years CR would add to one lifespan. Your Dr Speakman makes good point about malnourishment and the caloric restriction being too extreme. That’s why people speaks about CRON – calorie restriction with optimal nutrition. And also people doing it are trying to do a minimal restriction, usually around 10-15% restricted. Imminst has a forum with many active CRONies, and they seems to enjoy the process.
I would personnally never do it has, again, it’s not even sure that in the end it makes that much of a big difference. I know some people are using it in the hope of gaining a few years to be able to use upcoming anti-aging medicine.
My main point was that if we were to use Rosendal logic regarding glucose, we should apply it to all macros (since they all have their own problems) and well… stop eating? It does not makes much sens. Eating is indeed paradoxal as it is needed to survive, but it’s also participating in our aging process and that’s not just glucose per se. Not a very strong argument against glucose IMO.
Hi Iris,
I would probably suggest intermittent fasting, and during the fast taking a bit of MCT oil (following the Seth Roberts “tasteless calories” strategy, and using ketosis to suppress hunger during the fast). Then following our regular diet during the 6-8 hour daily feeding window. Hopefully the MCT oil and intermittent fasting strategy will fix the food craving issue.
@ Frank;
I think you’re right that the metabolic processes of using oxygen to convert all the different components of food into energy may cause an accumulation of detriments which ultimately leads to illness and death. To focus on one of these may be short-sighted, and also obsessive, which has its own problems.
The prospect of death, however, does not worry me at all. I’m perfectly happy to take my turn at being food for whatever microbes take an interest when the time comes. All healthy ecosystems depend on a cycle of birth, eating, death and decay.
In relation to illness, however, I would like to enjoy what life I have in good health, with energy, warmth and good humour to boot, and I like Paul’s approach of trying to find the optimum level of all nutrients. The optimum level, which is carefully poised between observed increasing detriments for the whole organism at either extreme, must include qualitative measures not only quantitative ones.
Vincent, good Ray Peat link http://raypeat.com/articles/articles/salt.shtml, thanks.
Covers a lot different items/areas that i have been interested in of late…..eg. sodium (salt), body temp, thyroid, estrogen, GABA, aldosterone, cortisol, inflammation…to name a few
I love people who realize the power of graphs. Without even reading the whole article I can vouch that this is goodie!
work appreciated!