Jimmy Moore is graciously continuing the conversation about safe starches with a post from Dr Ron Rosedale. For those trying to keep track, here’s how the discussion has gone:
- Jimmy’s original seminar on safe starches, featuring Paleo and low-carb luminaries.
- My main reply appeared both here and at Jimmy’s. I also wrote further on how to minimize hyperglycemic toxicity, and offered an appreciation of Dr Kurt Harris.
- Now, Dr Ron Rosedale has replied to my reply.
Today, I’ll reply to Dr Rosedale.
Dr Rosedale argues that glucose is toxic, so we should want to have less of it in our bodies; and that low-carb diets deliver less of it. He cites a lot of papers on the relationship between blood glucose levels and health, and uses blood glucose levels as a proxy for the level of glucose in the body.
Two basic matters are at issue: (1) What blood glucose level is best for health? (2) Which diet will generate those optimal blood glucose levels?
Let’s look at what the evidence shows.
What Blood Glucose Level is Best for Health?
In my main reply, I had written:
What is a dangerous level of blood glucose?
In diabetics, there seems to be no detectable health risk from glucose levels up to 140 mg/dl, but higher levels have risks. Neurons seem to be the most sensitive cells to high glucose levels, and the severity of neuropathy in diabetes is correlated with how high blood glucose rises above 140 mg/dl in response to a glucose tolerance test. [1] In people not diagnosed with diabetes, there is also some evidence for risks above 140 mg/dl. [2]
Dr Rosedale seemed to feel that this was the weakest point in my argument, and directed his fire here. My statement was a description of what the scientific literature shows, and the adjective “detectable” carries a lot of weight here. To refute my statement, you would have to find study subjects whose blood glucose never goes above 140 mg/dl, and yet show health impairments attributable to glucose.
Dr Rosedale argues there is no threshold separating safe from harmful levels of glucose, because glucose acts as a toxin at all concentrations:
I will spend a fair amount of time and show a fair number of studies to show that there is no threshold. Very simply, the higher the blood sugar rise, the more damage is done in some linear upward slope.
I emailed Ron to make sure that he really did mean there was no threshold, so that glycemic toxicity begins at 0 mg/dl. He replied:
I mean the former; that glucose will cause some damage when above 0 mg/dl … obviously a moot point and theoretical when glucose very low and incompatible with life and likely a minute amount of damage when that low. At any level of glucose compatible with life some more meaningful degree of glycation, hormonal response and genetic expression will take place. We will always want/need to repair the damage done to stay alive, but with age the repair mechanisms become damaged also. Eventually damage outdoes repair and we “age”, acquire chronic disease, and die.
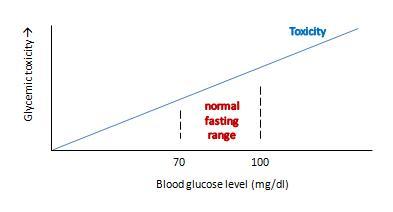
Ron’s view can be graphed like this:
This view makes sense as a matter of molecular chemistry: the number of glycation reactions may be proportional to the concentration of glucose, and if glycation products are health damaging toxins then toxicity may be proportional to glucose levels.
The trouble with this is that it doesn’t really get at what we want to know: what blood glucose level optimizes human health?
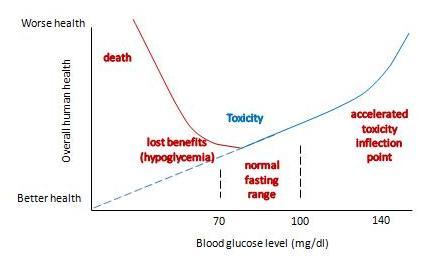
If we change the y-axis so that it doesn’t measure glycemic toxicity, but rather overall health of the human organism, then the shape of the curve is going to change in two major ways:
- First, in translating toxicity to its impact on health, we have to account for Paracelsus’s rule: “the dose makes the poison.” The body can readily repair small doses of a toxin with no ill effect – possibly even a hormetic benefit – but large doses of a toxin multiply damage exponentially and can prove fatal. So the impact of a toxin on health will not rise linearly, but non-linearly with a steeper slope as one moves to the right.
- Second, we have to account for the fact that glucose has a role as a nutrient. As Ron himself says, having too little blood glucose is “incompatible with life.” So low blood glucose – depriving us of the benefits of normal levels of this nutrient – is a catastrophic negative for health. This means that the left side of the curve needs radical adjustment.
With these two changes, our graph becomes something like this:
It now has a U-shape. I’ve drawn the inflection point where toxicity starts rising rapidly at around 140 mg/dl, and the inflection point on the other side where hypoglycemia causes substantial health damage at around 60 mg/dl. But the precise numbers don’t matter much; the point is that there is a U-shape, and somewhere in that U is a bottom where health is optimized.
What do we know about the precise shape of that U, and the location of the bottom?
We can’t intuit the shape of the bottom of the U using theoretical speculations. Theory doesn’t allow us to balance risks of hypoglycemia against toxicity on such a fine scale. The bottom of the U could be very flat, and it might not matter much whether blood glucose levels are 80 or 100 mg/dl. Or the bottom of the U could be tilted, so that the optimum is either at the low end, near 80 mg/dl, or the high end, near 100 mg/dl.
Empirical evidence is limited. Most studies relating blood glucose levels to health have been done on diabetics eating high-carb diets. There are few studies on healthy people, very few testing low-carb diets, and most are insufficiently powered to determine the precise shape of the bottom of the U.
Dr. Rosedale cites a good selection of studies in his response, and let’s review a representative subset. I was familiar with most of the studies; indeed some were cited in our book’s discussion of the dangers of hyperglycemia.
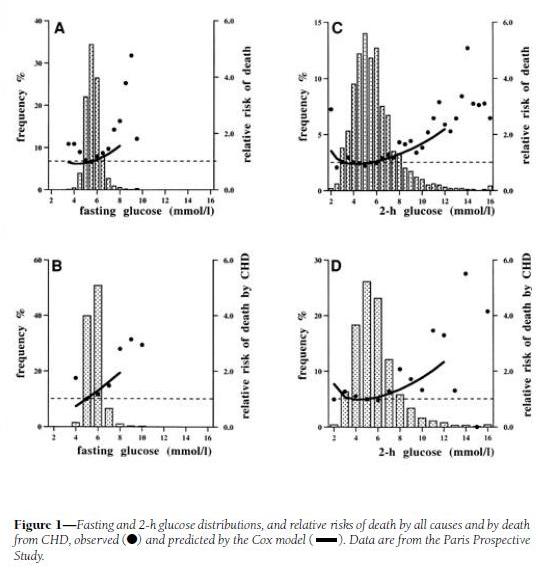
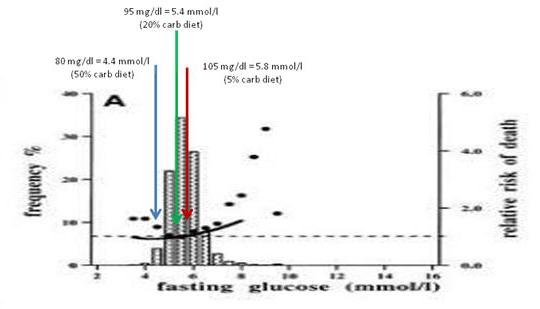
His first cite is “Is there a glycemic threshold for mortality risk?” from Diabetes Care, May 1999, http://pmid.us/10332668. Here is their data:
Look at the black dots, which are the actual data, not the fitted curves which are model-dependent; and at panels A and C, which treat all-cause mortality, not B and D, which are specific for coronary heart disease.
For both fasting and 2-h postprandial blood glucose, the black dots are lowest between about 4.5 and 6.0 mmol/l, which translates to 81 to 108 mg/dl. However, note that there is very little rise in mortality – only about 10% higher relative risk – in 2-h glucose levels of 7 mmol/l, which is 126 mg/dl. Since the postprandial peak is rarely at 2-h (45 min is a common peak), most of these people may well have been experiencing peak levels above 140 mg/dl.
My interpretation: I would say that this study demonstrates that mortality is a U-shaped function of blood glucose levels, but it doesn’t tell us the shape of the bottom of the U. It is consistent with the idea that significant health impairment occurs only with excursions of blood glucose above 140 mg/dl or below 60 mg/dl.
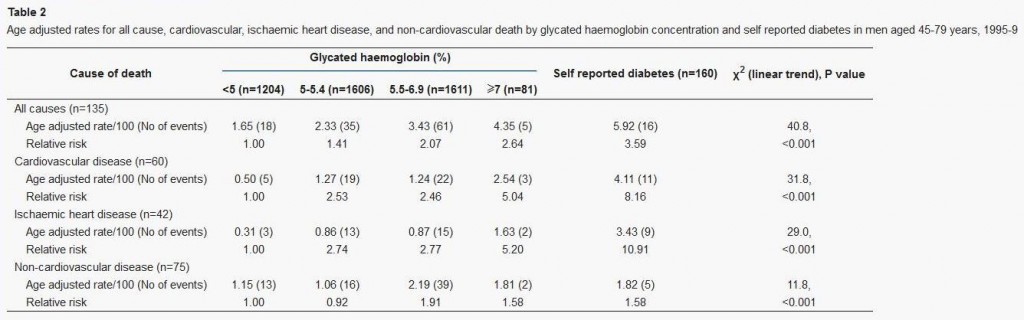
Dr Rosedale’s second cite is actually to a commentary: “‘Normal’ blood glucose and coronary risk” in the British Medical Journal, http://pmid.us/11141131, commenting on a paper by Khaw et al, “Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of european prospective investigation of cancer and nutrition (EPIC-Norfolk),” http://pmid.us/11141143.
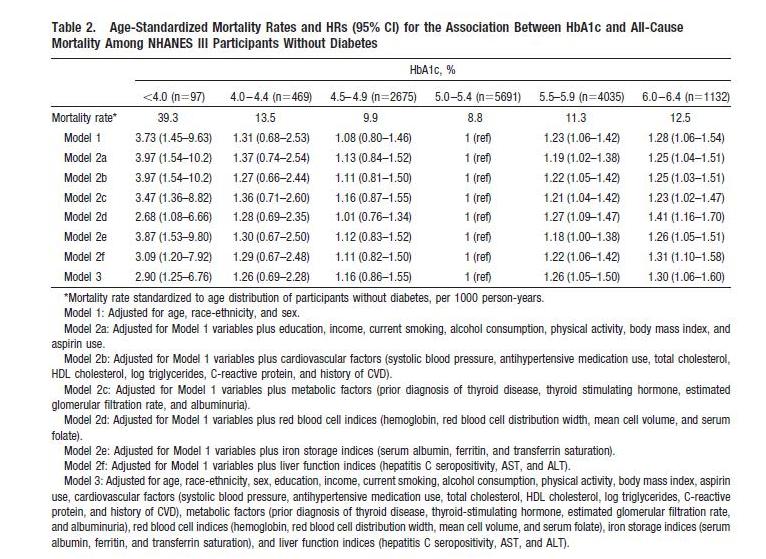
This study used glycated hemoglobin, HbA1c, which can serve as a measure of average blood glucose over the preceding ~3 weeks. Here is the data:
This supports the “blood sugar should be as low as possible” thesis, since lower HbA1c levels were associated with lower mortality. However, this study has a few flaws:
- It includes diabetics. Diabetics have poor glycemic control, and episodes of hypoglycemia as well as hyperglycemia, so HbA1c levels (which represent average blood sugar levels) may be a poor proxy for the levels of glycemic toxicity. Also, diabetics are usually on blood-glucose lowering medication, which may distort the blood sugar – mortality relationship.
- It lumps the population together in very large cohorts. Effectively there were only three cohorts, since the highest HbA1c cohort had only 2% of the sample; the other three cohorts contained 27%, 36%, and 36% of the study population respectively.
We can get a finer grip on what happens by looking at studies that lack these flaws. Here’s one: “Low hemoglobin A1c and risk of all-cause mortality among US adults without diabetes,” Circulation, 2010, http://pmid.us/20923991.
This study is an an analysis of NHANES III; it excludes diabetics and has 3 cohorts, not 1, with HbA1c below 5%. Here’s their data:
The U-shaped mortality curve is very clear. In raw data and all models, the lowest mortality is with HbA1c between 5.0 and 5.4. Mortality increases with every step down in HbA1c: in Model 1, mortality is 8% higher with HbA1c between 4.5 and 4.9, 31% higher between 4.0 and 4.4, and 273% higher below 4.0.
Via Ned Kock of Health Correlator comes a formula for translating HbA1c to average blood glucose levels:
Average blood glucose (mg/dl) = 28.7 × HbA1c – 46.7
Average blood glucose (mmol/l) = 1.59 × HbA1c – 2.59
So the minimum mortality HbA1c range of 5.0 to 5.4 translates to an average blood glucose level of 96.8 to 108.3 mg/dl (5.36 to 6.00 mmol/l).
This result is almost identical to the finding in Dr Rosedale’s first cite, from which Dr Rosedale quoted: “the lowest observed death rates were in the intervals centered on 5.5 mmol/l [99mg/dl] for fasting glucose.”
My interpretation: Once again, we find that there is a U-shaped mortality curve, and minimum mortality occurs with average or fasting blood glucose in the middle of the normal range – in the vicinity of 100 mg/dl or 5.5 mmol/l.
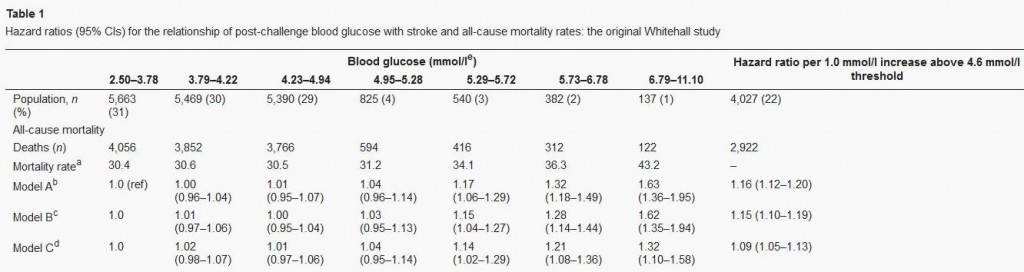
Let’s finish our examination of this issue with a quick look at Dr Rosedale’s third cite. That paper, “Post-challenge blood glucose concentration and stroke mortality rates in non-diabetic men in London: 38-year follow-up of the original Whitehall prospective cohort study,” Diabetologia, http://pmid.us/18438641, is a familiar one; it was cited in our book (p 36, fn 35).
This study looked at blood glucose levels 2 hours after swallowing 50 grams of glucose, and then followed the men for 38 years to observe mortality rates. CarbSane makes an important observation: this study used whole blood rather than plasma to assay blood glucose. Whole blood has more volume (due to inclusion of cells) but the same glucose, and so less glucose per deciliter. According to this paper, standard (plasma) values are about 25 mg/dl higher, so 95 mg/dl in whole blood actually corresponds to a plasma value of about 120 mg/dl.
Here is the data:
There is no significant difference in mortality among any group with post-challenge whole blood glucose up to 5.29 mmol/l (95 mg/dl), corresponding to 120 mg/dl or 6.7 mmol/l in standard measurements.
The study was designed to look at high blood glucose levels: there were 4 cohorts in the top 10% of blood glucose levels, but the bottom cohort in blood glucose had fully 31% of the sample. This cohort consisted of everyone with 2-hr whole blood glucose levels below 68 mg/dl, or plasma glucose below about 90 mg/dl. Mortality in this large group was indistinguishable from that in the next two groups, who had plasma glucose between 90 and 120 mg/dl.
My interpretation: This study wasn’t designed to observe the lower end of the U. At the higher end, it is consistent with the other studies: mortality rises with 2-hr plasma glucose above 120 mg/dl.
Summary: Optimal Blood Glucose Levels
All of the papers cited by Dr Rosedale are consistent with this story:
- Mortality and health have a U-shaped relationship with blood glucose.
- Optimum health occurs at blood glucose levels around 100 mg/dl – at normal levels, not exceptionally low levels.
- The impaired health seen with fasting or 2-hr blood glucose levels of 110 or 120 mg/dl may be largely attributable to the portion of the day in which those people experience blood glucose levels over 140 mg/dl.
I should note that Dr Rosedale acknowledges that high-normal blood glucose is better than low blood glucose for some aspects of health, like fertility:
Safe starch proponents say that raising blood glucose and raising insulin is a very natural phenomenon and needn’t be avoided. However, if we evolved in a certain way and with certain physiologic responses to the way we eat, it was not for a long, healthy, post-reproductive lifespan. It was for reproductive success. The two are not at all synonymous, in fact often antagonistic.
He’s saying that higher blood glucose favors “reproductive success,” while lower blood glucose favors “post-reproductive lifespan.” I guess one has to choose one’s priorities. Not everyone will choose maximum lifespan.
But suppose Dr Rosedale is right, and that low blood glucose levels are most desirable for at least some persons. I’m willing to stipulate, for the sake of argument, that optimal health for some persons may occur at below-normal blood glucose levels – say, 80 mg/dl. That brings us to the second issue: which diet will produce these low blood glucose levels?
Which Diet Minimizes Blood Glucose Levels?
If the key to health is achieving below-normal blood glucose levels, then low-carb diets are in trouble.
In general, very low-carb diets tend to raise fasting blood glucose and 2-hr glucose levels in response to an oral glucose tolerance test.
This is a well-known phenomenon in the low-carb community. When I ate a very low-carb diet, my fasting blood glucose was typically 104 mg/dl. Peter Dobromylskyj of Hyperlipid has reported the same effect: his fasting blood glucose is over 100 mg/dl. From one of Peter’s posts:
Back in mid summer 2007 there was this thread on the Bernstein forum. Mark, posting as iwilsmar, asked about his gradual yet progressively rising fasting blood glucose (FBG) level over a 10 year period of paleolithic LC eating. Always eating less than 30g carbohydrate per day. Initially on LC his blood glucose was 83mg/dl but it has crept up, year by year, until now his FBG is up to 115mg/dl….
I’ve been thinking about this for some time as my own FBG is usually five point something mmol/l whole blood. Converting my whole blood values to Mark’s USA plasma values, this works out at about 100-120mg/dl.
Peter notes that low-carb dieters will generally perform poorly on glucose tolerance tests, but that increasing carb intake to about 30% of calories is sufficient to produce a normal response to a glucose challenge:
The general opinion in LC circles is that you need 150g of carbohydrate per day for three days before an oral glucose tolerance test.
This is at the high end of the 20% to 30% of energy (400 to 600 calories on a 2000 calorie diet) that is the Perfect Health Diet recommendation for carbs.
The Kitavans eat more than 60% of calories as carbohydrate, mostly from starches. Their fasting blood glucose averages 3.7 mmol/l (67 mg/dl) (http://pmid.us/12817903).
Studies confirm that high-carb diets tend to lower fasting glucose and to lower the blood glucose response to a glucose challenge. CarbSane forwarded me some illustrative studies:
- “High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults,” http://pmid.us/2168124. Switching healthy adults to a higher carb diet reduced fasting blood glucose from 5.3 to 5.1 mmol/L (95.5 to 91.9 mg/dl) and reduced fasting insulin from 66 to 49.5 pmol/l.
- “Effect of high glucose and high sucrose diets on glucose tolerance of normal men,” http://pmid.us/4707966. On diets with glucose as the only carb source, 2-hr plasma glucose after a glucose challenge was 184 mg/dl on a 20% carb diet, 183 mg/dl on a 40% carb diet, 127 mg/dl on a 60% carb diet, and 116 mg/dl on an 80% carb diet. The 80% carb diet was the only one on which blood glucose never went above 140 mg/dl.
This last study did not report fasting glucose, but did track blood glucose for 4 hours after the glucose challenge. If we take the 4-hr blood glucose reading as representative of fasting glucose, we find that dieters eating 60% or 80% carb diets had fasting glucose of 76 and 68 mg/dl, respectively.
My interpretation of the evidence from multiple sources: A plausible conclusion is that a high-carb diet produces a low fasting glucose (let’s say, 80 mg/dl), a PHD type 20% carb diet an intermediate fasting glucose (95 mg/dl), and a very low-carb diet a high fasting glucose (say, 105 mg/dl).
Just for fun, I decided to see where these fasting glucose levels show up on the mortality plot from Balkau et al:
The 20% carb diet lines up pretty well with the mortality minimum, and both high-carb and very low-carb diets wind up at bins with slightly elevated mortality.
Now, I don’t believe we can infer from data on high-carb dieters what the relationship between blood glucose levels and mortality will be in low-carb dieters. It was Dr Rosedale, not me, who introduced this study into evidence.
But if we believe that lowest mortality really does occur with 2-hr post-challenge blood glucose around 100 mg/dl and fasting blood glucose below 100 mg/dl, as argued by the studies Dr Rosedale cited, and that this result applies to low-carb dieters, then I think the evidence is clear. One must eat some carbohydrates – at least 20-30% of energy.
This is the standard Perfect Health Diet recommendation. It seems that Dr Rosedale is supporting my diet, not his!
What About Diabetics?
Perhaps the boldest passage in Dr Rosedale’s reply was this:
We are all metabolically damaged to some extent. None of us has perfect insulin and leptin sensitivity…. It is for that reason that I say that we all have diabetes, some more than others, and should all be treated as such.
Well, if we all have diabetes, more or less, then I guess I have to consider whether our regular diet – which recommends about 20% of energy (400 calories) as carbs – is healthy for diabetics.
Now, before I begin this discussion, let me say that I don’t claim that this is optimal for diabetics. I think it is still an open question what the optimal diet for diabetics is, and different diabetics may experience a different optimum. I have often said that diabetics may benefit from going lower carb (and possibly higher protein) than our regular dietary recommendations. However, Dr Rosedale is here saying that even a healthy non-diabetic should eat a diet that is appropriate for diabetics. I want to see whether our regular diet meets that standard.
How do diabetics do on a 20% carb diet? Here’s some data that I found in a post by Stephan Guyenet at Whole Health Source. It’s from a 2004 study by Gannon & Nuttall (http://pmid.us/15331548) and the graph is from a later paper by Volek & Feinman (http://pmid.us/16288655/). Over a 24 hour period, blood glucose levels were tracked in Type II diabetics on their usual diets (blue and grey triangles) and after 5 weeks on a 55% carb – 15% protein – 30% fat (yellow circles) or 20% carb – 30% protein – 50% fat diet (blue circles):
The low-carb diet was a little higher in protein and lower in fat than we would recommend, but very close overall to our recommendations and spot-on in carbs.
What happened to blood glucose? It came close to non-diabetic levels. Fasting blood glucose dropped to 7 mmol/l (126 mg/dl), roughly the level at which diabetes is diagnosed. Postprandial blood glucose elevations were modest – peaking below 160 mg/dl which is about 20 mg/dl higher than in normal persons. Average daily blood glucose looks to be around 125 mg/dl.
What would have happened on a zero-carb diet? Fasting blood glucose probably would still have been elevated, near 126 mg/dl; this is common in diabetics because the loss of pancreatic beta cells creates a glucagon/insulin imbalance that leads to elevated fasting blood glucose. This blood glucose level would have been maintained throughout most of the day, with the postprandial peaks and troughs flattening. Average daily blood glucose level would have been similar to that on the 20% carb diet.
So the big benefit, in terms of glycemic control for diabetics, comes from reducing carbs from 55% to 20%. Further reductions in carb intake do not reduce average 24 hour blood glucose levels, but may reduce postprandial glucose spikes.
In fact, we have some Type II diabetics eating Perfect Health Diet style. Newell Wright reports good results:
I am a type II diabetic and a Perfect Health Diet follower, so I want to chime in with my experience….
I switched from the Atkins Induction diet to the Perfect Health Diet. I have been eating rice, potatoes, bananas, and other safe starches ever since, as well as fermented dairy products, such as plain, whole milk yogurt. I have also slowly lost another seven pounds. I enthusiastically recommend the book, Perfect Health Diet by Paul and Shou-Ching Jaminet.
Today, my fasting blood glucose reading was 105. Note that since following the Perfect Health Diet, my fasting blood glucose reading has gone down. Previously, I was suffering from the “dawn phenomenon.” My blood glucose levels overall were well below 140 one hour after a meal and 120 two hours after a meal. Only my fasting BG reading was out of whack, usually between 120 and 130, first thing in the morning.
For dinner tonight, I had a fatty pork rib, green beans, and a small baked potato with butter and sour cream. For dessert, I had a half cup of vanilla ice cream. One hour after eating, my blood glucose level was 128 and two hours after, it was 112.
So not only am I losing weight on the Perfect Health Diet, my blood glucose levels have actually improved, thanks to the increased carbs counteracting the dawn phenomenon, just as Dr. Kurt Harris (another proponent of safe starches) said it would.
So for me, as a type II diabetic, this “safe starches” exclusion is pointless…. [D]espite the type II diabetes, I am doing just fine on the Perfect Health Diet, thank you. I reject the diabetic exclusion of safe starches.
Note that Newell’s fasting blood glucose went down from 125 to 105 mg/dl when he raised his carb intake from Atkins Induction to Perfect Health Diet levels, and postprandial glucose levels on PHD were no higher than his fasting levels on Atkins Induction. It looks like he reduced blood glucose levels by adding starches to his diet.
To repeat: I’m not claiming that our regular diet, providing 20% of energy from “safe starches,” is optimal for diabetics. I don’t know what the optimal diabetes diet is, and it may be different for different diabetics. But I think there is plentiful evidence that even for diabetics, our “regular” diet is not a bad diet. And for some, it might be optimal.
Summary: Putting It All Together
It looks like 20% of energy is a sort of magic number for carbs. It:
- Averts glucose deficiency symptoms while achieving normal insulin sensitivity and glycemic control on oral glucose tolerance tests;
- Avoids significant hyperglycemic toxicity even in diabetics.
Why does this magic number, which happens to be the Perfect Health Diet recommendation for carb intake, do so well?
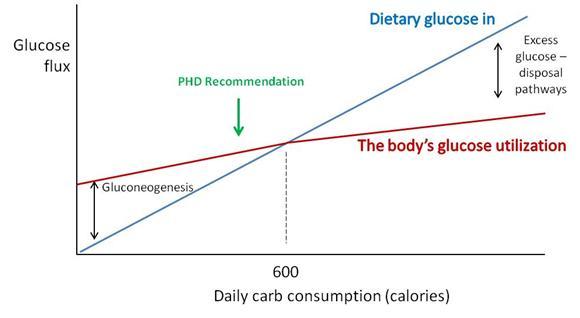
Perhaps a chart will make the science a little clearer.
“Dietary glucose in” (blue) represents the amount of carbs obtained from diet. “The body’s glucose utilization” (maroon) is how much glucose will be put to useful purposes at a given daily carb consumption. Glucose utilization does not vary as strongly as glucose intake; at low intakes a deficit is made up by gluconeogenesis (manufacture of glucose from protein) and at high intakes an excess of glucose is destroyed by thermogenesis or conversion of glucose to fat.
Where the blue and maroon lines cross, dietary glucose in matches the body’s glucose utilization. For most sedentary adults, this level will be around 600 carb calories per day. We recommend eating close to or slightly below this point (“PHD Recommendation”).
There are dangers in straying too far from this intersection point:
- Eating too few carbs creates a risk of health impairment due to insufficient glucose or protein.
- Eating too many carbs results in unnecessary exercise of glucose disposal pathways, and possible unhealthy fluctuations in blood glucose levels if those disposal pathways fail.
Hitting just below the intersection is a safe, low-stress point which will work well for most people.
For diabetics, the excess glucose disposal pathways are broken. However, this is not a major problem if you have no excess glucose to dispose of. Eating up to 20% of calories from carbs doesn’t require the use of disposal pathways – glucose can be stored as glycogen and then released as needed, so the effect of dietary glucose is primarily to reduce the amount of gluconeogenesis. Suppressing gluconeogenesis requires some residual insulin secretion ability, so Type I diabetics cannot achieve this, but most Type IIs can.
The upshot: A 20% carb diet meets the body’s glucose needs without much risk of hyperglycemic toxicity even in diabetics.
The Issue of Thyroid Hormones and Anti-Aging
The most distinctive element of Dr. Rosedale’s diet is its emphasis on longevity as the supreme measure of health, and its emphasis on calorie restriction (especially, carb and protein restriction) and metabolic suppression as the means to long life.
Our book, Perfect Health Diet, relied strongly on evidence from evolutionary selection to guide us toward the optimal diet.
Dr. Rosedale rejects evolutionary selection as a helpful criterion, since evolution did not necessarily select for longevity:
[I]f we evolved in a certain way and with certain physiologic responses to the way we eat, it was not for a long, healthy, post-reproductive lifespan. It was for reproductive success. The two are not at all synonymous, in fact often antagonistic. We have no footsteps to follow as far as the best way to eat for long healthy post reproductive life. We can only use the best science pertaining to the biology of aging and apply it to proper nutrition. That is what I feel I am doing.
We actually share much of Dr Rosedale’s perspective on what influences longevity; it is for longevity that we recommend slightly under-eating carb and protein compared to what evolution selects for. However, we don’t go as far in that direction as Dr Rosedale does.
We have written of the suppression of T3 thyroid hormone levels which is part of the body’s strategy for conserving glucose in times of scarcity, and how this is a risk factor for “euthyroid sick syndrome.” See Carbohydrates and the Thyroid, Aug 24, 2011.
Dr Rosedale acknowledges this and believes it to be beneficial:
I believe that Jaminet and most others misunderstand the physiologic response to low glucose, and the true meaning of low thyroid. Glucose scarcity (deficiency may be a misnomer) elicits an evolutionary response to perceived low fuel availability. This results in a shift in genetic expression to allow that organism to better survive the perceived famine…. As part of this genetic expression, and as part and parcel of nature’s mechanism to allow the maintenance of health and actually reduce the rate of aging, certain events will take place as seen in caloric restricted animals. These include a reduction in serum glucose, insulin, leptin, and free T3.
The reduction in free T3 is of great benefit, reducing temperature, metabolic damage and decreasing catabolism…. We are not talking about a hypothyroid condition. It is a purposeful reduction in thyroid activity to elicit health. Yes, reverse T3 is increased, as this is a normal, healthy, physiologic mechanism to reduce thyroid activity.
Note that Dr Rosedale acknowledges that his glucose-scarce diet reduces body temperature. Many Rosedale dieters have had this experience. Darrin didn’t like it:
This comment from Rosedale support may be of interest to you;
“The best place to measure is under the tongue. Ideal basal temperature is what you have when you first wake up in the morning, and on the Rosedale diet should be upper 96’s lower 97’s. We have found that when someone starts our diet, their basal temperature will go down about 1-2 degrees Fahrenheit which is a great improvement”.
Personally, i did not feel good on a lower body temp when i was low carb (sub 50g) & have been working hard (following phd diet & supps) to get my body temp back up. i would say my basal/morning oral temp is now around the 97.5F on average (up from around 96.5F average pre PHD).
Low body temperatures are associated with a variety of negative health outcomes. For instance, low body temperature is immunosuppressive, leads to poor outcomes in infections, and is a significant independent predictor for death in medical patients. Fever is curative for most infections, low body temperature is a risk factor for infections. Readers of our book know that we think infections are a major factor in aging and premature death. Whether a diet so restricted in carbs that it significantly lowers body temperature is really optimal for longevity is, I think, open to question.
There is a plausible case to be made for the Rosedale diet as a diet that sacrifices certain aspects of current health in the hope of extending lifespan. It cannot however claim to be the optimal diet for everyone. It is certainly not optimized for fertility, athleticism, or immunity against infections.
Conclusion
I am sympathetic to the broad perspective that underlies Dr Rosedale’s diet. Both our diets are low-carb, low-protein, and high-fat, and studies of longevity are the biggest factor motivating the recommendation to eat a fat-rich diet.
However, Dr Rosedale takes low-carb and low-protein dieting to an extreme that I think is not well supported by the evidence.
Dr Rosedale’s direct attempt at refuting our diet consists mainly of two claims:
- Lower blood glucose is better than higher blood glucose.
- The way to lower blood glucose is by eating fewer carbs.
Neither claim is supported. Mortality is a U-shaped function of blood glucose and blood glucose levels around 90 to 100 mg/dl are healthiest, not low blood glucose levels. Moreover, the diet that delivers the lowest blood glucose levels is a high-carb, insulin-sensitizing diet, such as the Kitavans eat, not a low-carb diet.
If I truly believed Dr Rosedale’s argument for lower blood glucose, he would have persuaded me to eat a high-carb Kitavan-style diet. However, I am not persuaded.
I believe that:
- Optimal blood glucose levels are in the 90 to 100 mg/dl range. High-carb diets cause below-optimal levels of blood glucose, especially during fasts. (Indeed, high-carb dieters routinely experience hunger and irritability during long fasts.) Very low-carb diets cause elevated blood glucose due to the body’s efforts to conserve glucose by suppressing utilization. Excessive suppression of glucose utilization is unhealthy.
- A 20% carb diet, while not optimal for every single person, is healthy for nearly everyone. Twenty percent may be the best single prediction of the optimal carb intake for the population as a whole. Even diabetics can do well eating 20% carbs.
And that is why we recommend moderate consumption of safe starches.












Excellent as usual Paul! I await the “epic” response 😉
I’m confused. How long could you eat an Kitavan-style, 80% carb (“high carb/insulin-sensitizing”) diet before you get fat and diabetic? I mean, aren’t your BG levels low on such a diet b/c your pancreas is constantly pumping out insulin to deal with all the glucose?. Just as much as leading to low BG levels ~ 80, wouldn’t the bigger problem be that you are constantly storing fat and burning out your beta cells (or whatever)? Once you become “damaged”, that high-carb diet ceases to produce relatively lower BG levels, and your BG starts creeping up, right?
I just can’t reconcile your 80% carb example with the rest of your post, other than with what I suggest above.
Paul,
On page 89 of your book you talk about the tri/HDL ratio, and state, “When this is high, LDL particles are mostly in the small dense form; when it is low, LDL paticles are in the healthy, large bouyant form”. You didn’t give any numerical examples, so i’m a little confused. My doc is freaking out because my total cholesterol and LDL are high, and wants to put me on drugs (I’m fit, 50, slim and feel great) and at my last (recent)testing my HDL was 66 and my tri’s were 44. This gives me a low “low” ratio, right? Could you elaborate on this a bit?
Thanks (love the book, I’m on my second time through)
Dan
Hi Chris,
You can eat 80% carb and, though it’s suboptimal for health, without some additional causal factor like infections and/or omega-6 fats you probably won’t become fat or diabetic. Carbs and insulin are not the cause of obesity or diabetes. However, once you have these diseases, you tend to have difficulty dealing with an “excess” of any macronutrient, so you don’t want to eat more carbs than the intersection point of my last diagram.
There’s no evidence that you burn out beta cells by eating carbs. That’s within their normal function. Same with cycling of fats in and out by adipose cells.
I think if you think through the post you’ll see everything is consistent.
Hi Dan,
We’ve done a lot of posts this year on why LDL and cholesterol may be high. Usually it boils down to (a) low thyroid hormone status, sometimes due to eating too few carbs; or (b) deficient minerals, especially the antioxidant minerals zinc, copper, manganese, and selenium, or (probably) magnesium, vitamin C, glutathione, vitamin D, vitamin K2.
I wouldn’t go on drugs, unless you turn out to need thyroid replacement hormone. I would just supplement more nutrients, eat more carbs if you’re very low carb, and get a thyroid panel that includes T3 and rT3.
And read posts in this category: http://perfecthealthdiet.com/?cat=140
Best, Paul
manganese is this a new one ?
Hi Herb,
It’s in foods and multivitamins so I don’t talk about it much. I’m not aware that a deficiency is common.
Paul, thanks for your reply.
Maybe I’m missing something, or taking too simplistic a view, or maybe you are saying that consuming carbs doesn’t drive this process, but in a post last November (11/12) you wrote:
“Insulin resistance is a key step in the development of diabetes:
“Insulin resistance in the liver causes the liver to release more glucose into the blood (since insulin inhibits glucose release by the liver). This is discussed in a nice paper [3] found by LynMarie Daye and cited in the comments by CarbSane.
Peripheral insulin resistance means that the rest of the body is less sensitive to insulin. The pancreas has to produce more insulin to dispose of the excess glucose that the liver is releasing.
“This elevation of insulin and glucose levels is a crucial step toward diabetes; it is “pre-diabetes.”
“Persistently elevated glucose levels can then poison the beta cells of the pancreas, diminishing insulin secretion capability and causing diabetes. [4] ”
Maybe I’m using the wrong verbs, or maybe I’m misunderstanding the causal implications of your argument?
…just to answer my own question a bit, perhaps the point is that if the carbs in the 80% carb diet were from wheat and fructose, with some omega-6 oils thrown in to boot, then you’d be in trouble?
Is it toxins, plus choline deficiency, and maybe some other causes, that drive insulin resitance?
Hi Chris,
Insulin resistance is a hallmark of these diseases.
But eating carbs isn’t the cause of insulin resistance. Once you have insulin resistance, then eating carbs causes an elevation of blood glucose that is greater than in people who are insulin sensitive.
Think of it this way. Suppose you need to be infected with a germ, the diabetes virus, to get diabetes. It causes insulin resistance and makes you lose control of blood glucose levels. Then carbs become a problem for you. But carbs didn’t cause the diabetes, the virus did.
To go back to the Kitavan diet, the answer is no, their fasting blood glucose levels are low NOT because their pancreases are pumping out huge amounts of insulin, but because their tissues have adopted a phenotype characterized by high glucose utilization, and this draws blood glucose levels down if you don’t eat carbs for a while. There are many hormones involved in tissue glucose utilization, such as T3 thyroid hormone.
On your last question, yes, wheat and fructose can cause problems. But an 80% carb diet is imperfect also because it doesn’t supply macronutrients in the proportions needed by the body. So carbs have to be transformed into fat, and utilization changed to second-best ways. If the body isn’t working well, then this can become a significant defect. Diabetics are an extreme case, there are plenty of milder cases where there’s no overt symptoms to create a diagnosed disease, but the high carb consumption is still slightly degrading health a bit.
Paul,
Thanks again for your reply – very helpful and I appreciate the time you take to illuminate the issues. I’ve been trying to reconcile what I’ve been reading in your book and this blog with GT’s carb hypothesis, and I think you’d agree that if you don’t have all the pieces of the puzzle in front of you, the carb–>insulin–>obesity/diabetes causal chain makes empirical and logical sense (it fits a lot of the data, but the ‘observed’ relationships require elaboration by identifying exogenous and mediating variables, and specifying the full complexity of various pathways).
The main exogenous ’cause’ I’m still wondering about is, what ’causes’ insulin resistance? I think your answer would be that it is toxins, infection, and malnutrition?
Hi Chris,
Yes … I’m going to be blogging on that next. Basically, two main causes appear to be central — infections which disrupt glucose regulation, and a complex assortment of causes that lead to “cellular obesity”, an excess of metabolic substrates in cells which causes them to resist import of energy by becoming insulin and leptin resistant.
Hi Paul
I have been following all this with avid interest. Just one question for now, one of those few things I always don’t quite understand in your reasoning and comes up again in your previous comment.
“an 80% carb diet is imperfect also because it doesn’t supply macronutrients in the proportions needed by the body.” What do you have in mind that would make the first part of the sentence follow from the second?
“So carbs have to be transformed into fat, and utilization changed to second-best ways.” –again how do we know that transforming is second best?
“If the body isn’t working well, then this can become a significant defect.” Sure. But if it is working well, than it may in principle also be a significant drawback, if the body prefers to convert. I’m not saying that it is a drawback in this case, but in general avoiding such conversions might also be like putting a healthy arm in splints.
I mean for example you wouldn’t presumably recommend that a healthy person supplements with active vitamin D or with estrogen, testosterone, progesterone, cortisol, etc in the proportions the body needs (even if we could tell exactly) instead of ensuring adequate sunshine and cholesterol. This seems to me the general case: we want to let our bodies do what they are designed to do, and they are typically designed to convert nutrients. But then what makes the situation different for (carb to fat) macronutrient conversion?
I understand the logic of the argument for eating some carbs: you argue that the body is not designed to optimally get all its glucose from protein, that can create problems. But have you given also arguments that I missed that the healthy human body is not designed to create some fat from carbs, that it can only do so in an “imperfect” “second-best” way?
Hi donat,
That’s kind of a big question – it would be like the “Safe Starches Symposium”, but with a high-carb dieter instead, making the argument for lower-carb dieting. But my last graph is basically my answer, it’s good to eat the stuff you’re body wants to utilize and bad to eat far from that and force your body to adapt.
I’ll have more on this in the next month.
But macronutrients are quite different than hormones. Your body has to adjust hormone levels very precisely at different times and in different places. There’s no way you can achieve that with exogenous hormones, so you have to let your body determine its own levels. Macronutrients, we’re designed to get them exogenously and in lumps (meals). Very different.
Hi Paul,
Will your book be out in a Kindle version soon? If so, when?
Love your work.
D
Just a quick question, what if your fasting blood glucose is constantly measured in the high 70’s? is that healthy or signaling of something pathological?
This is while eating a relatively low carb diet (aka phd-esque)
Hi D,
Not before mid-December, it looks like now. I’ve been looking for formatters to do it for me, so far without success; if I have to do it myself I’ll start at Thanksgiving and it will probably take me a few weeks. There will be color and black-and-white formats.
Hi Sam,
I wouldn’t take it as pathological unless there is some independent evidence for ill health. There isn’t enough evidence yet for how different people respond to low-carb diets, and why.
Ketogenic substrates will lower blood glucose, so if you eat coconut oil or take BCAAs then that would explain a lower blood glucose.
How do you do on long fasts? Intolerance of fasting would suggest a pathology, ability to do long fasts would suggest keto-adaptation.
In general, I think your body adapts to whatever circumstances you place on it to optimize itself. So I would be reluctant to treat a “biomarker” like blood glucose. Rather I would just observe.
Best, Paul
Also, at what body temp does immune function begin to become suppressed?
Sorry for all the stray comments, I see them only after i post and end up messing everything up. But in regards to intolerance to fasting (severe neuroglycopenic symtpoms) and the aforementioned fasting bg, what type of pathology would could that suggest?
Fairly similar conclusion here re optimal blood glucose levels, even based on a study that had been cited as supporting a different conclusion:
http://bit.ly/phWCVh
Hi Sam,
I would think temperatures below 98 F are probably suboptimal for immunity or wound healing, but note that some variation in temperature over the course of the day is normal.
If you have neuroglycopenia then you know that you are experiencing pathological hypoglycemia and your fasting blood glucose in the 70s is a danger sign. I think you should get a blood glucose meter and start monitoring yourself, to understand how blood glucose varies in response to a meal and over the course of a day (eg when fasting in the morning, when is the hypoglycemia worst) and try to link cognitive symptoms with blood glucose levels. Also test if eating MCT oil relieves symptoms.
What do your doctors have to say?
Hi Ned,
Thanks for the link. Readers may also want to visit this post, linked in the one you link, on the effects of growth hormone and exercise on blood glucose:
http://healthcorrelator.blogspot.com/2011/05/strength-training-plus-fasting.html
Very interesting stuff, and relevant to Sam’s question about individual variability and blood glucose level interpretation.
Best, Paul
Paul, will the Kindle version be identical to the original or will it have any updates?
Hi D,
It will have errata corrections but no significant changes.
Hey Vincent,
that salt article reminds me of our now 18 y.o. persian cat. We got him as a puppy and 90% of his calories since then comes from canned tuna (in brine which is kinda salty too) with the occasional chicken breast here and there or a small piece of salmon. He always disliked all kind of industrial cat foods and we didn’t know what to feed him then, tried the tuna and it stuck.
I don’t know if he has a high metabolism but he’s either eating or sleeping (understandable in his age I think), not one gramm of fat on his body either.
His age is remarkable not only because persians usually don’t live that long but also because he was diagnosed with “heart problems” 10 years ago (the vet said he will live 1 or max.2 years more then) and with bad kidney markers around 7-8 years ago as well (again the vet didn’t give much hope behound 1 year).
We don’t give him any meds.
Sure in his case a high protein diet did work for longevity!
Not that I want to draw any conclusions regarding the human diet from this, just thought it might be interesting in the context of the Ray Peat article.
Uh! Must be “Sure in his case a high protein diet DOES work for longevity!” as he’s still alive and kicking! Well, maybe not exactly “kicking” but still catching some butterflies from time to time. 😉
The gentleman you quoted that is a type II diabetic that was having bs in the 120-130 range after eating your diet, he failed to mention what insulin he was on, Though i would presume no insulin, but then he still refers to himself as a current diabetic. Would be great to know if he is on insulin and if so how many units and of what kind, and great news if he is not taking any insulin.
Hi Fiona,
Newell Wright addressed his medications on his blog, here: http://lowcarbwisdom.blogspot.com/2011/10/safe-starch-debate-diabetics.html?showComment=1320024535787#c6284833866642085590. He is off insulin but does take Metformin ER.
Hi Paul,
I much appreciate the interchange of information. My reply to this post is now posted on my blog;
http://drrosedale.com/blog/2011/11/22/is-the-term-safe-starches-an-oxymoron/
Thanks much,
Ron
More than proving that one diet is better than another, debates like this demonstrate that no one diet is best for everyone.
Questions:
Does 20% carb diet mean 20% of the weight of the food? For example: 2g carbs,5 grams of fat, and 3 grams of protein.
Hi Alex,
No, it means % of calories or energy. In general, the weight of plant foods has to be larger than the weight of animal foods to provide 20% of energy as carbs.
This discussion has been very interesting to follow. I’m surprised to see that the concept of “resistant starch” has not yet come out, as it is completely relevant to many parts of this discussion. “Resistant starch” resists digestion and ends up in the large intestine. It used to be thought that all starch was digested in the small intestine, but autopsies in the 1970s found starch in the large intestines of automobile accident victims. It was officially defined in the early 1990s. Essentially, any type of starch that reaches the large intestine is “resistant starch”. Foods such as intact whole grains, beans, peas, under-ripe bananas, high amylose corn contain high or reasonable quantities of resistant starch. Cooked and cooled starchy foods (think potato salad, sushi rice and pasta salad) contain relatively low quantities of resistant starch. Even bread crust contains tiny amounts because it is formed by retrograded starch after cooking.
On to the good reasons why it’s relevant. Starch that is slowly digested changes the hormonal signaling in both the small intestine and the large intestine. It’s easier to explain by focusing on the large intestinal part, so I’ll focus there first. Starch that reaches the large intestine is fermented by the resident bacteria, producing short-chain fatty acids (SCFA). These SCFAs are biologically active – some are used as energy by the colon cells (butyrate), while others are absorbed and used as energy or biochemical signals throughout the rest of the body (propionate and acetate). Several studies are tracking the fermentation effects from a high amylose corn resistant starch and showing that it increases the production of glucagon-like peptide 1 (GLP-1) and peptide YY (PYY) from the large intestine. Mike Keenan and his colleagues at Louisiana State University is doing a lot of this work in this area. It is turning out that GLP-1 and PYY are involved in satiety, hunger management as well as insulin sensitivity. Their animal studies are showing that animals that eat resistant starch have 50% less body fat than animals that eat high glycemic starch. (Keenan M et al, Effects of resistant starch, a non-digestible fermentable fiber, on reducing body fat. Obesity (2006) 14(9):1523-1534). He has also shown that resistant starch changes hormones known to be involved in energy balance in the hypothalmus as well (Shen L et al, Dietary resistant starch increases hypothalamic POMC expression in rats. Obesity 2009 17(1):40-45.) His latest study showed that high amylose corn resistant starch added to the diet of pregnant, diabetic rats not only improved insulin sensitivity in the dams, it improved glycemic control in the offspring. (Shen L et al, Dietary resistant starch improves maternal glycemic control in Goto-Kakizaki rat. Molecular Nutrition & Food Research, Epub ahead of print June 3, 2011). All very good results and all beneficial effects.
To date, 5 studies have shown that high amylose corn resistant starch significantly increases insulin sensitivity – it makes the body’s tissues more sensitive to insulin. Denise Robertson at the University of Surrey is a strong pioneer in this area. She is being funded by Diabetes UK and has published human clinical trials in healthy people, insulin resistant people and has just begun a study in type 2 diabetics. (For instance, Resistant starch improves insulin sensitivity in metabolic syndrome. Johnston KL, Thomas EL, Bell JD, Frost GS, Robertson MD. Diabet Med. 2010 Apr;27(4):391-7.) The effects are not modest either – another study in insulin resistant men found a 56% improvement in insulin sensitivity with 3 tablespoons of high amylose corn resistant starch sprinkled into food. The 6 tablespoon dose delivered a 73% improvement in insulin sensitivity. (Maki KC, Pelkman CL, Kelley KM, Lawless AL, Schild A, Rains TM. Effects of type 2 resistant starch consumption on insulin sensitivity in men and women. Poster #587.9 at Experimental Biology, April 10, 2011). I can dig out all of the references, but they’re readily available on http://www.resistantstarch.com. The EB poster from April is also available on ResistantStarch.com. It turns out that intestinal fermentation of this type of starch helps shifts metabolism in ways that assist in weight control and insulin sensitivity. There is a lot about the hormonal changes that isn’t known, but the multiple animal studies and multiple human studies all agree that dietary consumption of resistant starch is beneficial for weight and blood sugar control.
Speaking of intestinal fermentation, Australian researchers are showing that high protein diets increase the damage to DNA within the large intestine – it’s carcinogenic. However, resistant starch completely protects against this DNA damage. (O’Callaghan NJ et al. Colonocyte telomere shortening is greater with dietary red meat than white meat and is attenuated by resistant starch. Clinical Nutrition. Epub ahead of print Sept 29, 2011. This is the latest of about 5 or 6 studies published on this subject by this research group.)
Now, returning to the small intestinal effects, the story isn’t quite as clear, but multiple studies have shown that hormonal changes occur after animals eat resistant starch. (Shimada M et al. Feeding rats dietary resistant starch reduces both the binding of ChREBP and the acetylation of histones on the Thrsp gene in the jejunum. Journal of Agricultural and Food Chemistry. Feb 2011; 23:59(4):1464-9) It seems that the location of the digestion matters and resistant starch contains a component that is digested lower in the small intestine, which triggers hormonal changes. It’s not a coincidence that gastric bypass patients experience significant and immediate improvements in insulin sensitivity when the contents of their stomach are re-routed to lower in the small intestine via surgery. Just like people have improved insulin sensitivity 30 minutes after eating foods with resistant starch. As I said – it’s not a coincidence and is part of the reason why a presentation on resistant starch’s effects on insulin sensitivity were presented at the American Society of Bariatric Physician’s meeting on October 28th of this year. (http://www.asbp.org/siterun_data/vegas_courses/doc3248653091309468331.html)
Finally, the National Institutes of Health have funded a study with high amylose corn resistant starch as well. (http://www.clinicaltrials.gov/ct2/show/NCT01027325?term=%22resistant+starch%22&rank=6). Results will be available later next year so stay tuned.
Starches are not all the same. Breaking out the strong scientific evidence differentiating resistant starch from other types of high glycemic starches seems to me a valuable distinction that contributes to this discussion.
Hi Rhonda,
Thanks much for a great comment. In fact our book discusses resistant starch, but you’ve provided even more detail, much of it of recent origin. I appreciate it.
Best, Paul
I’m curious as to your take on resistant starch after reviewing your recommendations to avoid grains and legumes except for rice and potatoes. Rice and potatoes can contain relatively low levels of resistant starch if they’re eaten after cooking and cooling. How do you reconcile the two approaches?
Hi Rhonda,
We recommend eating about 1 pound per day of our “safe starches”, which include not only rice and potatoes but others such as taro and sago. These will provide a fair amount of resistant starch.
In general, we think you can get too much of a good thing, and while the resistant starch from a pound of starchy plant foods is probably highly beneficial, greater quantities may not be. The immune system regulates the bacterial population of the gut and providing too much food to bacteria will increase immune activity as well, which probably isn’t desirable.
Best, Paul
I haven’t seen any studies measuring the resistant starch content of sago or taro. A 2010 study in the Asia Pacific Journal of Clinical Nutrition reported on resistant starch in the Chinese diet, but I haven’t yet seen the actual study. I am assuming that the content is low because we’ve measured the resistant starch content in tapioca, and it was very very low.
Over the past 20 years, about 360 studies have been published on resistant starch benefits. Some of the studies fed a lot of resistant starch. The first insulin sensitivity study by Denise Robertson (Diabelogia, 2003) fed healthy people 100 grams of high amylose corn resistant starch in one day – that’s 9 tablespoons and about 60 grams of dietary fiber. She found more than a 90% improvement in insulin sensitivity as measured by meal tolerance test the next morning. Her subsequent studies have used substantially less. The second study (2005 AJCN) used 50 grams of high amylose corn resistant starch for healthy people, which delivered about 30 grams of dietary fiber in about 4.5 tablespoons. Still a substantial improvement in insulin sensitivity. Her third study was in insulin resistant people, and found that people that are insulin resistant are highly sensitive to resistant starch – and demonstrated higher improvements in insulin sensitivity.
The digestive health studies with resistant starch also used high quantities. One expert estimated that it would take 15-20 grams of resistant starch/day to realize the optimal intestinal benefits. (Baghurst et al, Food Australia, 1996 48(3) suppl. pages 1-36). A tolerance study at the University of Toronto fed healthy people up to 100 grams of high amylose corn resistant starch/day and found that they had to eat 45 grams of fiber (from 75 grams of high amylose corn resistant starch) before they started getting significant quantities of gas. Naturally occurring resistant starch is an insoluble starch granule, which ferments very slowly in the large intestine. It produces SCFAs much deeper into the large intestine than soluble fibers, which are quickly fermented. There is a lot of research suggesting that the production of SCFAs (particularly butyrate) in the distal colon would be beneficial to prevent colonic diseases, most of which occur in the distal colon.
There is no evidence that there are negative effects from getting higher quantities of resistant starch, and much evidence that it is beneficial.
A 2008 JADA study (Murphy MM et al, Resistant starch intakes in the United States, 2008; 108:67-78) found that people eating a typical American diet would consume about 5 grams of resistant starch, but it came from breads, cooked cereals and pastas, vegetables and bananas/plantains. People eating the Perfect Health Diet would not be getting even this quantity. I can see your point about minimizing glycemic carbohydrates, but encouraging the consumption of resistant starch would be beneficial – if only for its insulin sensitivity benefits. If someone is sensitive to carbohydrates (most likely insulin resistant), focusing on increasing a specific type of carbohydrate that specifically addresses an underlying metabolic condition would be beneficial.
If you could improve insulin sensitivity by 20-50% within hours, wouldn’t that be worth adding some resistant starch as a supplement to the diet? You wouldn’t have to eat grains or legumes to get these benefits.
also being a physicist, i find your “potential well” curve makes more sense.
there’re very few phenomena in nature (life science or physical science) that can maintain such linearity.
regards,
what an incredible thing… to have an open/public, intelligent, reasonable, respectful discussion on a subject of major importance to the health of all of us… as though we were all united in recognizing the value of good nutritional and preventative practices (wow, what a concept). if only it were possible to replicate this for other areas where major contradictions exist. as a former cancer patient what i found hard to bear were the differences in opinions about treatments and follow-up (including complementary as well as pharmaceutical and conventional) whereby a protocol according to one source would cure you and to another kill you, e.g. antioxidants during radiation, soy, Tomoxifen, wheat germ extract. inquiries to such places as sloan-kettering, md anderson and NIH were a dead-end. i had imagined starting a radio show along these lines, but this is even better. i hope the concept will increasingly be replicated. thank you and dr. rosedale for showing it’s possible!
Thanks, Robin!
Wow – Thanks for your comments Robin also! What a great complement!
I have 2 questions.
1.) I would like to know how well the body processes fat. If a high fat diet is supposed to be good for glucose and weight issues, then what affect does that have on the organs?
Disregard cholesterol, fat tissue stores, veins, arteries, heart tissues, and other physical presence of fats in the body and focus on ONLY processing of the fatty foods. I would like REAL info as to how this works because a lot of studies show organs are overworked when breaking down the high fat foods.
Either those studies are wrong or right. And, if it is true that fat is hard to process, then what is eaten with it to resolve this dilemma?
2.) What foods can one eat to have a high fat content and yet be LOW in protein? If 50-70% is fat calories, I am lost as to how this gets accomplished.
I would appreciate clarification.
Paul,
Had a tasty Jicama Slaw. Looked it up as a Yambean from the legume family. It is a tuber.
http://nutritiondata.self.com/facts/vegetables-and-vegetable-products/2727/2
Thoughts on this tuber as a safe starch would be appreciated.
Hi Rich,
Well, jicama is not very starchy. Most of the calories are in the form of fiber. I am not sure how safe it is. Wikipedia says the above-ground parts of the plant are highly toxic, and the root/tuber portion does go bad quickly if refrigerated. I assume “go bad” means it develops toxins.
I would take it as one of those vegetables that is fine as a diversification of the diet but shouldn’t be a staple.
Is there any merit to this scenario…(i hope my statements/inferences are correct, let me know if not);
If you have a low or reduced T3 from eating low carb, will it follow that you then have a lower basal metabolic rate compared with if your T3 was higher?
Then does it follow that you will need to intake less calories to maintain your body weight in the reduce T3 state compared to the higher T3 state?
Therefore does it follow that you need to intake less calories on a low carb diet than a higher carb diet to maintain your body weight?
Hi Darrin,
Yes, I think those are true. But the difference in total calories is small.
I am very interested in this phenonmena described in Jaminet’s article which states that long term carbohydrate deprivation leads to fasting blood glucose levels above 100 mg/dl. Is this a proven fact? Is this a bad thing, or is this how humans are supposed to live? I say this because it seems to me that people always crave to have their blood glucose around the 100 mg/dl range which makes them feel euphoric and so forth. Now when I eat carb foods like milk, and fruits I wonder if I am preventing my body from transferring into the state that it is meant to be in.
I tried the extreme diet view of Rosedale in which I eliminated all non fiber carbohydrates (almost) and I made it for about three days before I got scared for my own health and ate some carb food again. Here is what I ate: Unlimited amounts of: coconut, coconut milk/oil, almonds, eggs, and meat. I used some fiber harmony as well.
Hi Paul,
Just wondering if you have the power point handouts from the WAPF conference in Dallas, TX? Thank you.
Cindy Konopasek
It must be true that a nutrient is toxic in one way, even with no threshold, while needed in another way. In HONEST NUTRITION, I called it the good-bad principle. Almost everything is good in some ways, and bad in others. The balance determines the healthful range. That is certainly true with insulin, and likely with glucose. If we focus on either good or bad, we miss the balance.
Bob Ranson (in TYPE 4 DIABETES) could control his autonomic neuropathy only if his blood sugar was up to 100. This non-professional book may hold clues to what is a healthful glucose level.
Ira Edwards