[1] Interesting posts this week: Peter at Hyperlipid links to a new wonder drug that could rescue pharmaceutical company fortunes. In another post, Peter introduces a puzzle: The obese burn more calories at rest than the lean … but they don’t lose weight faster on calorie-restricted diets.
Via @DrEades, lack of sun exposure during childhood may be the cause of nearsightedness; 2 hours per day outdoors prevents myopia.
Mark’s Daily Apple had a nice post on oral hygiene which observes that rice farming did not introduce caries in Asia, whereas wheat farming did in Europe, and maize was the most tooth-destructive grain.
Via Fight Aging!, evidence from beetles that early life immune activity accelerates aging and shortens lifespan.
Art Ayers returned from a long hiatus with an endorsement of fecal transplants. Seth Roberts argues that personal science is becoming more productive than institutional science. Melissa McEwen declares chicken “the ultimate crap meat” and argues that “much of human history has been about the acquisition of starch and fat.” Wired discusses the mystery of the Canadian whiskey fungus.
Julianne Taylor offers “My Plate” alternatives. Dr. John Briffa writes that MSG can increase brain glutamate levels leading to neurotoxicity and promoting obesity. Beth Mazur gives us “Triggers”:
[2] Music to read by: I like the choreographed trombone throwing and handkerchief wiping. Best listened to from a standing desk:
[3] Food reward fascination: So many people have contributed intelligently to the food reward discussion that it’s impossible to link to all of them; I would say that roughly a dozen blog posts and well over a hundred comments were interesting to me.
Let me just mention a few posts:
- Stephan’s series deserves reading in its entirely, but here’s a few that speak to the issue of blandness in diets: from Thursday this week, “modern people would find [traditional diets] bland, and in some cases even unpalatable”; the first post in the series, listing “some of the qualities of food that are inherently rewarding”; and the second post, with the liquid food diet that cures obesity.
- Seth Roberts is a highly creative innovator and, via his Shangri-La Diet, pioneer of food reward therapy for obesity. He states: “At the heart of the theory behind the Shangri-La Diet is the idea that we learn to associate flavors (more precisely, smells) with calories.” The more closely a flavor is associated with calories in our mind, the more we want it. Dissociating flavor from calories leads to less wanting, lower food intake, and lower weight.
- JS Stanton has an outstanding post at Gnolls.org: Why Snack Food Is Addictive: The Grand Unified Theory of Snack Appeal.
- Emily Deans is sympathetic to tasty food.
A few comments that caught my eye:
- Todd Hargrove has set forth an interesting idea: “Even if eating bland food reduces your need for calories, it does not necessarily reduce your need for reward. Perhaps there is a reward set point just as there is a fat mass set point. If this is true, it would suggest that moving the weight set point down by eating less palatable food would fail unless it also reduced the reward set point. Perhaps this explains the emotional struggles that some people have with losing weight, and why people can tend to trade one addiction for another.”
- Andrea Reina notes that if the goal of the Shangri-La Diet is to dissociate flavor from calories, then eating tasty non-calories should be just as helpful as eating tasteless calories. R.K. replied with a link to a piece by Todd Becker quoting Seth Roberts endorsing that idea.
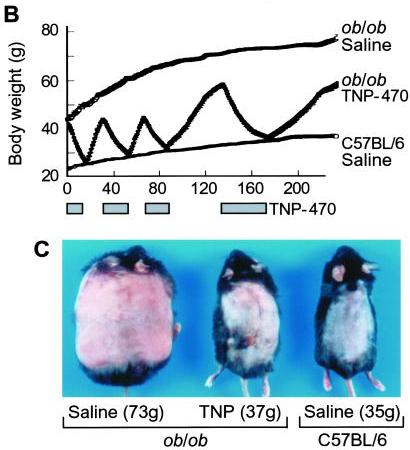
- ItsTheWooo2 has a fascinating story. She has shared her biography starting here, discusses the role of leptin and insulin starting here, and discusses exogenous leptin as a weight maintenance therapy here. Briefly, she believes that the obese develop extranormal numbers of adipose cells, do not lose fat cells when they lose weight, so that to achieve normal weight they have to shrink the fat cells to subnormal size, but that subnormal cell size eliminates leptin secretion. As a result, normal weight obese have subnormal leptin levels, which convinces the brain they are starving, which leads to weight regain. Therefore, the obese need small doses of exogenous leptin to maintain normal weight.
- Betty tells her story of becoming obese following an infection and then becoming slender again during a pregnancy. It sounds to me like the infection induced autoimmunity which caused her obesity, and pregnancy cured the autoimmunity which returned her fat mass setpoint to normal. Of course, Chris Kresser has previously discussed possible autoimmune origins of obesity.
[4] More insight into food reward: In an email Aaron Blaisdell introduced me to the work of psychologist Kate Wassum, who apparently has generated evidence that “the processes that control how much a reward is ‘liked’ are dissociable from those that control the ability of reward-paired cues to trigger reward ‘wanting’.”
This distinction can help resolve many of the puzzles in food reward:
- The optimal diet should be strongly liked (and thus healthy because our evolved biology likes what is good for us) but not wanted (since wanting drives appetite and addictive eating which tends to reduce the variety of the diet and induce malnutrition).
- The most obesity-inducing diet will be strongly wanted but not liked. A not-liked diet is probably unhealthy and promotes disorders such as obesity, while a wanted diet promotes overeating.
If liking and wanting are truly dissociable, then the strategy of eating bland food strikes me as a dubious one.
Bland food is food that is not liked. Eating bland food strives to reduce wanting by reducing liking. But if the two are dissociated, this strategy may not work. If Todd Hargrove is right and we need a certain amount of reward, the strategy might backfire as lack of healthy stimulation of the reward system may increase pathological wanting.
[5] Malnutrition and Obesity: JS Stanton’s snacking-and-food-reward post makes a number of interesting points, but I particularly liked his mention of the “nutritional leverage hypothesis” – basically, the idea that malnutrition causes obesity – put forward by Mike of Fat Fiction.
I have long believed that malnutrition is a major cause of obesity, but it is difficult to show that from published data, in part because the obesity often occurs long after malnourishment begins. (Possibly suggesting that methylation deficits leading to epigenetic changes are important.)
But I think that in the already metabolically damaged, it may be much easier to show that malnutrition is important, because malnutrition has a strong effect on appetite and interacts with the food reward system. So food reward research may help prove the importance of malnutrition in obesity.
In support of the nutritional leverage hypothesis, JS and Mike cite a Chinese trial in which taking multivitamins triggered weight loss.
[6] Cute animal photo:
Via Yves Smith.
[7] Kids like to splash:
[8] New US “Food Plate” to test the food reward theory: The US Department of Agriculture is replacing its “Food Pyramid” with a “Food Plate”:
One might think the USDA has adopted the food reward theory of obesity and has intentionally designed the “Food Plate” to create a bland, unrewarding, fat-less diet. But it gets worse.
They demonize some of the healthiest fats as “Empty Calories”:
Currently, many of the foods and beverages Americans eat and drink contain empty calories – calories from solid fats and/or added sugars. Solid fats and added sugars add calories to the food but few or no nutrients….
Solid fats are fats that are solid at room temperature, like butter, beef fat, and shortening.
Among the approved foods, “Dairy” includes calcium-fortified soymilk and soy beverages; and “Protein” features beans, nuts, and seeds including soy products such as tofu. Approved “Oils” include corn oil, cottonseed oil, safflower oil, soybean oil, sunflower oil, and canola oil – but not butter or animal fats. They do count a few liquid fats among the demonized “solid fats”:
A few plant oils, however, including coconut oil, palm oil, and palm kernel oil, are high in saturated fats and for nutritional purposes should be considered to be solid fats.
I’ve long believed that Department of Agriculture bureaucrats have entirely captured the Center for Nutrition Policy and Promotion, and use it to promote support for agricultural subsidies by propagandizing in favor of the heavily subsidized crops: wheat, corn, and soybeans. This Food Plate is entirely consistent with that idea.
As I mentioned to Steve in the comments, we’ll be working on our own graphical representation of our diet this summer. It will be slightly more complex than the Food Plate – not quite as suitable for kindergarteners, but hopefully more appealing to the food reward system!
[9] I didn’t know that’s what Little Richard looked like:
[10] Meet Bill Lands: In our book, we devoted several pages to Dr. William E. Lands’s work on omega-6 and omega-3 fats. He could give some good advice to the USDA on which oils are healthy. Via O Primitivo, here is a video of Dr Bill Lands discussing polyunsaturated fats.
[11] XMRV link to chronic fatigue a false alarm?: We’ve previously discussed the possibility that a new human gamma retrovirus, known as XMRV, causes chronic fatigue syndrome (see Retroviruses and Chronic Fatigue Syndrome, Aug 24, 2010). This week, Science published two papers arguing that the claimed link was due to laboratory errors, and their editorial called the XMRV-chronic fatigue link “seriously in question’’. The Whittemore Peterson Institute, where the link was discovered, has written a detailed reply.
[12] More on mucin deficiency and GI tract cancers: One of our most popular posts, Dangers of Zero-Carb Diets, II: Mucus Deficiency and Gastrointestinal Cancers (Nov 15, 2010), discussed the possibility that a downregulation of mucin production in order to conserve glucose elevate risk of gastrointestinal cancers.
A new paper out this week (“Suppression of MUC2 enhances the proliferation and invasion of human colorectal cancer LS174T cells”) adds more evidence that a deficiency of mucus in the gut promotes cancer.
Meanwhile, yogurt consumption reduced colon cancer risk by 35%.
[13] Not the weekly video: Would you buy vegetables that were run over by a train?
[14] Shou-Ching’s photo art:
[15] Weekly video: A juggling otter:
























Recent Comments