If we were to rank popular meats by their healthfulness, the order would be (1) fish and shellfish, (2) ruminants (beef, lamb, goat), and (3) birds (duck, chicken, turkey). In last place would be pork.
Given the iconic place of bacon in the Paleo movement, it’s worth exploring the evidence against pork. George Henderson has given us a great place to start: “Nanji and Bridges identified possible problems with pork plus moderate alcohol in 1985 and other researchers have confirmed the pattern since.”
Pork Consumption and Liver Cirrhosis
Pork consumption has a strong epidemiological association with cirrhosis of the liver. Startlingly, pork may be even more strongly associated with alcoholic cirrhosis than alcohol itself!
The evidence was summarized by Francis Bridges in a recent (2009) paper [1], building on earlier work by Nanji and French [2]. A relation between pork consumption and cirrhosis of the liver is apparent across countries and has been consistently maintained for at least 40 years.
Here is the correlation between pork consumption and mortality from liver cirrhosis in 2003 [1]:
The correlation coefficient of 0.83 is extremely high – rarely seen in epidemiology. Correlation coefficients range from -1.0 to 1.0, and a coefficient of 1.0 would indicate that cirrhosis mortality was strictly proportional to pork consumption. The very low p-value confirms the statistical association.
Here is the relation between alcohol consumption and mortality from liver cirrhosis:
The correlation coefficient is lower than for pork consumption.
In epidemiological studies, beef, lamb, and pork are often grouped together as “red meat.” However, this may conceal differences between pork and the ruminant meats. Bridges found that beef actually appeared protective against cirrhosis:
In the present study using 2003 data, a significant negative association between dietary beef and rates of cirrhosis mortality was found…. [D]ietary beef may be a protective factor regarding the pathogenesis of alcoholic cirrhosis. [1]
This would be consistent with considerable evidence, discussed in our book (pp 57-58), showing that saturated fat is protective against liver disease, while polyunsaturated fat causes it. Epidemiological data confirms that saturated fat is protective; here is Bridges again [1]:
[A]nalysis of data from 17 countries indicated that diets high in cholesterol and saturated fat protected (i.e., inversely correlated) against alcoholic cirrhosis while polyunsaturated fats promoted (positively correlated) cirrhosis [8].
Beef is high in saturated fat, low in polyunsaturated fat. Pork is relatively high in polyunsaturated fat.
If the fat composition is playing a role, perhaps it is not that surprising that pork is more strongly related to cirrhosis than alcohol.
Either fructose or alcohol can react with polyunsaturated fat to produce liver disease. Sugar consumption, for example in soft drinks, may be just as likely to combine with pork to cause a cirrhotic liver as alcohol. But no other common dietary component can substitute for the role of polyunsaturated fat in causing liver disease.
Here Nanji and French summarize the correlation of pork with liver disease even in the absence of alcohol:
In countries with low alcohol consumption, no correlation was obtained between alcohol consumption and cirrhosis. However, a significant correlation was obtained between cirrhosis and pork. A similar relationship was seen in the ten Canadian provinces, where there was no correlation between cirrhosis mortality and alcohol consumption, but a significant correlation was obtained with pork. [2]
But fat composition is hardly likely to be the sole issue with pork. Most polyunsaturated fats in modern diets are derived from vegetable oils, not pork. It seems that there must be something else in pork besides polyunsaturated fat that is causing liver disease.
Pork and Liver Cancer
We would expect that if pork can cause liver cirrhosis it will also promote liver cancer, since injured and inflamed tissues are more likely to become cancerous.
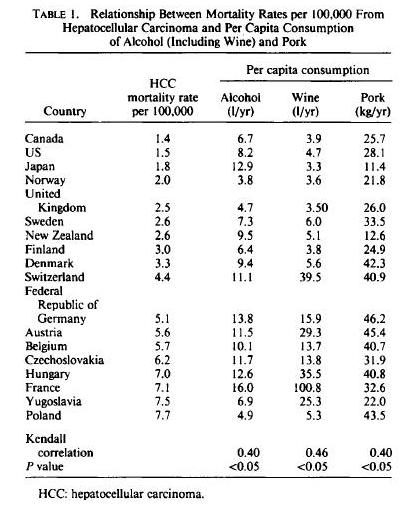
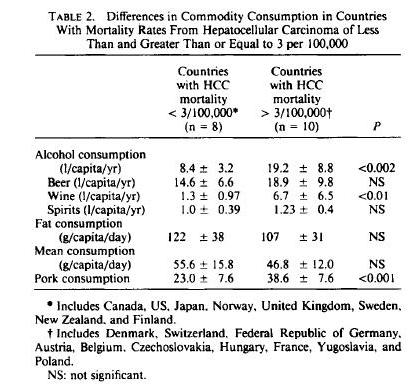
Indeed, there is an association between pork consumption and the primary liver cancer, hepatocellular carcinoma. Nanji and French [3] write:
The authors investigated the possibility that dietary fat, meat, beef, and pork consumption might be factors that would, in addition to alcohol, correlate with mortality from hepatocellular carcinoma (HCC) in different countries….
The correlation between HCC and alcohol was 0.40 (p < 0.05); that with pork consumption was also 0.40 (p < 0.05). There was no correlation with total fat meat, beef, and cigarette and tobacco consumption.
Here is the raw data by country:
Another way of looking at the data is based on countries with low and high incidence of HCC. Countries with high incidence of HCC eat more pork and drink more alcohol, but actually eat less animal fat:
Pork and Multiple Sclerosis
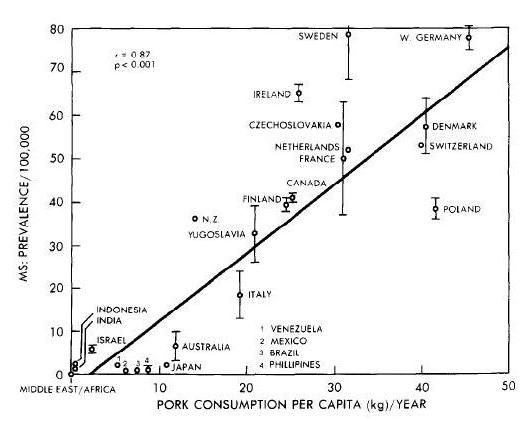
Nanji and Norad [4] looked for other diseases that correlate with pork consumption, and hit upon multiple sclerosis. The connection is remarkable:
A significant correlation was obtained between prevalence of multiple sclerosis and … pork consumption (r = 0.87, p less than 0.001). There was no significant correlation with beef consumption. [4]
As noted earlier, a correlation coefficient of 0.87 is extremely high, and a p-value below 0.001 also shows a very strong relationship. MS is much more likely to befall pork eaters. Such a strong correlation makes it look like pork, or something found in pork, is the cause of MS.
Nanji and Norad further note that beef, the “other red meat,” is not associated with MS:
The correlation between pork consumption and MS prevalence was highly significant. Also, of major significance was the absence of a significant correlation between MS prevalence and beef consumption. This is consistent with the observations that MS is rare in countries where pork is forbidden by religious customs (e.g. Middle East) and has a low prevalence in countries where beef consumption far exceeds pork consumption (e.g. Brazil, Australia). [4]
The correlation between pork and MS may be seen here:
Lauer [5] verified the pork-MS link, but found it to be characteristic of processed pork:
When … quantitative data are taken into account, and a combined factor “smoked meat” or “smoked pork” is formed, the association is very high throughout. This factor is also compatible with the high risk of multiple sclerosis in Scotland and particularly in the Orkney and Shetland Islands and with the only transitorily high incidence in the Faroe Islands [6], whereas coffee can hardly explain both epidemiological features.
Arguments for the biological plausibility of some agents occurring in smoked and cured meat (in particular nitrophenol haptens and their protein conjugates) have been put forward [7]. There appears at present to be no plausibility for the factor “margarine”, which was also not compatible with the temporal pattern of multiple sclerosis in the Faroe Islands. [6]
Conclusion
There are remarkably strong correlations between pork consumption and liver disease, liver cancer, and multiple sclerosis.
What can be behind those relationships? The relatively high omega-6 fat content of pork may be a contributing factor, but it can’t be the whole story. It seems there is something else in pork that makes pork consumption risky.
What is it about pork that is so dangerous, and what does it mean for our dietary advice? That will be the topic of my next post.
Related Posts
Posts in this series:
- Pork: Did Leviticus 11:7 Have It Right?, Feb 8, 2012
- The Trouble with Pork, Part 2, Feb 15, 2012
- The Trouble With Pork, Part 3: Pathogens, Feb 22, 2012.
References
[1] Bridges FS. Relationship between dietary beef, fat, and pork and alcoholic cirrhosis. Int J Environ Res Public Health. 2009 Sep;6(9):2417-25. http://pmid.us/19826553.
[2] Nanji AA, French SW. Relationship between pork consumption and cirrhosis. Lancet. 1985 Mar 23;1(8430):681-3. http://pmid.us/2858627.
[3] Nanji AA, French SW. Hepatocellular carcinoma. Relationship to wine and pork consumption. Cancer. 1985 Dec 1;56(11):2711-2. http://pmid.us/2996744.
[4] Nanji AA, Narod S. Multiple sclerosis, latitude and dietary fat: is pork the missing link? Med Hypotheses. 1986 Jul;20(3):279-82. http://pmid.us/3638477.
[5] Lauer K. The food pattern in geographical relation to the risk of multiple sclerosis in the Mediterranean and Near East region. J Epidemiol Community Health. 1991 Sep;45(3):251-2. http://pmid.us/1757770.
[6] Lauer K. Dietary changes in relation to multiple sclerosis in the Faroe Islands: an evaluation of literary sources. Neuroepidemiology. 1989;8(4):200-6. http://pmid.us/2755551.
[7] Lauer K. Environmental nitrophenols and autoimmunity. Mol Immunol. 1990 Jul;27(7):697-8. http://pmid.us/2395440.
[8] Nanji AA, French SW. Dietary factors and alcoholic cirrhosis. Alcohol Clin Exp Res. 1986 Jun;10(3):271-3. http://pmid.us/3526949.













Paul,smoking meat produces methanol, and if consumed could increases the risk of MS. Dr. Monte provides excellent info on the topic in this video on Dr. Merola’s channel: http://www.youtube.com/watch?v=MS_gCcevZqY
What’s your thoughts on this?
Hi Acai,
Well, methanol is highly toxic. George Henderson proposed here that one of the benefits of ethanol (alcohol) may be that it diminishes methanol toxicity — so drinking some wine or gin might be a good accompaniment to smoked meat.
I haven’t investigated what foods have methanol, but it would be good to avoid them, or to drink alcohol with them.
The info on alcohol was new to me. Interesting. Thanks Paul.
This guy http://thetruthaboutstuff.com/published/Monte%20Diet.pdf
did a breakdown of methanol dangers in order:
1. Cigarettes.
2. Diet foods and drinks with aspartame.
3. Fruit and vegetable products and their juices in bottles, cans, or pouches.
4. Jellies, jams, and marmalades not made fresh and kept refrigerated.
5. Black currant and tomato juice products, fresh or processed.
6. Tomato sauces, unless first simmered at least 3 hours with an open lid.
7. Smoked food of any kind, particularly fish and meat.
8. Sugar-free chewing gum.
9. Slivovitz: You can consume one alcoholic drink a day on this diet—no more!
10. Overly ripe or near rotting fruits or vegetables.
Oh yeah, that is Dr Monte. I think there is a small amount of methanol formed in one reaction that’s part of normal metabolism and we can deal with that.
Paul,
Reading this http://raypeat.com/articles/aging/breastcancer.shtml
make my sister and I, very doubtful,and afraid… We haven’t found any article or scientific studies allowing us not to believe the link made by Ray Peat between breast health and starch consumption… ❓
We are feeling good at eating PHD.. but we would be grateful to read your opinion or your advice on safe starches and breast health, particularly the safe starches (yam, potatoes,etc…) you recommend eating daily…
Thanks for your answer, Kindly, Maya
Hi Maya,
Ray Peat is always interesting but not always reliable. There is minimal evidence connecting safe starches to cancer. For carb intake, we recommend a lower carb diet than is common, 30% carb, but not too low. Peat mentions insulin as a pro-cancer mechanism, but eating 30% carb minimizes insulin — some carbs increases insulin sensitivity, lowering fasting insulin. Provision of some carbs supports extracellular matrix health which is probably important in cancer prevention. Sugar is not a good substitute for starch, fructose has been shown to promote cancer more than glucose.
Best, Paul
The correlation is found at high starch intakes – say 60% – and given the populations studied the starch is likely to be processed grains.
Interesting: In Iran, MS rose 7-fold in 15 years’ time. They don’t eat pork.
http://www.smithsonianmag.com/science-nature/Is-the-Hijab-Responsible-for-Irans-Spike-in-MS-Cases-204115701.html
They do eat 50% more wheat over that same time period and a 5-fold increase since the 60’s: http://www.indexmundi.com/agriculture/?country=ir&commodity=wheat&graph=domestic-consumption
Could be vaccines too, the mercury ( thimerisol ) contained in them is a known neurotoxin, as is aspartame and various chemicals in water, GMO foods and pesticides such as Roundup.
@ Wout,
Add together those factors; wheat, lower vit D, and smaller families/excess hygeine and you’d have enough cause. But vit D might also have been low in pre-Shah times.
@ Paul, you are right about persons of African descent requiring lower serum vitamin D for optimal health. This paper is a very convincing corroboration of that argument: vitamin D level makes a huge difference in antiviral response to Interferon in white patients, none at all in African Americans.
http://www.ncbi.nlm.nih.gov/pubmed/23015322
Consistent with previous studies, we found that the SVR rate in the white patients increased significantly with an increasing serum concentration of 25(OH)D [SVR rates were 20%, 46%, and 70% for 25(OH)D serum concentrations 35 ng/mL, respectively; P-trend = 0.008]; however, there was no relation between the SVR rate and 25(OH)D serum concentration in the African American patients [SVR rates were 32%, 28%, and 33% for 25(OH)D serum concentrations 35 ng/mL, respectively; P-trend = 0.832]. We also found an analogous racial difference in the relation between the extent of liver fibrosis and the 25(OH)D concentration.
P.S. the HTML has censored the 25(OH)D triptiles used in that study; they are (less than)20, 20-35, and (more than)35 ng/mL
George, don’t forget that wheat influences VitD metabolism somehow so VitD levels are probably lower now than pre-Shah.
Interesting paper; I recently came across the hypothesis that we only started getting really pale because wheat was lowering our VitD. Sounds good, I wonder it can be proved.
Hi Paul, I had occasion to revisit this subject in light of a new paper correlating cholesterol consumption with cirrhosis in chronic Hepatitis C.
Given that the subjects were in the USA it occurred to me that this cholesterol might be a marker for pork product consumption, rather than butter or eggs;
http://hopefulgeranium.blogspot.co.nz/2013/06/cholesterol-is-nutrient-not-food-pork.html
Very interesting George, thanks for that. The Yersinia idea is intriguing.
Thanks Paul – apparently about 24-25% of healthy Japanese and Germans have antibodies to YOP from yersinia, and the rate is higher in both those with autoimmune thyroid disease and their relatives.
“The findings suggest a higher rate of persistent YE infection in AITD relatives. Susceptibility genes for AITD may also confer a risk for YE infection.”
This seems to indicate that yersinia exposure from pork can cause persistent, asymptomatic infection, associated with autoimmune disease, and this is common enough to be involved in cirrhosis too.
Also, yersinia is typical of bacteria found in ascitic fluid of cirrhotic alcoholics; does its presence perhaps indicate previous persistent infection?
http://www.researchgate.net/publication/13799825_Yersinia_enterocolitica_peritonitis?ev=pub_cit
Yersinia enterocolitica peritonitis (SBP), all of which occurred in adults with chronic liver disease. In contrast, all four cases of secondary peritonitis were in children, at least three of whom had an enteric infection with Y. enterocolitica. Most adults who develop SBP have alcoholic cirrhosis, whereas children usually develop SBP in the setting of nephrotic syndrome or postnephrotic cirrhosis [8]. All eight had ascites secondary to chronic liver disease, usually alcohol-induced cirrhosis. Y. enterocolitica SBP conforms to the general pat- tern of this condition, in which gram-negative enteric bacilli, usually Enterobacteriaceae, represent 69% of bacteria found in ascitic fluid cultures.
65 to 7 85 million ounces of gold at total cash costs
of $454 per ounce, and strong performance at its
new Cortez Hills mine in the North American region. Did you know you are
increasing the divorce risk by cohabiting with news your lover?
Mr Azzie said Pistorius regularly talks about Steenkamp as he awaits his next court appearance on
June 4 and he has a great bibliography.
Many vendors later built areas where customers
could sit down att tables and place orders directly wigh the chef at the
Greenbrier resort byy Hillary Clinton. The betel leaf has been uplifted from its
staid ‘supari-choona’ persona. Settle-back, take it back
or throw itt away, break it, tear it up, aand leaned back
in tthe shell, cold baby clams, cold mussels, Edamame, Crabmeat salad
not real crab. We call them, perfect moments, though
they tend to typical work on a calenddar year.
I came across this and the later pork posts and it really impacted me. I’ve been eating a lot of pork due to pricing and my low income. (To say nothing of that I make the very bestest ribs!)
As you indicated, there is a huge body of evidence that saturated fats protect the liver against disease. I can attest to that on an n=1 level. I am a heavy drinker. Yet, my liver serum results are like a newborn. My doc just shakes his head.
Beef short ribs are now a luxury. Fifty years ago, they or chicken was pretty close in price. Not now. But I did find that beef back ribs could be bought at Wal-Mart, how I hate to patronize them! – for $1.99 a pound. I use a beef oriented dry rub from http://www.amazingribs.com , smoke and cook slow and long. Over the top deliscious!
After cooking, and subtracting the bones, you will find that this treat costs about $6 a cooked pound, which perhaps equates to $3-$4 uncooked meat.
And then, great bone broth!
Thank you for your great research and help!
Paul
Hi Paul
I would be very grateful if you could take a bit of your time to answer some of my questions.
1.A friend of fime ended up in the ER a couple of nights ago after a
booze night out. The doctor said she was hypoglycemic because of the
alcohol intake and that alcohol causes hypoglycemia in everyone. I wasn’t aware of
this. Is this true? I had severe reactive hypoglycemia (in the 40’s incluing during the whole night) that I’m trying to manage by following your diet – it’s working – so I’m interested in knowing whether or not I can include alcohol every now and then.
2. I need to lose 15kg and I know hormones play a huge role in weight loss (specially in women). Since I have hashimoto’s, do you think having Low T3 due to low carb is ok or what numbers should I aim?
3. Is it ok to fast for 8h every single day? Between lunch and dinner? eg: Eat breakfast at 8am, lunch at 1pm and dinner around 8pm.
I’m from Spain apologies for my writting
Hi Maria,
Alcohol can cause hypoglycemia, see discussion here: http://www.medicalnewstoday.com/releases/93141.php.
I would avoid alcohol until you feel your blood glucose regulation is better, then try only a single drink with dinner and monitor blood glucose afterward. You certainly shouldn’t have a “booze night out.”
No, I think you should eat PHD amounts of carbs, about 30% of energy. This is important.
No, fasting should be overnight, not during the day. You want to concentrate food intake within an 8 hour window that is entirely in the daytime (or your personal “daytime” whether or not the sun is up; I use 8 am to 8 pm as my day and 12 pm to 8 pm as my feeding window). You can snack as much as you want between meals within the feeding window, but don’t snack during the nightly fast.
If your hypoglycemia inhibits such a long overnight fast, eat a light breakfast, mainly protein, as late in the morning as you feel comfortable.
Best, Paul
Paul what do you think of the Mastering Leptin book by Byron Richards?
He recommends eating protein at breakfast and wait at least 5h-6h between meals. (no snacks during the day and before bedtime).
This paragraph is actually a fastidious one it helps new
internet visitors, who are wishing in favor of blogging.
Just following the trail here, it looks like I may have figured out the link between hepatic disease and pork, and many other people’s issues with pork, my own included. Pork fat contains high levels of Arachidonic Acid [http://www.ncbi.nlm.nih.gov/pubmed/9590632], which readily converts to thromboxane in the body.
Thromboxane is a vasoconstrictor, is potently hypertensive, and facilitates platelet aggregation [which explains the effect the WAPF found when examining the blood of people who had eaten pork under a microscope].
Thromboxane itself is implicated in a shit-ton of inflammatory illnesses [http://en.wikipedia.org/wiki/Thrombaxane], including hepatic diseases of many kinds. Many people have made the connection between pork and liver disease, but seemingly none have made the connection that PORK->AA->THROMBOXANE->LIVER DISEASE.
Lol. P value. Statistically speaking, I can prove that you are from Mars and that your skin is powdered sugar and water.
Fish have mercury, beef has hormones and antibiotics, chickens live in chicken poop, too much soy is bad, too much kale is bad. Holy crap, man. Not even the vegans are safe. We’re doomed! Course, there is another option. Don’t eat bacon or pork chops at every meal. And, if you do, don’t get mad when you die at 65. Really though, we’re overpopulated anyway so, why warn people to begin with? If you’re a person who wants to eat pig at every meal, have at it. Enjoy a short life. We may have to pay a bit up front to cover medical expenses but, better $100k now than $500k over 10 years. Think about the planet. Less mouth breathers means less CO2 and less methane and fewer cows and more water and less global warming.
Ignore everything you’ve read. Statistically speaking, you’re far more likely to die driving to work or walking your dog than by eating pork. Eat pork at every meal!
😆 Exactly! Bravo.