I’ve had about ten requests for thoughts on the new paper in Nature Medicine [1] that finds red meat can promote atherosclerosis by a roundabout route: carnitine in the meat is metabolized by gut bacteria into a compound called TMA, which the liver converts to TMAO, which in high doses promotes growth of atherosclerotic plaques.
The same group has done similar studies with other molecules; two years ago the culprit was not carnitine but phosphatidylcholine. [2]
The Scare
Some of the news stories:
- Wall Street Journal, “New Health Worry in Red Meat”
- New York Times, “Culprit in Heart Disease Goes Beyond Meat’s Fat”
- Scientific American, “Red Meat May Clog Arteries Because of Gut Bacteria”
- ScienceDaily, “New Link Between Heart Disease and Red Meat: New Understanding of Cardiovascular Health Benefits of Vegan, Vegetarian Diets”
- The Scientist, “Steak Linked to Heart Disease”
It sounds like red meat is dangerous! The best line came from the New York Times:
Lora Hooper, an associate professor of immunology and microbiology at the University of Texas Southwestern Medical Center, who follows the Paleo diet, heavy on meat, exclaimed, “Yikes!”
The Big Picture
The issue here is closely related to one discussed in page 77 of our book:
Protein is not food for us alone; gut bacteria can ferment protein.
Although fermentation of carbohydrates by gut bacteria is usually beneficial, fermentation of protein is not: it generates toxic compounds, including amines, phenols, indoles, thiols, and hydrogen sulfide, which make a foul-smelling stool.
It seems likely, therefore, that high protein intakes are suboptimal for gut health.
When protein is fermented, nitrogen is released, and many nitrogenous compounds are toxic.
The group behind the new research, led by Stanley Hazen, has been looking at another pathway by which bacterial fermentation of meat might be dangerous – the pathway that runs through Trimethylamine. Trimethylamine (TMA) has a simple structure; three methyl groups bonded to a nitrogen atom: N(CH3)3.
Compounds such as choline and carnitine that contain both methyl groups and nitrogen are potential precursors to TMA.
TMA is responsible for the fishy smell of decaying fish. It is highly abundant in fish.
The liver converts TMA into its oxide, TMAO. The Hazen group in a series of papers has argued that higher TMAO levels in blood are associated with atherosclerosis. In a recent paper they assert, “TMAO levels explain 11% of the variation in atherosclerosis.” [3]
So, the equation they are putting together is: fermentation of meat in the gut produces TMA leading to TMAO production which may increase your chance of atherosclerosis by 11%.
Risk is Highly Dependent on the Nature of Your Gut Flora
Here is the key data from the new paper [1]. The “d3” prefix means that the carnitine was labeled with deuterium, an isotope of hydrogen, to help trace its molecular destinations.
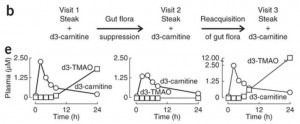 In the left panel of part (e), subjects have been fed a steak (eaten in 10 minutes) plus a 250 mg deuterated carnitine supplement – in total, the carnitine equivalent of 1.5 pounds of meat. Deuterated TMAO levels in blood rise to about 1.8 parts per million after 24 hours.
In the left panel of part (e), subjects have been fed a steak (eaten in 10 minutes) plus a 250 mg deuterated carnitine supplement – in total, the carnitine equivalent of 1.5 pounds of meat. Deuterated TMAO levels in blood rise to about 1.8 parts per million after 24 hours.
Then subjects are given antibiotics for a week to suppress their gut flora, and fed steak and deuterated carnitine again. On antibiotics, their blood has no deuterated TMAO at all 24 hours after the meal.
In the right panel, 3 weeks after coming off antibiotics to allow gut flora to regrow, subjects are challenged again with steak and deuterated carnitine. Their blood level of deuterated TMAO now exceeds 12 parts per million – 7 times higher than before the antibiotics.
They go on to test the mix of flora in subjects, and show that flora composition is closely correlated with blood levels of deuterated TMAO after consumption of deuterated carnitine. Some types of gut bacteria produce a lot of TMA from food carnitine, others produce little.
So the amount of TMAO entering the blood from bacterial metabolism of food carnitine is highly dependent on the nature of the gut flora. If you kill off normal flora with antibiotics, then eat meat and carnitine, you will get an overgrowth of bacteria specialized to feed on meat and carnitine. That might not be good for you.
The Vegan vs Omnivore Comparison
Food carnitine is far from the only source of blood TMAO. In fact, TMA is a natural breakdown product of choline, one of the most abundant molecules in the body, and the body has evolved an enzyme for converting TMA into TMAO — the gene is FMO3. So we should ask, how much does metabolism of carnitine by gut bacteria affect blood TMAO levels? For that we need measurements of normal TMAO, not just deuterated TMAO.
We can see what that data looks like in a plot comparing blood TMAO levels between vegans and omnivores (panel c of their Figure 2):
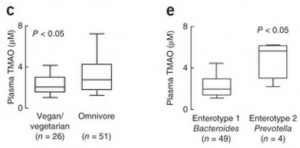 These are the TMAO levels normally circulating in the fasting blood of SAD omnivores and vegetarians. As you can see, there’s considerable overlap between the two distributions. 75% of the omnivores had TMAO levels within the same range as 90% of the vegetarians.
These are the TMAO levels normally circulating in the fasting blood of SAD omnivores and vegetarians. As you can see, there’s considerable overlap between the two distributions. 75% of the omnivores had TMAO levels within the same range as 90% of the vegetarians.
So about 75% of omnivores and 90% of vegetarians have normal TMAO levels. What about the 25% of omnivores and 10% of vegetarians whose TMAO levels are elevated?
In panel e, you can see that the enterotype of the gut flora is a much better predictor of blood TMAO levels than whether someone eats meat. Those with high Prevotella, low Bacteroides averaged about triple the TMAO levels of those with low Prevotella, high Bacteroides flora.
So it really is the gut flora that determine blood TMAO levels.
What Drives the Gut Flora?
What determines whether you have the bad gut flora?
The general picture is this. The immune system regulates the number of microbes living in the gut. When levels become high, antimicrobial peptides are released into the gut to kill some off. When levels are low, antimicrobial peptide production is reduced to let microbes multiply.
This means that if the proportion of bacteria who feed on protein, carnitine, and choline is too high, it’s probably because there is insufficient food for the competing bacteria who feed on carbohydrate forms of fiber. If you have a lot of gut bacteria feeding on fiber, there’s no room in the gut for large amounts of bacteria who feed on meat.
So the 25% of omnivores and 10% of vegan/vegetarians with high TMAO levels are probably the people on low-fiber diets – the ones who get their carbs from flour and sugar. On such a diet, the good bacteria are starved and the bad bacteria that produce TMA multiply.
How Does TMAO Produce Atherosclerosis?
The explanation offered by the Hazen group is that TMAO suppresses “reverse cholesterol transport” conceived broadly as the process of migrating excess cholesterol out of macrophages for transport to the liver and excretion in feces via the bile.
Basically, the idea here is:
- Atherosclerosis begins with metabolic syndrome, a state characterized by high LDL levels and caused by endotoxemia (high levels of endotoxins entering the body from the gut).
- As we’ve discussed (“Blood Lipids and Infectious Disease, Part II,” July 12, 2011), LDL particles have an immune function. They are oxidized by microbial cell wall components. The resulting oxLDL particles are taken up by macrophages, which then present the microbial cell wall components to other immune cells for antibody formation.
- Endotoxemia initiates the process of atherosclerosis by (a) poisoning the liver to cause metabolic syndrome which raises LDL levels, and (b) oxidizing LDL – since endotoxins are bacterial cell wall components that can oxidize LDL – and driving the oxLDL into macrophages.
- After macrophages have separated the microbial cell wall components from their accompanying LDL particle, the cholesterol and fat have to be exported to keep them from building up in the cell.
- If cholesterol and fat cannot be exported quickly enough, the macrophage is injured and becomes a “foam cell.” Disabled foam cells accumulate in specific locations and form atherosclerotic plaques.
- TMAO suppresses bile acid creation, reducing the excretion of cholesterol from the body and leading to higher LDL levels and a greater likelihood that macrophages will become foam cells.
If this is true, then TMAO is not intrinsically atherosclerotic. TMAO in blood only becomes atherosclerotic in the context of metabolic syndrome brought on by endotoxemia.
What causes endotoxemia? A dysbiotic flora generated by a diet high in sugar, flour, and omega-6 fats (see our book, pp 220-222).
Conclusion: Lessons Learned
The lessons of this study are:
- Don’t eat a high-sugar, high-flour, low-fiber diet.
- Do eat natural whole foods that have the kind of fiber we and our probiotic gut flora co-evolved eating; mainly, resistant starch from in-ground starches like potatoes and soluble fiber from fruits and vegetables.
- Don’t eat excessive amounts of meat. As we noted in the book, excess protein is available to gut bacteria for fermentation and that produces a number of toxic byproducts.
- Do eat PHD levels of meat – one-half to one pound per day. This level of meat consumption will provide healthful and nourishing amounts of protein, choline, and carnitine, and will not cause any harm if accompanied by PHD levels of healthy plant foods.
None of these lessons is new. This study doesn’t overturn any established dietary wisdom. It is just one more piece of data reminding us to eat a balanced diet consisting of the foods we evolved eating – plant as well as animal.
References
[1] Koeth RA et al. Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013 Apr 7. http://pmid.us/23563705.
[2] Wang Z et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011 Apr 7;472(7341):57-63. http://pmid.us/21475195.
[3] Bennett BJ et al. Trimethylamine-N-oxide, a metabolite associated with atherosclerosis, exhibits complex genetic and dietary regulation. Cell Metab. 2013 Jan 8;17(1):49-60. http://pmid.us/23312283.











What about eggs in the diet? Will the combination of 1/2 lb grass fed/finished beef PLUS several patured eggs cooked in butter provide too much choline for the system to process?
No.
Thanks! I was hoping you would tackle that study.
I’d like to take a moment to remind everyone how to maximize RS in their diet.
When preparing potatoes, eat a slice or two raw. Then cook your potatoes in a variety of ways (roasted, fried in good oil, boiled, baked, cooked and cooled) There are many studies that show different prep methods greatly effect the RS in potatoes, but raw always has the most!
Eat cold rice. Eat green bananas. Eat plantains.
Here are two ways to get a huge amount easily:
Many researchers recommend 20-30g/day of RS. that’s almost impossible to do eating PHD levels with no grain.
1. Raw, unmodified potato starch, like Bob’s Red Mill sells, is about 8g RS per TBS. Put a couple scoops in a glass of milk or other cold drink for a huge dose.
2. Buy green plantains, slice and dry them, eat as you would a cracker. Nearly 100% RS by weight, a large, dried plantain weighs about 100g so each plantain is 3-4 days worth of RS.
If you are on the fence, just google Resistant Starch! You will soon be a convert.
White rice doesn’t have any fiber to speak of, does it?
Not when it’s freshly cooked but if you let it cool after cooking then resistant starch forms.
does resistant starch remain after reheating?
I don’t think raw potatoes should ever be eaten raw — not even a slice. Potatoes must always be cooked in order to reduce the toxic solanine content. There are more reasons why potatoes should be cooked linked here. Plus, your starch can’t be accessed when potatoes are uncooked — your digestive tract can not digest them raw.
“your digestive tract can not digest them raw.”
that’s the point and that’s why it’s called Resistant Starch.
just don’t eat green potatoes, then they are not toxic.
Raw potato was traditionally one of the biggest sources of vit C and thus invariable source of scurvy prevention in Siberia
i also dont’ believe potato should be eaten raw for the same reason;
there is a reason potato is rarely eaten raw traditionally
it probably causes indigestion big time, for me, at least.
(well, overdoing raw veg disagrees w/ me anyway.
Chinese do not believe veg should be eaten raw, too “cold”
i wonder my ancestors all had IBS…. XD)
so no thanks, i prefer to stay w/ fermented veg.
if it’s not natural to get so much from the paleo diet (PHD/real food), to me, that just means that we probably don’t need that much.
i’m not disputing the benefits of RS; i’m only skeptical about optimal dosage for gut health.
ps. having said that, i do eat moderate amount grains (white rice or properly soaked)
Can you tell me how to make the plantains come out tasty? Literally slice and dehydrate? No oil or —? How thin or thick sliced? (I have a dehydrator but am very inexperienced with it.)
The only plantains I’ve ever enjoyed were brown and fried, but someone told me the green ones are the only one with the good starch. But — I hate fried green plantains. Even if boiled first.
thank you!
I guess stay away from seafood since it causes up to 100x the levels of TMAO? See Chris Masterjohn’s recent post. Hmmm.
Yes, if TMAO were really a major problem then seafood would be really bad. It isn’t.
Nice post, I think you might be right about the flora. Initially I thought the omnivorous outliers were probably the heavy fish eaters for the reasons Chris Masterjohn mentioned, that’s certainly plausible, though fiber and general gut health is obviously a big factor.
So antibiotics are bad for us.
It’s still hard to see how TMAO is a toxin. It’s an osmolyte, protects proteins from stressors such as urea (so even if it did slow cholesterol export, it might still have other benefits).
“Some osmolytes, such as trimethylamine-N-oxide (TMAO), are known to protect proteins against harsh environments (1, 2). In particular, TMAO counteracts the destabilizing effect of urea on protein structure (3–5). Addition of TMAO to a protein solution usually results in increased protein stability against denaturation (6, 7), and higher rigidity of the protein backbone (8, 9). Mechanistically, TMAO compacts a protein globule, while urea does the opposite (8, 10, 11)”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3075470/
A Fat Head commenter pointed out this suspect extract from the study:
“An analyte with identical molecular weight and retention time to
l-carnitine was not in the top tier of analytes that met the stringent
P value cutoff for association with CVD. However, a hypothesis-driven
examination of the data using less stringent criteria (no adjustment for
multiple testing) revealed an analyte with the appropriate molecular
weight and retention time for l-carnitine that was associated with cardiovascular event risk (P = 0.04).”
I am loving the PHD book by the way. After owning a credit card for 2 or 3 years I finally used it online. The book is great value for money, stuffed full of facts and food for thought, and exceptionally well written.
Hi George,
Obviously TMAO is more healthful than TMA, that’s why we have an enzyme for converting TMA to TMAO. It’s probably not just sexual selection against the unpleasant body odor that led to this.
Also obviously, the body doesn’t try to reduce TMAO levels to zero, but maintains a physiologically “normal” level across a range of diets, vegan to high meat. That suggests it is doing something good.
I saw that sentence noted by the Fat Head commentator. It is followed by the sentence “In further studies we were able to confirm the identity of the plasma analyte as L-carnitine and develop a quantitative stable-isotope-dilution liquid chromatography tandem mass spectrometry (LC-MS/MS) method for measuring endogenous L-carnitine concentrations in all subsequent investigations (Supplementary Figs. 1–3).” I’ll give them the benefit of believing it really is carnitine.
Thanks George!
A great point in Chris Masterjohn’s article:
“this same group has previously shown that the enzyme responsible for converting trimethylamine to TMAO is suppressed by androgens, and its activity is low in males compared to females.”
Females make more TMAO. What is a risk factor for CVD? Male gender.
Part of the study compared one (n=1) female omnivore with one (n=1) male vegan. The (male) vegan made less TMAO.
So this was a confused hodgepodge of an experiment, one that produced results that the authors themselves were in a perfect position to discount. Why didn’t they?
Hi George,
I saw that too. The previous study is my reference [3]. Another twist is that the enzyme that oxidizes TMA to TMAO, FMO3, is induced by bile acids so that bile acids raise TMAO levels, while TMAO suppresses bile acid production. So there is a feedback loop, tending to produce stable TMAO levels. This too suggests that TMAO is biologically useful and physiologically regulated.
Now, TMAO is an osmolyte and so is taurine. Taurine is used to make bile salts. Does a high level of TMAO suppress taurine synthesis to maintain osmolytic tone?
Could be a mechanism…
Osmolytic tone might be important because too much protecting of proteins might inhibit autophagy and protein turnover.
Or not…
What about those of us who currently have a gut dysbiosis? I am having trouble digesting even with a lot of betaine HCL and acidopholous and enzymes–I was told by a naturopath my intestine was very inflammed, infected, full of bad bacteria… Would it behoove someone like me to cut down on protein? If so, how low on protein is too low? (especially for someone who is very underweight like me, trying to nutritionally recover, and thus eating a lot of calories in a very unequal body weight/caloric intake ratio?)
Hi grae_bird,
It’s difficult to give advice over the Internet. What sort of trouble do you have – bloating, gas, constipation, diarrhea, reflux, brain fog, fatigue, food sensitivities? What diagnostic steps / lab tests have you undertaken?
It’s appropriate to eat normal amounts of protein and some carbs. If you tolerate carbs OK, try to get 30% of calories from them.
I know it is hard to diagnose over the internet. My chief complaints are constipation, insomnia, and depression. But symptoms include bloating, burping, gas, pain, constipation up to 2 or 3 weeks unless living on laxative, headaches, fatigue, depression, anxiety, irritability, impaired thinking and memory, insomnia, inability to concentrate, muscle pain, clumsiness, incredible thirst, increasing food intolerances…. Traditional endoscopies and colonoscopies, stomach motility tests, and normal blood panels have shown nothing. I just had a more complete protein, adrenal, thyroid, autoimmune testing but hte results have not come back yet.
But with a probable gut dysbiosis would 15% of caloric intake (although that makes it about 1.2 g protein per lean lb body weight) from protein (1 lb plus 2 eggs usually)be too much?
I do try to get 15% caloric intake from protein, 30% carb from safe starches and green veggies, and the rest from fat.
Hi grae,
Some things to try:
– Make homemade kimchi/fermented mixed vegetables and eat a small amount daily.
– Make homemade bone & joint broth soups and eat regularly.
– 1 g vitamin C per day.
– 500 mg NAC per day.
– Liver regularly – 1/4 lb beef/lamb liver per week plus 1/4 lb duck/goose/organic chicken liver
– Optimize vitamin D levels
– Minimize other supplements, but experiment with magnesium which is key for constipation
Best, Paul
Thank you! I am grateful for the advice.
Have you had any sort of stool microbiology testing?
and thank you so, so, so much for taking the time to reply. i know you are busy. but it means a lot.
If fish are high in TMA, what are the implications of high fish intake vs red meat?
If TMA were harmful then fish would be worse than red meat, but I don’t think TMA is harmful and I think fish is very healthful.
I think TMAO levels are regulated and if you eat a good diet they’ll be regulated successfully and none of these atherosclerosis concerns will come to pass, no matter how much fish you eat.
Hi Paul,
For reasons I am now second guessing (to detox and boost immunity) I started taking a Modafilan Seaweed Extract http://www.modifilan-seaweed-extract.com/ iodine supplement about 3 weeks ago. The dose recommended 4-6 capsules a day, I only took 2-3 because it sounded excessive and expensive to me. I have also put on 5-7 lbs since around the time I started. It could be my imagination or an unrelated coincidence, but I feel more bloated and look heavier as well. Is this a result of the Iodine? The detox? Although I can’t be sure it’s from the supplement it’s the only change I can think of that may be causing this. I will stop taking for now but any advice you have would be so appreciated. My partner also got a severe acne flare up since starting.
Regards,
Sana
Hi Sana,
That does sound like hypothyroidism – maybe hyperthyroidism. It is probably excess iodine, possibly compounded by other items in the seaweed extract. That site doesn’t tell us the dose of iodine in a capsule but it might be large. Suddenly starting high doses of iodine often generates hypothyroidism.
I would drop that supplement immediately. If you want to take iodine, try buying the NOW Potassium with Iodide on our supplement recommendations page and cut it into quarters with a razor blade and try one quarter daily. Double the dose once a month and when you reach one tablet daily, stay there. That will be 225 mcg/day.
For the acne, try taking extra salt, water, and vitamin C. Acne usually results from bromine detox and is a sign that you need iodine.
Thank you Paul 🙂
One also has to suspect that eating meat in the way a normal HG would (alongside some plants or at least fermented plant juice), rather than in a lab with a carnitine chaser, might have a beneficial effect, perhaps through modulating the gut flora.
Epidemiologist!! ??
TMAO “explains” 11% of the variation – is it any wonder that the response of those wish to see convincing data is LMAO.
Dear Paul, My sister and brother have been following you and your wife’s work. I went to your website to read about intermittent fasting and came across your current post on the TMAO from meat paper. You confirmed my immediate reaction to the study concluding consumption of meat was dangerous. I have read a lot about the human biome (Wild Life of Our Bodies and other articles) because of my involvement in the food fermentation movement. (The Art of Fermentation by Sandy Katz). When I saw the article I immediately said: it’s probably a problem because of the wrong mix of microorganisms in peoples guts from a high carb plus meat diet.
Since it’s my one year anniversary of adopting the PHD and part of my story bears on protein consumption, I’ll post this here:
About 4 1/2 years ago, I began a gradual (but methodical and thorough) implementation of the WAPF diet. But I adjusted it to be lower carb, high protein as I thought that would help with weight loss. At a typical meal, I would have only a small portion of carbs and would compensate by doubling the meat. This diet resolved many health issues (obesity, depression, panic attacks, hypertension, dyslipidemia, constant hunger, unrelenting tiredness, hyperhidrosis and night sweats, nocturnal brain fog/slurred speech/uncoordination). But I developed what I THINK is CVS (cyclic vomiting syndrome): reoccurring vomiting (3-4 week interval in my case), at the same time of the day, lasting about 3 hours per occurrence, coupled with sulfurous burping, sulfurous gas and foul diarrhea. In addition to finger joint pain and stiffness (which remains unresolved, but goes away completely if I fast for two days or longer and resumes when I start eating again…seems to correlate with the volume of food eaten rather than any particular food).
Undeterred, I half starved myself over the summer of 2011 to lose the last of my overweight. I did indeed lose it. I also kept vomiting. Hoping to maintain my weight (and having read Taubes’ “Why We Get Fat”), I quit starving myself and went VLC/very high fat and gained 10 pounds in 2 months…and got an eye infection. It was then (April, 2012) that I discovered PHD when trying to troubleshoot low carb/eye infection.
After one year of faithful PHD adherence, the CVS has dramatically lessened. I get the attacks less frequently and when I do, it is usually just nausea and a little diarrhea and little or no vomiting. I attribute this, primarily, to optimizing resistant starch (more) and protein (less). When I read the book, the comment on pg. 77 regarding the pitfalls of too much protein jumped off the page. I was careful from then on to moderate protein. I also try to eat most of my protein at lunch and have most of my carbs at dinner. Protein at night is a CVS trigger…as is egg white, which is difficult for some to digest. I eat three egg yolks/day, but pass on the whites. The carbs at dinner also give me a more restful sleep.
CVS has a psychological component (correlated with anxiety) but I suspect that this anxiety is a symptom of dysbiosis/protein maldigestion, as is the vomiting.
Paul, would you recommend for me to take Betaine HCl at protein containing meals? If so, how much? Any thoughts on supplementing enzymes for protein digestion in my case?
Thanks!
Hi Christopher,
It does sound like a gut dysbiosis with too much of the meat-eating bacteria. Of course meat is almost identical to human tissue, and the vomiting might be a reaction of the body trying to get rid of microbes that are trying to eat your digestive tract. You might consider getting a stool test or other diagnostic testing to see if these microbes are recognizable and treatable.
If you are not properly digesting protein due to a lack of stomach acid, then betaine HCl might help you. It would be a good change to digest protein better and eat less of it. Both would help starve the bad bacteria.
It’s well known that gut dysbiosis can cause anxiety and other “psychological” symptoms, so I would expect everything else to clear up along with the gut issues.
I believe that as we age, our bodies do not make as much enzymes to break down the proteins into amino acids. So the problem of bacteria fermenting proteins is exacerbated by lack of enzymes. I myself take digestive enzymes looking for the one with higher protease activity. Protease is the enzyme that breaks down protein into amino acids.
Hi Paul,
Nice article as always. As I posted over at syontix.com, this appears to be a reaction to certain strains of Clostridia. The fact that broad-spectrum antibiotics made it worse seems to confirm that. I pointed out how previous medical treatment ups the risk of Clostridia infections.
That said, the stupidity of fingering red meat as the sole or major cause of heart disease via this route is mind-numbing. As I tell my readers, when you have gut dysbiosis, damn near anything you eat will cause problems via metabolic endotoxemia. And this also holds true for vegans and vegetarians because I’ve been contacted by a few complaining of gut issues.
Give me a typical American eating the SAD diet who has either: 1) been born by C-section, 2) formula fed as an infant 3) received any amount of antibiotics in the past, 4) consistently eats gut-stopping gluten, 5) has spent anytime in a hospital, 6) binge drinks, 7) smokes and/or 8) suffers from chronic stress, and I can assure you they have some form of gut dysbiosis.
Nevertheless, these researchers would have people believe that if they only cut out or drastically reduced red meat intake then all would be peachy keen with their hearts. All I can say is good luck following that advise because you’ll need it.
what is metabolic endotoxemia? it is one thing that the internet was NOT helpful in defining….
It’s a chronic endotoxemia caused by a bad diet which generates bacterial overgrowth in the small intestine. It’s discussed in the book and Pubmed has 460 papers: http://www.ncbi.nlm.nih.gov/pubmed/?term=metabolic+endotoxemia. Papers by Cani PD are especially relevant, eg: http://www.ncbi.nlm.nih.gov/pubmed/17456850 and this recent review: http://www.ncbi.nlm.nih.gov/pubmed/22572877.
Here is Wikipedia: http://en.wikipedia.org/wiki/Endotoxin
What are your thoughts on the latest “lead in rice” scare?
http://healthland.time.com/2013/04/11/high-levels-of-lead-found-in-imported-rice/
Lead is an environmental contaminant so the key is to choose rice from unpolluted locations. Unfortunately Asia is becoming increasingly polluted.
I take it as one more reason to get starches from a diversity of sources, not rice only.
http://www.alphagalileo.org/ViewItem.aspx?ItemId=130204&CultureCode=en
A study embargoed until today is in contradiction to the much publicized study.
Hi David,
Sorry, the link isn’t working for me.
the link just worked ok for me
OK, now it works for me too. Funnily enough I tweeted that paper earlier today.
It’s no surprise because carnitine is a useful nutrient. Heart tissue dies in a heart attack from lack of ATP, and carnitine helps support ATP production, so it’s not surprising it helps.
It doesn’t contradict the other study, except superficially. The other study was about elevated TMAO levels causing atherosclerosis, which is very different than carnitine intake protecting tissue. As I noted in this post, elevated TMAO has little to do with how much carnitine you eat and much to do with what kind of gut flora you have, ie how much sugar etc you eat.
Hi Dr. Paul Jaminet,
Can you give some critique to this study? Thank you.
http://www.foodconsumer.org/newsite/Nutrition/Diet/saturated_fat_insulin_resistance_0313131114.html
Hi Alex,
It’s this study, from 1997: http://www.ncbi.nlm.nih.gov/pubmed/9112020.
High carb diets lead to high insulin sensitivity and therefore low fasting glucose and low fasting insulin. High fat/low-carb diets lead to low insulin sensitivity and therefore high fasting glucose and high fasting insulin. All this is well known, and commonly experienced by low-carb Paleo dieters. It is a long leap from that observation to any conclusions about our optimal diet.
Now I am confused. Isn’t low insulin sensitivity bad? Isn’t PHD for high fat and low carb? I have not been following you closely recently. Have you changed your opinion and now advocates for low fat and high carb?
Hi Alex,
Normal insulin sensitivity is best, either too much sensitivity or too little is bad. PHD is about 30% carb 15% protein and 55% fat. It is neither high carb nor low carb. It is lower carb than the standard American diet, but still has sufficient carbs to avoid insulin resistance.
You want your cells to be insulin sensitive. You do not want your cells to be insulin resistant. The terms “high” and “low” are relative terms. I think you have to find the right amount of carbs for your particular individual body. For some people (especially those with abdominal adipose tissue), eating too many carbs for their particular body leads to insulin resistance. But for other people (especially very thin people without any body fat) eating too little carbs for their particular body also leads to insulin resistant (although for a different reason).
Same with blood sugar levels. Eating too much carbs and eating too little carb both can cause high blood sugar. What is “too much” and what is “too little” varies greatly from individual to individual.
Granted, most of the population in the world is probably consuming too much carbs. But some few people (perhaps in the low-carb and paleo community) are probably consuming too few carbs.
“You want your cells to be insulin sensitive. You do not want your cells to be insulin resistant. ”
Most of the time . . . I’m sure we can come up with scenarios a cell needs to be insulin resistant.
Our modern diet has too much simple carbs. We need a drastic change to get more complex carbohydrate into our daily diet.
K
What does normal insulin sensitivity feel like? My body is messed up. I don’t know what things like that are supposed to feel like anymore.
This study irked me more than similar studies usually irk me. I try to think the best of scientists, and I realize that often they make very limited, specific statements of their findings, and irresponsible media persons blow those statements out of all proportion.
But I think in this case, the very design of the experiments and research suggest deliberate misdirection – not outright deception, in that I’m sure that they reported their results truthfully, but something almost as bad.
The authors were very clever in demonstrating that the gut bacteria of carnivores and vegans process carnitine differently – even given their tiny sample size, that looks credible. I think they did an okay job of showing a correlation between elevated TMAO levels and CHD, too – not a particularly strong correlation, but whatever – statistically significant, anyway.
They (kind of) proved thesis “A” – that steak raises TMAO when a carnivore eats it, and doesn’t when a vegetarian eats it. They gave some supporting evidence for thesis “B” – that elevated TMAO might cause CHD. But they were absolutely silent about any *other* factors that might elevate TMAO, besides beef.
As Masterjohn’s thorough takedown makes clear, even if we accept their “proof” of hypotheses A and B as 100% iron-clad, you can only get to their conclusion “C” (beef causes heart disease) by completely ignoring the question of magnitude of effect.
Imagine a study about cardiovascular exercise.
One could demonstrate rigorously, in a lab with a treadmill and volunteers breathing into tubes, that physical exertion increases a human’s output of CO2, in a statistically significant and predictable amount. One could also demonstrate with existing climatology research that increased CO2 in the atmosphere correlates with rising global temperatures.
Has one then “shown” that physical exercise causes global warming?
Hi Bob,
Good analogies.
I think it is a ubiquitous problem in modern science — researchers are focused on getting grants and publications, rather than on discovering truths, much less useful truths. A false but interesting story, which would be important if true, is much easier to generate than an important and novel truth.
An interesting take on fermenting protein, but that then raises another question.
What about fermented protein foods, like cheese, and fermented (raw) meats?
Both of these have a long history of human consumption, and the widespread existence of fermented meat dishes in traditional diets suggests they are beneficial.
Granted, they are fermented under different conditions (and outside the body), so maybe the type of bacteria doing the fermenting makes a difference?
Hi Paul,
I think there are a number of reasons why fermented dairy is safer than fermented meat or fish:
1) Antimicrobial compounds and oligosaccharides designed to promote probiotic species create a better mix of flora. Thus, yogurt and cheese species closely resemble the bacterial species in infant guts.
2) Dairy is acellular and lacks most of the compounds in cells that might be fermentation risks.
I think fermented meat dishes are much riskier.
Hi Paul, I wasnt sure where to post this. I seem to have problems eating fish such as well as meats. I suspect it could be due to histamine. Have you written about histamine intolerance? I’m having trouble finding any articles on it.
Many thanks!
I have to ask why is it that the carnitine isn’t fully absorbed in the small intestine? Based on the graph it appears that tmao only rises once reaching the colon (it usually takes 8-12 hrs for food to reach the colon). Could the antibiotics actually have improved the absorption of carnitine? The chart shows a slower rise in d3-carnitine when on antibiotics. Did they state which antibiotics were taken by the way?
regarding fermentation of meat in the gut, doesn’t this suggest a chloride and vitamin k deficiency?
what about the manner in which meat is cooked and the sourcing? are grain fed high omega 6 beef sources, which are the most commonly consumed and most inflammatory more of a risk than properly cooked (low temperature/rare) grass fed beef?
please consider the following statement:
“Meat contains complex polysaccharides, e.g. glycosaminoglycans, such as chondroitin sulfate and heparan sulfate proteoglycans, which are bacterial fodder equivalent to soluble fiber.”
( http://coolinginflammation.blogspot.com/2012/06/dr-oz-on-gut-flora-repair.html )
now if the meat consumed was grain fed beef, already higher in omega 6 than desired, fed hormones and anti-biotics and cooked at high temperatures, thereby making it deficient in polysaccharides and thereby more difficult to digest lead to a higher probability of bad fermentation? not all red meat is the same, wouldn’t you agree?
Well here is the latest, Latest Red Meat Scare.
http://news.yahoo.com/gut-bugs-implicated-heart-attacks-stroke-210106749.html
Keep in mind as Anthony Colpo pointed out, Hazen, the leading Cleveland Clinic researcher on the study, has patents for this TMAO testing.
None the less, I thought all the take downs of the carnitine study didn’t address the point that if one has a certain gut bacteria, endogenous levels of TMAO will soar and Hazen now has established a correlation to event risk.
Interesting, they no longer focus on carnitine but implicate other nutrients. Of course they hint at lowering TMAO levels with a drug instead of identifying and changing gut microbiata in question. Good researcher now, sit boy, roll over, bark.
Not to mention, there’s still no evidence of high TMAO being a CAUSE of heart disease. Without such evidence, TMAO-lowering drugs would be as dumb as recalibrating speedometers to prevent speeding.
Which isn’t to say it won’t happen anyway, a la statins.
here is the NY times write up
http://www.nytimes.com/2013/04/25/health/eggs-too-may-provoke-bacteria-to-raise-heart-risk.html?_r=0
Hi Paul and everyone!
Any thoughts on cholesterol sulfate? It seems quite interesting and terribly important.
Cheers,
Sakari
Hi Sakari,
Well, Stephanie Seneff thinks so, and it’s an interesting hypothesis, but there’s very little supporting evidence in Pubmed. I would say the jury is out on the importance of sulfur/sulfate. Ingesting too much sulfur promote some harmful gut bacteria and generates toxic compounds like hydrogen sulfide, so if sulfur is beneficial it’s not clear how to get it — breathing it? Transdermally?
I have been on PHD for 4 months and feeling great. I have lost 16 pounds and have really begun to take control of my health. As part of that I had a blood test done recently and my LDL is at 143. My doctor ordered a coronary calcium score CT which I did and the score was a 79 which puts me in the 94 percentile for my age (45 yrs old). My first ever visit with a cardiologist was very demoralizing. He told me to eliminate eggs, coconut oil, red meat, butter, and told me to get on the south beach diet. I told him about PHD and he scoffed. He pulled up an October 22 meta data study on red meat which shows a 23 percent increases in mortality from red meat. He laughed at me when I told him that I heard that saturated fat was not the enemy, but PUFAs and cereal grains and sugar. I’m not sure what to do? Have you seen this study? Red Meat and Processed Meat Consumption and All-Cause Mortality: A Meta-Analysis.
i seem to recall that while someone is losing body fat, cholesterol numbers will be affected (negatively i assume?).
& you only get a ‘true picture’ once the weight/fat loss has stopped/plateaued for a few weeks.
may be something worth looking in to if you are still dropping body fat.
Hi Chris,
We’ve looked several times at those studies. First, they get bad numbers by grouping processed meats with natural red meats — the processed meats are much worse, red meats are never found to have significant associations by themselves. (Including in the study you cited, http://aje.oxfordjournals.org/content/early/2013/10/21/aje.kwt261.short?rss=1) Secondly, there are confounding factors in that people who eat a lot of red meat are people who don’t respect authorities and don’t care about their health — they smoke, don’t exercise, stay up late, etc — and it is hard to correct in these associational studies for confounders. Basically epidemiology gives us no reason to reject red meat. Third, the red meat category includes pork as well as beef and pork has worse performance than beef, it is associated with liver disease and metabolic syndrome, we’ve discussed this, search on the trouble with pork. Overall beef and lamb come out very well.
Re your numbers, coronary calcium develops over decades and is not reversed quickly. So your calcium score is indicative of what you were doing before PHD, not in the last four months. LDL of 143 is a bit higher than I would like, 130 is a good number, but 143 is only the 33rd percentile or so in the Framingham Study so that puts you with a lot of company. It is by most standards in the “normal range” of LDL. You might read our “high LDL on Paleo” to see some nutritional reasons why LDL might be too high. Lack of iodine supplementation, being too low carb, and being low in zinc or copper are primary reasons.
The cardiologists advice to eliminate eggs, coconut oil, red meat, and butter is exactly wrong.
The other things to focus on are vitamin D optimization, eating liver, and vitamin K2 supplementation (or eating fermented foods and aged cheese).
Finally, circadian rhythm entrainment is important for vascular health. See chapter 42 of our book.
The fact that you are feeling great and have lost 16 pounds indicate you are doing most things right. A few minor tweaks, and your next coronary calcium score will probably show regression.
Best, Paul
@Chris
Okay – what will you do if you get retested in 4-6 months and there is little improvement?
If your LDL-C is 143 and your Calcium Score is 79 you have some problems which need to be dealt with.
1) What are you currently eating? What does an average day look like?
2) Appx what % of your totaol calories are saturated fat?
Thanks Charles. I’m hoping that continuing on PHD will help me. I’m guessing my recent blood tea would have been much worse 4 months ago.
My typical day is fast until 11am then eat 3 eggs with butter veges and cheese. Lunch is typically either a salad with chicken or rice bowl with veges sautéed in cocunut oil and leftover meat, or bone broth soup with rice and leftover meat. Dinner is either rice or baked potato and butter, meat or fish, and salad. Salad dressing is almost always olive oil and red wine vinegar. Dark chocolate after dinner. I eat red meat about 4-5 times a week 1/2 to 1 pound. I drink coke zero and sometimes have cremmys sugar free and gluten free ice cream
Hi Chris,
You are eating quite well. The drinks could be improved — try flavoring water with vitamin C powder, lemon juice, or vinegar, and coffee or tea. Ice cream is fine in moderation. You might try to work more collagen into your diet by making soups and stews with joint material.
1) Drop the coke zero and the cremmys sugar free and gluten free ice cream.
2) I would consider cutting out the coconut oil and the cheese as well.
3) ANY history of heart disease in the family – in your direct blood lines?
No history of heart disease. Just personal history of eating lots of sugary foods and grains.
Thank you for your recommendation. Did anyone read the October meta study on red meat?
1) What is your non HDL-C? (TC-HDL)
2) Have you had your ApoB measured? This is a surrogate for LDL-P
Total HDL is 45 mg/dL. HDL-2 is 11mg/DL, HDL 3 is 34 mg. total cholesterol is 208 mg. triglycerides are 76 mg/dL. Non HDL C is 163 mg/dL. Remnant lipoprotein is 35 mg/dL ( the cardiologist said this is not good). I’m getting a full NMR in 2 months. LDL is pattern A. APOB100 calculated is 107 mg/dL
Hi Chris,
It’s hard to interpret these numbers without an earlier test to compare them to. Aside from LDL and remnants this is better than the average population. It has probably improved significantly from before.
Overweight people, which you were, commonly have high LDL because metabolic endotoxemia causes both obesity and high LDL. It’s possible that your LDL was higher earlier but remains high due to a persistent small intestinal bacterial overgrowth.
To treat that, you want to improve mucosal immunity by optimizing vitamin D, eating vitamin A rich foods (liver is essential, also colorful plants like spinach, sweet potatoes, and persimmons), and improve gut barrier integrity by eating collagen and supplementing vitamin C.
Chris, I think you are doing well, just tweak nutrition a bit, get daily exercise, tend to circadian rhythms, and all will be well. Health improvements come quickly but perfect health takes time. You are on your way.
“Aside from LDL and remnants”
Aren’t these really important?
Question – if these markers do not improve significantly in the next few months what would you then suggest he do?
http://www.lecturepad.org/dayspring/lipidaholics/pdf/LipidaholicsCase291.pdf
“”Let’s get rid of the nonsense seen all over the internet that atherosclerosis is an inflammatory disease, not a cholesterol disease. That is baloney-with the reality being that it is both. One cannot have atherosclerosis without sterols, predominantly cholesterol being in the artery wall: No cholesterol in arteries – no atherosclerosis. Plenty of folks have no systemic vascular inflammation and have atherosclerotic plaque. However clinicians have no test that measures cholesterol within the plaque – it is measured in the plasma. It is assumed, that if total or LDL-C or non-HDL-C levels are elevated the odds are good that some of that cholesterol will find its way into the arteries, and for sure there, are many studies correlating those measurements with CHD risk. Yet, we have lots of patients with very low TC and LDL-C who get horrific atherosclerosis. We now recognize that the cholesterol usually gains arterial entry as a passenger inside of an apoB-containing lipoprotein (the vast majority of which are LDLs) and the primary factor driving LDL entry into the artery is particle number (LDL-P), not particle cholesterol content (LDL-C). Because the core lipid content of each and every LDL differs (how many cholesterol molecules it traffics) it takes different numbers of LDLs to traffic a given number of cholesterol molecules: the more depleted an LDL is of cholesterol, the more particles (LDL-P) it will take to carry a given cholesterol mass (LDL-C). The usual causes of cholesterol depleted particles are that the particles are small or they are TG-rich and thus have less room to carry cholesterol molecules. Who has small LDLs or TG-rich LDL’s? – insulin resistant patients! After particle number endothelial integrity is certainly related to atherogenic particle entry: inflamed endothelia
have inter-cellular gaps and express receptors that facilitate
apoB-particle entry. So the worse scenario is to have both high apoB and an inflamed dysfunctional endothelium. Is it better to have no inflammation in the endothelium – of course! But make no mistake the driving force of atherogenesis is entry of apoB particles and that force is driven primarily by particle number not arterial wall inflammation: please see Ira Tabas, Kevin Jon Williams, Jan Borén. Subendothelial Lipoprotein Retention as the Initiating Process in Atherosclerosis
Update and Therapeutic Implications Circulation. 2007;116:1832-44.”
http://www.nobelprize.org/nobel_prizes/medicine/laureates/1985/brown-goldstein-lecture.pdf
Nobel lecture, 9 December, 1985
by
MICHAEL S. BROWN AND JOSEPH L. GOLDSTEIN
Department of Molecular Genetics,
University of Texas Health Science
Center, Southwestern Medical School, 5323 Harry Hines Blvd. Dallas, Texas,
U.S.A.
“The LDL receptor studies lend experimental support to the epidemiologists’ suggestion that the levels of plasma cholesterol usually seen’ in Western industrialized societies are inappropriately high (9). This support derives from knowledge of the affinity of the LDL receptor for LDL. The receptor binds LDL optimally when the lipoprotein is present at a cholesterol concentration of 2.5 mg/dl (28). In view of the 10 to 1 gradient between concentrations of LDL in plasma and interstitial fluid, a level of LDL-cholesterol in plasma of 25 mg/dl would be sufficient to nourish body cells with cholesterol (118). This is roughly one-fifth of the level usually seen in Western societies (Fig. 16 and ref.119). Several lines of evidence suggest that plasma levels of LDL-cholesterol in the range of 25-60 mg/dl (total plasma cholesterol of 110 to 150 mg/dl) might indeed be physiologic for human beings. First, in other mammalian species that do not develop atherosclerosis, the plasma LDL-cholesterol level is generally less than 80 mg/dl (Fig. 16 and ref. 120). In these animals the affinity of the LDL receptor for their own LDL is roughly the same as the affinity of the human LDL receptor for human LDL, implying that these species are designed by evolution to have similar plasma LDL levels (9,119). Second, the LDL level in newborn humans is approximately 30 mg/dl (121), well within the range that seems to be appropriate for receptor binding (Fig.16). Third, when humans are raised on a low fat diet, the plasma LDL-cholesterol tends to stay in the range of 50 to 80 mg/dl. It only reaches levels above 100 mg/dl in individuals who consume a diet rich in saturated animal fats and cholesterol that is customarily ingested in Western societies (116)”
“Once LDL receptors become saturated, the removal rate of LDL is proportional to the number of receptors. Whenever the number of receptors is reduced, plasma LDL levels must rise. Experiments in animals indicate that the consumption of a high fat diet decreases the number of LDL receptors in the liver (123, 124). We believe that this mechanism operates through feedback suppression as described above. That is, when excess dietary cholesterol accumulates in the liver, the liver responds by decreasing the production of LDL receptors (Fig. 13C). The entry of dietary cholesterol into the liver is mediated by a receptor, termed the chylomicron remnant receptor, whose activity is genetically distinct from the LDL receptor (125). The chylomicron remnant receptor is unaffected by cholesterol accumulation (126), and it causes cholesterol to accumulate to high levels in liver when the diet contains excess fat. The combination of saturation and suppression of hepatic LDL receptors contributes in a major way to the buildup of LDL in plasma when a diet rich in saturated fats and cholesterol is ingested. Insofar as such a diet also may increase production of LDL in the face of a fixed or declining removal capacity, the LDL level would rise even higher If the LDL receptor does limit the removal of LDL from plasma, then maneuvers that increase LDL receptor activity might be effective in individuals who have high plasma LDL-cholesterol levels, but who do not have defective LDL receptor genes. Such therapy seems feasible with the development of HMG CoA reductase inhibitors. However, it is still too early to tell whether such therapy would decrease the incidence of myocardial infarctions in individuals with moderately elevated plasma LDL-cholesterol levels in the range of 100 to 200 mg/dl. There is much circumstantial evidence to expect such improvement (127), but unequivocal data are simply not there. Hopefully, with the availability of powerful receptor-stimulating drugs, the hypothesis should be susceptible to testing in the near future. In considering the role of diet and drugs in treatment of high cholesterol levels, physicians and public health authorities must bear in mind the genetic variability between individuals. This variability exists at three levels: 1) The degree of increase in plasma cholesterol upon ingestion of a high cholesterol diet is variable. Not all people develop hypercholesterolemia. Some people, such as the Pima Indians, maintain low plasma cholesterol levels despite ingestion of a high fat diet (10). 2) Even when the plasma cholesterol level becomes elevated, the propensity for atherosclerosis varies. For example, a substantial proportion of FH heterozygotes (10 to 20%) escape myocardial infarction until the 8th or 9th decade despite pronounced hypercholesterolemia from birth (14). 3) Genetic susceptibility to contributory risk factors is variable. Some people can withstand hypertension and cigarette smoking for decades without developing atherosclerotic complications; others are highly sensitive.”
Paul – what are your thoughts on this?
Charles,
Yes, LDL and lipoproteins are important.
But what do they indicate? We have extensive experience with lipoproteins and serum cholesterol on our diet. Nearly everyone experiences improvements and their numbers migrate toward optimal. In some people bad LDL numbers are persistent, but in these people other health problems — chronic infections and disorders they cause like diabetes — are also persistent. Both the disorders and the LDL numbers seem to improve slowly with time, and together.
The logical inference is that our diet is excellent, indeed optimal, and that the few cases of persistent bad biomarkers reflect an uncured underlying health disorder, usually chronic infections.
What should be done is to continue with the healthful diet and lifestyle and to place greater emphasis on immune-enhancing lifestyle tactics like intermittent fasting, circadian rhythm entrainment, nourishment with vitamins D, A, C, zinc, and iodine, etc. And pushing doctors to diagnose and treat the underlying conditions, if possible.
When you suggest changing diets, you are advising people to begin a wild goose choose. Other diets are likely to make any underlying disorders worse, not better. Cardiologists’ diet advice doesn’t work, that’s why they rely on statins to lower cholesterol.
In Chris’s case, we don’t even have any previous tests to tell us that there is even any cause for concern about his current diet or lifestyle, which were only recently adopted. It is very possible that every number, including LDL and coronary calcium and lipoprotein remnants, has improved over the last four months. Since he says he’s feeling better and weight loss is typically associated with improvements in these numbers, that’s the way to bet. If his diet is faulty, it’s probably fixable with minor tweaks, eg slightly more carbs, iodine, zinc, copper, collagen, and vitamins A, D, K2, and C.
“it is very possible that every number, including LDL and coronary calcium and lipoprotein remnants, has improved over the last four months.”
Do you have any studies which indicate that the type of diet that you recommend can lower coronary/stabilize coronary calcium?
I was under the impression that only a combination of a low fat diet + statins (in certain cases) can do this.
I’m referring to Caldwell B. Esselstyn, Jr. and his work.
http://www.heartattackproof.com/articles.htm
Also Dr Dean Ornish and his work
We’ll generate them. The vegetarian advocates have had a 40 year head start on creating studies. The record of their diets is quite poor. Ours will do better.
Another good thing to do with sibo is wait at least 4 hours between meals to allow the ‘cleansing wave’ or ‘migrating motor complex’ to try to clean out the bacteria in the small intestine.
Ornish and Esselstyn have clinical data to back up their claims. All you can say is that you’ll generate the proof!
Suppose you can’t?
Also – don’t you think Chris should have acomplete thyroid panel done?
We’ll have higher quality data than they have in a year. Look at Esselstyn’s data in your link — 18 people selected from a clinical practice of much larger numbers. What a weak paper. Furthermore his diet made every one of them lipid deficient, with certain negative health effects.
Whereas, we have hundreds of accounts of lipid changes on PHD and they essentially all move in a positive direction. We’ve similarly been getting before and after labs from participants at the Perfect Health Retreats. The Retreat participants will give us a clear look. Unlike Esselstyn’s sample selected from a much larger group (and surely biased), our Retreats data will be unbiased — we’ll have everyone who cooperates, which so far has been all but one.
Yes, I do think Chris should have his thyroid status looked into. But, he feels better, so his thyroid status is probably improving.
Hi Paul,
I’m curious what you are using as a criteria for lipid success?
The PHD recommended lipids wouldn’t currently be considered healthy in the mainstream. There also doesn’t even seem to be agreement within the ancestral community. There just doesn’t seem to be enough evidence.
Thanks,
Mark
Non HDL-C = 163 is VERY VERY HIGH
Remnant lipoprotein @ 32 is VERY DANGEROUS (your cardiologist is correct)
A full NMR test is not necessary.
If I were you I might consider major changes to your diet and possible use of low dose statins.
I’m sticking with PHD. It is definitely helping I think. I don’t not think the kind of diet my cardiologist is recommending is sustainable for the long haul. I have been supplementing iodine, vitamin c, magnesium, k2, and d3 for the past 2 months. I will also incorporate more bone and joint broths, vitamin a rich foods like liver, cut out the coke zero and replace with water. I have been exercising with a fantastic trainer 3 times a week who does not overdo it and I have been doing moderate bike riding cardio 5 times a week. I am going to incorporate and reread the section on circadian rhythm entrainment. I will keep posting my results as they come in.
Hi Paul,
Might you be able to comment on the following study: http://archinte.jamanetwork.com/article.aspx?articleid=1134845
It finds a correlation between red meat intake and mortality among over 100,000 observed participants – although it relies on food questionnaires for data collection, so the results may not be completely reliable.
Thanks!
Jordan
I found your reaction here: http://perfecthealthdiet.com/2012/03/red-meat-and-white-rice-oh-my/. Thanks.
Hi Jordan,
There are problems with processed meats and undercooked pork, which I’ve discussed on the blog – search the Trouble with Pork. Beef and lamb are beneficial and appear that way in studies that isolate them from pork and processed meats.
Bravooooo…. You happy marriage and family. This the first site where I have consider to the best….
We are all going crazy about Prevotella related to RA,ATHROSCLEROSIS,VIH, INFLAMMATIONS and other diseases.
Lcarnitine in the presence of PUFAs in whole grain becomes toxic. These “essential fatty acids” are highly unstable and cause oxidative stress easily because they UNSATURATED thus producing TAMOs as a systemic inflammatory factor.
Prevotella is just running the show.
Grains….grains….again causing damage and suffering.
i love whole grains, but I was born again when I got rid of them, I had RA,ATHROESCLEROSIS and CIRROSIS chronic symptoms and it took me years and pain to open my eyes and admit that my loved grains were the culprit
I suspect that fruits and vegetables lead to a beneficial Prevotella.
Thanks for the work that you are doing for all humans…..
Best wishes for you all….
Tito