In Part 1, we found that taking vitamin C after orthopedic surgery is a good idea, and that vitamin C could help in other surgical situations as well. But that’s only half the story. Here’s the other half.
Vitamin C as a prooxidant?
The world of vitamin C was tipped upside down in 1998, with the publication of a controversial paper in the prestigous journal Nature entitled “Vitamin C exhibits pro-oxidant properties”. News media was all over it, predictably warning readers to be afraid…very afraid of taking vitamin C supplements. But the paper had a lot of holes, to put it mildly.
The study showed that some DNA was oxidized by vitamin C, but some DNA was also protected from oxidation by vitamin C (with the protection being around ten times greater in magnitude! A fact that was conveniently left out of the paper.). Plus the experimental technique may have oxidized some DNA by itself. So what happens when throngs of angry vitamin C supporters wrote in to the journal? The primary author backtracked, and his reply concluded “our study shows an overall profound protective effect of this vitamin.” Case closed. Or is it?
IRONing out the details…
Vitamin C is neither always an anti-oxidant or always a pro-oxidant, and not all studies are applicable to what goes on in your body. Take lab mice for example. Unlike humans, mice can synthesize vitamin C, and supplementation can paradoxically reduce their vitamin C levels. In humans, study results are mixed, with most showing either an anti-oxidant effect or no effect, and some showing both anti and pro-oxidant effects. Timing could also be an issue. In a study where vitamin C was added before LDL was experimentally oxidized, it displayed antioxidant properties. But vitamin C actually showed prooxidant properties when added AFTER the LDL was mildly oxidized. So what does this mean for surgery?
First things first: if you have iron overload (for example, due to hereditary haemochromatosis), be careful with high doses of vitamin C, especially during times of surgery. Unbound iron can interact with vitamin C to produce oxidative stress. Iron is typically bound to transfer proteins and largely safe from vitamin C, but a portion of iron stores may be released when tissue is injured and blood vessels are compromised. And when is a large mass of tissue injured? Surgery!
For people without iron overload, the implications of iron and vitamin C interactions are not so clear. There doesn’t seem to be much data about the interaction of vitamin C and iron during the surgical and post-surgical period. In vitro and trial evidence conflicts on whether vitamin C protects or chemically reduces (i.e. harms) iron in humans, and evidence is also mixed on whether vitamin C protects or occasionally causes protein glycation. Vitamin C can have differing effects on oxidation of depending on the target (lipids, proteins, or DNA) as well.
So the takeaway here may simply be: avoid taking supplements that contain iron and too many iron-enriched foods around surgery time (unless you are advised to by your doctor), and don’t go much beyond the PHD-recommended vitamin C intake. If you have a crappy diet and think vitamin C will save you, be careful. Overloading on vitamin C after tissue components are already oxidized could theoretically lead to further oxidation.
Crohn’s and Ulcerative Colitis
Crohn’s and ulcerative colitis patients often take vitamin C in combination with iron for anemia. That might be a bad idea, as high doses of iron worsen symptoms in Crohn’s patients. Even a single high dose of iron can cause intestinal lining oxidative damage in healthy individuals, and supplementing with quite small amounts of vitamin C and iron together leads to oxidative damage. Iron-enriched diets increase colon cancer in mice and injected vitamin C combined with iron causes ulcers in rats.
The combination of vitamin C, certain metals, and hydrogen peroxide makes up a free-radical generating process called the “Udenfriend system”. Diseased tissue, such as the intestinal tissue in bowel disorders, may contain higher levels of these components. While some in vitro studies show that the Udenfriend system is NOT your friend, others show that it doesn’t cause lipid or protein oxidation in vivo. Without a conclusive answer, it might be prudent to avoid going overboard with vitamin C and iron if you have Crohn’s or UC, especially around surgery.
Other surgeries
There are many different surgeries for many different conditions, and vitamin C hasn’t been studied for most specific examples. One type of surgery that there is evidence for is vascular surgery. In a randomized trial of vascular surgery patients, 2 grams of prophylactic vitamin C was tested for the purpose of decreasing inflammation and tissue damage. It ended up actually increasing oxidative lipid damage, which can lead to further vascular damage. Cardiac surgery can cause tissue injury when blood supply returns after a period of low oxygen. And guess what else happens when blood returns? Extra iron is released from storage, and this iron can theoretically be reduced (damaged) by vitamin C.
Conversely, vitamin C has shown promise for other surgeries. In a study of GI surgery, post-surgical oxidative stress was reduced by taking 500 mg/d of IV vitamin C. Note that IV vitamin C can lead to more than six times higher blood levels than oral intake. Since vitamin C is consumed at high rates during some surgeries, this effect seems logical, and certain patients may be very low in vitamin C before surgery and hence really need a vitamin C boost. Most often, studies combine a few antioxidants rather than testing just one, which makes singling out the effect of vitamin C difficult.
Physical therapy
In some surgeries (e.g. orthopedic surgery), surgery is only the beginning of the treatment. The rest of the treatment comes in the form of grueling, sometimes scream-inducing physical therapy that can last for weeks or months. Since muscles atrophy if a body part isn’t used much before surgery, the post-surgical period is important for muscle growth.
While vitamin C is important for joint healing, there is a small amount of evidence that vitamin C supplementation can interfere with muscle growth. And physical therapy is a combination of growing muscle, healing joints, and re-training the nervous system.
Reactive oxygen species (ROS) are not universally bad, and one of their important functions is to signal the body to increase protein synthesis as part of the mTOR pathway. Vitamin C in extremely large doses inhibits muscle growth (in rats) by quenching not just bad ROS, but helpful ROS as well. In humans the effect is uncertain, as the impact of supplemental vitamin C varies widely by study. Given the importance of vitamin C in wound healing and collagen formation, it’s likely unwise to avoid vitamin C in the post-surgical period. The takeaway may be to avoid massively overloading on antioxidants in general — large amounts of antioxidants other than vitamin C may impair muscle adaptation to exercise. And taking vitamin C to bowel tolerance directly after physical therapy may be both uncomfortable and unwise.
Conclusion
A healthy diet should support the entire endogenous oxidative system, as antioxidants often work together. So as usual, focus on getting a balance of nutrients from your diet, especially before and after surgery when nutrition is critical for healing tissue.
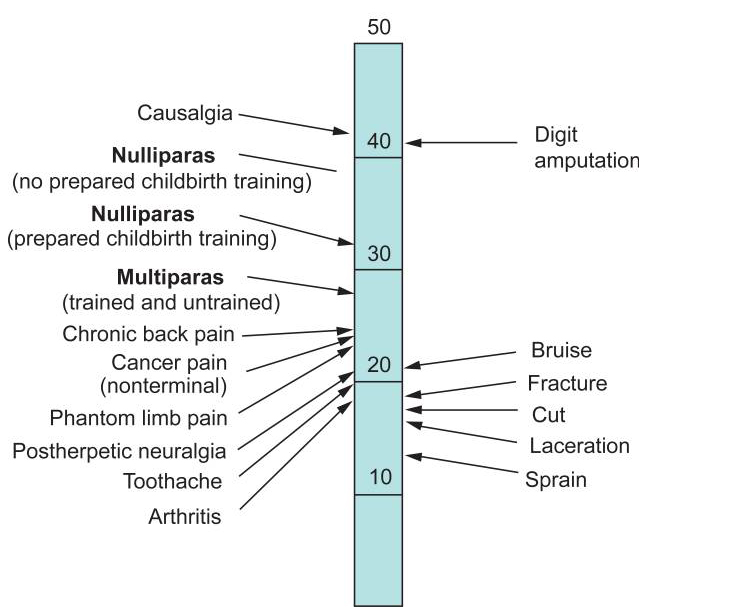
Vitamin C intake should be at least 500 mg/d after surgery in order to avoid the terrible pain condition RSD/CRPS. Moderate doses of vitamin C typically show benefit for oxidation, and are likely helpful before and after surgery. Only very high doses over extended periods or extremely high IV doses have been linked to adverse events like renal failure, and vitamin C studies typically only show prooxidative effects when combined with iron supplementation or in higher doses.














Recent Comments