Obesity seems to have the same cause the world over, in both humans and lab animals: It results from food toxicity compounded by malnourishment.
The most important food toxins are cereal grains (especially wheat), omega-6-rich vegetable oils, and fructose from sugar and corn syrup.
The United States government in its wisdom chose to give agricultural subsidies to wheat, corn, and soybeans, thus reducing the price of the most toxic food crops. The natural result was to make Americans the fattest people in the world, as this chart comparing body-mass index (BMI) in 30 countries attests (from http://diabetescure101.com/BMI.htm, via Matthew Yglesias):
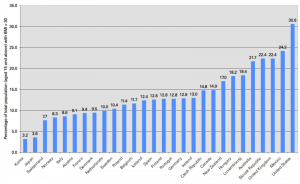
Look at the two low-obesity countries at the left of the chart: Japan and Korea are the only two Asian countries in the sample. What are they doing right?
Well, everything:
- Their staple starch is rice, not wheat. Rice is the only non-toxic cereal grain and one of our “safe starches.”
- They consume far less vegetable oils than Americans.
- They consume far less sugar than Americans.
With a minimally toxic diet, it’s almost impossible to become obese.
Of the three main toxins, which is the most important single factor in causing obesity?
An interesting place to look for an answer is the China Study. Since some regions of China traditionally eat wheat and others rice, the China Study is especially effective at distinguishing the obesity-promoting effects of wheat toxins. The China Study compiled massive epidemiological data by region, including correlations between wheat and rice consumption and body weight and body-mass index (BMI).
Denise Minger, who is fast making herself the world’s leading interpreter of the China Study, has continued her analysis of the raw data. Denise points out that in China, wheat eaters are “fatter with fewer calories”:
In both China Study I and II, wheat is the strongest positive predictor of body weight (r = 0.65, p<0.001) out of any diet variable. And it’s not just because wheat eaters are taller, either, because wheat consumption also strongly correlates with body mass index (r = 0.58, p<0.001).
Here is the data in pictures:
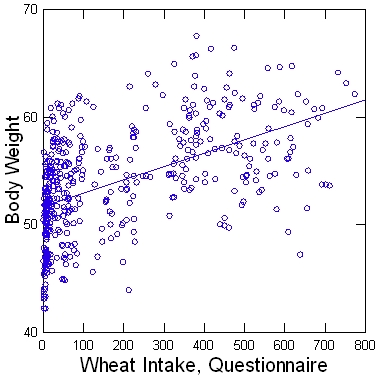
Denise goes on to point out that the correlation of BMI with wheat intake is 56%, with calorie intake only 13%.
It seems the evidence is consistent. It’s not eating more calories that makes a person fat. It’s overdosing on toxins – especially wheat toxins.











Recent Comments