The gut is the front line of health. The human gut houses 100 trillion bacteria from a thousand different species [1]; they weigh several pounds and make up about half the dry weight of stool. To control these bacteria 70% to 80% of the body’s immune cells are normally found in and around the gut.
A healthy gut is protected by a mucosal layer that is designed to promote commensal (friendly) bacteria, while providing a barrier to pathogenic bacteria. Humans have evolved ways to “feed” commensal species of bacteria. For instance:
- Human mucus is made of glycoproteins, or compounds made of protein and sugar. Certain probiotic bacteria, such as Bifidobacterium bifidum, are able to digest human mucus. [2] Thus, the human intestine has evolved to produce “food” for beneficial gut bacteria, assuring that they are maintained even during long fasts.
- Mother’s milk contains special sugars, called human milk oligosaccharides, which specifically feed Bifidobacterium bifidum and assure that this species successfully colonizes the baby’s intestine and wards off infection. [3]
The absence of this protective barrier of mucus and friendly bacteria makes the intestine extremely vulnerable to infectious disease. Premature babies who are fed formula, not human breast milk, often contract a dangerous intestinal infection, necrotizing enterocolitis. [3]
In addition to pathogenic bacteria, the gut is confronted by a heavy load of toxins. Bruce Ames and Lois Gold have estimated that the average person eats 5,000 to 10,000 different plant toxins, amassing to 1500 mg per day, plus 2000 mg of burnt toxins generated during cooking. [4]
Today’s post will focus on how those 1500 mg of natural plant toxins damage the intestinal wall and its mucosal barrier, thereby bringing about infectious bowel diseases.
Cereal Grain Toxicity
Grasses became the staple foods of agriculture because of their rich yields: a single plant may generate tens of thousands of seeds annually.
Yet this prolific seed production has always made grasses attractive to herbivores, and caused seeds to evolve high levels of toxins designed to poison mammalian digestive tracts, thus enabling their seeds to pass through herbivore guts undigested. It is these toxins that make the cereal grains so dangerous to human health.
The effectiveness of grain toxins at sabotaging human digestion is illustrated by the increase in fecal mass they produce:
For every gram of wheat bran eaten, fecal weight increases by 5.7 grams. [5]
By inhibiting human digestion, wheat toxins dramatically increase the amount of undigested starch reaching the colon. This increased food supply substantially increases the bacterial population – and the presence of starch, which is ordinarily unavailable in the colon, favors the growth of pathogenic species.
Unfortunately wheat toxins do much more than inhibit digestion of food. They also damage the gut itself.
Wheat contains an ingenious cocktail of toxins:
- Gluten, a complex of proteins, inspires on immune response which inflames the intestine in at least 83% of people [6], and makes the intestine permeable, allowing gut bacteria and their toxins to enter the body. [7] Gluten triggers anti-wheat antibodies in at least 30% of the population, and auto-antibodies – that is, antibodies that attack human cells – in at least 0.4% of the population. [8] These unlucky folks suffer celiac disease, which devastates the intestine, as well as autoimmune thyroiditis. [9]
- Opioid peptides produce effects similar to morphine and heroin. Wheat opioids have been implicated as causes of schizophrenia. [10]
- Wheat germ agglutinin is a lectin, or protein that binds sugars. At extremely low doses, a few parts per billion, WGA causes gut inflammation and leakiness. At typical dietary doses, WGA causes shedding of the intestinal brush border and shrinkage in the surface area of the intestine. [11] WGA alone can induce celiac disease in rats. [12]
By unknown mechanisms, grains can induce vitamin deficiency diseases. Wheat and oats induce rickets [13] while corn induces pellagra. [14]
Since as little as 1 milligram of gluten per day can prevent recovery from bowel disease [15], it is essential that grains be eliminated entirely from the diet.
Legume Toxicity
Legumes also contain an array of toxins which suspend digestion and damage the gut. Some examples:
- Phytohaemagglutinin, a kidney bean lectin, makes the gut leaky; blocks stomach acid production, promoting bacterial overgrowth of the small intestine; overpopulates the gut with immature cells that are easily colonized by E. coli and other pathogens; disturbs the mucus and shortens villi. [16]
- Alpha-amylase inhibitors in legumes prevent starch digestion and leads to gut bloating and multiplication of pathogenic gut bacteria. [17]
- Antibodies to soy proteins have been identified in duodenitis, Crohn’s disease, ulcerative colitis, and coeliac disease, and these diseases are sometimes cured when soy is removed from the diet. [18]
It should be noted that peanut and soybean allergies are among the most common allergies. This testifies to the significant immune response legume toxins can generate.
Omega-6 Toxicity
Most people are familiar with the evidence linking the omega-6 to omega-3 ratio to cardiovascular disease. Most Americans have an omega-6 to omega-3 ratio in tissue that is ten-fold too high; cultures with a better omega-6 to omega-3 ratio, such as Greenland Inuit and Japanese, have much lower rates of heart disease.
Since the effect of an excessive omega-6 to omega-3 is to greatly increase inflammation while impairing immune function, it’s logical that an elevated ratio would worsen inflammatory bowel disease.
And it does. The EPIC (European Prospective Investigation into Cancer and Nutrition) study took food diaries from 203,193 people and followed them for four years [19]:
- Being in the upper quartile of intake of omega-6 fatty acids raised the risk of ulcerative colitis by 149%.
- Being in the upper quartile of intake of the omega-3 DHA, which is abundant in salmon and sardines, reduced the risk of ulcerative colitis by 36% – 77% after adjustment for omega-6 intake. (Apparently those who ate more omega-3s also ate more omega-6s.)
Another study found that being in the upper third of DHA intake reduced the risk of ulcerative colitis by about 50%. [20]
The upshot: anyone with inflammatory bowel diseases should strictly limit omega-6 consumption and strive to eat a pound per week of salmon or sardines.
Fructose Toxicity
Fructose is a sugar that is toxic and useless to humans – but it is a rich source of energy to bacteria. Fructose consumption strongly promotes bacterial growth in the intestine and increases levels of bacterial endotoxins in the body. [21]
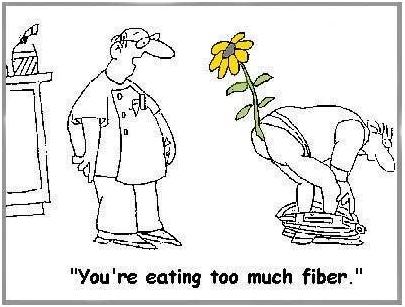
Of Fiber
Most people think that fiber is indigestible, and that it comes out in their stool. This is not true. Fiber is indigestible to humans, but not to bacteria. Fiber is bacterial food that enables gut bacteria to multiply. Bacteria, not undigested food, make up most of the dry weight of stool. [22]
Doctors often recommend fiber to bowel disease patients. While not wholly without merit, this advice usually backfires.
There are three problems: helping bacteria feed and multiply may be undesirable; fiber, such as the brans of cereal grains, often contains toxic proteins; and, finally, whole grain fibers and other “roughage” scrape and injure the intestinal wall. Dr. Paul L. McNeil explains that:
When you eat high-fiber foods, they bang up against the cells lining the gastrointestinal tract, rupturing their outer covering. [23]
That can’t be a good thing.
And it isn’t. In the Diet and Reinfarction Trial (DART), published in 1989, 2,033 British men were divided into a high-fiber group and a control group. The high-fiber group ate whole grains and doubled their grain fiber intake from 9 to 17 grams per day. The result? Deaths in the high fiber group were 22% higher over the course of the study – 9.9% of the control group died versus 12.1% of the high-fiber group. [24]
Softer soluble fibers from fruits and some vegetables are much more likely to help than wheat bran, but even they may be a good thing only in moderation, or only in a healthy bowel. Fiber feeds pathogenic bacteria as well as probiotic bacteria, and increases the populations of both. When the gut is damaged and leaky, more bacteria mean more bacterial toxins and more pathogens infiltrating the body. A low-fiber diet, leading to reduced bacterial populations in the gut, may be desirable for bowel disease patients.
Yes, it is possible to get too much fiber!
(via Peter at Hyperlipid)
Other Toxic Foods
Nightshade plants and seeds of all species can also contain toxins and may also need to be restricted in people with damaged intestines.
Dairy proteins, especially pasteurized cow casein, are also often problematic for people with damaged intestines.
In general, any foods that commonly produce allergies are likely to give trouble to people with damaged intestines.
All plant proteins are risky, as are dairy and egg proteins. It is possible to minimize risk by:
- Eating clarified butter, but refraining from protein-rich dairy foods.
- Eating cooked egg yolks, but avoiding the protein-rich egg whites.
Summary of Toxic Foods to Eliminate or Avoid
In short, bowel disease patients should eliminate toxic foods from their diet:
- Eliminate all grains except rice. Wheat, oats, and corn, and their products such as wheat flour, cornstarch, bread, and pasta, must be eliminated.
- Eliminate all legumes, especially soy, beans, and peanuts.
- Eliminate omega-6 rich oils, such as soybean oil, safflower oil, corn oil, peanut oil, and canola oil.
- Eliminate fructose sugars, except from fruits and berries. Drink no sugar-containing beverages.
- Minimize fiber to keep down gut bacterial populations and avoid mechanical injuries to the intestinal wall.
- Minimize other potentially toxic protein sources. In general, protein should be obtained from animal and fish meats, not eggs, dairy, or plants. However, fats from dairy and eggs are highly desirable.
When gut health is restored, dairy and fiber may be restored to the diet. However, the major toxic foods – grains, legumes, omega-6-rich oils, and most fructose – should be eliminated for life.
Filling the Gaps in the Diet
For most people, eliminating grains will leave a large gap in the diet. Foods that should be used to fill that gap include:
- Healthful plant foods are the safe starches, such as white rice, taro, sweet potatoes and yams, and fruits and berries.
- Saturated-fat rich oils and fats, like beef tallow, clarified butter, coconut oil, palm oil, cocoa butter (yes, chocolate desserts are healthy!), along with modest quantities of olive oil and lard. Make homemade salad dressings with these oils, rather than buying supermarket dressings made with soybean or canola oil.
- Further balance the omega-6 to omega-3 ratio by eating low-omega-6 meats, such as the red meats (beef and lamb) and seafood, and eating 1 lb per week salmon or sardines for fresh omega-3 fats.
When the small intestine is damaged, fatty foods may be difficult to tolerate, since the enzymes that digest dietary fats and proteins may also digest human cells. In such cases the diet must focus on starchy foods like rice until bowel health is restored. Be sure to supplement with vitamins and minerals in such cases.
Conclusion
Eliminating food toxins may cure bowel diseases and always improves prognosis. Pedro Bastos of The Paleo Diet Update writes:
From the feedback we have received over the years, IBS patients respond dramatically and rapidly to the Paleo Diet. Their experience indicates that milk, grains and legumes seem to be the main culprits in this condition via a number of mechanisms. [The Paleo Diet Update v.4, #18]
Auto-antibodies generated by wheat against the thyroid, pancreas, and gut typically disappear within 3 to 6 months after removal of wheat from the diet. [25, 26] This is probably a reasonable estimate for the time frame in which bowel disease patients can expect significant improvements from the elimination of dietary food toxins.
Related Posts
Other posts in this series:
- Bowel Disorders, Part I: About Gut Disease July 14, 2010
- Bowel Disease, Part III: Healing Through Nutrition July 22, 2010
- Bowel Disease, Part IV: Restoring Healthful Gut Flora July 27, 2010
References
[1] Fujimura KE et al. Role of the gut microbiota in defining human health. Expert Rev Anti Infect Ther. 2010 Apr;8(4):435-54. http://pmid.us/20377338.
[2] Ruas-Madiedo P et al. Mucin degradation by Bifidobacterium strains isolated from the human intestinal microbiota. Appl Environ Microbiol. 2008 Mar;74(6):1936-40. http://pmid.us/18223105.
[3] Bode L. Human milk oligosaccharides: prebiotics and beyond. Nutr Rev. 2009 Nov;67 Suppl 2:S183-91. http://pmid.us/19906222. Hat tip Dr. Art Ayers.
[4] Ames BN, Gold LS. Paracelsus to parascience: the environmental cancer distraction. Mutation Research 2000 Jan 17; 447(1):3-13. http://pmid.us/10686303
[5] Cummings JH. The effect of dietary fibre on fecal weight and composition. Pp 547–73 in: Spiller GA, ed. Handbook of dietary fibre in human nutrition. 2nd ed. Boca Raton, FL: CRC Press, 1993.
[6] Bernardo D et al. Is gliadin really safe for non-coeliac individuals? Production of interleukin 15 in biopsy culture from non-coeliac individuals challenged with gliadin peptides. Gut 2007 Jun;56(6):889-90. http://pmid.us/17519496.
[7] Drago S et al. Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scand J Gastroenterol. 2006 Apr;41(4):408-19. http://pmid.us/16635908.
[8] Not T et al. Celiac disease risk in the USA: high prevalence of antiendomysium antibodies in healthy blood donors. Scand J Gastroenterol. 1998 May;33(5):494-8. http://pmid.us/9648988.
[9] Sollid LM, Jabri B. Is celiac disease an autoimmune disorder? Curr Opin Immunol. 2005 Dec;17(6):595-600. http://pmid.us/16214317.
[10] Singh MM et al Wheat gluten as a pathogenic factor in schizophrenia. Science. 1976 Jan 30;191(4225):401-2. http://pmid.us/1246624. Dohan FC et al 1984 Is schizophrenia rare if grain is rare? Biol Psychiatry. 1984 Mar;19(3):385-99. http://pmid.us/6609726.
[11] Lorenzsonn V, Olsen WA. In vivo responses of rat intestinal epithelium to intraluminal dietary lectins. Gastroenterology. 1982 May;82(5 Pt 1):838-48. http://pmid.us/6895878.
[12] Sjölander A et al. Morphological changes of rat small intestine after short-time exposure to concanavalin A or wheat germ agglutinin. Cell Struct Funct. 1986 Sep;11(3):285-93. http://pmid.us/3768964.
[13] Mellanby E. (March 15 1919) An experimental investigation on rickets. The Lancet 193(4985):407-412.
[14] Carpenter KJ, Lewin WJ. A critical review: A reexamination of the composition of diets associated with pellagra. J Nutr 1985 May;115(5):543–552. http://pmid.us/3998856.
[15] Biagi F et al. A milligram of gluten a day keeps the mucosal recovery away: a case report. Nutr Rev. 2004 Sep;62(9):360-3. http://pmid.us/15497770.
[16] Kordás K et al. Phytohaemagglutinin inhibits gastric acid but not pepsin secretion in conscious rats. J Physiol Paris. 2001 Jan-Dec;95(1-6):309-14. http://pmid.us/11595455. Pusztai A et al. Kidney bean lectin-induced Escherichia coli overgrowth in the small intestine is blocked by GNA, a mannose-specific lectin. J Appl Bacteriol. 1993 Oct;75(4):360-8. http://pmid.us/8226393. Prykhod’ko O et al. Precocious gut maturation and immune cell expansion by single dose feeding the lectin phytohaemagglutinin to suckling rats. Br J Nutr. 2009 Mar;101(5):735-42. http://pmid.us/18644165.
[17] Pusztai A et al. Inhibition of starch digestion by alpha-amylase inhibitor reduces the efficiency of utilization of dietary proteins and lipids and retards the growth of rats. J Nutr. 1995 Jun;125(6):1554-62. http://pmid.us/7782910.
[18] Haeney MR et al. Soya protein antibodies in man: their occurrence and possible relevance in coeliac disease. J Clin Pathol. 1982 Mar; 35(3):319-22. http://pmid.us/7040491.
[19] IBD in EPIC Study Investigators. Linoleic acid, a dietary n-6 polyunsaturated fatty acid, and the aetiology of ulcerative colitis: a nested case-control study within a European prospective cohort study. Gut. 2009 Dec;58(12):1606-11. http://pmid.us/19628674.
[20] John S et al. Dietary n-3 polyunsaturated fatty acids and the aetiology of ulcerative colitis: a UK prospective cohort study. Eur J Gastroenterol Hepatol. 2010 May;22(5):602-6. http://pmid.us/20216220.
[21] Bergheim I et al. Antibiotics protect against fructose-induced hepatic lipid accumulation in mice: role of endotoxin. J Hepatol. 2008 Jun; 48(6): 983-92. http://pmid.us/18395289.
[22] Stephen AM et al. Effect of changing transit time on colonic microbial metabolism in man. Gut. 1987 May;28(5):601-9. http://pmid.us/3596341.
[23] Quoted in Science Daily, http://www.sciencedaily.com/releases/2006/08/060823093156.htm. Hat tip Dr. Michael Eades.
[24] Burr ML et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989 Sep 30;2(8666):757-61. http://pmid.us/2571009. Hat tip Stephan Guyenet.
[25] Berti I et al. Usefulness of screening program for celiac disease in autoimmune thyroiditis. Dig Dis Sci. 2000 Feb;45(2):403-6. http://pmid.us/10711459.
[26] Mainardi E et al. Thyroid-related autoantibodies and celiac disease: a role for a gluten-free diet? J Clin Gastroenterol. 2002 Sep;35(3):245-8. http://pmid.us/12192201.











This is amazing. I’ve copied to my HD so I pore over it. Have you heard of anyone being able to follow such regimen while living with a main-lining pasta eater?
Sorry, I forgot.
Q. My ophthamologist wants us to take 3 1000 mg flax oil capsules daily for dry eyes. Does that factor in at all?
Hi erp – It’s really tough to eat a different diet than your spouse. However, you can try cooking pasta with rice noodles. Asian supermarkets have a wide selection of rice noodles. We make lasagna, spaghetti, and other pasta dishes with rice noodles.
We also sometimes make low-carb lasagnas with boiled cabbage substituted for the noodles. And you can try converting your husband to risottos.
For dry eyes, you should definitely eat 1 lb/wk salmon or sardines, plus get abundant vitamin C as well as normalizing vitamin D.
Re the flax seed, I have two objections:
1. First of all, it’s the long omega-3s DHA and EPA that help dry eyes (see, e.g., http://www.ncbi.nlm.nih.gov/pubmed/20202804 and http://www.ncbi.nlm.nih.gov/pubmed/19227095). But flax oil does not contain DHA or EPA, and is inefficiently converted to these, especially if the diet contains significant omega-6s. So eating salmon and sardines would be much better for your dry eyes than the flax seed.
2. Omega-3 fats quickly become rancid. Capsules are dangerous. I did a post on this (http://perfecthealthdiet.com/?p=55). You should get omega-3s from food, not capsules.
Thanks, Canned salmon okay?
I’ll check out rice noodles. That’s a good idea.
I read your comment about lasagna made with cabbage to my husband and I think he’s fainted. ;-{
Canned salmon is great.
Sorry to hear he’s fainted. Maybe the aroma of cabbage lasagna would wake him? 🙂
Wow! There’s a lot here that goes against the conventional wisdom.
I don’t mind that, but it also goes against what I consider two good dietary choices for me — tomatoes and red bell peppers.
Just wondering … what do you think of avocados?
Hi Jim,
We eat tomatoes and red peppers. Remember, nightshades were mentioned in a section about foods that might possibly be difficult for people with bowel disease. In general, people with healthy bowels are more tolerant of low-level food toxins. The evidence against nightshades is mostly anecdotal at this point. The Weston A Price Foundation newsletter had an article on it: http://www.westonaprice.org/food-features/1897-nightshades.html. See what you think of their evidence.
We strongly endorse avocados and eat them regularly — every week. One of our favorite foods.
Paul,
You discussed the potential adverse effects of fiber, particularly wheat bran. What about psyllium?
Hi David,
I’m not aware of specific evidence for food toxins in psyllium, but it’s quite likely that it’s never been investigated. I am skeptical of seeds as a source of fiber because on evolutionary grounds seeds are quite likely to develop toxins that attack the gut. In general I don’t believe there’s a need for fiber supplements; fiber should be obtained from food and excellent sources are sweet potatoes, berries, avocado, and safe starches, fruits, and vegetables generally.
Psyllium is usually recommended for constipation. Although constipation can sometimes be caused by a deficiency of gut bacteria, it’s usually the result of hypothyroidism or nutrient deficiencies. For constipation I would start with selenium (200 mcg or Brazil nuts), iodine (1 mg or seaweed), vitamin C (2 g), vitamin D (2500 IU or sunshine), and glutathione (500 mg), and get a thyroid panel. If TSH is above 1.5 after the selenium and iodine supplements, I would ask for a thyroid hormone prescription and see if that cures the constipation.
In general, I’m not impressed by the clinical evidence for psyllium. It seems to be helpful in acute infections that produce diarrhea for 2-3 days. Other than that, it doesn’t seem to do much. A representative study is http://www.ncbi.nlm.nih.gov/pubmed/2169535 in which glutamine, a simple energy source which has only modest benefits, outperformed psyllium fiber.
In short, there is little evidence for either benefits or harm from psyllium. Personal experience trumps the medical literature in such cases. If it works for you, great … but I think if you don’t notice any benefits it’s probably safer to drop it. I won’t be trying it myself.
Great post. But I have some doubt on the fiber issue.
According to Stephan Guyenet of whole health source:
http://wholehealthsource.blogspot.com/2009/12/butyric-acid-ancient-controller-of.html,
Butyrate suppresses inflammation in the Gut and other Tissues and the major source of butyrate is fiber.
According to him:
“Butyrate, or dietary fiber, prevents the loss of intestinal permeability in rat models of ulcerative colitis”
Daniel,
Great point. I’ve been saving butyrate for later in this series. It’s therapeutically important and you definitely want to maximize butyrate while minimizing pathogen populations and bacterial endotoxins. Unfortunately these are conflicting goals, if the butyrate is obtained from fiber.
Butyrate can also be obtained from other sources, like butter. As Stephan mentions, butyrate enemas or supplements have been used in research studies. (They have not been so successful as to enter clinical practice yet.)
I don’t want to sound like I’m hostile to fiber. The Perfect Health Diet recommends getting 400 carb calories from sources like sweet potatoes (300 carb calories per pound), fruit (typically 200 carb calories per pound), and berries (typically 150 carb calories per pound). Plus vegetables (calories not counted). So this adds up to about 2 pounds of plant foods per day, and most of this mass consists of fiber. So, because our diet is free of calorie-dense low-fiber foods like grains and sugars, we actually recommend a diet with more fiber than the average American gets.
However, it’s an open question what the optimum amount of fiber is for bowel disease patients.
What I would like bowel disease patients to be aware of is that (1) toxin-containing or rough fibers, such as wheat bran, should absolutely be eliminated, (2) fiber is most likely to be beneficial if it comes from nutritious food, not supplements, and (3) there is an optimum amount of fiber for them which may not be large. More is not necessarily better. They should listen to their bodies and form their own judgments whether fibrous plants are helping them.
Thanks for the reply, Paul. I agree with your point of view. We should get our fiber from safe sources like sweet potatoes, veggies and fruits. Eating butter would be another way to get butyrate without eating too much fiber, but I think dairy proteins could be problematic for some people. So maybe clarified butter or yogurt could be a better option?
Yes, clarified butter is always good. Yogurt can still be a problem, but pre-digestion of the proteins by bacteria makes it less risky than milk.
People with bowel problems will usually do well to avoid dairy proteins, but my belief is that people with healthy bowels can usually manage dairy. Of course Loren Cordain is of the opposite view. Fortunately if you listen closely to your body you can usually tell if you’re sensitive to dairy proteins.
How about homemade kefir for those of us with bowel disease? In my case, I experience chronic bloat – it seems nothing leaves my stomach. Your diet with the addition of a potato starch smoothie has almost eliminated my constipation – but all is not well, as there is this constant bloat. I’m going to begin eliminating FODMAPS, but I know I can’t give up the cream in the coffee – I’ve tried, I just can’t do it. I’m also wondering about fermented cabbage – does the fermentation mean it’s no longer considered toxic? I haven’t had wheat or grains in ages, but clearly I’m missing something. Thanks so much for your wonderful book and blog.
Hi Paul,
First off, great post – thank you. I could not agree with you more. We try to educate when asked on these topics all the time. I grew up on raw milk straight from the cow, made our own butter, yogurt, etc. and lived a pretty much Paleo lifestyle until we moved to the US. Then all of a sudden I had horrible reactions when I had milk (same with my husband – but we didn’t know each other then) could not eat pork or cauliflower anymore either…weird…turns out we had a major reaction to gluten, grains, sugars, CORN everything and since going back to a Paleo way of life, enjoy raw milk from a local dairy, pork etc. all of it again with zero problem. No more lactaids, no more pain, no more processed food. So yes, you are right in every way. Thanks for the opportunity to share my little six pence. 🙂
Hi Josephine, Thanks for writing.
So many people report that raw milk is fine for them but pasteurized milk is problematic. It seems that pasteurization folds cow casein into shapes that humans can’t digest well. What a shame that in the US our governments have made it so difficult to obtain raw milk.
Your food pictures at http://nuttykitchen.com look fantastic! We will have to try some recipes.
Great series!
There is evidence to suggest that some bowel disease related conditions are affected by oxalates in foods. Sweet potatoes are particularly high in oxalates. Thoughts?
Hi Peter,
Yes, I agree. Oxalates are scarfed up by fungal species which make calcium oxalate biofilms. So oxalates can promote Candidal overgrowth. I had to give up green tea myself for that reason.
I never gave up sweet potatoes though, since they are one of my favorite foods.
Bowel disorders are hard, since so many normally healthy things can give trouble. In bowel disorders you have to find compromises that work for you.
Hi Paul,
As a big green tea drinker can you please expand on why you had to give it up?
I drink de-caffeinated green tea and now when I drink regular black tea or caffeinated green tea I get diarrhea even at 1 cup.
Regards,
WP
Hi Winalot,
Green tea is generally healthy. I stopped it for a year or so because of concern about oxalates — I have a long history of recurrent fungal infections, which might or might not be gone now. We get expensive large-leaf green tea from Taiwan and I used to use keep the same leaves in my teacup throughout the day, regularly adding water, so I got a lot of compounds from the tea leaves. Now I’m much more cautious and only let the leaves steep 10 minutes, have 2-3 cups, then discard the leaves. So I drink a lot less tea and it is very mild and delicate in taste now. I think this is safer. I started drinking coffee, heavily diluted with cream, as a replacement beverage.
I some how came across the Healthy Skeptic, and from there, found my way to The Perfect Diet. I have recently realized I must try to modify my diet to help my poor inflamed digestive system, but I must say that much of what you have to say seems pretty shocking, compared to mainstream ideas about good nutrition. I am willing to give this a try, but maybe you could give me a few reassurances? For example, if I eliminate grains, am I not going to become deficient in B-vitamins? Why are the legumes to be avoided? I thought they were considered a very healthy form of protein, and that gassiness from them can be dealt with by Beano or similar enzymes. And here’s a really big one: are you sure about all that saturated fat? Yikes! This is all feeling pretty topsy–turvy. Eagerly await your response!
hi there,
can you please remove our email address from the comments section? I thought that it was not going to be published. thanks, marla
Hi marla,
The email address isn’t published. No one else can see it.
Lots of foods have B vitamins and no, you won’t become deficient if you eliminate grains. Grains are not a particularly good source of B vitamins. In any case we recommend taking a daily multivitamin, which with food should give you about 3x the RDA of most B vitamins.
Legumes contain a lot of toxins. There may be ways to prepare them that reduce toxin levels to acceptable levels (such as overnight soaking followed by thorough cooking), but I think most people will not do that. It’s better to eat non-toxic or less toxic foods.
Yes, we are sure about the saturated fat!
The book has all the evidence, and it takes dozens of pages to cover it, so I won’t repeat it here. If our diet would mean a big change, you might find it would bring big improvements in health.
Hi Paul,
Thank you for your in-depth work, I enjoy reading helpful informed articles such as yours. So many articles I read – especially by weight loss folk ie nutritionists – take no account of actual human digestion.
The toxins you refer to re: grains seeds and legumes, are they the same as the phytates/phytic acids referred to by Sally Fallon and Mary Enig PhD in their book Nourishing Traditions? I see you have referred to an article from the Weston A Price Foundation, of which Sally Fallon is president.
For the last 7 or more years I’ve sought out sprouted grain breads thinking it was good for me, and have been tested as not sensitive to wheat. My naturopath at the time was very surprised, though I’m definitely intolerant to soy and albumin, as well as allergic to pork and peanuts (joint pain).
Thanks also for more encouragement to eat sweet potatoes, taro, and chocolate – yum!
PS What are your thoughts on inulin? When I’ve supplemented with the powder, it gave horrible gas. Is it the natural fibre in sweet potatoes? Articles I’ve read tout it as helpful to feed good bacteria and help it take up residence in the gut.
Hi Sonja,
We are fans of Sally Fallon and Mary Enig but don’t agree with them on everything.
Phytate is a potential issue but far from the major concern with grains and legumes. Phytate binds minerals and can reduce mineral absorption from food.
However, the proteins and protein fragments that sabotage the gut, enter the body, and exert toxic and immunogenic effects are much more concerning to us. These include gluten and equivalents, lectins, and other toxic proteins.
I would avoid sprouted grain breads. Better safe than sorry.
Inulin – I’m undecided about it. I wouldn’t supplement but would eat foods that contain it. Inulin is present in sweet potatoes and especially in certain other tubers like Jerusalem artichoke and burdock. It’s definitely a rich food for gut bacteria, that’s why you got gas – the bacteria were having a feast! It will definitely give you more bacteria but I personally would like more evidence that it’s beneficial in all or nearly all people before I would recommend it.
Hi Paul,
Thank you for your thoughtful reply. I’ll stay tuned 🙂
Hi Paul. How can we definitively find out if we have an unhealthy gut? What’s the first step? Is there a specific doctor we can see/test we can take or is our best option an elimination diet and our own judgment? I suspect that I do have an unhealthy gut, but knowing for sure would give me greater motivation to strictly abstain from problematic foods. For example, you’ve previously mentioned that as little as 1 milligram of gluten per day can prevent recovery from bowel disease, so it is essential that grains be eliminated entirely from the diet. I try not to let my dietary changes affect other people too much so I don’t always follow my typical dietary style in some social or family situations. However, I would NOT be lenient anymore if I knew that I had a leaky gut or some other bowel disease.
Hi Kaitlyn,
It’s a good question, because many people have unhealthy guts without knowing it.
On the other hand, good diet and nutrition is the best treatment for mild gut dysbiosis or injuries, so the first step should be diet and nutrition rather than tests.
When a leaky gut is severe, so that lots of toxins and bacteria are being allowed to enter the body, then you will feel tired after eating a meal. The extra food makes bacteria multiply and generate toxins; the surge of toxins entering the body excites immune activity; the inflammation causes you to get tired.
There may also be specific food sensitivities. In general, food sensitivities go away once the gut is healthy.
Other symptoms include acid reflux, abdominal bloating, constipation, occasional diarrhea.
Since antibiotics will make many gut problems worse, diet, nutrition, and some antibiofilm actions are the best first step.
For instance, it’s now cranberrry season and I have a bowl of raw cranberries on my desk which I’m munching as I work. Cranberries are good biofilm disruptors.
Hello,
Hope that you and your family are enjoying the holidat season. After today feeling the impact of unfortunate holiday food choices (I guess with a leaky gut that too much coconut flour and butter can cause a problem), I have renewed my intention to heal my ailing digetsive system this year. I have more seriously been considering trying GAPS yet I am I wondering if the assertion that polysaccharides can not be digestive by a leaky gut is actually true, it seems to be the reason that starches, even safe starches, are not allowed on the diet. The only starch I eat now are potatoes/sweet potatoes, are these really hampering my recovery? Are the enzymes that digest starches truly comprised in digestive illness?
Thanks so much,
Devi
Hi Devi,
Dairy proteins are definitely challenging for people with leaky guts; if you clarify the butter it should be OK. An easy way to do a 90% clarification is to melt butter with some water in the microwave, let it separate, and keep the fatty yellow top part and discard the milky white part. Real clarification requires bringing the butter to a low boil so that the proteins in the fatty part will form a crispy solid.
All protein-containing plants are potentially problematic. I’m not sure what in coconut flour is troublesome but it’s not a surprise if something is.
Different gut ailments call for different foods. Potatoes and sweet potatoes have a lot of fiber and this will feed colonic bacteria and, if they are pathogenic, potentially give you problems. You might find rice works better, since it is low in fiber and is mostly digested in the small intestine so doesn’t feed colonic pathogens much.
The enzymes that digest starches are working, but keep in mind that they only digest simple starch chains and bacteria will get the branching structures and “resistant” starch. Warm rice is probably the most digestible of starches.
You have to experiment to find what works best for you. In some gut ailments you want to provide fiber to feed commensal bacteria, in some you want to starve the bacteria.
Every gut ailment is a bit different. I find berries are good for mine because I had a yeast/fungal infection take over my colon while on antibiotics and very-low-carb dieting; berries are rich in anti-mold anti-fungal toxins. But other people would find the fructose in berries feeding a small intestinal bacterial overgrowth.
It helps if you get an idea exactly where your problem is — colon or small intestine — and what pathogens you have, and whether you have enough commensal bacteria to help you fight the pathogens with appropriate kinds of fiber.
So experimentation is needed in gut ailments.
Best, Paul
Paul,
Thank you for the reply–it helps to clarify my concerns. Is there a definitive way of finding out exactly where the problem is and the nature of the pathogens? The hydrogen breath test for SIBO was negative, so much so that my gastro asked me if I was on antibiotics at the time of the test–which I was not. Im still not sure what that means. Endoscopy last year revealed nothing and H Pylori negative. Im guessing that mine is a yeast issue–my history includes a fever of unknown origin in the fall of 2001 at which time I was given massive amounts of antibiotics for several months and also years of restrictive eating (very low carb, lots of vegetable fiber).
Interesting about white rice, through lots of experimentation I have discovered that white rice does not work for me, makes my acid reflux double and I feel intoxicated after eating it. Potatoes (small purple/red ones cooked without skin) seem to be okay actually. I try to keep fiber low in general Daily symptoms are food intolerances, acid relfux, some constipation, headaches after eating, belching.
Thanks again,
Devi
Hi Devi,
It’s good that the hydrogen test was negative but that only rules out some pathogens, not all.
Yeast is very possible, yeast ferments rice to alcohol which would explain intoxication. However, yeast infections of the small intestine are rare except when there is a severe yeast infection of the colon. (Colon is more favorable for them, so you don’t normally get one without the other.) Do you have abdominal bloating (which I associate with yeast)?
Those symptoms do indicate leaky gut and small intestinal infection of some kind. You should keep calcium intake low, since both bacteria and yeast biofilms use it. You might try a complex of carbohydrate/polysaccharide digesting enzymes (which are benign to humans) and probiotics with both Bifidobacterium and other species.
You might try fermented vegetables like kimchi and sauerkraut. They’ll probably make you feel worse just after you eat them, and might give a brief infection, but they might help provide some missing commensal species.
Are you following our basic suggestions from the book?
Best, Paul
Hello,
I am following the suggestions in the book–it is a tremendous resource for me, particularly the amounts and kinds of protein, fats. I was eating way over the amount of recommended protein. Its with the safe starches where I have been doing the most experimentation. I have eliminated all grains, legumes, vegetables oils and calcium supplements.
I do have abdominal bloating. I have been using digestive enzymes since March, however I have been trying to reduce them as they are multi-enzyme (amylase, protease, lipase, etc..). I have not been able to find an enzyme supplement which is solely for carbs, are there any that you are aware of?
Probiotics I have been doing again recently and interesting re: fermented vegetables, I have been trying them off and on. I often find that I get terrible headaches from fermented food yet would be willing to incorporate them again. Also, want to try more intermittent fasting.
Thanks again,
Devi
Hi Devi,
Interfase from Klaire Labs and Wholezyme from Whole Foods are, if I recall correctly, high in the polysaccharide digesting enzymes and low in lipase/protease. I haven’t taken either in a long time and don’t have the formulas handy but those might be worth a try.
In general, traditional herbs and herbal foods tend to promote gut health. So spices like oregano, turmeric, etc. are worth including in meals. Lemon juice may be helpful.
Since you get headaches, I would stay away from fermented foods for a while until you feel healthier.
Best, Paul
Hi Paul, you said that warm rice is probably the most digestible of starches.
I usually cook all my food and eat them in a 20-30 minutes time. Do you think waiting this time may increase the resistant starch significantly?
I read some research about RS formation after cooling but they wait for 24+ hours, do you have some data?
Hi Kratos,
I don’t have data but I think it’s mainly temperature and moisture dependent, rather than time dependent. The 24 hours might have been chosen to allow it to dry. Water and warmth tend to prevent RS bonds from forming. Salt, fat and protein also affect it, see http://en.wikipedia.org/wiki/Starch_gelatinization. So I think there’s not a simple answer.
Best, Paul
Paul, do you know if there are gut problems that could produce halitosis? My 14-year-old had a very sudden and acute onset of halitosis that her dentist determined was not orally based and her pediatrician said might be from GERD. We gave her Prilosec for many months, and eventually it cleared up. However, I was never satisfied with the lack of a definitive diagnosis. She had previously tested negative for H pylori (which her father got after a trip abroad). She is a carb addict.
I just ordered your book, in the hopes that it is the handbook I need after reading Gary Taubes’ Why We Get Fat and What to Do About it. I’m just learning, for example, that my daily doses of wheat germ may be the reason my basal thumb arthritis has progressed so remarkably over the past two years!
Hi Donna,
Wheat germ is awful! Bad fats and toxins to boot.
Definitely gut problems can cause halitosis. Acid reflux will do it, as will bad bacteria in either the gut or the mouth. Gut dysbiosis can actually feed mouth bacteria.
Julianne had a good post about bad breath: http://paleozonenutrition.wordpress.com/2010/11/20/bad-breath-frequent-strep-throat-ear-infections-try-mouth-and-throat-probiotics/. The oral probiotic she mentioned can be obtained in the US, Amazon sells it here: http://www.amazon.com/Probiotic-Formula-Strawberry-Flavor-Chwbls/dp/B0031XEF0Y/
Digestive tract issues should be addressed directly; Prilosec provides only temporary relief but generally makes gut problems worse later.
Just adopting our diet and supplements will fix many gut problems and cure acid reflux in many. If more is needed, our bowel disease series (http://perfecthealthdiet.com/?cat=47, scroll down to the bottom and read upward) is a good primer on how to fix gut problems / acid reflux.
Please keep me posted, I’ll be happy to answer questions. Your arthritis should be curable, and perhaps we can convert your daughter to fat a little bit!
Best, Paul
Hi Paul
I’ve been eating a few ounces of (Del Monte canned no-salt) sweet corn each day to ensure an adequate food intake of lutein and zeaxanthin. (Both my parents had macular degeneration and cataracts.)
Does sweet corn count as:
–a grain (bad)
–a vegetable (neutral)
–or a safe starch (good)?
John
grain (bad)
It’s derived from teosinte, an American grass. http://en.wikipedia.org/wiki/Teosinte
There are lots of other sources of lutein and zeaxanthin. I rely on egg yolks mainly but green leafy vegetables and paprika are alternatives.
Paul, I apologize if that came across as a dumb question. I understand ‘corn is corn’, but ‘sweet corn’ being a special stage in the life cycle of the plant, I thought it might make a difference, as germination perhaps might.
I have one can short of six months’ worth of the Del Monte on hand, so I felt a need to check.
We are eating eggs now, two a day, so perhaps that obviates the concern.
Thanks.
Hi JBG,
It’s not a dumb question at all! Much more likely to be a dumb answer. The trouble is that the toxins in corn aren’t well studied. So I can’t really say whether they’re absent in sweet corn.
Fruit becomes naturally sweet and low in toxins at the same time, because it evolved to have mammals spread the seeds. But corn kernels don’t have indigestible seeds inside, so I don’t think the same process would be operative. And they were artificially bred for sweetness, the sweetness didn’t evolve naturally. There was no artificial breeding for non-toxicity that I’m aware of.
So maybe the corn is OK, maybe not. Personally, I would be cautious about restocking after you eat what you have. Or donate the cans to a food pantry if you’re worried.
But yes, if it’s just lutein and zeaxanthin that you want, I would go for the eggs and leafy greens.
Hello,
I wasnt sure where to place this on the blog..would be very appreciative of your feedback as my situation has unfortunately taken a perplexing turn. I was on Lexapro (5 mg) for about a year, and decided to taper off with medical help, I stopped taking the meds about a month ago. Shortly thereafter I began having pains in my lower left/right sides, different than the usual stomach issues (yeast, reflux).I have no idea if this is related to the med cessation. That eventually escalated to one week of headaches, high fever (now gone), and increase in bloating, nausea, and change in bowel habits. Abdominal CT scan is negative, blood cultures negative for various bacteria, however elevated SED rate (74) and now low iron (28). Doctor now suggesting a colonoscopy to rule out inflammatory bowel issues (possibly crohns) as the pain, bloating, and other symptoms continue. My main issue is diet at this time. I am unable to tolerate potatoes/sweet potatoes any longer or most starches (rice) without pain and bloating, yet the protein/fat and vegetable juices I am currently eating doesnt seem that healthy either. I just finished re-reading the bowel disease posts and know that you recommend to not cut out carbs with bowel disease and Im quite hungry without the starch. What are your recommendations for safe starches (low in fiber and not feeding the new level of toxins in my gut?) I am supplementing D, selenium, reduced gluth, magnesium, copper, trying zinc although irritating my gut, probiotics. I have no idea whats going on in my gut and trying to maximize my diet for healing.
Thanks!
Devi
Hi Devi,
Well, it seems likely it’s some kind of bowel infection with the high SED rate and low iron both confirming that.
The drug does have immune system effects (see http://www.ncbi.nlm.nih.gov/pubmed?term=Escitalopram%20immunity) and it’s possible there could be some relation between cessation of the drug and flaring of the infection or immune activity against it.
Since the infection seems to be primarily in the colon, I would think that fiber, such as resistant starch, is the biggest problem and fast-digesting carbs might be tolerated. Have you tried rice syrup? It’s basically pre-digested rice. Chew any carbs thoroughly and let them mix with saliva before swallowing. Dextrose would be even easier to digest. Do you tolerate table sugar? Foods containing simple sugars like fruit and berries?
You might want to ask for a fecal screen for pathogens (something like http://www.ibstreatmentcenter.com/4_a.htm ).
Best, Paul
Thanks Paul for your quick reply! Im also wondering if the infection is in the small intestine as Im still belching a lot and the pain is on the lower right side. Im definitely going to try the rice syrup. Ive had some trouble with fruits and berries due to the fiber content and concerns about too much fructose feeding pathogens–are there fruits that you would recommend? Im finding the biggest issue is hunger actually, without the carbs which are satiating Im finding that Im really overeating protein which is concerning. Is there a certain level of carbs to shoot for each day to keep my immune system healthy?
Thanks again,
Devi
It could be. Bananas are relatively low in fructose and fiber so you could try those.
The best level of carbs will vary but I think you should shoot for at least 200 calories as a minimum.
Hi Paul,
I just tested positive for SIBO and am fructose intolerant. I have IBS and have many food sensitivies. I just started a round of Rifaximin and am confused as to what I can eat. I have not had luck coming up with a diet, as there so much conflicting information out there. Should I be taking enzymes after each meal? I do take probiotics, but am wondering the best one to take.
Thanks,
Lisa
Hi Lisa,
It is confusing, largely because everyone’s bowel disease is a little different.
So you have to experiment a bit to find what’s best for you, diet-wise.
The easiest carb calorie sources may be rice syrup or dextrose, which are pre-digested starch. You can experiment with low-fructose carb sources to find the ones that give the least trouble.
As far as enzymes, polysaccharide digesting enzymes are good to take at any time. Proteases can do harm as well as good and, if taken, should be taken only with food; lipases, mostly harm and I would avoid them. I would look for a formula rich in cellulase, hemicellulase, etc.
Probiotics – I think fermented vegetables are best. Primal Defense (not Ultra) is good because it has a wide range of species. L. reuteri may be a specific species to look for as well.
Best, Paul
Hi Paul
Can you explain more how proteases do harm?
Paul,
This is an old post, but I came across is as I was doing some research on my never-ending (since I was about 11) stomach pains. I have established that bouts of heavy alcohol drinking, high caffeine intake and possibly dairy work together to wreak havoc on my stomach. But even during spans of time when I am not involved in such raucous activity I always have a little bloating and a reasonable amount of belching… going on more than 15 years now.
Recently, I spent several hours reading up on milk and the controversy surrounding the whole milk sensitivity issue. Ray Peat seems to think that milk is not actually the issue–instead he blames the milk sensitivity on carageenan which is found in many mass produced milk products. I did a little hunting around on pubmed and found at least one study that may support his claim… But am wondering what is your take on this? Is it in fact lactose? I buy milk and other dairy products from local pasture-raised sources so there should not be anything in my milk but the milk itself and maybe D3.
It’s 2011… it would be nice if there was a little more advanced knowledge about the wild world of intestines. I for one, am ready to rip mine out.
Hi Lindsay,
Carrageenan is problematic. We’ve had discussions about this before, see eg Perry’s comment: http://perfecthealthdiet.com/?p=1788#comment-13116.
The symptoms you describe in the first paragraph could be indicative of Candida overgrowth. Candida metabolizes alcohol to acetaldehyde which is highly toxic (and carcinogenic). See http://www.ncbi.nlm.nih.gov/pubmed/19793674.
Popular anti-Candida diets recommend excluding caffeine and dairy but I’m not sure how solid the evidence is for that. Caffeine does have effects on Candida (http://www.ncbi.nlm.nih.gov/pubmed/7746292) but it’s not obviously good for them. Some species flourish in milk (http://www.ncbi.nlm.nih.gov/pubmed/21349344).
I found Chinese medicine has a good assortment of antifungals and with a detox aid like cholestyramine/charcoal/bentonite clay/chlorella and probiotics / fermented vegetables works pretty well.
If it’s lactose intolerance, probiotics and regular eating of yogurt would solve the problem.
Best, Paul