The gut is the front line of health. The human gut houses 100 trillion bacteria from a thousand different species [1]; they weigh several pounds and make up about half the dry weight of stool. To control these bacteria 70% to 80% of the body’s immune cells are normally found in and around the gut.
A healthy gut is protected by a mucosal layer that is designed to promote commensal (friendly) bacteria, while providing a barrier to pathogenic bacteria. Humans have evolved ways to “feed” commensal species of bacteria. For instance:
- Human mucus is made of glycoproteins, or compounds made of protein and sugar. Certain probiotic bacteria, such as Bifidobacterium bifidum, are able to digest human mucus. [2] Thus, the human intestine has evolved to produce “food” for beneficial gut bacteria, assuring that they are maintained even during long fasts.
- Mother’s milk contains special sugars, called human milk oligosaccharides, which specifically feed Bifidobacterium bifidum and assure that this species successfully colonizes the baby’s intestine and wards off infection. [3]
The absence of this protective barrier of mucus and friendly bacteria makes the intestine extremely vulnerable to infectious disease. Premature babies who are fed formula, not human breast milk, often contract a dangerous intestinal infection, necrotizing enterocolitis. [3]
In addition to pathogenic bacteria, the gut is confronted by a heavy load of toxins. Bruce Ames and Lois Gold have estimated that the average person eats 5,000 to 10,000 different plant toxins, amassing to 1500 mg per day, plus 2000 mg of burnt toxins generated during cooking. [4]
Today’s post will focus on how those 1500 mg of natural plant toxins damage the intestinal wall and its mucosal barrier, thereby bringing about infectious bowel diseases.
Cereal Grain Toxicity
Grasses became the staple foods of agriculture because of their rich yields: a single plant may generate tens of thousands of seeds annually.
Yet this prolific seed production has always made grasses attractive to herbivores, and caused seeds to evolve high levels of toxins designed to poison mammalian digestive tracts, thus enabling their seeds to pass through herbivore guts undigested. It is these toxins that make the cereal grains so dangerous to human health.
The effectiveness of grain toxins at sabotaging human digestion is illustrated by the increase in fecal mass they produce:
For every gram of wheat bran eaten, fecal weight increases by 5.7 grams. [5]
By inhibiting human digestion, wheat toxins dramatically increase the amount of undigested starch reaching the colon. This increased food supply substantially increases the bacterial population – and the presence of starch, which is ordinarily unavailable in the colon, favors the growth of pathogenic species.
Unfortunately wheat toxins do much more than inhibit digestion of food. They also damage the gut itself.
Wheat contains an ingenious cocktail of toxins:
- Gluten, a complex of proteins, inspires on immune response which inflames the intestine in at least 83% of people [6], and makes the intestine permeable, allowing gut bacteria and their toxins to enter the body. [7] Gluten triggers anti-wheat antibodies in at least 30% of the population, and auto-antibodies – that is, antibodies that attack human cells – in at least 0.4% of the population. [8] These unlucky folks suffer celiac disease, which devastates the intestine, as well as autoimmune thyroiditis. [9]
- Opioid peptides produce effects similar to morphine and heroin. Wheat opioids have been implicated as causes of schizophrenia. [10]
- Wheat germ agglutinin is a lectin, or protein that binds sugars. At extremely low doses, a few parts per billion, WGA causes gut inflammation and leakiness. At typical dietary doses, WGA causes shedding of the intestinal brush border and shrinkage in the surface area of the intestine. [11] WGA alone can induce celiac disease in rats. [12]
By unknown mechanisms, grains can induce vitamin deficiency diseases. Wheat and oats induce rickets [13] while corn induces pellagra. [14]
Since as little as 1 milligram of gluten per day can prevent recovery from bowel disease [15], it is essential that grains be eliminated entirely from the diet.
Legume Toxicity
Legumes also contain an array of toxins which suspend digestion and damage the gut. Some examples:
- Phytohaemagglutinin, a kidney bean lectin, makes the gut leaky; blocks stomach acid production, promoting bacterial overgrowth of the small intestine; overpopulates the gut with immature cells that are easily colonized by E. coli and other pathogens; disturbs the mucus and shortens villi. [16]
- Alpha-amylase inhibitors in legumes prevent starch digestion and leads to gut bloating and multiplication of pathogenic gut bacteria. [17]
- Antibodies to soy proteins have been identified in duodenitis, Crohn’s disease, ulcerative colitis, and coeliac disease, and these diseases are sometimes cured when soy is removed from the diet. [18]
It should be noted that peanut and soybean allergies are among the most common allergies. This testifies to the significant immune response legume toxins can generate.
Omega-6 Toxicity
Most people are familiar with the evidence linking the omega-6 to omega-3 ratio to cardiovascular disease. Most Americans have an omega-6 to omega-3 ratio in tissue that is ten-fold too high; cultures with a better omega-6 to omega-3 ratio, such as Greenland Inuit and Japanese, have much lower rates of heart disease.
Since the effect of an excessive omega-6 to omega-3 is to greatly increase inflammation while impairing immune function, it’s logical that an elevated ratio would worsen inflammatory bowel disease.
And it does. The EPIC (European Prospective Investigation into Cancer and Nutrition) study took food diaries from 203,193 people and followed them for four years [19]:
- Being in the upper quartile of intake of omega-6 fatty acids raised the risk of ulcerative colitis by 149%.
- Being in the upper quartile of intake of the omega-3 DHA, which is abundant in salmon and sardines, reduced the risk of ulcerative colitis by 36% – 77% after adjustment for omega-6 intake. (Apparently those who ate more omega-3s also ate more omega-6s.)
Another study found that being in the upper third of DHA intake reduced the risk of ulcerative colitis by about 50%. [20]
The upshot: anyone with inflammatory bowel diseases should strictly limit omega-6 consumption and strive to eat a pound per week of salmon or sardines.
Fructose Toxicity
Fructose is a sugar that is toxic and useless to humans – but it is a rich source of energy to bacteria. Fructose consumption strongly promotes bacterial growth in the intestine and increases levels of bacterial endotoxins in the body. [21]
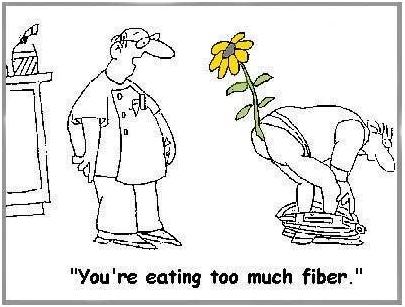
Of Fiber
Most people think that fiber is indigestible, and that it comes out in their stool. This is not true. Fiber is indigestible to humans, but not to bacteria. Fiber is bacterial food that enables gut bacteria to multiply. Bacteria, not undigested food, make up most of the dry weight of stool. [22]
Doctors often recommend fiber to bowel disease patients. While not wholly without merit, this advice usually backfires.
There are three problems: helping bacteria feed and multiply may be undesirable; fiber, such as the brans of cereal grains, often contains toxic proteins; and, finally, whole grain fibers and other “roughage” scrape and injure the intestinal wall. Dr. Paul L. McNeil explains that:
When you eat high-fiber foods, they bang up against the cells lining the gastrointestinal tract, rupturing their outer covering. [23]
That can’t be a good thing.
And it isn’t. In the Diet and Reinfarction Trial (DART), published in 1989, 2,033 British men were divided into a high-fiber group and a control group. The high-fiber group ate whole grains and doubled their grain fiber intake from 9 to 17 grams per day. The result? Deaths in the high fiber group were 22% higher over the course of the study – 9.9% of the control group died versus 12.1% of the high-fiber group. [24]
Softer soluble fibers from fruits and some vegetables are much more likely to help than wheat bran, but even they may be a good thing only in moderation, or only in a healthy bowel. Fiber feeds pathogenic bacteria as well as probiotic bacteria, and increases the populations of both. When the gut is damaged and leaky, more bacteria mean more bacterial toxins and more pathogens infiltrating the body. A low-fiber diet, leading to reduced bacterial populations in the gut, may be desirable for bowel disease patients.
Yes, it is possible to get too much fiber!
(via Peter at Hyperlipid)
Other Toxic Foods
Nightshade plants and seeds of all species can also contain toxins and may also need to be restricted in people with damaged intestines.
Dairy proteins, especially pasteurized cow casein, are also often problematic for people with damaged intestines.
In general, any foods that commonly produce allergies are likely to give trouble to people with damaged intestines.
All plant proteins are risky, as are dairy and egg proteins. It is possible to minimize risk by:
- Eating clarified butter, but refraining from protein-rich dairy foods.
- Eating cooked egg yolks, but avoiding the protein-rich egg whites.
Summary of Toxic Foods to Eliminate or Avoid
In short, bowel disease patients should eliminate toxic foods from their diet:
- Eliminate all grains except rice. Wheat, oats, and corn, and their products such as wheat flour, cornstarch, bread, and pasta, must be eliminated.
- Eliminate all legumes, especially soy, beans, and peanuts.
- Eliminate omega-6 rich oils, such as soybean oil, safflower oil, corn oil, peanut oil, and canola oil.
- Eliminate fructose sugars, except from fruits and berries. Drink no sugar-containing beverages.
- Minimize fiber to keep down gut bacterial populations and avoid mechanical injuries to the intestinal wall.
- Minimize other potentially toxic protein sources. In general, protein should be obtained from animal and fish meats, not eggs, dairy, or plants. However, fats from dairy and eggs are highly desirable.
When gut health is restored, dairy and fiber may be restored to the diet. However, the major toxic foods – grains, legumes, omega-6-rich oils, and most fructose – should be eliminated for life.
Filling the Gaps in the Diet
For most people, eliminating grains will leave a large gap in the diet. Foods that should be used to fill that gap include:
- Healthful plant foods are the safe starches, such as white rice, taro, sweet potatoes and yams, and fruits and berries.
- Saturated-fat rich oils and fats, like beef tallow, clarified butter, coconut oil, palm oil, cocoa butter (yes, chocolate desserts are healthy!), along with modest quantities of olive oil and lard. Make homemade salad dressings with these oils, rather than buying supermarket dressings made with soybean or canola oil.
- Further balance the omega-6 to omega-3 ratio by eating low-omega-6 meats, such as the red meats (beef and lamb) and seafood, and eating 1 lb per week salmon or sardines for fresh omega-3 fats.
When the small intestine is damaged, fatty foods may be difficult to tolerate, since the enzymes that digest dietary fats and proteins may also digest human cells. In such cases the diet must focus on starchy foods like rice until bowel health is restored. Be sure to supplement with vitamins and minerals in such cases.
Conclusion
Eliminating food toxins may cure bowel diseases and always improves prognosis. Pedro Bastos of The Paleo Diet Update writes:
From the feedback we have received over the years, IBS patients respond dramatically and rapidly to the Paleo Diet. Their experience indicates that milk, grains and legumes seem to be the main culprits in this condition via a number of mechanisms. [The Paleo Diet Update v.4, #18]
Auto-antibodies generated by wheat against the thyroid, pancreas, and gut typically disappear within 3 to 6 months after removal of wheat from the diet. [25, 26] This is probably a reasonable estimate for the time frame in which bowel disease patients can expect significant improvements from the elimination of dietary food toxins.
Related Posts
Other posts in this series:
- Bowel Disorders, Part I: About Gut Disease July 14, 2010
- Bowel Disease, Part III: Healing Through Nutrition July 22, 2010
- Bowel Disease, Part IV: Restoring Healthful Gut Flora July 27, 2010
References
[1] Fujimura KE et al. Role of the gut microbiota in defining human health. Expert Rev Anti Infect Ther. 2010 Apr;8(4):435-54. http://pmid.us/20377338.
[2] Ruas-Madiedo P et al. Mucin degradation by Bifidobacterium strains isolated from the human intestinal microbiota. Appl Environ Microbiol. 2008 Mar;74(6):1936-40. http://pmid.us/18223105.
[3] Bode L. Human milk oligosaccharides: prebiotics and beyond. Nutr Rev. 2009 Nov;67 Suppl 2:S183-91. http://pmid.us/19906222. Hat tip Dr. Art Ayers.
[4] Ames BN, Gold LS. Paracelsus to parascience: the environmental cancer distraction. Mutation Research 2000 Jan 17; 447(1):3-13. http://pmid.us/10686303
[5] Cummings JH. The effect of dietary fibre on fecal weight and composition. Pp 547–73 in: Spiller GA, ed. Handbook of dietary fibre in human nutrition. 2nd ed. Boca Raton, FL: CRC Press, 1993.
[6] Bernardo D et al. Is gliadin really safe for non-coeliac individuals? Production of interleukin 15 in biopsy culture from non-coeliac individuals challenged with gliadin peptides. Gut 2007 Jun;56(6):889-90. http://pmid.us/17519496.
[7] Drago S et al. Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scand J Gastroenterol. 2006 Apr;41(4):408-19. http://pmid.us/16635908.
[8] Not T et al. Celiac disease risk in the USA: high prevalence of antiendomysium antibodies in healthy blood donors. Scand J Gastroenterol. 1998 May;33(5):494-8. http://pmid.us/9648988.
[9] Sollid LM, Jabri B. Is celiac disease an autoimmune disorder? Curr Opin Immunol. 2005 Dec;17(6):595-600. http://pmid.us/16214317.
[10] Singh MM et al Wheat gluten as a pathogenic factor in schizophrenia. Science. 1976 Jan 30;191(4225):401-2. http://pmid.us/1246624. Dohan FC et al 1984 Is schizophrenia rare if grain is rare? Biol Psychiatry. 1984 Mar;19(3):385-99. http://pmid.us/6609726.
[11] Lorenzsonn V, Olsen WA. In vivo responses of rat intestinal epithelium to intraluminal dietary lectins. Gastroenterology. 1982 May;82(5 Pt 1):838-48. http://pmid.us/6895878.
[12] Sjölander A et al. Morphological changes of rat small intestine after short-time exposure to concanavalin A or wheat germ agglutinin. Cell Struct Funct. 1986 Sep;11(3):285-93. http://pmid.us/3768964.
[13] Mellanby E. (March 15 1919) An experimental investigation on rickets. The Lancet 193(4985):407-412.
[14] Carpenter KJ, Lewin WJ. A critical review: A reexamination of the composition of diets associated with pellagra. J Nutr 1985 May;115(5):543–552. http://pmid.us/3998856.
[15] Biagi F et al. A milligram of gluten a day keeps the mucosal recovery away: a case report. Nutr Rev. 2004 Sep;62(9):360-3. http://pmid.us/15497770.
[16] Kordás K et al. Phytohaemagglutinin inhibits gastric acid but not pepsin secretion in conscious rats. J Physiol Paris. 2001 Jan-Dec;95(1-6):309-14. http://pmid.us/11595455. Pusztai A et al. Kidney bean lectin-induced Escherichia coli overgrowth in the small intestine is blocked by GNA, a mannose-specific lectin. J Appl Bacteriol. 1993 Oct;75(4):360-8. http://pmid.us/8226393. Prykhod’ko O et al. Precocious gut maturation and immune cell expansion by single dose feeding the lectin phytohaemagglutinin to suckling rats. Br J Nutr. 2009 Mar;101(5):735-42. http://pmid.us/18644165.
[17] Pusztai A et al. Inhibition of starch digestion by alpha-amylase inhibitor reduces the efficiency of utilization of dietary proteins and lipids and retards the growth of rats. J Nutr. 1995 Jun;125(6):1554-62. http://pmid.us/7782910.
[18] Haeney MR et al. Soya protein antibodies in man: their occurrence and possible relevance in coeliac disease. J Clin Pathol. 1982 Mar; 35(3):319-22. http://pmid.us/7040491.
[19] IBD in EPIC Study Investigators. Linoleic acid, a dietary n-6 polyunsaturated fatty acid, and the aetiology of ulcerative colitis: a nested case-control study within a European prospective cohort study. Gut. 2009 Dec;58(12):1606-11. http://pmid.us/19628674.
[20] John S et al. Dietary n-3 polyunsaturated fatty acids and the aetiology of ulcerative colitis: a UK prospective cohort study. Eur J Gastroenterol Hepatol. 2010 May;22(5):602-6. http://pmid.us/20216220.
[21] Bergheim I et al. Antibiotics protect against fructose-induced hepatic lipid accumulation in mice: role of endotoxin. J Hepatol. 2008 Jun; 48(6): 983-92. http://pmid.us/18395289.
[22] Stephen AM et al. Effect of changing transit time on colonic microbial metabolism in man. Gut. 1987 May;28(5):601-9. http://pmid.us/3596341.
[23] Quoted in Science Daily, http://www.sciencedaily.com/releases/2006/08/060823093156.htm. Hat tip Dr. Michael Eades.
[24] Burr ML et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989 Sep 30;2(8666):757-61. http://pmid.us/2571009. Hat tip Stephan Guyenet.
[25] Berti I et al. Usefulness of screening program for celiac disease in autoimmune thyroiditis. Dig Dis Sci. 2000 Feb;45(2):403-6. http://pmid.us/10711459.
[26] Mainardi E et al. Thyroid-related autoantibodies and celiac disease: a role for a gluten-free diet? J Clin Gastroenterol. 2002 Sep;35(3):245-8. http://pmid.us/12192201.











Paul,
As always, thank you for the helpful information.
I was given a product called E3 Live, it is an algae that grows only in some part of Oregon (or at least that is my understanding). Do you have any knowledge of this product as far as it having detox properties similar to chlorella?
Also, I had looked into Candida a little and will continue to do so.. I am wondering as candida metabolizes alcohol to acetaldehyde would this lead to vomiting? I almost always vomit after a hard night of drinking. Additionally, it is a sort of joke with family and friends that if anyone is going to get “food poisoning” it is me. A group of people can all eat the exact same meal and I will be the only one to have a bad (read: violent) reaction. As you can imagine this is a slap in the face as I am also the only one in a group that is obsessed with food/nutrition. My mother has decided that it is because I eat “hippie” foods that I have stomach problems and I should just let go and eat junk like the rest of America.. I think she is being at least a little sarcastic.
Best,
Lindsay
Great site, Paul. I was referred her by P. Schoenf. . . RD. Interesting info, great dumpling recipe this week I plan to try. I have the spring roll wrappers waiting to be used in a new way.
Looking forward to perusing more of it.
Sorry to hear of your continued problems, Lindsay, even while eating what sounds like a natural, whole foods diet.
As a specialist with IBS, you still may be having some individual food sensitivities caused by your dysbiosis over the years. Getting adequate Vit D as well to help keep those gut cell junctures tight?
I’ve worked with many clients using the Mediator Release Test to help identify your specific triggers – get rid of them, continue to eat real food, reduce inflammation, heal the gut environment then slowly regain tolerance to foods that may be causing problems now. LEAP/MRT is one protocol that can work wonders for IBS. Jan
Hi Paul,
Great work here in general on your blog and book!
While I certainly agree that wheat is problematic in many ways, I’m confused by how you use the info from Ames and Gold regarding natural plant toxins to support your argument about grains and legumes (not that I necessarily disagree with your argument). I’m also confused as to what Ames and Gold recommend.
Granted this is from a 2006 interview, but Ames says that there are loads of natural plant toxins and then recommends eating less meat and more plants (fruits and vegetables) AND whole grains.
http://www.doctoryourself.com/ames.html
“AMES: You mean about diet? I’d say, “Your Mom knew.” Try and eat a good diet: lots of fruits and vegetables, less meat and more fish. Keep the meat within bounds. I try to never eat meat more than once a day, or even every day. Eat lots of whole grains, not so much refined, well, anything!. Avoid the cookies and white bread. Drink water instead of sugary soft drinks. Get some exercise. Get some sunshine. Your Mom knew all these things.”
So if plant toxins are a problem , why then recommend eating more plants (unless the nutritional benefits outweigh the toxins and/or our bodies can adequately handle the toxins)
And how does his recommendation to eat more whole grains translate into your recommendation to eliminate wheat and other problematic grains (granted while still including safe starches)
I’m not sure what he thinks about legumes
I apologize If I am misunderstanding him and/or you.
Keep up the great work!
Best,
Eric
oops… scratch half of that. I realize now that Ames clearly recommends lots of fruit and vegetables for the vitamins and minerals. So the positives outweigh the negatives of any natural toxins in the fruits and vegetables. So my question then is really about your focus on specifically avoiding the grains and legumes while he recommends whole grains.
Hi eric,
Well, scientists don’t always follow their own findings to a logical endpoint. The main reason is usually that they are specialists and don’t have enough general knowledge to reach valid conclusions.
Think about it from Bruce Ames’s point of view. He is an expert on identifying carcinogens. But cancer is not the whole of diet, and even in cancer we don’t know the optimal diet. So he can say that toxins are bad, but he doesn’t consider himself knowledgeable about the optimal diet. So he follows standard academic opinion.
In fact, plant toxins do a lot more harm than just cancer, and eating a low-toxicity diet of animal foods and safe plant foods is a huge health improvement.
By counseling avoidance of cookies and white bread, I’d say he’s doing OK for a non-expert in diet.
Best, Paul
I was searching for premature babies support group via Google on Wednesday, and I found your page Bowel Disease, Part II: Healing the Gut By Eliminating Food Toxins | Perfect Health Diet to be extremely relevant to premature babies support group. I would like to cooperate with you on my website, so please email me at jeremydurrant@yahoo.com.au if you are interested.
Hi Paul,
I know that white rice is on your list of “safe starches” to eat and luckily, I tolerate rice very well.
I find it very confusing that other diets recommend going low carb/starch free to starve off yeast/bacteria/heal the gut.
I’m trying to heal my leaky gut and potentially have SIBO, I’m wondering if my bodily/gut feedback is enough to tell me that it isn’t doing me any harm.
I know you said each person is different and respond differently and with that said, can I trust that if I don’t react badly to a food that I can safely eat it?
Thanks so much for all you do!
Hi Cherry,
Usually, low carb is good but very low carb is not.
You should experiment, but in SIBO often fructose and FODMAPS are the worst, while starch is well tolerated.
Another thing to try is rice syrup.
Yes, in general if you don’t react badly to a food you should be willing to include it in your diet. Moderation in all things however.
Best, Paul
Thanks so much Paul for your prompt reply!
You hit it on the nose about fructose & FODMAPS, I can’t tolerate those at all.
Can you help explain why rice is such a no-no according to other sources for Leaky guts? Or better, why it works so well. Thanks
Hi Cherry,
Starch takes a little longer to digest, and mainly feeds colonic bacteria. So it is more a problem in ulcerative colitis or other colon problems.
If you don’t eat any glucose, you can’t make gut mucus or maintain immune defenses, and you also don’t maintain a vigorous population of friendly bacteria. So that works against recovery.
You don’t need a lot of starch, but some is helpful.
Hi Paul,
Do you think Carrageenan in personal lubricant products may also be harmful?
-Brad
Hi Paul,
I was wondering aside from eating non-inflammatory foods, what other supplements/protocols are favorable to heal gastritis?
My current plan of attack is:
– aloe vera, DGL, L-glutamine & arabinogalactan powder mixture
– probiotics & kefir
– S.boulardii
– Pepzin GI
– week’s worth of flucanzole (Diflucan)for yeast
I get plenty of rice/sweet potatoes, animal fats/ coconut oil and meat.
Thanks again for all you do,
Cherry
Hi Cherry,
What you’re doing is pretty good … Be well nourished I would say is most important. See our recommended supplements page. The other aspect of nourishment is “eat the part that ails you.” Tripe would be a good food to add to your diet.
Hi again Paul! I’m happy to say that I haven’t had any more episodes of Gastritis attacks- ouch after cleaning up my diet and taking the supplements.
Shortly after my attacks, I started to notice “needle-pricking” sensations in my left lower back after eating. I’ve had my abdominal ultrasounded and everything came back normal.
My GI says it might be a nerve issue. Could Gastritis or food cause this? I do notice that stress makes it spread around to my middle upper back, sometimes my shoulder and leg.
It doesn’t hurt but it’s a small electric shock and itches.
Hi Cherry,
I don’t know what’s causing it, but you might stop the non-food non-micronutrient supplements now (things like aloe vera, fiber, DGL, glutamine).
This is on the principle of first, do no harm.
Cherry, when I go through a period of eating off-diet, with sugar and wheat included, I sometimes experience something very much like you describe. Before I began PHD, I had started developing acid reflux, and this pinpricking feeling would happen quite often. I would experience it on the left side of my back, although higher up, near the bottom of the ribcage. Mine doesn’t reach the level of intrusive pain, but it’s annoying and uncomfortable. After getting back to PHD it disappears in a day or so.
Thanks Peter for your feedback, I’m relieved to know that someone else has experienced the same. Yes, my pricking occurs in that same exact location! It’s been a few months now but I’m hopeful that it will subside while I clean out my system.
I do find that sugar triggers it very quickly or just being stressed so I try not to think about it too much. I was afraid it was my pancreas but ultrasound says I’m clear.
Thanks Peter, acid reflux sounds like a very likely explanation.
Cherry, you might find help from stomach acid supports (salt and bitter herbs with food, maybe betaine hydrochloride supplements with meals); digestive enzymes; removing irritants like the aloe vera from your supplement list; and eating fermented vegetables and dairy.
Paul and Peter, I don’t suffer from any reflex or heartburn, not that I can feel at least and I’m sure it would be something I would feel?
I first felt heartburn from the gastritis and I haven’t felt it since and the sensation was very obvious.
Aloe vera I heard could be bad but some people use it for stomach healing? That’s why I’ve been taking it and have been taking it for a while now without issues that I can feel.
I do take digestive enzymes often but betaine pills didn’t help.
Paul, I took your advance “do no harm” and stopped taking my supplements….and the prickly/needle sensations stop!
It does happen again if I ingest non-paleo/sugary foods but it’s disappeared dramatically. Thanks for your help!!!
Paul
I just found your site via an email from US wellness meats. I am very grateful to have found something else to try. Your research is so interesting. I have ordered your book and can’t hardly wait for it to arrive. I have ulcerative colitis and have had a horrible 6 months. I have been doing SCD/GAPS for nearly 3 years without remission. So many people have been successful. Along the way a gave a go at the Body Ecology Diet and the Guts and Glory program. These all have merit but I have come to realize there is not a one size fits all diet for every pathogen even if the “disease” has the same name. With some experimenting I seem to do very well with white rice, fructose IS a problem for me, and fiber is problematic which I was eating lots of butternut squash,coconut flour, other vegetables and fruit. I have had two stays in the hospital incredible weight loss been on prednisone for 6 months and just started immune suppressant drugs. Last night I did my first DIY fecal transplant using my very healthy 5 yr old nephew for a donor. I don’t know if it’s a placebo effect but I seem to have a bit less pain already. I was not able to retain it as long as I would have liked but do intend to repeat the process a few times over the next 2 weeks. The most frustrating part of my illness is that my menstrual cycle always triggers bowel symptoms and every bad flare has started the same day as my period. I thought maybe endo but nothing was found. I have been on continuous birth control for 3 months to suppress having a cycle but it has not helped my current flare and it has it’s own unpleasant side effects. My cycles have always been bad and now I’m scared to stop taking them but that is my next step. Thanks for all your insights I will continue reading info here till I get the book.
Hi Paul
Regarding one of your comments to Cherry: “Starch takes a little longer to digest, and mainly feeds colonic bacteria. So it is more a problem in ulcerative colitis or other colon problems”, would you recommend that someone with UC avoid safe starches and follow a more strictly paleo diet?
Thank you for your wonderful site.
Suzanne
Hi Adina,
Gut issues are the most challenging ones to address, because you have to eat so you have to feed your pathogens. On the good side there are tools available, from antibiotics and fermented foods to fecal transplants, along with a healthy diet and intestinal/immune supports.
It’s good that you’ve found a source of carbs you tolerate; we all need some carb calories, so finding which is the best for you is a step forward.
I’m not sure what the connection is between your cycles and the bowel symptoms. I’m not that knowledgeable in hormonal interactions with immunity.
Let me know how things go as you improve your diet and supplements. Hopefully the fecal transplants, diet, and nutrition will help. Maybe you can get a doctor to help with the fecal transplants, getting them deeper into the colon where they’ll be more effective.
Best, Paul
Hi Suzanne,
I think it’s best to test them yourself. If they don’t cause trouble for you, it’s better to eat them because they’ll support beneficial flora and nourish you.
If they do cause trouble, then look for pre-digested starches like dextrose powder or rice syrup.
I don’t recommend going very low-carb except as a last resort.
Best, Paul
Hi Paul and Adina,
I have IBD and it also is worst on the first day of my period. I wondered if the uterine contractions might irritate the bowel even more than normal.
Best wishes,
Jacqueline
Jacqueline,
This frustrated me to no end and no GI doc would even listen to me. I have always had painful periods I used to say that being born a girl was my first medical problem (long before a diagnosis of IBD). I kept thinking that my cycles triggered my GI distress. Now I think that GI issues were causing my menstrual issues. After doing a series of DIY fecal transplants I have cycled regularly 5 months in a row (never had that happen) and I don’t have cramps or excessive bleeding. This to me is a miracle. Oh and my UC is in “remission”, though I still have discomfort with elimination at times, I am on no drugs for either issue. I don’t really know why this has happened but my theory is that microbial action was disrupting my bodies efforts to eliminate spent hormones causing them to be reabsorbed and creating hormone imbalances. There is most likely much more to it. Interestingly the clinic in Australia that does fecal transplants don’t use donor stool from women because of excess hormones. I do hope you find relief.
Adina
this study might have something relevant
http://www.ncbi.nlm.nih.gov/pubmed/22841783
Hi Paul
Thank you for your quick response. I wondered about the strict paleo because I also read the testimonial on Robb Wolf’s site from the fellow who reversed his UC by following Robb’s dietary recommendations. My son is the one with UC, and his story is very similar to the young man in the testimonial with the exception that Remicade is not working for him, only resulting in short-lived improvements after each infusion, and he continues to have to take prednisone.
White rice is one side dish that’s often available in his dorm’s dining hall so makes it easier to avoid pizza and other problematic foods.
Suzanne
Hello Paul,
I have my mom with IBS and potentially SIBO, she has diverticular disease also,both in the colon and in the small intestine she has diverticula.She has intermittent diarrhea too. So we are wondering about your recommendation to focus more on starch for those who has trouble in the small intestine than on fats.Does my mother should reduce a lot the fat ingestion or have to reduce it just a few calories from ? We know at the same time fats are essential for intestinal health.
We appreciate so much your work and your advice.
Kind regards,
Christian
Hi Christian,
First, I think a high-fat diet is generally good for bowel diseases (but it must be low in omega-6 fat). This is because gut pathogens cannot metabolize fat, so it doesn’t feed them, but does feed you. There may be exceptions where the gallbladder is not functioning, or pancreatic lipases can damage the digestive tract, but those are rare.
Nevertheless, you need some carbs for optimal health. The sources least likely to feed pathogens are the pre-digested glucose-based sugars: dextrose, rice syrup, tapioca syrup.
Foods you can experiment with. The Specific Carbohydrate Diet, GAPS diet, FODMAPs diet, and others have specific advise about which foods people with gut issues are most likely to have trouble with and which they are more likely to tolerate.
She has to search a bit to find a set of foods that she tolerates that is able to deliver her the optimal nutrient mix.
Along with getting diet right, it’s important to optimize vitamin D levels and to try to diagnose pathogens. Stool tests can identify pathogens and give guidance about possible treatments.
Best, Paul
Thank you very much Paul for your answer. She has tested yesterday and finally she has no SIBO but lactose intolerance. Neither has diverticula in the small intestine , she had misunderstood the last radiography, and her doctor yesterday put in clear she just have diverticula in the colon and IBS.
We are waiting for the supplements you recommend and following the PHD +GAPS guidelines.
We are grateful to you.
Warm Regards
Christian
It’s good that her small intestine is healthy so she can digest simple sugars. Fiber is likely to be harmful, it will feed the colonic pathogens, and starchy foods have a lot of fiber. So PHD+GAPS should be a good combination. I favor glucose based sugars like dextrose, rice syrup, and tapioca syrup. Honey is not bad either. Fat-rich diet is important, but nourishing and low in omega-6.
Best, Paul
the two times i’ve been in the hospital with diverticulitis were after 1) 2 weeks on a 30 day paleo challenge and 2) 10 days on the gaps diet. i do much better with veggies and fruit thrown in, ala the Clean diet by Junger . (actually, do better on SAD diet, come to think of it. at least it doesn’t put me in the hospital after 10 days!) however Paul has talked a few times about the problems of too much undigested protein in the gut, and this rings true for me. i am considering revisiting the gaps diet with digestive enzymes, and slightly different proportions, but maybe i would be crazy to do so…but have to do something , as things are really not right…
oh, and really don’t allow constipation with diverticulitis. in the past magnesium oxcide saved my life, although now i use magnesium citrate. i think it has more effect than just the laxative effect, as both xlax and vit c were less effective at calming the flare down, even though they both moved things along.
Maybe the PHD community can chime in rather than Paul…
Per Paul, “…you need some carbs for optimal health. The sources least likely to feed pathogens are the pre-digested glucose-based sugars: dextrose, rice syrup, tapioca syrup.”
I’d like to experiment with reducing potatos/yucca/rice and using pre-digested glucose instead. But how do you incorporate these into your diet? My only ideas revolve around dessert. I hesitate to go down that route since I’ve finally gotten to the point when I can take or leave sweets and I’m don’t want sugar cravings to rear its ugly head again!
@Elyse,
I also have fears of going down the sugar slope as well. I’ve added rice (and rice syrup) to my diet and I’m not doing well with portion control. I do feel better, however, which I suspect is a ‘carb high’ and a strong liklihood that I’m not nourishing myself quite right yet. I’ll follow any replies with interest.
As far as a recipe idea, rice syrup combines nicely with some broth, rice vinegar, garlic and whatever flavors you like to make a nice sauce to go with a stir fry. You don’t need much.
Hi Elyse & HM,
After doing very low carb for so long, I was worried too. I started with fruit and sweet potatoes and it was hard to stop eating them at first. But now that my diet is more balanced, I have it under control. I think there was an adjustment period. I’m now taking the recommended supplements as well as some of the suggested supplements and am following the PHD guidelines, which have helped. My Omega 6/Omega 3 ratio was way out of balance for a long time. Paul has said the cravings are due to missing nutrients. It’s great to have a balanced diet – carbs, protein & fat – with NO cravings – it’s an amazing feat for me! I feel better and happier and don’t feel deprived. I also do the Intermittent Fasting (16 hour fast with 1 Tbs coconut oil and an 8 hour feeding window) and this has helped me too. Food is less important to me, it really is a lot easier than it sounds (I’m not suffering!) and I choose my foods carefully to get all the nutrients I need in 2 meals with a snack in the 8 hour window.
Sometimes I just have a spoonful of rice syrup to get some carbs. Or you could add it to a homemade salad dressing or drizzle it on some plain yogurt.
Good luck to you both!
HM and Connie,
Thanks so much for getting back to me. I’ve been adding starches to my diet for the past 6 months and find that I am more satisfied and eat far less “treats”– just 1-2 squares of 85% dark chocolate most days. Definitely agree that food just isn’t that big of a deal any more.
However, for how well I take care of myself I should be feeling a heck of a lot better than I do–back pain at night (inflammation?), recent rosiness in my cheeks (rosacea?), constipation, poor sleep (up for an hour at 3 every day not due to stress).
So I continue to tweak and tweak. This week I started intermittent fasting and maybe next I’ll give up potatos and white rice for rice syrup. The problem is that I really have been enjoying the starches and hate to give them up but it just might be what I need to try next. Having that third element/texture in my meals (meat, veggies, starch) has been most satisfying! Also on my list is the Metametrix GI Effects test but I need to first have a grapefruit sized ovarian cyst removed later this month (estrogen problems in past?).
Thanks for your ideas and support!
I would look in your digestion it doesn’t matter what you eat if you don’t digest it. ( HCL supplements and digestive enzymes) and look in your Gallbladder’s and liver’s health (coffee enema and Olive oil Gallbladder flush) You should look into it http://www.youtube.com/watch?v=TDhH1ZTCV_c
http://www.youtube.com/watch?v=qycZ3mfmQBM
Elyse,
If you haven’t seen them already, check out Paul’s posts about those issues – constipation, rosacea, sleep, etc. Maybe some more things to try! Maybe the back pain is related to the large cyst? Shou-Ching, I believe, had ovarian cysts and was helped by the diet.
I did find these interesting articles by Ray Peat which suggests raw carrots. Not sure what Paul thinks about it, but maybe the raw carrots would be a good thing to try. Peat talks about them in both of the following and maybe you can search with google for more:
http://raypeat.com/articles/articles/natural-estrogens.shtml
http://raypeat.com/articles/articles/menopause.shtml
I think I’ve read to eat the raw carrots between meals for optimum results. He suggests eating them shredded with coconut oil and vinegar (more effective this way).
Good luck with everything!
I have just recently had a flare after a year long remission. Once in remission I felt like I could do and eat/drink anything. Now that my flare has taken over my life I am in agony. I take 800mg of Sam-e, 300mg of seratonine, melatonin and GABA. I take omega 3 fish oil and VSL#3. I am up all night long running to the bathroom and don’t get my rest. I am passing only blood and mucous, no normal BM. I have been eating grains, otameal cookies w/o flour and organic sugar, fruits, veggies. I have been eating mayo and some breads, crackers and cheese. After reading the colums I think they are unwise choices. I am at a loss and am in much pain. I refuse to see a MD because I want to heal naturally through seeing my ND.you have any advice?
Hi Lacey,
Please see a doctor. Internal bleeding can be very dangerous.
I would also stop the grains and avoid anything with soybean oil or other seed/grain/legume oils. I assume you know what our dietary recommendations are.
I found this fantastic video that does a great job explaining the harm that grains can do. It’s like a chapter of PHD in a slide show!
I didnt know that all grains (even rice) contain some form of gluten. (from the video I learned that the gluten is in the endosperm which is removed in white rice!). There’s a study mentioned that shows that rice caused an inflammatory response in the bowel. I can’t find the study so I don’t know if the rice was brown or white.
My UC symptoms have become far worse after adding white rice. I never even gave thought that it may be the rice, but as Paul has mentioned, bowel disease diets have to be individualized as a person tolerates each food. I also have a difficult time limiting my intake of rice which may indicate that I should stop it for awhile at least. I guess I’ll be trying grain free PHD. Bye bye sushi 😥
http://www.youtube.com/watch?feature=player_embedded&v=cv5RwxYW8yA#!
I dont agree with cutting out legumes. These foods have many beneficial properties and support good flora, while starving bad flora. Lentils, peas, and beans have resistant starch that support the good flora. If properly prepared (soaking and cooking til soft), they shouldnt be an issue. If it is, then taking a plant based enzyme (with alpha-galactosidase and cellulase) would help, as people with GI issues often have deficiencies in enzymes. Pureeing into a hummus or sauce also helps
I agree with no grains, no dairy, and little starch, but legumes should not be vilified (same with nuts/seeds)
For the past 30 years I have experimented with ‘every possible diet’ and by a process of elimination, and trial and error, i now don’t eat milk protein or eggs, and i avoid grains, gluten and legumes. And everytime i bring some grains and legumes back into my diet, no matter how they are prepared, i end up getting some health problem.
Hi Abby,
Those are all good things to eliminate. You’ve rediscovered Paleo by self-experimentation!
Sir i have since 16years back problem becoz the neglegence of doctors simply i was having jaurdia diagnosed by stool test , but doctor did not gave me proper drug to protect this disease it gets prolonged which turns in to ucerativecollits bcoz of taking high dose ofdrugs which damaged my intestines dear sir i am 40 running i have my majour problem of diahoeria by eating nothing which is not suited fr me please advice me what i to do now i am from j&k state (india) where doctors are meanting money i suffers bcoz of doctor.plz do my help .i have done colonscopy .endoscopy. Sigdomoscopy nw i am totally tired
Hi Rais,
It is difficult to know what advice to give in an advanced case. A good, nourishing diet, fermented foods, and possibly a fecal transplant (or maybe enema) may be reasonable choices.
I would like to add you are wrong on some items.
Cocoa/chocolate will irritate the bowels, Rice is high in fructose, Sweet Potato is high in starch.
Now as good as the GAPTS diet is, it has flaws because it cant cater for everyone. People with IBS do suffer from Gastritis, high fat diet using bone broths for the first stage will irritate the GUT. Bone broth and fat filter works nicely.
I could sit here all day talking about flaws and getting past these, but my point is, you will need to learn your body and understand what works for you and doesn’t, using similar protocols to these.
p.s. HCL can make symptoms worse if your colon is not ready (referring to the GAPT’s protocol).
Great Article.
Thanks for this article Paul. It makes me wonder if the sorghum my sister eats may be the culprit of her unhealed bowel after years on a gluten free diet. She is quite sick and has limited her food to eggs, squash, carrots, and sorghum flour, as they don’t seem to aggravate her digestive tract. Usually you mention other grains but not sorghum. What are your thoughts?
Hi Beth,
Yes, I think sorghum is likely to be a serious problem. White rice is the proper grain to eat.
Her diet is very limited and malnourishing. She should include animal foods of various kinds as well, or dairy if she tolerates that.
Trying to decide whether to take up PHD after a year’s SCD. When I added white rice and potatoes, some symptoms returned that SCD had healed. Is it a transition? It has been about a month since I started breaking SCD rules and the symptoms are still troubling.
Very confusing whom to believe. Our bodies of course tell us more than anyone’s dietary facts; but … so many factors!
On SCD, the starchiest things I ate regularly were winter squash, lima beans, and bananas. I loved the SC diet, felt good. Just experimenting because of the things you say about needing safe starches.
One wierd thing on SCD I lost one dress size the first 2 or 3 months, then stabilized at a good weight. Then about 9 months into the diet, all the fat decided to migrate to my abdomen. This means hormones?? Cortisol?? I don’t know if it was SCD or just being 50.
thanks
Hi Stephanie,
If you get negative symptoms from rice and potatoes, it means you still have a predominance of bad bacteria in your colon and they are feeding on the fiber (resistant starch).
However, in order to build up the population of good bacteria, you need to be eating some of it.
So I would introduce small quantities of potato to your diet, just eat a bit every day, over time this will help the gut flora evolve to something more beneficial.
You can try various tactics to get more good bacteria in (fermented foods, probiotics, ranging up to fecal transplants)
The abdominal fat probably indicates a bit of inflammation / leaky gut. This could be lack of nutrition damaging the integrity of the gut matrix, it could be lack of dietary fiber, it could be some change in gut flora toward a more inflammatory mix. Try adding nourishing foods like bone and joint broth, liver, etc., and continue the flora remodeling effort.
Best, Paul
Hi Paul (and everyone),
I recently read your book and am currently devouring everything on your website. I’ve been paleo for a little over a year and, while it’s helped a LOT, I still have issues that I’m hoping to resolve.
One thing that I was hoping you could help with is a perplexing problem I seem to have with certain fats. I bought Green Pasture’s cod liver/butter oil blend because it was supposed to be SO AMAZING, but it gave me horrible diarrhea. The same thing happened when I started taking MCT oil. No matter how low I went with the either I would get an (explosive!) reaction.
One other thing – I normally use a 50/50 mix of coconut oil and ghee when I cook. I didn’t seem to have any problems, but when I was trying to accustom my body to the MCT oil I cut out the coconut oil and only used the ghee. Could that have something to do with it?
In your article you wrote “When the small intestine is damaged, fatty foods may be difficult to tolerate, since the enzymes that digest dietary fats and proteins may also digest human cells.” Could this be it? Or is there something else going on? I don’t seem to have any problems wiht fats in general. When I was eating low carb paleo it was very high in fat. I still had bowel issues but nothing like the “everyone out!!!” reaction from the FCLO/butter oil or MCT oil.
Thank you so much for all the amazing work you do. You are a superstar!
-Suzanne
Hi Suzanne,
I don’t know why the cod liver/butter oil blend and MCT oil would give you diarrhea but not coconut oil or a coconut oil/ghee blend. It sounds like MCT oil and long omega-3s are both problematic. But I have no idea what could account for that. If it were just MCT oil I would say it was a difficulty handling the short-chain fats, but that wouldn’t explain the cod liver oil. Maybe that is due to some sort of gut bacteria interaction. But that would be just a guess. Does regular cod liver oil do it? Or just the Green Pasture’s product?
It was just the blend. I also had problems while taking the MCT oil, along with a lot of ghee (which has short chain fats, rights?) I didn’t have any problems while taking straight fish oil.
But why would I have problems with short chain fats??? I thought they were soooo easy to disgest, that the cells were able to metabolize them directly?
No, short-chain fats have a different digestive process — they are transported to the liver separately from other fats. They are relatively difficult to digest. You may be thinking of even shorter fats like butyrate produced by gut bacteria, which are taken up directly by colonic cells.
So if it *is* the short chain fats, which it seems like it is, is there anything I can do so I can eventually take them? Could it be that I need to heal my small I intestine? Or am I just going to have to avoid these oils. I do have a tendency to a I’d reflux, which is generally much better on paleo…
And thank you so much for taking the time to answer this question!
paul,i have been taking black cumin oil for last 4 months,i think i read somewhere you were suffering from candida infection,i was in pubmed reading about black cumin seed oil(Nigella sativa)and how it was shown to help with candida infections,if you could look at paragraph 5.2 of this article and comment on it,it might be a benefit to your readers that are suffering with this problem http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3642442/ also i have been taking amla powder(Emblica Officinalis) also known as amalaki,i am sure it is what is regulating my blood sugars and might be useful for people that are diabetic or pre-diabetic,,,your comments on these completely natural plants would much appreciated…….leo
Hey Paul,
Ever since I was 12 years old I have been struggling with fructose malabsorption. Most of the doctors I have gone to have said this is a functional gut problem as in I lack the enzyme required to digest fructose. They have said that due to not being digested fast enough by enzymes the fructose just sits there and causes issues with gut bacteria. Do you think this is likely or is a small bowel infection and perhaps other infections a more likely problem with me? I recently got the Metametrix stool test done and am awaiting the results.
I am truly worried that I will have to avoid even small amounts of fructose for life.
Thanks
Hi Paul. I recently finished a 7 month long GAPS diet with my family (November 2012-May 13). My 7 yr old daughter has ADD and food intolerances (gluten casein), severe allergy to fire ants, and has needed to be on antibiotics on and off due to various infections. I have a number of health issues including migraines, lifelong acne (treated with Accutane as a teenager), lifelong bladder infections (treated with antibiotics on and off since age 4), kidney infection 3 years ago, and recently IBS including pain in lower left abdomen, heartburn and constipation. Yikes! So we tried GAPS and my headaches are much better, but my IBS issues are the same if not worse, and my daughter was more stable on GAPS but seemed low energy at times. So now I could really use some help deciding what to do next. I read your book and we have started eating rice again (which has been wonderful… I am half Korean and 7 months without rice was a challenge!!) but my IBS is still challenging me and I noticed if my daughter eats too much rice (and/or rice flour products) her hyperactivity returns. I have been trying very hard to heal our health but am feeling like I don’t know what to do. Any advise or suggestions would be very appreciated.
Use the clay and HCL when you eat http://www.youtube.com/watch?v=c3NHHQFA7dY
And coffee enema to detox the liver
http://www.youtube.com/watch?v=qycZ3mfmQBM
and keep up on the diet
You might need to tweak PHD with some other changes as well.
Norm Robillard thinks resistant starch can be a problem for some, so he advocates only eating Jasmine or sushi rice, low amylose potatoes and has some other things to be aware of
http://fasttractdigestion.com/
then there are the FODMAPS to consider. I have heard this was a good book
http://www.amazon.com/IBS-Change-Carbs-FODMAP-Elimination/dp/0982063520/ref=sr_1_2?s=books&ie=UTF8&qid=1376830317&sr=1-2&keywords=low+fodmap+diet
Paul, just to clarify your recommendations for Gastritis from the article.
1)Heavy Cream would be ok since it has no dairy proteins right?
2)Potatoes are not ok since it is a nightshade and Yams are ok right?
3)Grass Fed Butter not ok but clarified butter is ok
I have a question regarding gluten free steel cut oats. If you soak your oats overnight with added whey, do you think they are safe? I believe this soaking is supposed to break down the phytates in the oats. I am having trouble with constipation and eating soaked oats seems to help this, but I also have gastritis and don’t want to further irritate my stomach lining.
Thank you so much for your help.