Mario Renato Iwakura’s guest series on the place of iodine and selenium supplementation in treatment of hypothyroidism continues. This is part 2. Thank you Mario! – Paul
UPDATE November 2023: Since this article was written, PHD recommendations for iodine have become firm. We recommend consistent daily supplementation in the range of 150 to 225 micrograms (not milligrams) per day, plus frequent seafood consumption. The supplementation (a) ensures a healthful supply of iodine and (b) accustoms the thyroid to the presence of iodine which minimizes the risk of thyroid injury from intake of a large amount of iodine at once, possibly at a time of selenium deficiency, for example from an all-you-can-eat crab buffet. Supplementation of >1 mg high doses of iodine carries a high risk of thyroid injury, making some parts of the thyroid hypothyroid and possibly also creating nodules with hyperthyroid activity. … Although our recommendations are not in line with Mario’s, nevertheless Mario’s article is fascinating, and a few people have reported benefit from high-dose iodine. Please read his article and judge for yourself! Best, Paul
In Part I (Iodine and Hashimoto’s Thyroiditis, Part I, May 24, 2011) we looked at evidence from animal studies that iodine is dangerous to the thyroid only when selenium is deficient or in excess, and that optimizing selenium status allows the thyroid to tolerate a wide range of iodine intakes. In fact, there were some hints (such as an improved CD4+/CD8+ T cell ratio) that high iodine, if coupled with optimal selenium, might actually diminish autoimmunity.
If that holds in humans too, we should expect that populations with healthy selenium intakes should see a low incidence of thyroid disease and no effect from iodine intake on the incidence of Hashimoto’s thyroiditis. Is that the case?
Korean Study
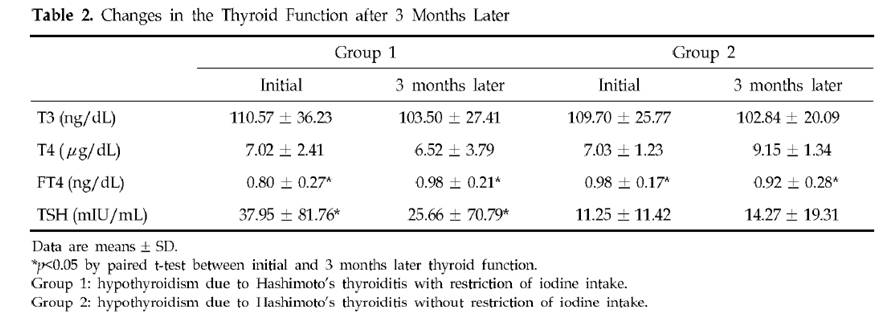
Dr. K [1] quotes a Korean study [3] of Hashimoto’s patients. Half restricted iodine intake to less than 100 mcg/day, the other half ate their normal seaweed and iodine. Of the 23 patients who restricted iodine, 18 (78%) became euthyroid in the sense of having TSH below 4.43 mIU/L, while only 10 (46%) of the 22 that did not restrict iodine became euthyroid. There was no measurement of symptoms at all, and no report of thyroid antibody titers after iodine restriction, so we don’t know if the iodine restriction relieved the underlying autoimmune disorder.
The selection of subjects for the two groups was odd. Group 1, the iodine restricted patients, had an extremely wide range of starting TSH, averaging 38 mIU/L but with a standard deviation of 82 mIU/L. Since all subjects began with TSH above 5 mIU/L, it’s clear that many of the Group 1 members had TSH near 5 and others had TSH well over 100 mIU/L. In comparison, Group 2, the controls, averaged a TSH of 11 mIU/L with a standard deviation of 11 mIU/L – less than 1/7 the standard deviation of Group 1. Few Group 2 members had a TSH above 30.
Table 2 presents the results. Mean TSH in Group 1 was reduced a little, but it did not even come close to normal. Since 78.3% of Group 1 had TSH below 4.43 mIU/L after 3 months, the other 21.7% had to have averaged a TSH above 102.2 mIU/L at the conclusion of the study. The standard deviation of Group 1 TSH at the end of 3 months of iodine restriciton was 71 mIU/L.
Meanwhile, Group 2 members still had a much lower standard deviation at the end of the study: 19 mIU/L.
A conclusion of this study was that “the initial serum TSH concentration was significantly lower in the recovered patients than in the non-recovered patients, which suggests that the possibility of recovvery is increasingly rare as the initial hypothyroidism becomes more severe.” Since Group 1 originally had a much larger fraction of members with very low TSH than Group 2 (plus a few with extremely high TSH to raise the average TSH), and the definition of recovery was a reduction of TSH to 4.43, perhaps it is not surprising that a higher fraction of Group 1 recovered.
Further calling into question the conclusion that lower iodine intake is beneficial is another observation. Looking at Table 1, we see that Group 2 (controls) had, at baseline, much higher iodine intake and higher urinary iodine excretion. Despite this, goiter size, TSH, antimicrosomal (MSAb) and antithyroglobulin (TGAb) antibodies were all lower!
A Japanese Study
A similar study with similar results was done in Japan [4].
In Asia, high iodine intake is due to high consumption of seaweed. Seaweed is high in naturally produced bromine compounds [5][6][7], arsenic [9][12][13], and mercury [9], and can accumulate radioactive iodine [8][9][10][11]. All these substances are known to interfere with thyroid function.
Bromide levels in urine in Asia are very high and are associated with seaweed consumption [6][7]. Values of 5 to 8.1 mg/l have been observed among Japanese, and 8 to 12 mg/l among Koreans.
It is quite possible that any benefits from “iodine restriction,” i.e. seaweed restriction, were due to reduced intake of bromine, arsenic, mercury, and radioactive iodine.
A China Study
Dr. Kharrazian [2] cites a study done in China [14] comparing three different areas: one with iodine deficiency (Panshan), another where iodine is more than adequate (Zhangwu) and a third where iodine is excessive (Huanghua). More than adequate and excessive iodine was associated with increased risk for subclinical and overt hypothyroidism.
But, another study [15], done in the same regions, showed that, coincidentally, Huanghua, the region with excessive iodine, and Zhangwu, the region with more than adequate iodine, had lower median serum selenium concentrations than Panshan, where iodine was deficient. Blood selenium concentrations were 83.2, 89.1 and 91.4 microg/L, respectively. So iodine consumption was inversely related to selenium consumption. Was it lower iodine, or higher selenium, that was beneficial?
TPOAb antibody levels were inversely associated with selenium levels. Patients with the highest TPOAb antibodies (>600 UI/ml) had lower selenium levels than patients with moderate and lower TPOAb antibodies (respectively 83.6, 95.6 and 92.9 UI/ml). [15]
Studies from Brazil, Sri Lanka, Turkey, and Greece
Dr K also cites a rise in Hashimoto’s incidence in Brazil, Sri Lanka, Turkey and Greece after salt iodinization began. Are these countries deficient in selenium? Well, lets see:
Brazil: The study was done in São Paulo, a city with a large Brazilian-Japanese population. Brazilian-Japanese have significant lower levels of Se than Japanese living in Japan [16].
Greece: Selenium status is one of the lowest of the Europe [17].
Turkey: Selenium status of Turkish children is found to be unusually low, only 65 ng/ml in boys and 71 ng/ml in girls [18]. Turkey is characterized by widespread iodine deficiency and marginal selenium deficiency [19].
Sri Lanka: Significant parts of the Sri Lankan female population may be selenium deficient [20].
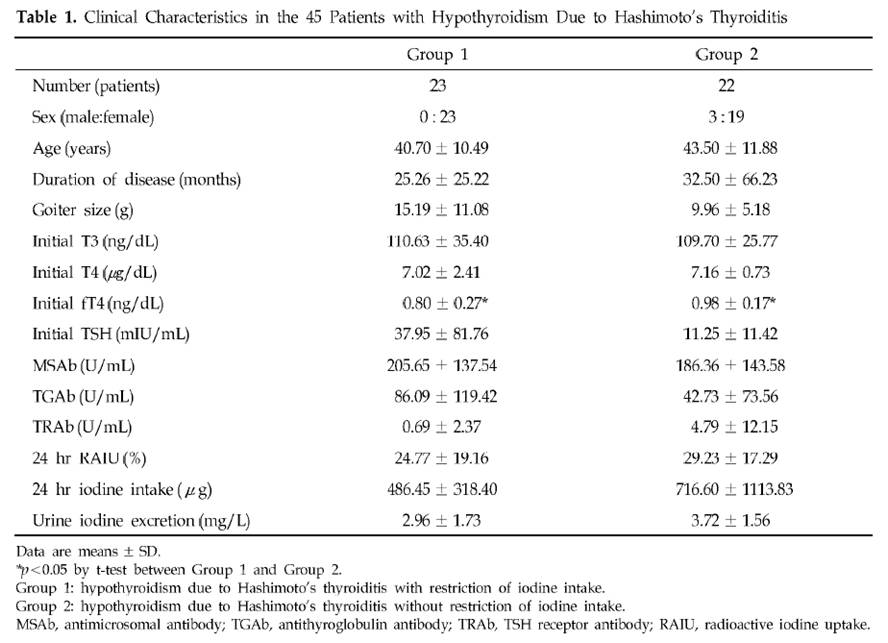
One study, done in Egypt, measured iodine excretation in urine and its relation with thyroid peroxidase antibody (TPOAb) [21]. Although the abstract said that a significant correlation was found, this is far from reality, as we can see from Fig. 2.
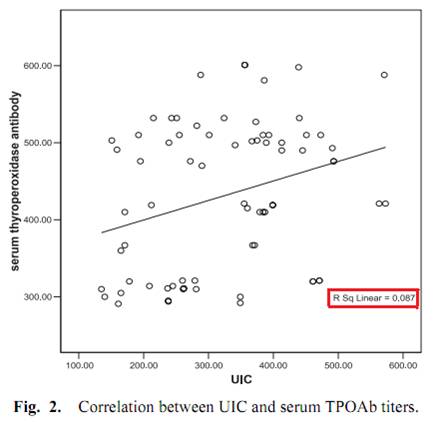
Another study from Brazil [2] measured urinary iodine excretation and serum TPOAb and TgAb antibodies from 39 subjects with Hashimoto’s, none of whom were receiving treatment at the time of the study. Both antibody titers had no obvious correlation with urinary iodine.
Two discordant epidemiological studies
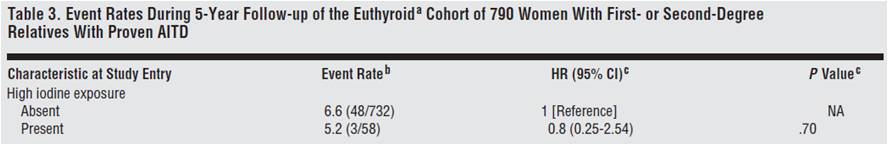
From the Netherlands, we have a prospective observational study looking at whether the female relatives of 790 autoimmune thyroid disease patients would progress to overt hypothyroidism or hyperthyroidism [22].
Although the relationship was not considered statistically significant, they found that women with high iodine intake (assessed through questionnaires) were 20% less likely to develop thyroid disorders.
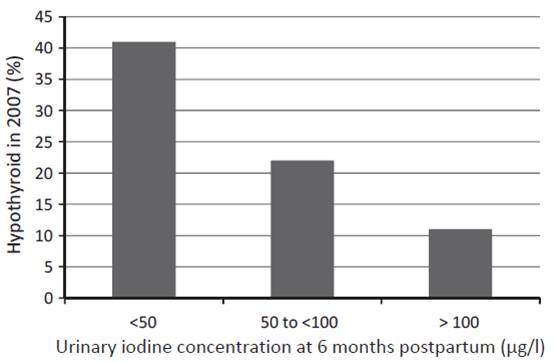
Another study from western Australia (a region that has previously been shown to be iodine replete) measured urinary iodine concentration (UIC) of 98 women at 6 months postpartum and checked their thyroid status both postpartum and 12 years later [23]. UIC at 6 months postpartum predicted both postpartum thyroid dysfunction and hypothyroidism 12 years later:
The researchers concluded:
The odds ratio (OR) of hypothyroid PPTD with each unit of decreasing log iodine was 2.54, (95%CI: 1.47, 4.35), and with UIC < 50 lg/l, OR 4.22, (95%CI: 1.54, 11.55). In the long term, decreased log UIC significantly predicted hypothyroidism at 12-year follow-up (p = 0.002) … The association was independent of antibody status.
In short, the more iodine being excreted (and thus, presumably, the more in the diet and in the body), the less likely were hypothyroid disorders – not only at the time, but also 12 years later.
Dangers of selenium supplementation in iodine deficiency.
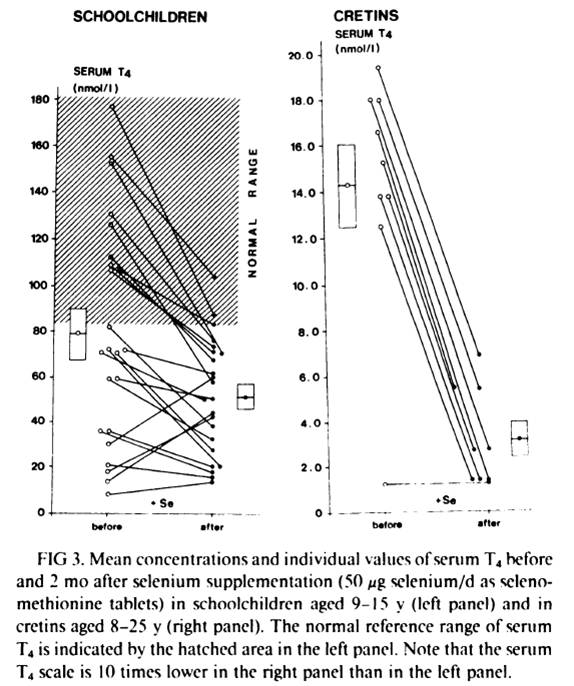
Selenium supplementation when iodine and selenium deficiencies are both present can be dangerous, as the experience in northern Zaire, one of the most severely iodine and selenium deficient population in the world, shows [25].
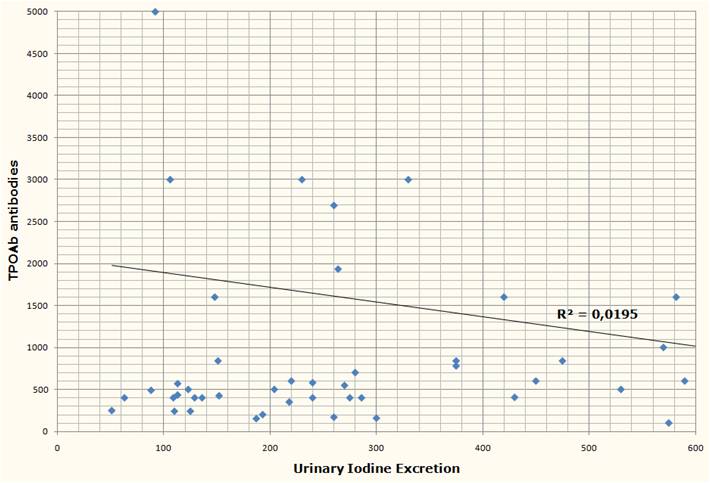
Schoolchildren and cretins were supplemented for 2 months with a physiological dose of selenium (50 mcg Se per day as selenomethionine). Serum selenium was was very low at the beggining of the study and was similar in schoolchildren and in cretins (343 +- 190 nmil/L in schoolchildren, n=23, and 296 +- 116 nmol/L in cretins, n=9). After 2 months of selenium supplementation, the massive decrease in serum T4 in virtually every subject can be seen in fig. 4 below:
In schoolchildren, serum free thyroxin (fT4) decreased from 11.8 +- 6.7 nmol/L to 8.4 +- 4.1 nmol/L (P<0.01); serum reverse triiodothyronine (rT3) decreased from 12.4 +- 11.5 nmol/L to 9.0 +- 7.2 nmol/L; mean serum T3 and mean TSH remained stable. In cretins, serum fT4 remained the same or decreased to an undetectable level in all nine cretins; mean serum T3 decreased from 0.98 +- 0.72 nmol/L to 0.72 +- 0.29 nmol/L, and two cretins who were initially in a normal range of serum T3 (1.32-2.9 nmol/L) presented T3 values outside the lower limit of normal after selenium supplementation; mean serum TSH increased significantly from 262 mU/L to 363 mU/L (p<0.001).
Another previous similar trial, this time done in 52 schoolchildren, reached the same results: a marked reduction in serum T4 [26][27]. This previous trial “was shown to modify the serum thyroid hormones parameters in clinically euthyroid subjects and to induce a dramatic fall of the already impaired thyroid function in clinically hypothyroid subjects” [27].
What stands out is the difference in the results between euthyroid schoolchildren and cretins/hypothyroids. Two months of selenium supplementation was probably not enough time to affect significantly the thyroid of the euthyroid schoolchildren (althougt already impacted T4 and fT4). But, in cretins and hypothyroids, where the thyroid was already more deficient, the impact was evident.
Conclusion and What I Do
Iodine and selenium are two extremely important minerals for human health, and are righly emphasized as such in the Perfect Health Diet book and blog. I believe they are fundamental to thyroid health and very important to Hashimoto’s patients.
A survey of the literature suggests that Hashimoto’s is largely unaffected by iodine intake. However, the literature may be distorted by three circumstances under which iodine increases may harm, and iodine restriction help, Hashimoto’s patients:
- Selenium deficiency causes an intolerance of high iodine.
- Iodine intake via seaweed is accompanied by thyrotoxic metals and halides.
- Sudden increases in iodine can induce a reactive hypothyroidism.
All three of these negatives can be avoided by supplementing selenium along with iodine, using potassium iodide rather than seaweed as the source of iodine, and increasing iodine intake gradually.
It’s plausible that if iodine were supplemented in this way, then Hashimoto’s patients would experience benefits with little risk of harm. Anecdotally, a number have reported benefits from supplemental iodine.
Other evidence emphasizes the need for balance between iodine and selenium. Just as iodine without selenium can cause hypothyroidism, so too can selenium without iodine. Both are needed for good health.
A few months after I was diagnosed with Hashimoto’s I started 50 mg/day iodine plus 200 mcg/day selenium. If I were starting today, I would follow Paul’s recommendation to start with selenium and a low dose of iodine, and increase the iodine dose slowly. I would not take any kelp, because of potential thyrotoxic contaminants.
Currently I’m doing the following to try to reverse my Hashimoto’s:
- PHD diet and follow PHD book and blog advices to enhance immunity against infections, since infections seems to be implicated in Hashimoto’s pathology [28][29][30]. I give special attention to what Chris Masterjohn calls “traditional superfoods”: liver and other organs, bones and marrow, butter and cod liver oil, egg yolks and coconut, because these foods are high in minerals, like iodine, zinc, selenium, copper, chromium, manganese and vanadium, all of which seems to play a role in thyroid health [31];
- High dose iodine (50mg of Lugol’s) plus 200 mcg selenium daily. These I supplement because of their vital importance to thyroid and immune function;
- 3 mg LDN (low dose naltrexone) every other day to further increase immunity. LDN resources are listed below [32][33][34][35][36];
- Avoiding mercury and other endocrine disruptors. When I removed 9 amalgams (mercury), my TPO antibodies increased for 3 months and took another 6 months to return to previous values. I also avoid fish that have high and medium concentrations of mercury. Cod consumption increased my TPO antibodies;
- 1g of vitamin C daily. Since it seems to confer some protection against heavy metal thyroid disfunction [37], improve thyroid medication absorption [38] and there is some evidence that it could improve a defective cellular transport for iodine [39];
- Donating blood 2 to 3 times per year. In men, high levels of iron seems to impact thyroid function [40].
Final Thanks
I would like to make a special thanks to Paul Jaminet for giving me the opportunity to write this essay, for gathering many, many papers for me, and for having the patience to revise both posts and suggest many changes that made the text clearer; and to Emily Deans who kindly sent me one key study that Paul could not get.
References:
[1] Dr Datis Kharrazian. Iodine and Autoimmune Thyroid — References. http://drknews.com/some-studies-on-iodine-and-autoimmune-thyroid-disease/.
[2] Marino MA et al. Urinary iodine in patients with auto-immune thyroid disorders in Santo André, SP, is comparable to normal controls and has been steady for the last 10 years. Arq Bras Endocrinol Metabol. 2009 Feb;53(1):55-63. http://pmid.us/19347186.
[3] Yoon SJ et al. The effect of iodine restriction on thyroid function in patients with hypothyroidism due to Hashimoto’s thyroiditis. Yonsei Med J. 2003 Apr 30;44(2):227-35. http://pmid.us/12728462.
[4] Kasagi K et al. Effect of iodine restriction on thyroid function in patients with primary hypothyroidism. Thyroid. 2003 Jun;13(6):561-7. http://pmid.us/12930600.
[5] Gribble GW. The natural production of organobromine compounds. Environ Sci Pollut Res Int. 2000 Mar;7(1):37-47. http://pmid.us/19153837.
[6] Zhang ZW et al. Urinary bromide levels probably dependent to intake of foods such as sea algae. Arch Environ Contam Toxicol. 2001 May;40(4):579-84. http://pmid.us/11525503.
[7] Kawai T, Zhang ZW et al. Comparison of urinary bromide levels among people in East Asia, and the effects of dietary intakes of cereals and marine products. Toxicol Lett. 2002 Aug 5;134(1-3):285-93. http://pmid.us/12191890.
[8] Leblanc C et al. Iodine transfers in the coastal marine environment: the key role of brown algae and of their vanadium-dependent haloperoxidase. Biochimie. 2006 Nov;88(11):1773-85. http://pmid.us/17007992.
[9] van Netten C et al. Elemental and radioactive analysis of commercially available seaweed. Sci Total Environ. 2000 Jun 8;255(1-3):169-75. http://pmid.us/10898404.
[10] Hou X et al. Iodine-129 in human thyroids and seaweed in China. Sci Total Environ. 2000 Feb 10;246(2-3):285-91. http://pmid.us/10696729.
[11] Toh Y et al. Isotopic ratio of 129I/127I in seaweed measured by neutron activation analysis with gamma-gamma coincidence. Health Phys. 2002 Jul;83(1):110-3. http://pmid.us/12075675.
[12] Miyashita S, Kaise T. Biological effects and metabolism of arsenic compounds present in seafood products. Shokuhin Eiseigaku Zasshi. 2010;51(3):71-91. http://pmid.us/20595788.
[13] Cleland B et al. Arsenic exposure within the Korean community (United States) based on dietary behavior and arsenic levels in hair, urine, air, and water. Environ Health Perspect. 2009 Apr;117(4):632-8. Epub 2008 Dec 8. http://pmid.us/19440504.
[14] Chong W, Shit Xg, Teng WP, et al. Multifactor analysis of relationship between the biological exposure to iodine and hypothyroidism. Zhongua Yi Za Zhi. 2004 Jul 17:84(14):1171-4. http://pmid.us/15387978.
[15] Tong YJ et al. An epidemiological study on the relationship between selenium and thyroid function in areas with different iodine intake. Zhonghua Yi Xue Za Zhi. 2003 Dec 10;83(23):2036-9. http://pmid.us/14703411.
[16] Karita K et al. Comparison of selenium status between Japanese living in Tokyo and Japanese brazilians in São Paulo, Brazil. Asia Pac J Clin Nutr. 2001;10(3):197-9. http://pmid.us/11708308.
[17] Thorling EB et al. Selenium status in Europe–human data. A multicenter study. Ann Clin Res. 1986;18(1):3-7. http://pmid.us/3717869.
[18] Mengüba? K et al. Selenium status of healthy Turkish children. Biol Trace Elem Res. 1996 Aug;54(2):163-72. http://pmid.us/8886316.
[19] Hincal F. Trace elements in growth: iodine and selenium status of Turkish children. J Trace Elem Med Biol. 2007;21 Suppl 1:40-3. http://pmid.us/18039495.
[20] Fordyce FM et al. Selenium and iodine in soil, rice and drinking water in relation to endemic goitre in Sri Lanka. Sci Total Environ. 2000 Dec 18;263(1-3):127-41. http://pmid.us/11194147.
[21] Alsayed A et al. Excess urinary iodine is associated with autoimmune subclinical hypothyroidism among Egyptian women. Endocr J. 2008 Jul;55(3):601-5. Epub 2008 May 15. http://pmid.us/18480555.
[22] Strieder TG et al. Prediction of progression to overt hypothyroidism or hyperthyroidism in female relatives of patients with autoimmune thyroid disease using the Thyroid Events Amsterdam (THEA) score. Arch Intern Med. 2008 Aug 11;168(15):1657-63. http://pmid.us/18695079.
[23] Stuckey BG et al. Low urinary iodine postpartum is associated with hypothyroid postpartum thyroid dysfunction and predicts long-term hypothyroidism. Clin Endocrinol (Oxf). 2011 May;74(5):631-5. doi: 10.1111/j.1365-2265.2011.03978.x. http://pmid.us/21470286.
[24] American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Evaluation and Treatment of Hyperthyroidism and Hypothyroidism. https://www.aace.com/sites/default/files/hypo_hyper.pdf.
[25] Vanderpas JB et al. Selenium deficiency mitigates hypothyroxinemia in iodine-deficient subjects. Am J Clin Nutr. 1993 Feb;57(2 Suppl):271S-275S. http://pmid.us/8427203.
[26] Contempré B et al. Effect of selenium supplementation on thyroid hormone metabolism in an iodine and selenium deficient population. Clin Endocrinol (Oxf). 1992 Jun;36(6):579-83. http://pmid.us/1424183.
[27] Contempré B et al. Effect of selenium supplementation in hypothyroid subjects of an iodine and selenium deficient area: the possible danger of indiscriminate supplementation of iodine-deficient subjects with selenium. J Clin Endocrinol Metab. 1991 Jul;73(1):213-5. http://pmid.us/2045471.
[28] Benvenga S et al. Homologies of the thyroid sodium-iodide symporter with bacterial and viral proteins. J Endocrinol Invest. 1999 Jul-Aug;22(7):535-40. http://pmid.us/10475151.
[29] Wasserman EE et al. Infection and thyroid autoimmunity: A seroepidemiologic study of TPOaAb. Autoimmunity. 2009 Aug;42(5):439-46. http://pmid.us/19811261.
[30] Tozzoli R et al. Infections and autoimmune thyroid diseases: parallel detection of antibodies against pathogens with proteomic technology. Autoimmun Rev. 2008 Dec;8(2):112-5. http://pmid.us/18700170.
[31] Neve J. Clinical implications of trace elements in endocrinology. Biol Trace Elem Res. 1992 Jan-Mar;32:173-85. http://pmid.us/1375054.
[32] David Gluck, MD. Low Dose Naltrexone information site. http://www.lowdosenaltrexone.org/.
[33] LDN Yahoo Group. http://groups.yahoo.com/group/lowdosenaltrexone/.
[34] LDN World Database. Where LDN users share their experience with various diseases. http://www.ldndatabase.com/.
[35] Those Who Suffer Much Know Much. A colection of LDN users testimonies. http://www.ldnresearchtrustfiles.co.uk/docs/2010.pdf.
[36] Elaine A. More. The Promise Of Low Dose Naltrexone Therapy: Potential Benefits in Cancer, Autoimmune, Neurological and Infectious Disorder. http://www.amazon.com/Promise-Low-Dose-Naltrexone-Therapy/dp/0786437154.
[37] Gupta P, Kar A. Role of ascorbic acid in cadmium-induced thyroid dysfunction and lipid peroxidation. J Appl Toxicol. 1998 Sep-Oct;18(5):317-20. http://pmid.us/9804431.
[38] Absorption of thyroid drug levothyroxine improves with vitamin C. The Endocrine Society. News Room. http://www.endo-society.org/media/ENDO-08/research/Absorption-of-thyroid-drug.cfm.
[39] Abraham, G.E., Brownstein, D.. Evidence that the administration of Vitamin C improves a defective cellular transport mechanism for iodine: A case report. The Original Internist, 12(3):125-130, 2005. http://www.optimox.com/pics/Iodine/IOD-11/IOD_11.htm.
[40] Edwards CQ et al. Thyroid disease in hemochromatosis. Increased incidence in homozygous men. Arch Intern Med. 1983 Oct;143(10):1890-3. http://pmid.us/6625774.












Hi Paul, with regards to my iodine dosage.
yep i know, i’m a naughty boy…:)
i have done a bit of experimenting on the iodine front.
Initially i was taking iodine drops &/or pills in the form of potassium iodide & i was indeed having hyper-type reactions to very small doses, even to 150mcg.
So i read some more & found that some people react to potassium iodide & some of the reactions matched mine.
to test this further i decided to do an experiment, i gave myself about 15mg of Potassium Iodide drops (which equated to 11.5mg iodine & 3.5mg iodide in the brand i used).
The result was;
1. definite: quite a few (slightly raised) red spots appeared on stomach (1st noticed 5 hours post dose).
2. probable: diarrhoea (but could have been unrelated).
So, i read some more, & found Iosol getting good feedback. Iosol does not contain Potassium Iodide, it uses Ammonium Iodide instead.
So i have been trying that, the only reaction i get is potentially diarrhoea with higher doses, the higher the dose the looser the stool.
I mentioned above that my dose since starting has average around 12mg per day.
My current dose is 7.2mg to 9mg (4 or 5 drops) per day, this alleviates the stool issues, esp if taken when there is food in the stomach.
Paul, with regards to the TSH blood test.
You mention the adaption period to a new Iodine dose.
Would you surmise that every time you increase iodine an increase in TSH will result.
I guess where i am heading is; how long would the TSH take to drop & stabilise once you stop changing the iodine dose. & hence how long should you wait before taking a TSH blood test (& thus get a true & hopefully much lower reading).
ps. do you think i am okay to continue taking the 4 or 5 drops of Iosol per day (7.2mg to 9mg) given that i am not having any adverse reactions to it?
Hi Darrin,
Yes, an increase in TSH is the usual first reaction.
Sometime after 4 weeks should give you a reasonable reading, I might go 6.
Yes, now that you’ve done it for several weeks I would just continue this dose. Looks like you’ve saved yourself some time.
Interesting about the ammonium iodide, thanks for the tip.
Can anyone recommend a good place to have testing done for hypo and hyper thryoid?
Thank you!
Hi Sally,
Any doctor’s office can do it. If you want to order your own, there are some suggestions in this article: http://thyroid.about.com/od/gettestedanddiagnosed/a/selftesting.htm.
Best, Paul
Hi Paul,
is there any explanation as to why a rise in TSH usually follows the addition or increase in iodine supplementation….what’s the mechanism?
Reading Colpo’s latest article and it was pertinent to this topic.
http://anthonycolpo.com/?p=1743
Basically, low carb lowers thyroid’s T3. He also mentioned lowering his iron to teenager levels made a change from insulin resistent to sensitive and now he’s high or at least higher carb …maybe 55% or more (above PHD plateau range limit) and thriving on high carb diet (PHD without dairy it seems to me). However, Colpo appears solely focused on athletes whom PHD says needs higher carbs, but Colpo goes further. The T3 connection was interesting. How does that influence this iodine/selenium and T3 discussion?
You guys ask tough questions. When I first started the blog the questions were usually easy. Now they’re all complex biology.
Darrin, there are some complex adaptations in the thyroid when iodine levels increase. I gave a brief discussion in this post: http://perfecthealthdiet.com/?p=2721.
Jay, I haven’t fully explored this literature but it looks like I will have to. Not all low-carb dieters experience lower T3. It would be interesting to understand the circumstances and biology.
Jaybird,
Thank you for the article. Very interesting, since my rT3 was high and I have been on a low carb diet (under 50 grams daily) for a year now. The first 5 months was low carb and low calorie. Now I guess I will have to experiment with adding back carbs and see. In the past they have made me gain weight quickly but I guess it’s worth a try.
Jaybird,
I do not have the time or will to refute Colpo’s intire article, but let’s have a look on his first example, the Vermont long term study:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC371281/pdf/jcinvest00683-0196.pdf
“The long-term study of fat overfeeding included four subjects studied before and after overeating fat for 3 mo. The excess fat in these diets averaged 895 kcal/d consisting of margarine, corn oil, a corn oil colloidal suspension, and fat enriched soups and cookies.”
Excess of omega 6 impacts the thyroid as explained by Stephan Guyenet in this article:
http://wholehealthsource.blogspot.com/2008/12/omega-6-linoleic-acid-suppresses.html
I have briefly read his article, and most, if not all, of his examples where either calorie restricted, short time or the fat used was not PHD approved…
And his last example, the short time study from Ullrich:
http://www.ncbi.nlm.nih.gov/pubmed/3900181
“One diet was high in polyunsaturated fat (HF), with 10%, 55%, and 35% of total calories derived from protein, fat, and carbohydrate, respectively.”
*** Reading Colpo’s latest article and it was pertinent to this topic. http://anthonycolpo.com/?p=1743 Basically, low carb lowers thyroid’s T3. ***
Broda Barnes also felt that a ketogenic low carb diet was not good for the thyroid, but that 50g of carbs daily was enough to keep the thyroid functioning. That’s still *low* by most standards.
But one reads in Colpo’s article:
“I still think non-ketogenic low-carbohydrate diets are a worthy option for diabetic and sedentary folks.”
as well as:
” After reviewing the research, I’m also convinced that low carb diets are not a bright choice for those susceptible to or suffering from impaired thyroid function.”
Hmmm, so I wonder what he recommends for someone who is BOTH diabetic AND suffering from impaired thyroid function???
I don’t know what he means by: ” I had successfully reduced my serum ferritin (a reliable marker for bodily iron levels) to the average levels of a teenager. Doing so has been shown to cause significant improvements in insulin sensitivity and glycemic control in both diabetic and non-diabetic folks.”
What is the average level of a teenager? I’m busily trying to RAISE my ferritin level, which was measured at 23 in a recent test, as both my medical practitioner and all my internet reading indicate you want it to be at least 70 for your thyroid to function properly.
I think I’m about to give up and just eat whatever I damn well please. Too much contradictory information overload. 🙂 🙂
Paul and Mario thanks for the response. Mario, excellent point. Looks like omega-6 strikes again. Wouldn’t it be great if PHD could be one of the study models on everything!
Debbie,
Anthony Colpo’s “Great Cholesterol Con” book counters the Lipid Hypothesis. In his later chapters on what might be causes of it, he suggests high iron as a possible cause. Pre-menopausal women have lower iron and less heart disease and then post-menopausal have higher levels like men and same higher heart disease. This is the first time I’ve read him connect iron to anything else besides heart disease. Colpo seems to be on a witch hunt for at least a year now. He was low carb paleo and now he’s high carb paleo. However, his lenses for seeing things are very colored by strenous exercise and athletics for diet. On another thread on rice recently here at PHD, a woman mentioned she was paleo but the “skinny asians” counter argument confused her until PHD reading accounted for it. The more I read the fewer anomalies. So don’t get discouraged, keep it up!
Hi Debbie,
I followed a ketogenic diet for 5 years and experienced a number of fluctuations in thyroid condition. They correlated 100% with my infection status and 0% with carb intake or degree of ketosis (after accounting for their affect on infection status).
I know of no biological reason why these diets should have a direct impact on thyroid function. Their effect is probably indirect, via infections that flourish on ketones (such as fungal or protozoal infections) or flaws in the diet involving malnutrition or toxicity. Heaven knows most clinical ketogenic diets have been malnourishing; most high-fat diets have been high in omega-6.
It takes a long time to sort through the papers, but it seems like a good topic to sift through, since so many people are hypothyroid and this critique of low-carb diets seems to be in fashion. It would be good to find out under what circumstances there’s merit in it.
Best, Paul
PS – Mario, great start toward a blog post! Thanks! If you decide to delve further, you’re welcome to guest post.
PPS – Jay, it would indeed be great if we could be a study diet!
Debbie,
I think that the relation of iron and thyroid is far more complicated from what you heard from some medical practioners and hypothyroidism forums and sites.
There are very few trials on iron supplementation for hypothyroidism. The results are mainly what this study found:
http://www.ncbi.nlm.nih.gov/pubmed/19070025
Some things are improved, some not (notably TSH and fT3).
I don’t know any trial that showed what is an ideal ferritin level in relation to thyroid function.
What we know, and Paul’s experience is a good example, is that thyroid function and Hashimoto’s autoimmune disease is close related to infections.
And iron levels plays a significant role in infections:
http://www.ncbi.nlm.nih.gov/pubmed/18297890
http://www.ncbi.nlm.nih.gov/pubmed/16597321
http://www.ncbi.nlm.nih.gov/pubmed/9356804
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC261386/
So, I think that any Hashimoto’s patient supplementing with iron may want keep a close and frequent look at they thyroid autoantibodies.
Ps. Paul: Yes, I think that we could look into a future guest post on the relationship between infections, diet (carbs, fats and protein), iron and thyroid/hashimoto’s.
Hi Paul,
Re: your post of June 17, one(1) drop of Iosol contains 1830 mcg. Iodine as Ammonium Iodide. Currently I take 1/2 an Iodoral + 1 drop Iosol (among other thing$) daily.
Would you please comment on the following passage from the Linus Pauling Institute: In iodine-sufficient populations (e.g., the U.S.), excess iodine intake is most commonly associated with elevated blood levels of thyroid stimulating hormone (TSH), hypothyroidism, and goiter. Although a slightly elevated TSH level does not necessarily indicate inadequate thyroid hormone production, it is the earliest sign of abnormal thyroid function when iodine intake is excessive. In iodine-sufficient adults, elevated TSH levels have been found at iodine intakes between 1,700 and 1,800 mcg/day. In order to minimize the risk of developing hypothyroidism, the Food and Nutrition Board (FNB) of the Institute of Medicine set a tolerable upper level of intake (UL) for iodine at 1,100 mcg/day for adults. Very high (pharmacologic) doses of iodine may also produce thyroid enlargement (goiter) due to increased TSH stimulation of the thyroid gland. Prolonged intakes of more than 18,000 mcg/day (18 mg/day) have been found to increase the incidence of goiter.
From the Institute’s page on Iodine. See: http://lpi.oregonstate.edu/infocenter/minerals/iodine/
Many thanks. Hope you and Shou-Ching are well, and enjoying the 4th.
Best, KKC
Hi KKC,
Epidemiologically high and low iodine are both associated with higher incidence of hypothyroidism and low iodine is associated with higher incidence of hyperthyroidism.
Several factors we know figure in. One is that high iodine is most often obtained through eating seaweed, especially kelp, that often has high levels of other halogens and toxic metals. Another is that, as Mario’s series shows, as iodine intake increases it becomes more crucial to be replete in other nutrients, especially selenium. Selenium deficiency (or excess) is more dangerous at high iodine intake than at low iodine intake.
A third factor is that irregularity in iodine intake causes the thyroid to have to adapt and each sudden change in iodine intake can induce a temporary hypothyroidism that can develop into pathology for unclear reasons in a fraction of people.
The studies that produced adverse effects from iodine supplementation are usually not all that helpful, because they typically started from iodine or selenium deficient populations, suddenly increased the iodine dose, and only tracked them for short periods of time that may not have given the thyroid enough time to adapt. For instance, http://www.nap.edu/openbook.php?record_id=10026&page=279:
It’s only 28 days long which is typical adaptation time for the thyroid, and the trouble was probably mostly in iodine-deficient (and maybe selenium-deficient) people.
Also, the adverse effects from high iodine are generally mild and reversible, http://www.nap.edu/openbook.php?record_id=10026&page=281:
As (almost) always, one could say that it needs further study. But I think anecdotally a lot of people have had benefits from higher iodine intake, and it seems that we’re gradually discovering the causes of trouble from iodine and figuring out how to increase iodine without significant adverse effects.
Best, Paul
More interesting posts & links to read, thx all.
Paul, with regards to your comment “..irregularity in iodine intake causes the thyroid to have to adapt and each sudden change in iodine intake can induce a temporary hypothyroidism..”
does this relate more to Iodine supplementation, when the body is Iodine &/or Iodide deficient?
If the body is Iodine & Iodide replete, i would have thought stopping Iodine/Iodide supplementation would be okay, as long as the body stores were not depleted. ie. once your body had sufficient iodine & iodide, then you would not need to supp every day, may be just once or twice a week to keep your stores topped up (which would mimic a natural food source more closely).
in relation to my comments above, can anyone tell me the half-life of supplemental Iodine & supplemental Iodide in the body?
I have read that we need both of these forms of iodine; Iodide for the thyroid gland and Iodine for the rest of the body.
thx
Hi Darrin,
Yes, the main problem is a sharp increase in iodine intake from a state of iodine deficiency. If you’re iodine replete it’s much easier to increase iodine. Stopping is generally fine, but restarting can be an issue.
Taking once or twice a week is probably OK.
Half-life is a good question. It ultimately gets excreted but I don’t know how long it takes between ingestion and excretion.
Iodide just signifies a salt of iodine, eg potassium iodide, they’re not distinct forms.
Best, Paul
Hi Paul – just wondering if starting/raising iodoral from a deficient state could raise blood pressure? My mother started 1/2 12.5 mg iodoral for 2 weeks and then raised herself to the whole tablet. She also started progesterone/estrogen at the same time. Over the weekend she experienced episodes of high blood pressure which the beta blocker she is on has been controlling. She has a heart murmur and prolapsed valve. She also has “acute” adrenal fatigue and a nasty rt3 issue. Any thoughts? I’m just trying to help her rule out the possibilities. (I think it’s the estrogen).
thanks
Miriam
Hi Miriam,
That’s a good question. There’s some evidence that subclinical hypothyroidism raises blood pressure: http://www.ncbi.nlm.nih.gov/pubmed/21796125, http://www.ncbi.nlm.nih.gov/pubmed/21777903.
Sudden high doses of iodine can induce a reactive hypothyroidism. High doses of radioactive iodine given for imaging have on occasion induced a sudden surge in blood pressure, http://www.ncbi.nlm.nih.gov/pubmed/21786102.
To avoid such effects, we recommend taking about 6 months to reach 6-12 mg iodine/day. Start at 500 mcg/day, spend a month at each dose and double the dose monthly – 1 mg after 1 month, 2 mg after 2 months, 3 mg after 3 months, 6 mg after 4 months, 12 mg after 5 months, but slow down if anything is awry.
It sounds like your mother may have gone too quickly with the iodine.
The progesterone/estrogen is a confounder, but I would recommend caution with the iodine. I would back off the supplementation, get thyroid hormone levels tested, and start again at a low dose and build up slowly.
Best, Paul
Paul and/or Mario, any thoughts on the safety of iodine supplementation for nursing mothers? My wife is still nursing our 2 yr-old daughter a few times a day.
We’ve been doing the PHD with most of the supplements (including selenium) for the past 6 months. So far, I’m the only one ramping up on iodine. Is it safe for my wife to do the same? Or should we wait until our daughter is no longer nursing?
To clarify, prior to the PHD, we’d been doing Mark Sisson’s Primal Blueprint for over a year, so I feel like our diet has been dialed in for some time. Iodine status is the last big thing on our list to get dialed in.
Hi Eric,
I think iodine is good for babies, so I would start it, but at a low dose, say 500 mcg. Try to get pure iodine rather than kelp.
Iodine deficiency in pregnant women causes mental retardation and I wouldn’t completely rule out that iodine still contributes to development as late as 2 years.
Thanks Paul. Any concerns about detecting side effects in our daughter as the concentration of iodine in the breast milk is ramping up? I’m not so much worried about my wife, as she would know and be able to articulate if she were having any hyperthyroid symptoms. Not so confident a 2 yr old could let us know if she’s having heart palpitations or experiencing nervousness.
Hi Eric,
Here’s a reference for the benefits of iodine in children: http://www.ncbi.nlm.nih.gov/pubmed/21802524. Note iodine has benefits through ages quite a bit beyond 2 years.
Here’s a paper discussing the risks: http://www.ncbi.nlm.nih.gov/pubmed/21276114. I think the risks come from high doses of seaweed, which has contaminants such as metals and bromine, and very uncertain iodine doses. It’s not uncommon for Asians to eat 20 mg or more iodine per day from seaweed, especially if they’re trying.
I think the risks from 1 mg or less pure iodine are minimal, will be present only if starting from a severe iodine deficiency, and will primarily affect the mother. But a quick search doesn’t show a lot of data about iodine in breastfeeding of 2 year olds.
Best, Paul
Well after 3.5 monthes of supplementing with iodine, all of my hypothyroid symptoms were made worse even at a small dosage,
after only one month at 450mcg the hair loss got much more severe especially in the eyebrows,
after 3 months(at 2mg a day) I noticed a big loss in libido and became very tired during the day and having hard time sleeping at night.
I’ve been reading that some people don’t react well to potassium iodide and might do better with Ammonium Iodine, should I try using Iosol formula or stop supplementing with Iodine completely?
Paul,
Beyond what you write in the iodine section of your book, do you have any further insights into why iodine supplementation might exacerbate hypothyroidism?
Whenever I attempt to increase iodine above 400mcg per day, my hypothyroid symptoms seem to get worse. The most obvious signs are dandruff and lowered body temperature.
After this happened a few times, I suspected an autoimmune problem and tested for thyroid antibodies, but the result was negative.
As far as I know, the other possibilities you mention in the book do not apply to me. And I am getting plenty of selenium.
Any ideas? I was very optimistic about high-dose iodine. I have had elevated TSH and clinical hypothyroidism for a long time but have resisted thyroid hormone in the hope that I would find a more fundamental way of addressing the problem.
Thanks for your time.
Hi Danny,
Those aren’t such small doses. 2 mg is a very large dose. It would have been better to stay at 450 mcg for the 3 months.
You can experiment with other types of iodine but I would expect the results to be the same.
I would make sure to look at all the other supplements, esp selenium but zinc, copper, magnesium too.
Do you have thyroid lab measurements? Any other symptoms besides hypothyroidism?
Hi MM,
Various interactions can occur. Iodine can increase glucose utilization and if you are on very low-carb can exacerbate a glucose deficiency. But I would expect the main issues to be thyroid adaptation and possibly bromine toxicity.
Dandruff suggests a fungal infection, which can also cause hypothyroidism. Have you made any changes that would promote a fungal infection?
Best, Paul
Thanks, Paul!
I find what you say about glucose utilization especially interesting, as I have indeed been very low carb for the last month or two. Unfortunately, I have had no choice: I cannot handle even tiny amounts of carb without major blood sugar issues. What is especially alarming as that this has worsened extremely rapidly. Only a few months ago I was eating large servings of sweet potato and other safe starches without noticeable problems.
Hi Paul – this is totally off topic…have you heard anything regarding the carcinogenic properties of coconuts? This was mentioned today in a conversation with a friend and it’s the first I’ve ever heard of anything of the sort….I was under the impression they were more ANTI carcinogenic!
Miriam
Hi MM,
I would look to nutrition or infection regarding the blood glucose utilization. Small bowel / pancreatic infections seem to be good at causing blood sugar issues. Do you have acid reflux?
Hi Miriam,
I haven’t heard anything either about coconuts being carcinogenic. I think your friend is probably confused.
Paul,
Thanks so much for your thoughts. Trial and error is not getting me very far, so I must ask, is there a reliable way to test for the possibilities you raise — especially pancreatic infection and fungal infection generally?
I live in a severely water-damaged apartment, so fungal infection is a real possibility.
Hi MM,
If you have a moldy apartment you have to account for the possibility of fungal toxins, like cell wall components, affecting you. Most molds don’t flourish in the body but they can deliver very high levels of biological toxins with symptoms that look just like an infection.
One thing to try are the detox aids like cholestyramine, bentonite clay, and charcoal. These help clear fungal toxins from the body and might relieve symptoms.
Tests are not terribly reliable. You can try anti-fungal shampoos and see if they help with your dandruff. If you have a white-coated tongue or gingivitis / oral problems, you can see how things you do modulate that. But in general, modulating diet and monitoring symptoms is a good way to track down causes.
Hi Mario
I have found it to be extremely informative although I feel as if I’m suffering from general information overload from scouring the net.
Here’s a brief history on my situation. I’m 41m fit and healthy (never smoked and do not drink much) but discovered a couple of years ago that I had high abnormal sperm morphology (97-99% abnormal forms). We tried IVF a couple of times but it failed so I began to look deeper into possible causes.
In September a friend suggested that it would be a good idea to check out my thyroid function as he read that the thyroid can affect fertility (especially for women). I took a number of tests (blood and saliva) which revealed I had high thyroglobulin antibodies (639 iu/ml) as well my TPO tested positive (261iu/ml) and that it was likely that I had an auto immune issue. My saliva tests revealed that both my testosterone and cortisol were also low possibly as a result of acute stress and that all the other tests were within normal ranges (TSH 2.75, FT4 14, T4 90, FT3 4.4).
This has come as a complete surprise to me as I feel ‘normal’ and do not appear to have any symptoms of autoimmune disorder. From my reading on the subject I assume that most results show that I have Hashimotos but as yet I am not hypothyroid.
Last week I saw an endocrinologist who did little to ease my mind as he confirmed that gradually my thyroid will be destroyed over the next 10-20 years. I asked about taking preventative thyroxine but he felt this would not serve any purpose as I will stop my body producing it naturally if I start taking it in the near future. Instead I should check my thyroid function each year and depending on the results, take appropriate action.
I came out of the meeting feeling OK until I started to read too much on the internet especially on the symptoms. I’m now in a huge panic and questioning everything pain and ache as a symptom (my eyes felt gritty a couple of days ago and are very watery today).
Is there any advice you could give me to help bring me back to reality? I am making my life and my families a misery as I am so concerned about what might or might not be. I am also due back to see the endo on Wednesday and wonder if there are any other questions I should ask. I did mention natural thyroid (armor) but he dismissed it but I am of the firm belief that you can keep your body in check and slow down the process if you know what to do.
In terms of supplements i have been taking selenium off an on for the past 12-18 months as well as vitamin C. We have a very good diet that consists mainly of organic food. My 9 metal fillings are due to removed over the next 3 weeks.
Any advice would be greatly appreciated!
Thank you
Hi David,
Here’s a free-access review paper: http://www.ncbi.nlm.nih.gov/pubmed/20573783. Here’s a paper specifically on male autoimmune infertility: http://www.ncbi.nlm.nih.gov/pubmed/8458465.
It looks like IgA antibodies from the gut may be responsible. I think you should eliminate wheat and any other foods that might cause an allergic reaction or sensitivity.
I would ask for referral to an allergist to investigate what you may be allergic too. It’s probably not the thyroid autoantibodies which are causing the infertility; more likely they’re just another symptom of a generalized problem with autoimmunity.
Although your endo has a case to be made on behalf of not taking T4, I think if the hypothyroidism is contributing to the sperm abnormalities and your goal is to have a baby in the near term, then supplementing thyroxine might improve your fertility for a period of time. Maybe he’s not taking the fertility aspect into account as much as he might; you might ask him about that.
Best, Paul
Hi David,
First and foremost: calm down and relax! We do bad decisions when in panic!
Second: if your endo doesn’t help, you have to find a more knowledgeable and open mind M.D. Natural Thyroid Hormones group in Yahoo mantains a file with “patient approved” doctors in the USA:
http://health.groups.yahoo.com/group/NaturalThyroidHormones/
Some doctors treat subclinical hypothyroidism, others do not. But, the fact is that thyroid autoantibodies seems to decrease significantly with T4 treatment, even on long-term:
http://www.ncbi.nlm.nih.gov/pubmed/18631004
Anyway, I’m on the opinion that you should not treat someone only based on numbers, but you have also to consider their symptoms. Low testosterone, low cortisol and abnormal sperm morphology are all symptoms that could indicate that your body is not functioning well. In the case of abnormal sperm morphology, levothyroxine treatment could improve it significantly:
http://www.ncbi.nlm.nih.gov/pubmed/19012472
My best wishes to you!
Mario
Hi Paul
Thanks for the quick reply. Some more test results came through yesterday that show my motility has now decreased dramatically as well as my morphology.
I’ll be seeing the endo tonight to see what he thinks but he is aware of the fertility issue.
Following your advice I will ask for a referal to an allergist to see if there is anything obvious but what makes you think that IgA antibodies are to blame? Is there a test I should ask for that?
I’m so confused at the moment and want to find a way that I can treat the cause and not the symptoms. Have you come across any studies on bio-identical hormones that could help rebuild my adrenal glands etc or is it all related to diet (and stress).
Thanks
David
Hi David,
I agree with your plan of treating the underlying causes. Unfortunately, this often takes a little time.
The basis for thinking IgA antibodies were to blame was the second paper I linked, http://www.ncbi.nlm.nih.gov/pubmed/8458465. An allergist/immunologist should know what to test for.
I don’t think adrenal hormone supplementation is a recommended approach, but I am not that knowledgeable about this.
I’ve been reading a good deal about iodine and other nutrients for awhile. One thing I have noticed that I don’t often see mentioned are:
1. There are several interdependent minerals which if you are deficient in any of them, are going to result in some bad effects if you supplement iodine. Such as iron, but also magnesium, calcium, potassium, copper for example.
2. Iodine by its nature will start flushing several toxic substances which means detox symptoms, which are not about the iodine but about suddenly having so much bromide and other junk in the system (one of several good reasons to supplement starting small and raise gradually).
3. It appears that increased protein intake might require an increased iodine intake, which might suggest that people already deficient in it, would in the long run see a worsening of the degree of their hypothyroidism, which might be behind the number of people who’ve said a low-carb diet allegedly messed up their thyroid. Chances are they were already iodine deficient and hypothyroid in order to be overweight or pcos and drawn to low-carb in the first place. Greatly upping protein might have aggravated it.
4. Iron being strong in red meat means that some low-carbers might get a lot more iron than they used to as more of their food becomes meat, but if they are deficient in any of the elements noted above, then this would only aggravate things. In particular I’ve seen it noted that a deficiency in the trace element copper would cause “dramatic” results thyroid response (not for the best).
#s 3 and 4 could potentially explain the seeming associate between lowcarb and thyroid.
The complication with the ‘wholistic’ nature of so many vitamins, minerals, trace elements, aminos, enzymes, etc. that one needs to have in ‘balance’, costs lots to test and (a) you can’t test everything anyway and (b) not all tests have very accurate results anyway and (c) you’d need to test repeatedly ongoing, and then your evaluation of what you intake has to take into consideration the negatives which are even in the food you buy in the grocery which has issues, but fluoridated water you have to shower in, and that sort of thing, and then that no matter what you do to get healthy you might have detox results, and . . . even if you don’t have grass-fed meat/dairy which is expensive, you’ve still got enough supplements to choke a horse (and cost about as much as one). Trying to wade through all this stuff has become a minor obsession on my part but it’s amounting to something like an autodidactic college degree on reading research papers and abstracts and articles and blogs… and now and then, I think that funny sizzling noise I hear is my brain frying.
PJ
Thanks, PJ. It’s true, you need to get the diet in general right in order to have the best results; and the more you diverge, the more likely problems are to arise.
Thanks for sharing your research. It looks thorough.
Hi Paul,
What is the best way of evaluating selenium or copper in the body — blood testing or hair analysis?
If I understand this article correctly, I need selenium balanced with iodine intake — but how to know whether I have enough selenium now (i.e. with current diet patterns)?
If it matters, I have Hashimoto’s and am taking thyroid replacement for that.
Thanks!
Kathy
Hi Kathy,
I would just supplement 200 mcg selenium per day. Our recommended supplements page has suggestions.
Copper can be a little trickier. It needs to be in balance with zinc and good ranges are 30-50 mg from all sources of zinc and 2-4 mg from all sources of copper. Depending on what you eat, and whether you use copper cookware or have copper pipes, intake levels can vary significantly.
The best way is probably to get both zinc and copper from food, eg by eating 1/4 to 1/2 lb beef liver per week (providing sufficient copper) and shellfish for zinc. A multivitamin would provide further safety.
High copper levels promote cancer, low copper levels promote cardiovascular disease, so adjust copper intake according to which disease you are most at risk for.
Best, Paul
Hello again guys. Hope you had a good Christmas and New Year.
It’s been a few months since my original posts and I’ve been following a gluten free diet. I have to say that I have not noticed any difference between eating gluten and not other than I have lost some weight through not eating bread. Last week I had a celaic test which came back negative (0.3 and normal range is 0.0-10) which would indicate no gluten intolerance.
I’m going to have another set of tests in the near future but have been taking selenium (pill or brazil nuts), vitamin c, co-q-10 and recently an adrenal supplement.
Has anyone read Dr Alexander Haskell’s book- hope for Hashimotos? I found it very interesting and it seems to make sense except I still need to meet an endo that will perscribe for my subclinical hypothyroidism. He suggests a compounded t3 t/4 combo as opposed to dessicated thyroid for people with Hashis to get your TSH down followed by another 5 steps to keep Hashis at bay including selenium supplementation, gut health, iodine supplementation (only when TSH has been lowered).
On another note my watery eyes I mentioned on my last post were due to bleparitis which is a bacterial infection of the eyelids. Never had it before but think that all the stress from work and personal life has effectively wiped out my immune system which means it’s very difficult to shake. From what I’ve read from other sources you need to address you adrenal glands before treating your thyroid- is this right in your experience?
Do you have any advice for rebuilding the adrenals or at least kicking this annoying eye infection?
Many thanks
Iron from supplements is not well absorbed. Iron naturally occurring in beef (heme iron) is very well-absorbed.
If you have some vit C w/ or immediately after eating beef, that will help you absorb the iron.
HOWEVER, if you have calcium, from supp or food – milk, cheese, etc. – with, immediately before, or soon after the beef, that will inhibit the absorption of the iron.
Hi,
Mario I really enjoy this series. Thank you!
I have been trying to increase my iodine intake and avoid the problems related to the release of accumulated halogens. Related to halogens I been wondering for a long time now if fluoride really is necessary for optimal dental health. After googling for several hours I came across this page, which I really like: http://www.smartahealth.com/
It seems to suggest a really god strategy without fluoride: http://www.smartahealth.com/daily_regimen.html
On a related note Xylitol seems to have some very good properties, both Anti-microbial and enamel mineralizing, ref http://en.wikipedia.org/wiki/Xylitol
I wanted to share this information and at the same time I was hoping to pick the brains of the PHD community. Do any of you have a better resources or advice for oral health?
Paul,
Have you seen this study?
http://www.ncbi.nlm.nih.gov/pubmed/17620655
RCT of 200 mcg selenium yeast found 55% increased rates of type-2 diabetes over 7.7 years in the intervention group. I’d be curious about your take on this.
Will