Mario Renato Iwakura is a Brazilian engineer and Hashimoto’s thyroiditis patient who is intimately familiar with the hypothyroidism literature. Mario has graciously agreed to do a guest series on the place of iodine and selenium supplementation in treatment of hypothyroid disorders. I’m very excited to have Mario’s thoughts, as he’s extremely smart and passionately engaged with the science. — Paul
Most doctors believe that iodine supplementation will aggravate autoimmune (Hashimoto’s) thyroiditis. This view is supported by observations that the incidence of Hashimoto’s hypothyroidism tends to increase in populations that increase their iodine intake. (The incidence of hyperthyroidism, on the other hand, increases as iodine intake decreases.). However not all epidemiological studies support this association [1][2][3][4].
Dr. Datis Kharrazian (“Dr. K”), whose 2010 book “Why Do I Still Have Thyroid Symptoms?”[5] is popular among Hashimoto’s patients, vehemently opposes the use of iodine in Hashimoto’s [5][6][7]. Chris Kresser of The Healthy Skeptic [8] has argued this point of view in his post “Iodine for hypothyroidism: like gasoline on a fire?”. And there’s little doubt that some patients have experienced bad consequences from high-dose iodine.
On the other side, doctors such as Dr. Guy E. Abraham [9], Dr. David Brownstein [10], Jorge D. Flechas [11] and Dr. David Derry [12] have claimed success prescribing high doses of iodine for Hashimoto’s and for breast and thyroid cancers.
Can these experiences by reconciled? What we will try to do is demonstrate that iodine acts synergistically with selenium, and that it is imbalances between the two that damage the thyroid.
First, Some Background
Thyroid peroxidase or thyroperoxidase (TPO) is an enzyme expressed mainly in the thyroid that liberates iodine for addition onto tyrosine residues on thyroglobulin (TG) for the production of the thyroid hormones thyroxine (T4) or triiodothyronine (T3).
The human body normally has low levels of auto-antibodies against both TG and TPO, which serve some physiological function. Autoimmune thyroiditis features high levels of these auto-antibodies, leading to immune attacks on the thyroid.
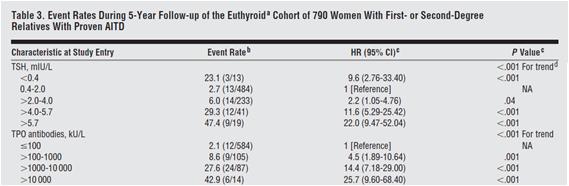
High levels of thyroid auto-antibodies are positively associated with hypothyroidism symptoms [13][14]. TPO antibodies and TSH levels are strongly associated with progression of subclinical hypothyroidism to overt hypothyroidism [3], as can be see in Table 3 below:
Selenium Can Cure An Iodine Excess
Dr. K said in his book and site that “iodine stimulates the production and activity of the thyroid peroxidase (TPO) enzyme” [5][7]. Since TPO is a target of autoimmune attack in Hashimoto’s patients, this might worsen the disease [5][6][7]. In his book he also states that excessive iodine will shut down TPO activity [5], but he neither cites a reference nor states what level of iodine intake will cause this to happen.
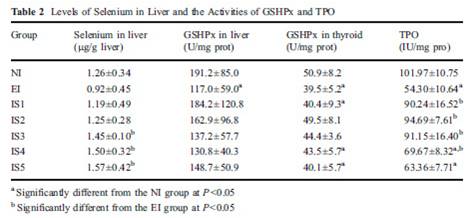
In fact, excess iodine combined with selenium insufficiency will reduce (not increase, not shut down) TPO activity [15]. Let’s look at a study that had seven groups: normal iodine and lab-chow selenium only (NI), excess iodine and lab-chow selenium only (EI), and five groups with excess iodine and steadily increasing levels of selenium added to water (IS1 to IS5). TPO activity was reduced by excess iodine (EI), but returned to control levels (NI) with moderate selenium (IS1 and IS2). With excess iodine and excessive selenium (IS3 to IS5), TPO activity was also decreased, as we can see from table 2 below.
Some other studies have also demonstrated this reduced TPO activity at high iodine intakes [23][24].
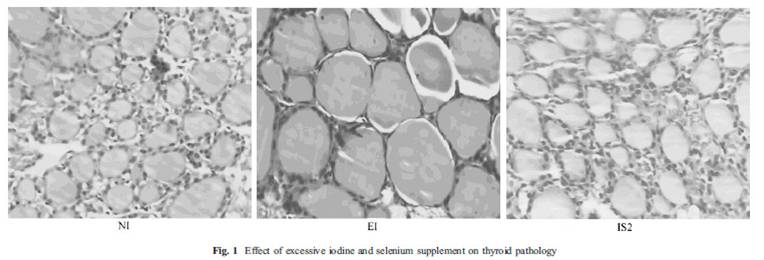
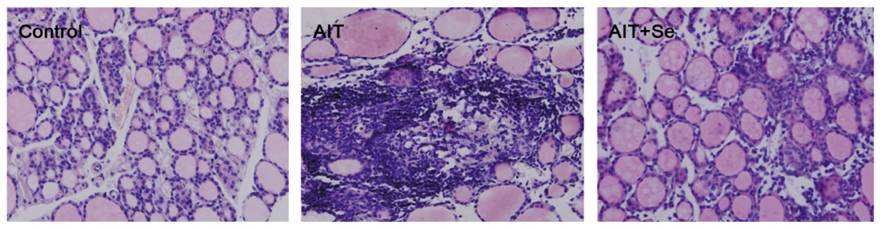
This study [15] also showed a picture (fig. 1) of thyroid follicles from rats receiving normal iodine diet (NI), excessive iodine (EI) and excessive iodine plus 0.2 mg/L selenium (IS2). Thyroid follicles from the excessive iodine group (EI) are enlarged, a characteristic of goiter. But, there is virtually no difference between the first and last picture! If selenium and iodine are increased together, no goiter occurred.
Note that the IS2 level of selenium, which protects against iodine toxicity, corresponds in a person who drinks 1-2 liters per day to a selenium dose of 200 to 400 mcg per day – which happens to be the Perfect Health Diet “plateau range” for selenium.
Selenium Can Cure Autoimmunity
Another paper, also from China, looked at the effects of selenium in an animal model of iodine induced autoimmune thyroiditis [16].
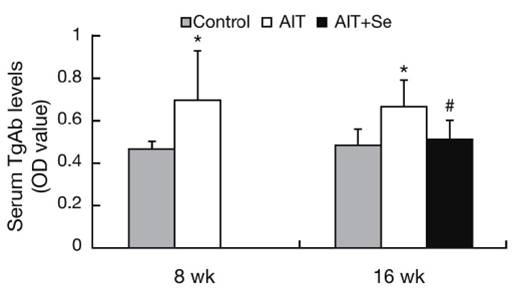
There were three groups of mice, a healthy control group, and groups with iodine induced autoimmune thyroiditis without (AIT) and with (AIT+Se) selenium. The AIT+Se group was given high iodine (AIT only) for 8 weeks to induce the disease, and then, for 8 weeks more, they were given iodine plus selenium. After 8 weeks of selenium supplementation their thyroid follicles were almost fully recovered, as we can see below, even though high-dose iodine had continued:
The AIT group has enlarged cells characteristic of goiter and dead tissue; the AIT-Se group thyroid section resembles a normal thyroid. Thyroid weight doubled in the AIT group, proof of goiter, but returned to normal after selenium supplementation.
Before selenium was given to the AIT+Se group, serum TgAb antibodies were elevated, but they returned to normal after selenium supplementation:
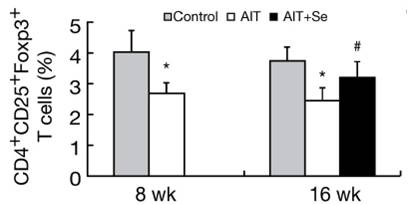
An interesting aspect of this study was the changing population of immune cells. A specialized subpopulation of T cells, negative regulatory T cells or Tregs, helps establish and maintain self-tolerance by suppressing response to self-antigens and suppressing excessive immune responses deleterious to the host. Deficits in Treg cell numbers or function lead to autoimmune diseases [17].
In this study, CD4+CD25+Foxp3+ Treg Cells were reduced by high iodine, but returned much of the way toward normal after 8 weeks of selenium even though high iodine intake continued. The implication is that selenium-iodine balance may be needed to maintain proper Treg cell populations, and that selenium supplementation may restore normal regulation of autoimmunity.
The researchers concluded:
“In the present study, we observed that Se supplementation increased the frequency of CD4+CD25+Foxp3+ T cells and enhanced expression of Foxp3 in vivo. These changes were accompanied by suppressed TgAb titers and reduced thyroiditis. Thus the benefit of Se treatment may be due to the increase of CD4+CD25+ regulatory T cells.”
Under What Circumstances Does Excess Iodine Induce Autoimmunity?
In the previous study high doses of iodine were used to induce autoimmune thyroiditis. Let’s look more closely into the circumstances in which that happens.
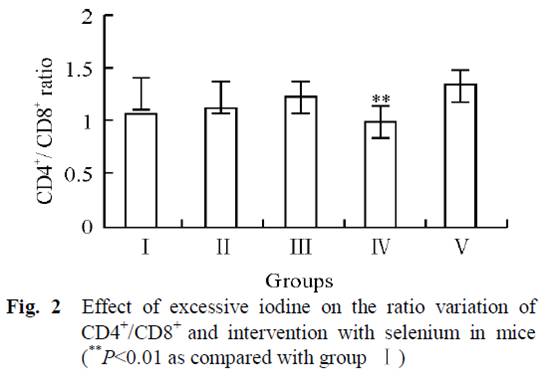
It’s often said that excessive iodine in Hashimoto’s triggers an immune response characterized by proliferation of T lymphocytes, a disrupted Th1/Th2 axis, and altered CD4/CD8 levels. Pathogenesis of autoimmune disease is believed to begin with the activation of T cell autoaggression (turning them into “allergized T cells”).
Our next study, also from China, showed that excess iodine can indeed cause such an autoimmune pathology, but only if there is a deficiency in selenium [18].
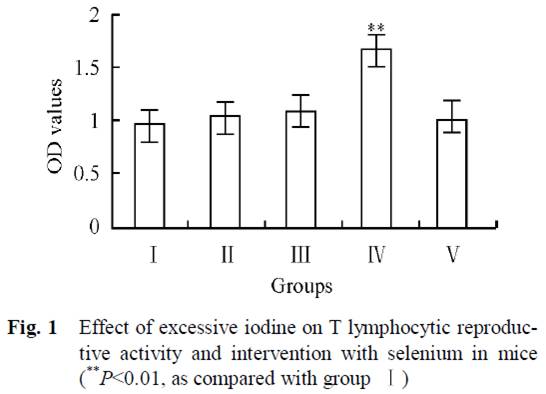
Mice in 5 groups were orally administrated different combinations of iodine and selenium for 30 days. Four groups had no selenium but varying amounts of iodine in their water: 0 μg/L (group I), 1500 μg/L (group II), 3000 μg/L (group III), and 6000 μg/L (group IV). The fifth group had 6000 μg/L iodine plus 0.3 mg/L selenium (group V).
In Group IV, high-dose iodine at 6000 μg/L caused a proliferation of lymphocytes. But this was completely abolished by the addition of selenium to water in Group V:
Normally there are relatively stable population of T cells and their subgroups in tissue till immune function is in disorder. As we can see from Fig. 1, increasing iodine increased T lymphocytic reproductive activity, and was clearly high in group IV. But group V, which also received selenium, had the same values as the control group (I).
Subjects with Hashimoto’s also have a lower ratio of CD4+ to CD8+ lymphocytes than controls [19][20]. From fig. 2, we can see that iodine supplementation in groups II and III actually increased the CD4+ to CD8+ ratio, until the onset of autoimmune symptoms at very high doses in Group IV when the ratio decreased. However, group V, which had the highest iodine intake but with selenium as well, had the highest CD4+ to CD8+ ratio of all groups. This suggests that high-dose iodine and selenium together may actually diminish the autoimmune syndrome compared to the low levels in the controls.
Another marker of autoimmune thyroiditis is the relative strength of the Th1 and Th2 responses, as indicated by the markers interferon-gamma and interleukin-4 (Th2). Th1(IFN-γ)/Th2(IL-4) ratios are increased in Hashimoto patients [21][22], and related with severity of Hashimoto’s disease [22].
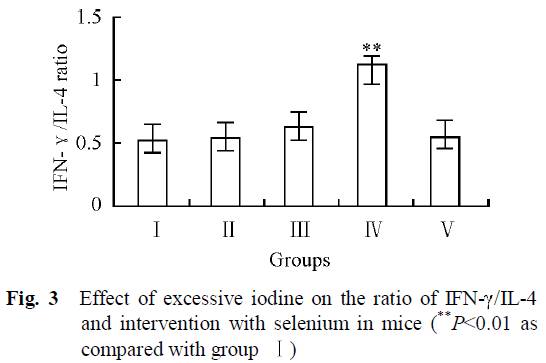 As we can see from Fig. 3, the group with the highest iodine intake but no selenium (IV) was the only group that had clearly higher Th1/Th2 ratio. High iodine plus selenium in group V had similar Th1/Th2 ratios than control group (I).
As we can see from Fig. 3, the group with the highest iodine intake but no selenium (IV) was the only group that had clearly higher Th1/Th2 ratio. High iodine plus selenium in group V had similar Th1/Th2 ratios than control group (I).
The researchers concluded:
“The results revealed that there was no significant difference in the immunotoxicity between interventional group (group V) and control group (group I), indicating that adequate selenium has a favorable interventional effect on excessive iodine intake.”
Conclusion
Excess iodine intake can cause an autoimmune thyroiditis that bears all the characteristics of Hashimoto’s. However, in animal studies this occurs only if selenium is deficient or in excess. Similarly, in animal studies very high iodine intake can exacerbate a pre-existing autoimmune thyroiditis, but only if selenium is deficient or in excess.
With optimal selenium status, thyroid follicles are healthy, goiter is eliminated, and autoimmune markers like Th1/Th2 ratio and CD4+/CD8+ ratio are normalized over a wide range of iodine intake. It seems that optimizing selenium intake provides powerful protection against autoimmune thyroid disease, and provides tolerance of a wide range of iodine intakes.
In the next post in this series (Iodine and Hashimoto’s Thyroiditis, Part 2, May 26, 2011), we’ll transition from animals to humans. Does epidemiological evidence suggest that these animal findings are transferable to humans?
References:
[1] F. Aghini-Lombardi et al. The spectrum of thyroid disorders in an iodine-deficient community: the Pescopagano Survey. J. Clin. Endocrinol. Metab. 84, 561–566 (1999). http://pmid.us/10022416.
[2] Marino MA et al. Urinary iodine in patients with auto-immune thyroid disorders in Santo André, SP, is comparable to normal controls and has been steady for the last 10 years. Arq Bras Endocrinol Metabol. 2009 Feb;53(1):55-63. http://pmid.us/19347186.
[3] Strieder TG et al. Prediction of progression to overt hypothyroidism or hyperthyroidism in female relatives of patients with autoimmune thyroid disease using the Thyroid Events Amsterdam (THEA) score. Arch Intern Med. 2008 Aug 11;168(15):1657-63. http://pmid.us/18695079.
[4] Stuckey BG et al. Low urinary iodine postpartum is associated with hypothyroid postpartum thyroid dysfunction and predicts long-term hypothyroidism. Clin Endocrinol (Oxf). 2011 May;74(5):631-5. doi: 10.1111/j.1365-2265.2011.03978.x. http://pmid.us/21470286.
[5] Dr. Datis Kharrazian. Why Do I Still Have Thyroid Symptoms? When My Lab Tests Are Normal: A Revolutionary Breakthrough In Understanding Hashimoto’s Disease and Hypothyroidism.
[6] Dr. Datis Kharrazian. Iodine and Autoimmune Thyroid — References. http://drknews.com/some-studies-on-iodine-and-autoimmune-thyroid-disease/.
[7] Dr. Datis Kharrazian. Iodine and Hashimoto’s. http://drknews.com/iodine-and-hashimotos/.
[8] Chris Kresser. Iodine for hypothyroidism: like gasoline on a fire?. http://thehealthyskeptic.org/iodine-for-hypothyroidism-like-gasoline-on-a-fire.
[9] Dr. Guy E. Abraham. http://www.optimox.com/.
[10] Dr. Brownstein. Iodine, Why You Need It. https://www.drbrownstein.com/homePage.php.
[11] Dr. Jorge D. Flechas. http://cypress.he.net/~bigmacnc/drflechas/index.htm.
[12] Dr. David Derry. Breast Cancer and Iodine : How to Prevent and How to Survive Breast Cancer.
[13] Ott J et al. Hashimoto’s thyroiditis affects symptom load and quality of life unrelated to hypothyroidism: a prospective case-control study in women undergoing thyroidectomy for benign goiter. Thyroid. 2011 Feb;21(2):161-7. Epub 2010 Dec 27. http://pmid.us/21186954.
[14] Díez JJ, Iglesias P. Relationship between thyrotropin and body mass index in euthyroid subjects. Exp Clin Endocrinol Diabetes. 2011 Mar;119(3):144-50. Epub 2010 Nov 17. http://pmid.us/21086247.
[15] Xu J et al. Supplemental Selenium Alleviates the Toxic Effects of Excessive Iodine on Thyroid. Biol Trace Elem Res. 2010 Jun 2. http://pmid.us/20517655.
[16] Xue H et al. Selenium upregulates CD4(+)CD25(+) regulatory T cells in iodine-induced autoimmune thyroiditis model of NOD.H-2(h4) mice. Endocr J. 2010 Jul 30;57(7):595-601. Epub 2010 Apr 27. http://pmid.us/20453397.
[17] Sakaguchi S et al. Foxp3+CD25+CD4+ natural regulatory T cells in dominant self-tolerance and autoimmune disease. Immunol Rev. 2006 Aug;212:8-27. http://pmid.us/16903903.
[18] Chen X et al. Effect of excessive iodine on immune function of lymphocytes and intervention with selenium. J Huazhong Univ Sci Technolog Med Sci. 2007 Aug;27(4):422-5. http://pmid.us/17828501.
[19] Gopalakrishnan S et al. The role of T-lymphocyte subsets and interleukin-5 blood levels among Indian subjects with autoimmune thyroid disease. Hormones (Athens). 2010 Jan-Mar;9(1):76-81. http://pmid.us/20363725.
[20] Zeppa P et al. Flow cytometry phenotypization of thyroidal lymphoid infiltrate and functional status in Hashimoto’s thyroiditis. Anal Quant Cytol Histol. 2006 Jun;28(3):148-56. http://pmid.us/16786724.
[21] Colin IM et al. Functional lymphocyte subset assessment of the Th1/Th2 profile in patients with autoimmune thyroiditis by flowcytometric analysis of peripheral lymphocytes. J Biol Regul Homeost Agents. 2004 Jan-Mar;18(1):72-6. http://pmid.us/15323363.
[22] Nanba T et al. Increases of the Th1/Th2 cell ratio in severe Hashimoto’s disease and in the proportion of Th17 cells in intractable Graves’ disease. Thyroid. 2009 May;19(5):495-501. http://pmid.us/19415997.
[23] Müller K et al. Effect of iodine on early stage thyroid autonomy. Genomics. 2011 Feb;97(2):94-100. http://pmid.us/21035537.
[24] Man N et al. Long-term effects of high iodine intake: inhibition of thyroid iodine uptake and organification in Wistar rats. Zhonghua Yi Xue Za Zhi. 2006 Dec 26;86(48):3420-4. http://pmid.us/17313856.











Excellent article, Mario.
I have softened my stance on the iodine issue since I wrote that series, after further reading of the literature and after experimenting with iodine supplementation with Hashimoto’s patients.
I agree that selenium deficiency may be one factor that can explain the difference in how Hashimoto’s patients react to iodine. However, I don’t think it’s the only one because I have Hashi’s patients that have been supplementing with the optimal selenium dose for months that still respond negatively to even small amounts of iodine (i.e. as little as 200-400 mcg).
I’m not sure what’s happening in these cases, but it does suggest that selenium may not be the only factor here.
Thanks for this series. I look forward to reading the subsequent articles.
Chris wrote: “I have Hashi’s patients that have been supplementing with the optimal selenium dose for months that still respond negatively to even small amounts of iodine (i.e. as little as 200-400 mcg)”
Chris, I’m curious what you mean by “respond negatively.” What exactly happened to these patients?
Hi Chris,
One thing you might want to look into for those patients is copper status. When my wife had copper-deficiency hypothyroidism she reacted exactly the same to copper and iodine — either would give her hyperthyroid symptoms (esp difficulty sleeping, active brain at night and foggy brain during the day). She would react to tiny doses of iodine.
She had low antibody titers however, so no diagnosis of Hashimoto’s. I’m sure the two conditions can be combined however.
Best, Paul
Great article! Thanks so much, Mario
Thanks for article – very interesting. My Hashimotos is still subclinical at this stage. I am one of those that responded badly to iodine. Within weeks my TSH went from 4 to 13, my thyroid enlarged noticeably, weight increased and I started feeling tired and anxious. I dropped iodine and went back to being symptomless, within weeks.
I’m taking selenium now and a little iodine in my multivite. I’m very nervous about increasing it above this. Confounding the issue is peri-menopause. No symptoms though – It is quite amazing that since being strict gluten free paleo I get no more hot flushes. (I was paleo with cheats – including gluten ones up until about a year ago)
I’ve put on weight recently, but given no other symptoms, I’ve put it down to mindless eating!
I think the other thing some people forget is that zinc levels also need to be good for thyroid function and also copper zinc ratio. http://www.ncbi.nlm.nih.gov/pubmed/20688624
http://www.ncbi.nlm.nih.gov/pubmed/10442272
Well, the patients I have in mind were on a multi with 2 mg copper (the same one that contained selenium as well), so I suppose it’s possible but it doesn’t seem likely.
When I say “negative reaction”, I mean any of the following:
– flare up of hypothyroid symptoms
– temporary hyperthyroid symptoms (palpitations, agitation, etc.)
– swelling or soreness in the neck
– other general signs of intolerance
Paul,
How does one determine a copper deficencey hypothyroidism?
Hi Bill,
Take some copper. For my wife, just 0.5 mg copper would produce hyperthyroid symptoms. The more she supplemented copper, the less her reaction to copper and the better her hypothyroidism.
Hi Chris,
Yes, that would seem to rule out a copper deficiency.
Hi Julianne,
Thanks, yes zinc is important too, and trace minerals as well!
If you’ve been Paleo long enough, and have fixed nutrition, then you might try adding iodine back in slowly.
Whoa, timely. Indeed we were just talking about this at Julianne’s blog. Definitely looking forward to the rest of the series.
Byron Richards (Mastering Leptin) says that he opposes the use of Lugol’s because the potassium iodide/iodine has the tendency to “congest” the thyroid and is not well-used by the body. He recommends Iosol. I just ordered some and am going to try it out. I have been using Lugol’s for the last month and will compare them. I just wonder if the negative reactions to high-dose Lugol’s/iodoral are due to the form of iodine and not necessarily iodine itself.
Cheers.
Paul,
Do you recommend one supplements with copper or eats liver once a week?
As far as supplementation goes, I am thinking of using this one by LEF
http://www.iherb.com/Life-Extension-Only-Trace-Minerals-90-Capsules/10266?at=0
Seems to have everything balanced… just worried about toxicity. I used to drink a chlorophyll drink that had like 200% of my daily copper.. maybe more. Not consistently though, maybe like every other night or so for 2-4 months?
Cheers,
Bill
Thanks, Stabby, that’s interesting. Let me know what you find. We’ll try the Iosol eventually too.
Hi Bill,
Eating beef or lamb liver is better, that’s what I do, but supplementation is fine too.
The only thing that worries me about the LEF supplement is the high manganese levels. They seem to like to err on the high side. There is concern about toxic effects from high manganese, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3018493/?tool=pmcentrez.
200% of daily copper is OK as long as you’re not getting another 100% from a multi, 100% from beef liver, etc.
Paul, Mario, Bill or anyone
The link between increased T cell activity and iodine could explain the predicament I currently find myself in.
Approximately 6 weeks ago I began low dose iodine in addition to the amount in a multi, about 250 mcg, then a little higher around 500 mcg. I had an immediate reaction of right side muscular weakness and/or excitation in the arm and leg. If I stopped the iodine, the symptoms went away, bring the iodine back and they came back until one day about 2 weeks in, they muscle weakness stayed permanently even with zero iodine intake.
My selenium status should be good, some in the multi and 2-3 Brazil nuts for 3 months preceding the iodine.
If I’m a guy on the verge of full blown MS, the energized T cell attacks could be explained by the iodine and account for the symptoms.
Of course, Mario’s selenium protection factor only applies to the thyroid and might have little impact on iodine energized T cells behind the blood brain barrier attacking open nerve sheathes, at least this is how I read this. If anyone acres to sanity check my thinking or has any suggestions, I’d greatly appreciate it.
P.s. Bill, thanks for your input a ways back. I did contact Dr Fletchas, I haven’t heard back but I did find a link between mercury fillings and iodine as a chelater of that heavy metal in pub med 1999. I have at least one metal filling maybe the iodine chelated the mercury leading to MS symptoms or just muscle weakness. Thanks again.
Bill,
I noticed that both the Life Extension ‘Mineral Formula for Men’ & ‘Only Trace Minerals’ lack selenium, which seems like a strange oversight.
Hi All!
To Chris,
My wife had been using antihistaminc that is high in bromide for several years. She do not have thyroid antibodies, only increased TSH, probably due the bromide.
She clearly had bromide detox symptoms when started Lugol’s (a high dose), two years ago. We stopped, and at the beggining of this year she started taking 1 tablet of Now´s Kelp 325mcg. After 2 weeks, she increased to 4 tablets. Soon after, she started having all symptoms you describe. Much, much worsen symptoms that when she was taking Lugol’s.
Stopped kelp, and re-started Lugol’s at a smaller dose, around 1 mg. Increased sea salt consumption. Within a week, all symptoms desappeared! Now she’s taking 6 mg, without any symptoms. What we discover, and will show in part 2, is that kelp and other seaweed is high not only in iodine, but in bromide, arsenic, radioactive iodine, among other contaminants.
And we are in Brazil… Bromide levels are much higher in the US. So, I it’s reasonable to think that bromide detox symptoms should be very frequent in US.
To Stabby,
I have not seen any study that support Byron’s position that Lugol’s “congest” the thyroid and is not well used by the body.
To Perry,
As much as I like brazilnuts, and some studies show that it could be a efficient way to increase your selenium levels (http://pmid.us/18258628), the content of selenium varies from nut to nut and the region where it growns (http://pmid.us/7889353). So, I sometimes eat some brazilnuts, but, for selenium, I prefer supplementing.
To All,
Iodine/selenium interaction is perhaps the most studied and probably the important, but hardly the only one that matters. Vitamins, like A, B’s, C, D and E; minerals, like copper, zinc, iron, vanadium, manganese, chromium, etc, all matters. So, eating a PHD diet, not forgetting to eat some eggs, liver and other nutritionally dense food is a smart thing to do.
But, for me, selenium and iodine is too important, then I supplement.
To Perry,
Forgot. Your symptoms, besides mercury from your amalgam, could be related with bromide from kelp (along with other environmental sources of bromide you may be exposed to):
“Of note, chronic use of bromide-containing drugs may result in serum bromide levels capable of interfering with chloride measurements without causing signs or symptoms of overt bromide toxicity. In one reported case of a myasthenic patient taking a total daily dose of 360 mg of PB (four times the daily PGW dose, and 110.4 mg bromide per day) (Wacks, Oster, et al., 1990), this measurement problem occurred. The patient was admitted with symptoms of myasthenia (but no symptoms of bromism). The abnormal anion gap was noticed in the course of evaluation of the patient for symptoms of reduced muscle strength, facial weakness, and slurred speech, compatible with myasthenia undertreatment or overtreatment. Serum bromide was 8.1 mEq/L (64.8 mg/dL).”
http://www.gulflink.osd.mil/library/randrep/pb_paper/mr1018.2.chap10.html
Chris and Julianne,
Regarding the kinds of problems you are reporting following iodine supplementation, I think it is important not to jump to the conclusion that the iodine is harmful. The iodine doctors have observed such problems, but they almost always seem to be temporary and manageable.
They seem to generally reflect toxicity reactions to bromine and other toxic halides being driven from tissues by the iodine. Or improvements in thyroid function that may require dose adjustments for people on thyroid medication. Or temporary, benign TSH elevation due to upregulation of thyroid metabolism once iodine starvation is rectified. There are a few other possibilities as well.
I personally experienced both bromine toxicity and hyperthyroid symptoms (confirmed by labwork showing near-zero TSH), but the longer-term results have been great, with my need for thyroid medication reduced almost by half. My Hashimoto’s got better; it did not flare. The short-term symptoms were sometimes a bit alarming, but I was prepared for them based on my study of others’ experiences.
The iodine itself does not appear to be toxic, except in very rare cases, e.g., in people with autonomous functioning thyroid nodules. At least this has been the experience so far after thousands of people have been treated with iodine in doses of 12.5 to 50 mg, sometimes much higher in very ill people. This is not to say that iodine could not be problematic for some people, or that longer-term problems will not reveal themselves over the years. I don’t think any of this is risk free. But short-term difficulties do not necessarily mean one should stop experimenting with iodine.
Also, as I’ve said before, I think the safest approach is to follow the entire, holistic iodine protocol developed by Dr. Abraham since this is the protocol the iodine doctors have had such good luck with in practice. Regarding selenium, which is critical, I don’t think relying on either a multivitamin or Brazil nuts is prudent, as the amounts may well be inadequate. Better to supplement with the 200 to 400 ug per day as per the iodine protocol.
Here is a link to a pretty authoritative explanation of the entire iodine protocol as currently understood:
http://f1.grp.yahoofs.com/v1/UP3cTcHexSETYhgdeiUvqescVeLKxbBxlrZ2l9R9WbJwfCRhMM8OgoVoMuYt0MhMJvP4up1TZNGJ_NqtsgSAfRRkG1N3-mofFME/01%20NEW%20MEMBERS%20-%20READ%20FIRST/01%20-%20New%20Member%20Iodine%20Q%20and%20A.doc
Perry,
I don’t know if iodine could stimulate autoimmune disease. I don’t think so, but it certainly doesn’t seem impossible. I have not read of this.
Mario’s concern about bromine toxicity seems very reasonable (although I think it’s rare to see detox symptoms on the low doses of iodine you took). The good thing here is that you can easily test for bromine toxicity if you want to, using Dr. Abraham’s 24-hour iodine loading test with bromine testing added on. My bromine result, as I’ve mentioned, was so high that Dr. Flechas said I was lucky I wasn’t having frank schizophrenic symptoms! My bromine level came way down after three months on 50 mg of Iodoral and I will test again at some point.
The only negative, aside from cost, that I can see is that the loading test requires taking one 50 mg dose of iodine. I could understand if you don’t want to do that right now. One benefit, on the other hand, would be the opportunity for you, or your doctor, to consult directly with Dr. Flechas if you use his lab for the test (I’m disappointed he hasn’t gotten back to you so far). He has enormous experience with iodine supplementation and might have further thoughts for you.
Perhaps asking your doctor for a serum bromine level would be less fraught since you would not have to take any iodine. I don’t think it’s as informative, because it does not reflect bromine stored away in tissues, but I do remember reading that Dr. Abraham has found serum levels correlate pretty well with those from the iodine loading test. It might be a good start, anyway.
As for mercury, I believe you are correct that iodine can chelate it. I had my own amalgam fillings removed several years back, and the doc I worked with for the subsequent mercury detox always warned about the potential dangers of liberating mercury from tissues with chelators too quickly or if the elimination pathways are not functioning properly. So maybe that’s a possibility, too. There is also testing for heavy metals toxicity, which I’ve had as well. If you go that route, I suggest you search out a really good, experienced doctor to work with, someone careful and mindful of the potential dangers as well as benefits. Some of the tests use provoking agents to drive out metals so they can be measured, so I imagine you’d want to be careful there, too.
Good luck, and keep us posted!
Bill,
The multi I use is Nutrient 950 with vitamin K/K2, which has 200 mcg of selenium. I also recommend people eat 3 6oz. servings of fish per week. 16 of the 25 highest sources of selenium are ocean fish, so my patients if they follow these recommendations are almost certainly not selenium deficient.
Thank you, Mario, for this information. I’m trying to heal from what I believe was iodine deficiency induced hypothyroidism (first briefly hyper, then hypo). My doctor didn’t even want to check my iodine levels, but when she did I was deficient. I do take 90 mg Armour thyroid each day, but would like to get off of it eventually.
I started a low multi-vitamin supplement of 150 mcg of iodine, then added a Thyroid Support formula (http://www.swansonvitamins.com/SWC038/ItemDetail, which added another 150 mcg. The selenium is 200 mcg in the multi and 50 mcg in the support formula. I also started slowly upping it with diluted Lugol’s.
It is hard to sort out, because I was also being treated with Diflucan for a yeast infection when the body pain started, I’ve read Diflucan can cause body aches and pains.)The body pain largely went away (knees still hurt) about a week after quitting the Diflucan, but I now have swelling of fingers and odd tingling in my arms, legs and constipation, which I never have. After reading about bromide detox, I’m beginning to think that may be what is going on.
I read about bromide detox symptoms here (http://www.breastcancerchoices.org/bromidedetoxsymptomsandstrategies.html) and find this all very interesting.
By the way, I had full work ups for arthritis (negative), but was treated for lyme disease (no valid positive) and bartonella infections (positive test) with two years of strong antibiotics and Valtrex for reactivated Epstein Barr Virus, so I’ve had issues. Not to mention acquiring gluten intolerance during that time and also lifetime alopecia totalis (thought to be autoimmune), so I’ve had health issues! My chronic sinusitus has, however, cleared up! My psoriasis is almost all gone.
The PHD diet is my last stop. I’ve read about health and sought health/fitness my entire life. After a brief wrong turn down the vegan path, which didn’t work, I decided to do the opposite. That led me to the paleo diet and PHD diet. My husband is doing terrifically. He’s 59 and says he feels 30 again. His hayfever even appears to have cleared up. He no longer takes medicine after only five months on this diet. I’ve had more health issues, so it will, no doubt, take longer.
Can’t say how much I appreciate Paul’s work. It’s a gift. Appreciate everyone, so much. I’ll post occasionally with progress, but don’t want to burden you all. Believe me, I’m taking notes!
Cris,
At least for some Hashimoto patients, eating fish is not advisable. Mercury in some patients increases tpoab and tgab antibodies.
http://www.ncbi.nlm.nih.gov/pubmed/16804512
When I removed my amalgams was exactly what happened. Three months of increasing antibodies and then other three months to decrease to previous levels.
Right after that I started eating around 12 oz of cod every week (because I like cod). Cod has moderate amounts of mercury. My tpoab and tgab started to increase again… And, decreased right after I quit eating cod. So no fish for me…
Mary,
Yes, I’m also very grateful for Paul’s work! Good luck!
Hi Mary,
Your symptoms sound very much like Candida die-off toxicity. I’ve experienced that and characteristics are joint stiffness, muscle stiffness, swollen feet, impaired mood, reduced athleticism and strength, reduced vascular function, peripheral neuropathy, and constipation.
I think the thing to do is continue the anti-fungals, but perhaps at a lower dose until the die-off effects recede, but to use detox supplements. For fat-soluble toxins, cholestyramine (by prescription), charcoal, chlorella, or bentonite clay. Warning – these will aggravate constipation, but it’s worth it. For water-soluble toxins, salt and water.
Best, Paul
Hi Mario, Paul
What form of Selenium are we referring to in the article above? Are we talking about Selenomethionine, Selenite or Methylselenocysteine? Different forms of Selenium have for example different effects on anti-cancer activity, so would they work the same way for these thyroid related autoimmune conditions? Or does it not matter?
Hi Pascal,
In mouse studies I think they usually used selenite in the water.
Selenomethionine may be best in general. But I’m not aware offhand of studies comparing different forms of selenium in thyroid conditions. Good question. Maybe Mario knows of something.
Great post, Mario. I was diagnosed with huge bromide levels using the Hakala test. I excreted 38 mg of bromide over the 24 hours the test covers. Hakala says my blood levels in mg/L are double those of urine in 24 mg/24 hours. So I may have 76 mg/L in bromide.
Should I do anything other than take iodine and sea salt? Currently I am on 100 mg of iodine a day.
Any idea what could be causing high bromide levels?
Pascal,
Although I’m not either aware of any study comparing selenium forms, selenomethionine is the form that most take.
Jeremy,
Three things one must do to reduce bromine levels is to take iodine plus selenium, eat some sea salt (http://pmid.us/15717853 “Biological half-life of bromide in the rat depends primarily on the magnitude of sodium intake”) and avoid sources of bromide that can be avoided.
Bromide main source for most is thru brominated flame retardants. This is found in everything, cars, computers, carpeting, furniture, mattresses, etc.
But it is also in some brominated citrus sodas, like Mountain Dew, some medicine, seaweed, etc.
http://www.cleanproduction.org/library/HCWHBF%20Report.pdf
http://www.cerc.usgs.gov/pubs/center/pdfDocs/PBDE.pdf
http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1246260026626
Does anyone know the amount of iodine in a drop of Lugol’s 2% solution (the only one I can get)? Based on some info I found on the ‘net, I calculated that 10 drops = 12.5 mg but I’m not real confident in those numbers.
Frosty,
Each ml of Lugol’s 5% has 130 mg of iodine/iodide [1]. So, each ml of Lugol’s 2% should have 52 mg of iodine/iodide.
From Wikipedia (http://en.wikipedia.org/wiki/Drop_(unit)), there are several definitions of “drop”, among others:
“the “metric” drop, 1/20 mL (50 µL).
the medical drop, 1/12 mL (83 µL).
the Imperial drop, 1/36 of a fluidram (1/288 of an Imperial fluid ounce, or 1/1440 of a gill) (approximately 99 µL).”
The standard drop is metric, so:
Lugols 5%: 130 mg * .05 = 6.5 mg/drop
Lugols 2%: 52 mg * .05 = 2.6 mg/drop
[1] Herreros de Tejada, Alberto. Guía para el Desarrollo de Servicios Farmacéuticos Hospitalarios: Formulaciones Magistrales. Organización Panamericana de La Salud (OPAS). Page 24. http://www.opas.org.br/medicamentos/site/UploadArq/hse-05-07.pdf
Mario,
Curious to hear your opinion/experience on Iosol.
Chris,
I have no personal experience with Iosol.
At the same time, I have not seen any convincing evidence that potassium iodine can cause any harm to the thyroid.
Regarding forms of selenium, have you guys seen this?:
http://jnci.oxfordjournals.org/content/101/19/1363.long
Also, Chris Masterjohn said he would opt for selenocysteine instead of selenomethionine.
Hi Jaquen,
Very interesting! I hadn’t seen that. Good to know that the forms of selenium used might resolve the different trial results.
Perhaps yeast extract (Vegemite?) has something to recommend it!
I meant to say the one Chris recommended in my comment above – I got confused. But selenoglutathione/selenodiglutathione might actually be best, I saw a paper where one of those had great results. Haven’t seen either available as a supplement however.
Paul,
Life Extension has a selenium mix that looks interesting and has (a little) selenodiglutathion:
Selenium (L-selenomethionine) 50 mcg
Selenium (sodium selenate) 50 mcg
Selenium (selenodiglutathione) 25 mcg
Selenium (Se-Methyl L-Selenocysteine) 75 mcg
http://www.lef.org/Vitamins-Supplements/Item00578/Super-Selenium-Complex.html
Hi Mario,
Looks like a great mix! I’ll have to try it.
I’ve updated our Supplements page to link to this and other higher-quality mixes of selenium.
I’ve found one selenocysteine supplement, but it’s rather expensive & contains vitamin E and something extracted from broccoli (?):
Jarrow Formulas Selenium Synergy 200 mcg
Serving Size: 1 Capsule
Servings per Container: 60
Amount Per Serving % Daily Value
Vitamin E (as d-alpha tocopheryl succinate) 30 IU 100%
Vitamin B2 (as riboflavin) 2 mg 118 %
Selenium (as methylselenocysteine) 200 mcg 225 %
Broccoli seed extract (brassica oleracea) 150 mg
I have a bit of a different question. Lets say some logistical issues kept me from being able to take 200 mcg of Selenomethionine each day, but I could only take it three days a week. Does anyone have an idea if it would work about as well taking Se over three days as 600mcg, 400mcg, and 600mcg? Seems the half life of Se in the body is long enough that might work about the same?
Now the harder part. Lets say I could also only take Lugol’s those three days. How well would that work for detox, slower obviously, but would it still work? I get the impression that I would NOT want to increase the Lugol dose to make up for missed days, but keep it at the seven day dose over those three days?
Doug,
I think it’s just fine, for both questions.
Dr. Abraham describes a case of a woman with a defective transport of iodine that did take 50mg iodine every other day, intercalating with vitamin C:
http://www.optimox.com/pics/Iodine/IOD-11/IOD_11.htm
If you feel fine, I think that there is no harm to increase Lugol to make up for missed days. Some people, mainly those with breast cancer, have been taking up to 200mg everyday for months, even years, without any bad reactions.
The results of a rat study suggest that the inorganic (selenite) form of selenium is ineffective when supplemented together with vitamin C, see:
http://www.ncbi.nlm.nih.gov/pubmed/3088312
Hi Peter,
Thanks much, that’s interesting. Looks like it’s important to take the right organic forms of selenium.
Best, Paul
@Frosty (26 May) if you’re still reading, and happen to be buying the Crow’s version of Lugol’s, their product statement on Swanson’s website is that a “vertical drop” (presumably from the dropper provided with the bottle) of 2% Lugol’s contains 3.125 mg iodine and 6.25 mg potassium iodide.
So is my Country Life selenium okay to take along with the low dose of iodine advised on the diet? I have hypothyroidism.
Also, I’ve been taking all of the supplements for three weeks, been gluten-free for three weeks and just started with the iodine on Monday.
Hi Lisa,
It should be OK, but you might want to switch to one of the versions other than selenomethionine when you next buy selenium. I’ve updated the recommended supplements page so that it no longer has selenomethionine-containing brands.
Best, Paul
Hello Paul.
In addiction to the Selenium Complex, Life Extension have a supplement with 200mcg of selenocysteine. Which do you think would be best?
Hi Eric,
They’re both good. If I had to choose I would go with the complex.
I did order the updated selenium from amazon and it came very rapidly. got it yesterday. I got a really bad sore throat and cold-like symptoms over the weekend. I think maybe it was iodine detoxing. not sure. I get sore throats whenever I get worn down. So I stopped the iodine and will start on the new selenium and build that up for a couple of weeks and restart the low dose iodine just to be safe.
Hi Everyone!
I’m a lot more medical-knowledge challenged than most of you seem to be, but I REALLY need some help/advice and my doctors, well that’s a another country heard from….If I’m barking up the wrong medical tree by writing here, please point me to the correct tree.
I have hypothyroidism and I’m going through menopause. I’ll be 59 years old next week.
I take Synthroid 0.125. The last test was 3 months ago and the doctor said it was ‘fine.’
I’m having strange symptoms:
My hair is starting to thin and come out in handfuls in my brush and the shower.
I’m sweating ALL the time:
1. Hot flashes and night sweats so bad, sometimes I feel like I can’t breathe.
2. Sweating for sweating’s sake — almost constantly.
It’s driving me crazy. It’s making me tired and depressed and I don’t want to go anywhere.
I used to take bio-identical hormones. Helped a little…
I never had a problem with my weight. I was always
around 100-115. I’m 5’3″ Then I blew up. Over the past 4-5 years I went up to over 200 lbs! I was also on pain medication for my back (oxy 20mg twice a day and Lyrica).
About 6 months ago, I got so frustrated, I went off the pain medication. I started to lose a little weight. I’ve been eating right (Special K in the a.m., chicken and salad mostly) and I’m at the gym 6-7 days a week. I’m starting to lose a little more weight, but not fast enough given the heavy workouts I do.
I need help with the sweating…PLEASE!!! and the hair thinning/loss and the weight gain. My doctor says eat less and exercise more. Is that a b*llsh*t answer or what?!?! Sorry, I’m just at the end of my rope and quite frankly I’m scared.
Should I try Selenium? Copper? Iodine?
Thanks so much for listening/reading!
Laura…
Hi Laura,
Welcome!
I’m afraid I don’t agree that Special K for breakfast and chicken and salad later is “eating right.” Special K’s second and third ingredients are wheat gluten and sugar, both bad. Chicken and salad is better but is not well nourishing.
Unfortunately, doctors often think thyroid numbers are “fine” when they’re not. The “normal” ranges are too broad and most people are mildly hypothyroid even though they’re within the “normal” range. Therefore, it’s helpful if you get the test numbers yourself and form your own judgment as to whether things are fine.
Hair falling out is a classic sign of thyroid dysfunction, as is weight gain and impaired temperature control, so there’s a fair chance things are not fine.
I think the best thing to do would be to buy our book and follow our diet and program. There are so many different pieces to health that it is difficult to enumerate them in a comment. But our book covers them comprehensively.
To help you get started, you might look at this post: http://perfecthealthdiet.com/?p=2145.
The good news is that these sorts of problems almost always improve greatly when the diet is better.
Best, Paul