One of the more mysterious conditions afflicting low-carb Paleo dieters has been high serum cholesterol. Two of our most popular posts were about this problem: Low Carb Paleo, and LDL is Soaring – Help! (Mar 2, 2011) enumerated some cases and asked readers to suggest answers; Answer Day: What Causes High LDL on Low-Carb Paleo? (Mar 4, 2011) suggested one possible remedy.
On the first post, one of the causes suggested by readers was hypothyroidism – an astute answer. Raj Ganpath wrote:
Weight loss (and VLC diet) resulting in hypothyroidism resulting in elevated cholesterol due to less pronounced LDL receptors?
Kratos said “Hypothyroidism from low carbs.” Mike Gruber said:
I’m the guy with the 585 TC. It went down (to 378 8 months or so ago, time to check again) when I started supplementing with iodine. My TSH has also been trending up the last few years, even before Paleo. So hypothyroidism is my primary suspect.
Those answers caused me to put the connection between hypothyroidism and LDL levels on my research “to do” list.
Chris Masterjohn’s Work on Thyroid Hormone and LDL Receptors
Chris Masterjohn has done a number of blog posts about the role of LDL receptors in cardiovascular disease. His talk at the Ancestral Health Symposium was on this topic, and a recent blog post, “The Central Role of Thyroid Hormone in Governing LDL Receptor Activity and the Risk of Heart Disease,” provides an overview.
His key observation is that thyroid hormone stimulates expression of the LDL receptor (1). T3 thyroid hormone binds to thyroid hormone receptors on the nuclear membrane, the pair (a “dimer”) is then imported into the nucleus where it acts as a transcription factor causing, among other effects, LDL receptors to be generated on the cell membrane.
So higher T3 = more LDL receptors = more LDL particles pulled into cells and stripped of their fatty cargo. So high T3 tends to reduce serum LDL cholesterol levels, but give cells more energy-providing fats. Low T3, conversely, would tend to raise serum cholesterol but deprive cells of energy.
Other Pieces of the Puzzle
Two other facts we’ve recently blogged about help us interpret this result:
- LDL particles are not only lipid transporters; they also have immune functions. See Blood Lipids and Infectious Disease, Part I, Jun 21, 2011; Blood Lipids and Infectious Disease, Part II, Jul 12, 2011.
- T3 becomes low when glucose or protein are scarce. Thyroid levels alter to encourage resource utilization when resources are abundant and to conserve resources when they are scarce. See Carbohydrates and the Thyroid, Aug 24, 2011.
We can now assemble a hypothesis linking low carb diets to high LDL. If one eats a glucose and/or protein restricted diet, T3 levels will fall to conserve glucose or protein. When T3 levels fall, LDL receptor expression is reduced. This prevents LDL from serving its fat transport function, but keeps the LDL particles in the blood where their immune function operates.
If LDL particles were being taken up from the blood via LDL receptors, they would have to be replaced – a resource-expensive operation – or immunity would suffer. Apparently evolution favors immunity, and gives up the lipid-transport functions of LDL in order to maintain immune functions during periods of food scarcity.
High LDL on Low Carb: Good health, bad diet?
Suppose LDL receptors are so thoroughly suppressed by low T3 that the lipid transport function of LDL is abolished. What happens to LDL particles in the blood?
Immunity becomes their only function. They hang around in the blood until they meet up with (bacterial) toxins. This contact causes the LDL lipoprotein to be oxidized, after which the particle attaches to macrophage scavenger receptors and is cleared by immune cells.
So, if T3 hormone levels are very low and there is an infection, LDL particles will get oxidized and cleared by immune cells, and LDL levels will stay low. But if there is no infection and no toxins to oxidize LDL, and the diet creates no oxidative stress (ie low levels of omega-6 fats and fructose), then LDL particles may stay in the blood for long periods of time.
If LDL particles continue to be generated, which happens in part when eating fatty food, then LDL levels might increase.
So we might take high LDL on Paleo as a possible sign of two things:
- A chronic state of glucose deficiency, leading to very low T3 levels and suppressed clearance of LDL particles by lipid transport pathways.
- Absence of infections or oxidative stress which would clear LDL particles by immune pathways.
The solution? Eat more carbs, and address any remaining cause of hypothyroidism, such as iodine or selenium deficiency. T3 levels should then rise and LDL levels return to normal.
Alternatively, there is evidence that some infections may induce euthyroid sick syndrome, a state of low T3 and high rT3, directly. And these infections may not oxidize LDL, thus they may not lead to loss of LDL particles by immune pathways. So such infections could be another cause of high LDL on Paleo.
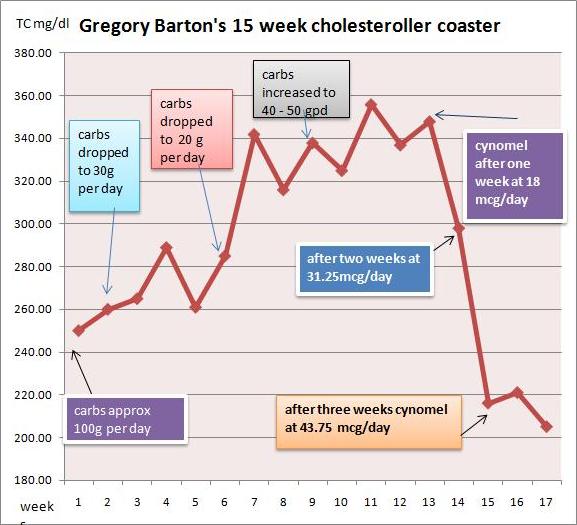
Gregory Barton’s Experience
Gregory Barton is an Australian, 52 years old, living in Thailand, where he keeps goats, makes goat cheese and manages a large garden which can be seen on http://www.asiagoat.com/.
Gregory left a comment with an intriguing story, and I invited him to elaborate in a post. Here’s Gregory’s story. – Paul
Gregory’s Writing Begins Here
One of the claims of low carb dieting is that it will normalize the symptoms of metabolic syndrome. Blood pressure, blood sugar and blood lipids, it is claimed, will all come down on a low carb diet, in addition to weight. For most people this happens. But there is a significant minority of people on Paleo and other low carb diets whose blood lipids defy this claim. (See the list of low-carb celebrities with high LDL in this post.)
Why should this happen? Why should some people’s lipids fall on low carb while other people’s lipids rise? Suboptimal thyroid might be the proximate cause for lipids rising on a low carb or paleo diet. Broda Barnes and Lawrence Galton have this to say about thyroid disorders:
“Of all the problems that can affect physical or mental health, none is more common than thyroid gland disturbance. None is more readily and inexpensively corrected. And none is more often untreated, and even unsuspected.” — Hypothyroidism: The Unsuspected Illness
I went very low carb in April in an effort to address metabolic issues, eating as little as 15grams carbohydrate per day. I had great results with blood pressure, sleeping, blood sugar and weight loss. But lipids bucked the trend.
I had expected triglycerides and cholesterol to drop when I cut the carbs, but they did the opposite: They surged. By July my total cholesterol was 350, LDL 280, and triglycerides bobbed around between 150 and 220.
I did some research and found several competing theories for this kind of surge:
- Saturated fat: The increase in saturated fat created a superabundance of cholesterol which the liver cannot handle. Also, Loren Cordain has claimed that saturated fat downregulates LDL receptors.
- Temporary hyperlipidemia: The surge in lipids is the temporary consequence of the body purging visceral fat. Jenny Ruhl has argued that within a period of months the situation should settle down and lipids should normalize.
- Hibernation: The metabolism has gone into “hibernation” with the result that the thyroid hormone T4 is being converted into rT3, an isomer of the T3 molecule, which prevents the clearance of LDL.
- Malnutrition: In March, Paul wrote that malnutrition in general and copper deficiency in particular “… is, I believe, the single most likely cause of elevated LDL on low-carb Paleo diets.”
- Genetics: Dr. Davis has argued that some combinations of ApoE alleles may make a person “unable to deal with fats and dietary cholesterol.”
I could accept that saturated fat would raise my cholesterol to some degree. However, I doubted that an increase in saturated fat, or purging of visceral fat, would be responsible for a 75% increase in TC from 200 to 350.
There are two basic factors controlling cholesterol levels: creation and clearance. If the surge was not entirely attributable to saturated fat, perhaps the better explanation was that the cholesterol was not being cleared properly. I was drawn to the hibernation theory.
But what causes the body to go into hibernation? According to Chris Masterjohn, a low carb diet could be the cause. Although he does not mention rT3, he warns,
“One thing to look out for is that extended low-carbing can decrease thyroid function, which will cause a bad increase in LDL-C, and be bad in itself. So be careful not to go to extremes, or if you do, to monitor thyroid function carefully.”
If low carb is the cause, then higher carb should be the cure. Indeed, Val Taylor, the owner of the yahoo rT3 group, commented that “it is possible that the rT3 could just be from a low carb diet.” She says, “I keep carbs at no lower than 60g per day for this reason.”
Cortisol and Getting “Stuck” in Hibernation
So what about temporary hyperlipidemia? Bears hibernate for winter, creating rT3, but manage to awaken in spring. Why should humans on low carb diets not be able to awaken from their hibernation? There are many people who complain of high cholesterol years after starting low carb.
A hormonal factor associated with staying in hibernation is high cortisol. It has been claimed that excessively high or low cortisol, sustained over long periods, may cause one to get “stuck” in hibernation mode. One of the moderators from the yahoo rT3 group said:
High or low cortisol can cause rT3 problems, as can chronic illness. It would be nice if correcting these things was all that was necessary. But it seems that the body gets stuck in high rT3 mode.
James LaValle & Stacy Lundin in Cracking the Metabolic Code: 9 Keys to Optimal Health wrote:
When a person experiences prolonged stress, the adrenals manufacture a large amount of the stress hormone cortisol. Cortisol inhibits the conversion of T4 to T3 and favours the conversion of T4 to rT3. If stress is prolonged a condition called reverse T3 dominance occurs and lasts even after the stress passes and cortisol levels fall. (my emphasis)
What I Did
First, I got my thyroid hormone levels tested. A blood test revealed that I had T4 at the top of the range and T3 below range. Ideally I would have tested rT3, but in Thailand the test is not available. I consulted Val Taylor, the owner of the yahoo rT3 group, who said that low T3 can cause lipids to go as high as mine have and, “as you have plenty of T4 there is no other reason for low T3 other than rT3.”
I decided to make these changes:
- Increase net carbs to ~50 grams per day. Having achieved my goals with all other metabolic markers I increased carbs, taking care that one hour postprandial blood sugar did not exceed 130 mg/dl.
- Supplement with T3 thyroid hormone.
- In case the malnutrition explanation was a factor, I began supplementing copper and eating my wife’s delicious liver pate three times per week.
I decided to supplement T3 for the following reasons:
- The surge in TC was acute and very high. It was above the optimal range in O Primitivo’s mortality data.
- I increased carbs by 20-30g/day for about a month. TC stabilized, but did not drop.
- The rT3 theory is elegant and I was eager to test my claim that the bulk of the cholesterol was due to a problem with clearance rather than ‘superabundance’.
What happened?
I started taking cynomel, a T3 supplement, four weeks ago. After one week triglycerides dropped from 150 to 90. After two weeks TC dropped from 350 to 300 and after another week, to 220. Last week numbers were stable.
Based on Paul’s recent series on blood lipids, especially the post Blood Lipids and Infectious Disease, Part I (Jun 21, 2011), I think TC of 220 mg/dl is optimal. As far as serum cholesterol levels are concerned, the problem has been fixed.
I believe that thyroid hormone levels were the dominant factor in my high LDL. Saturated fat intake has remained constant throughout.
My current goal is to address the root causes of the rT3 dominance and wean myself off the T3 supplement. I hope to achieve this in the next few months. My working hypothesis is that the cause of my high rT3 / low T3 was some combination of very low carb dieting, elevated cortisol (perhaps aggravated by stress over my blood lipids!), or malnutrition.
Another possibility is toxins: Dr Davis claims that such chemicals as perchlorate residues from vegetable fertilizers and polyfluorooctanoic acid, the residue of non-stick cookware, may act as inhibitors of the 5′-deiodinase enzyme that converts T4 to T3. Finally, Val Taylor claims that blood sugar over 140 mg/dl causes rT3 dominance. I couldn’t find any studies confirming this claim, and don’t believe it is relevant to my case. Val recommends low carb for diabetics to prevent cholesterol and rT3 issues but warns not to go under 60g carb per day.
Issues with T3 Supplementation
There are some factors to consider before embarking upon T3 supplementation:
- Preparation: In order to tolerate T3 supplement you have to be sure that your iron level and your adrenals are strong enough. This requires quite a bit of testing. I’ve read of people who cut corners with unpleasant results.
- Practicalities: T3 supplementation requires daily temperature monitoring in order to assess your progress. People who are on the move throughout the day would find this difficult.
- Danger: Once you get on the T3 boat you can’t get off abruptly. Your T4 level will drop below range and you will be dependent on T3 until you wean yourself off. If you stopped abruptly you could develop a nasty reaction and even become comatose.
My advice for anyone doing very low carb
As Chris Masterjohn said, in the quote above, if you are going to do very low carb, check your thyroid levels. I would add: Increase the carbs if you find your free T3 falling to the bottom of the range. It might be a good idea to test also for cortisol. A 24-hour saliva test will give you an idea whether your cortisol levels are likely to contribute to an rT3 issue. It might also be a good idea to avoid very low carb if you are suffering from stress – such as lipid anxiety!
Gregory Barton’s Conclusion
I also think my experience may help prove thyroid hormone replacement to be an alternative, and superior, therapy to statins for very high cholesterol. Statins, in the words of Chris Masterjohn,
“… do nothing to ramp up the level of cholesterol-made goodies to promote strength, proper digestion, virility and fertility. It is the vocation of thyroid hormone, by contrast, to do both.”
Paul’s Conclusion
Thanks, Gregory, for a great story and well-researched ideas. The rapid restoration of normal cholesterol levels with T3 supplementation would seem to prove that low T3 caused the high LDL levels.
However, I would be very reluctant to recommend T3 supplementation as a treatment for high LDL on Paleo. If the cause of low T3 is eating too few carbs, then supplementing T3 will greatly increase the rate of glucose utilization and aggravate the glucose deficiency.
The proper solution, I think, is simply to eat more carbs, to provide other thyroid-supporting nutrients like selenium and iodine, and allow the body to adjust its T3 levels naturally. The adjustment might be quite rapid.
In Gregory’s case, his increased carb consumption of ~50 g/day was still near our minimum, and he may have been well below the carb+protein minimum of 150 g/day (since few people naturally eat more than about 75 g protein). So I think he might have given additional carbs a try before proceeding to the T3.
Gregory had a few questions for me:
GB: What if one is glucose intolerant and can’t tolerate more than 60 grams per day without hyperglycemia or weight gain?
PJ: I think almost everyone, even diabetics, can find a way to tolerate 60 g/day dietary carbs without hyperglycemia or weight gain, and should.
GB: What if raising carbs doesn’t normalize blood lipids and one finds oneself ‘stuck in rT3 mode’?
PJ: I’m not yet convinced there is such a thing as “stuck in rT3 mode” apart from being “stuck in a diet that provides too few carbs” or “stuck in a chronic infection.” If one finds one’s self stuck while eating a balanced diet, I would look for infectious causes and address those.
Finally, if I may sound like Seth Roberts for a moment, I believe this story shows the value of a new form of science: personal experimentation, exploration of ideas on blogs, and the sharing of experiences online. It takes medical researchers years – often decades – to track down the causes of simple phenomena, such as high LDL on low carb. We’re on pace to figure out the essentials in a year.











Hi Paul,
Thanks so much for your brilliant book and blog!
My situation is very similar to Gregory Barton’s. Including the concerning additional risk factors that I’m Australian, keep goats, make goats cheese and manage a large garden 🙂
I had been eating strict Paleo (lowish carb) about 4 months or so, then for a period of about 6 weeks I went zero carb in an attempt to resolve intestinal pain and wind by starving gut bacteria. A couple of weeks ago I began the Perfect Health Diet using white rice as my safe starch and keep my vegetables at low enough quantities to minimize intestinal discomfort. I began the essential supplements a few days ago, although I’m still waiting on the vitamin K I ordered. All is going well with the diet and I’m loving it.
I have always been on the underweight side of things and lost even more weight during my ZC experiment.
A week and a half ago I got a call from my doctor about my cholesterol levels. TC: 406 LDL: 313 HDL: 58 TRIG: 77. My only other cholesterol test was around 15 years ago and all I know was that the doctor thought my results were excellent and I believe I still would have had excellent figures six months ago. My TSH was in the normal range. Last week I requested tests for T3, T4, RT3 as well as VIT D. The lab didn’t test for T3 or T4 but instead did another TSH test. I have an appointment tomorrow with my doctor to again request for T3 and T4. The result from the RT3 test was 467 pmol/L. It seems likely to me that this level of RT3 will likely mean I’ll have a low T3 result when I get it.
I’m hoping you can please answer some questions:
My vitamin D levels came in at 18.8 ng/ml. I’m currently supplementing D3 at 1000IU, what level should I supplement at to bring it into range?
I want to try your approach of seeing if my dietary change can resolve the T3 / RT3 and LDL issue as I don’t want to get stuck on supplementing T3 if I can avoid it. However I am concerned that there may be the potential for my LDL to increase significantly further while trying this approach. If the problem is low T3 not clearing LDL and there is no infection then what is there to stop the accumulation of LDL continuing to unheard of levels?
With the Perfect Health Diet being still a relatively high fat diet am I better off significantly lowering my fat intake and increasing carbs until I resolve this problem one way or the other? Obviously I’m not concerned about putting on weight, my total concern is with resolving this problem so I’ll make whatever changes are best diet-wise. What are your thoughts on this?
With what frequency should I be re-tested to see if diet is making the required impact?
I’m taking 2 mg of copper. I also eat lamb’s liver a few times a week (total about 250g liver per week). I’m concerned about relying totally on liver for the copper as the lambs are raised in a very copper deficient soil. Am I at risk of too much copper? If so am I better to drop the liver rather than the supplement given the copper deficient soils?
I’ve started with 1 kelp tablet (iodine 240 mcg). I know you say no more than one doubling per month but should I try to push it further given the likelihood of my thyroid being tied up with the LDL?
Thank you so much for everything.
Adam,
Make sure you test Free T3 and Free T4, not total T3 and T4. I am not familiar with the calculation for determining rT3 dominance (the rT3 test is not available in Thailand). However, the Yahoo rT3 group will help you interpret the numbers. There is also an rT3 ratio calculator on the site:
http://health.groups.yahoo.com/group/RT3_T3/files/
You will also see my latest chart and data, current to 8th October 2011.
Good luck with the diet. As I mentioned above, I was a bit impetuous, only allowing a few weeks of increasing carbs and, according to Paul, not increasing carbs sufficiently. (I am now doing 70 to 80 grams carb per day and the same with protein – approaching Paul’s 150gm target.)
T3 supplementing is a chore and opens a can of worms dealing with your adrenals. You can only handle T3 if your adrenals are in order. On the other hand, getting your adrenals in order might not be a bad thing. Low adrenal function could be a contributing factor to hypothyroidism, rT3 dominance and very high LDL, such as yours. It might be a good idea to check out your cortisol levels.
The question I would ask is, how long will you try diet as a remedy for your high LDL? You mention concern about surging LDL to ‘unheard of levels’. How long is it safe to have such high levels? I don’t think there is an answer to that question, hence my impetuousness.
(Last test: October 8th TC: 151, LDL: 73; I’ll start weaning off T3 this week and we’ll see in a month or two whether the effects of rT3 clearance are enduring. Actually, I’d prefer my TC to rise a bit: 180 – 200 would be desirable.)
Hi Adam,
I would try at least 2500 IU D3, maybe 4,000 IU for a bit and drop to 2500 IU after, but try to get more sun. Summer is coming to Australia so perhaps it will be easier.
I don’t see why LDL would increase further if you are increasing carbs and improving nutrition. I would expect it to come down fairly quickly.
I would re-test in a few months.
If you’re eating 250 g lamb’s liver a week I wouldn’t supplement copper; or reduce it to 1 g/day, or 2 g every other day.
I would stick to doubling iodine only once per month. The thyroid can adapt to different iodine levels so 240 mcg is enough to avoid overt hypothyroidism. The benefits of higher iodine are best won slowly.
Best, Paul
Adam,
I am in Australia as well, out of interest, how long did it take to get your rT3 result back? i’ve been waiting 7 weeks so far, the lab has been waiting on the test kits required to run the rT3 test (they have arrived now, from the US). They now have a backlog of samples to get through.
On the T3, T4 subject; if you are using medicare, the labs will not test for T3 & T4 (or fT3 fT4) if your TSH is within the normal lab range.
As all my TSH tests have been within the normal lab range & i wanted to test my fT3 & fT4 & i was happy to pay for the tests, my Doctor wrote on the request ‘not covered by medicare’. Then the lab should have tested & medicare billed me. But the lab just did the TSH test & stopped there, because TSH was in range.
So my doctor called the lab & ask them to test my sample (which they keep for a while) for fT3 & fT4, & they did.
ps. with regards to Gregory’s comment on Free T3 & Free T4 (fT3 fT4). From my research it seems that in Australia (labs used by medicare) the ‘Free’ tests have replaced the ‘Total’ tests (they no longer do the Total tests). So if a Doctor asks for T3 & T4, the labs will automatically test fT3 & fT4.
Having said that, its still a good idea to specify the Free tests when requesting imo, better safe than sorry.
Paul, thanks for your advice. I’ll retest in a few months to see what impact the dietary change has had.
Gregory, thanks for the tips and link. I’m currently a around 165g carbs. It’ll be interesting to see where we both stand in a few months. It was only by chance I had a cholesterol test, by rights I shouldn’t know this. So once I get my free T3 and free T4 results I’ll try to put it to the back of my mind until I retest.
Darrin,
It took a bit under a week to get my rT3 result back. I’m in Tassie and the local lab had to send my sample to somewhere on the mainland to do the test.
Yes, I knew the whole medicare thing and made it clear to the doctor that I would pay but the same thing happened that you experienced. It’s good to know they keep the sample and I’ll see if my doctor can call them to ask for the test rather than taking yet another sample.
Adam,
I’d be interested know the contact details of the mainland lab that did the rT3 test, for future reference (if the doc gave you the lab results printout & it had that info).
Darrin,
I’ve got the printouts but there are no lab details on them. There is a contact phone no which I just Googled but that is for Hobart Pathology. Maybe they didn’t need to send the test away after all and that would explain why I didn’t have to wait long for the results. But I did find the following lab that can do the test: http://www.pathlabim.com.au/page.jsp?p_id=2&action=display&testID=49
I had my rT3 level tested out of interest & i’ve just got the result back (it took 2 months).
here it is;
rT3: 521 pmol/L (lab range 170-450) (test date 23Aug2011).
So at the time of the test (2 months ago), it looks a fair bit on the high side.
Also (even more out of date/older) I have a FT3 from 2 months prior to the rT3 (22Jun2011): 4.4 pmol/L (lab range 3.5-6.0).
So there’s not much value in calculating the FT3/RT3 ratio. But from what i have read the calculation for these units would be; (4.4*1000)/521=8.445. Which is way below the 20 or better number i have seen mentioned.
That said, its all academic really, until i get the tests done on the same day. & also find a lab that can turn the rT3 test around quickly (location NSW, Australia).
I also had my D3 taken as well.
It is now 65 ng/ml (163 nmol/), down from 80ng/ml (199nmol/L) 2 months earlier.
i previously posted on this here http://perfecthealthdiet.com/?page_id=1066&cpage=8#comment-30085
I was expecting a lower result. Hoping that stopping D3 supps for 10 days after the previous (80ng/ml) test. & then supping at 1000IU per day would bring it down closer to to the 40-50ng/ml range.
Maybe the recent Sun in Australia has slowed the reduction. Tho i really only get limited sun exposure on my arms & lower legs.
Darrin, did you have your LDL high at the time of the rT3 test? I’m looking for evidences of a conection rT3-LDL
Hi Paul,
At last I got my test results back and I had a conversation with the doctor who ordered them through the hospital (not private)
They’re interesting.
A bit of context. In 2003 I was about 66 kg, a bit overweight. In August 2008, after 2 pregnancies and more or less continuous bingeing I weighed 95 kg and I decided to go low carb (cut the carbs to around 50 grams, no starchy ones) to lose weight. After a year of low carbing I got to about 66 kg and the weight loss slowed down. I still managed to get to 59 after another one year, in July 2010. But after that I plateaued and couldn’t lose any, after Christmas I even put some back. My LDL cholesterol in the mean time started to bother my GP who sent me to the hospital, to the Metabolic Clinic. The first time I had my T3 tested was in August 09 and seeing it was low I thought there was a relationship to the high LDL, but nobody else cared about it. This year in February 2011 I started to take T3, 10 mcg twice a day. And then I had some tests done in September. Now to the numbers.
01.03 TC 5.97 HDL 2.27 LDL 2.82 Trig 0.72
06.07 TC 6.5
09.08 TC 7.1 HDL 2.1 LDL 4.7 Trig 0.6
08.09 TC 11 HDL 2.1 LDL 8.6 TSH 2.1 T3 0.9(L) FT4 15.3
10.09 TC 13.7 HDL 2.5 LDL 10.9 Trig 0.7
11.09 TC 15.4 HDL 2.32 LDL 12.7 Trig 0.9 TSH 1.6 FT4 16 T3 0.6(L)
02.10 TC 13.7 HDL 2.89 LDL 10.32 TSH 1.59 T3 0.8(L)
08.10 TC 12.5 HDL 3.1 LDL 9.2 Trig 0.46 TSH 1.93 FT4 15 T3 1.2(still low)
09.11 TC 7.35 HDL 2.85 LDL 4.31 Trig 0.42 TSH 0.02 FT4 8.2(L) T3 2.7(high)
So yes, my LDL has gone down dramatically, not to baseline though and my TSH is suppressed by the supplemental T3. (I see what Chris Kesser and you have said about it being an adaptive response that one shouldn’t mess with) I have to come off it and see what happens. Was it the weight loss and the starvation response, or the glucose deficiency and added to them the extra saturated fat I’m not sure. Why is not gone down lower? What else is there? My HDL is not gone down that much though although I cut some of the fat for 2 months before the last tests.
What do you think?
Hi simona,
Well, first your LDL at 4.3 is at the top of the normal range, so are HDL and TC, so I wouldn’t worry about lipids for the moment. There might be some minor issues to fix, but the main issue is how to get the thyroid back to normal.
Are you on our diet and supplements? Any nutritional defects should be fixed, including eating enough carbs and getting appropriate thyroid related nutrients.
It looks like your T3 dose is high, based on the low T4 and TSH and high T3 level. You should definitely be eating carbs if you’re taking T3.
Thanks Paul,
I think it was wrong that the doctor that prescribed T3 didn’t check the level in February. We don’t know what was the ‘number’ to treat. The tablets are small and of 20 mcg and I have to cut it in 2. At the moment I only take one half in the evening and I’m going to cut it in half again to take only 5 mcg for a while and then stop in December. The doctor said my thyroid has to start working again on its own. I have been eating more carbs and trying to keep to the PHD. Supplements are not regular or consistent, depends on availability, fex now there isn’t enough money for NAC. Mg and vit C is a must. I bought vit D, K2, and ubiquinol a while ago online and I have an average multi that has iodine, Zn, Cu, Se in it for another 3 months. I’ll retest next year.
My doctor was happy, but he doesn’t want to accept that it was the extra T3 that caused the huge drop. He hasn’t seen in his practice low T3 influencing LDL that much. I told him I must be in the 5%!
Great information!
I try to keep carbs <50g/day (to keep smLDL low due to atherosclerosis), protein is about 80-100g/day, and moderate fat plus MCT oil to give me a total of about 1800- 2000 calories.
I have low T3 with high rT3. I took increasing amounts of Armour for over a year. Recently, the Armour zapped my energy, increased my metabolism such that it seemed that it was consuming all my energy – I was on the edge of hyper. I am off Armour now. The doctor thinks that my thyroid may reset.
I would like to do all I can to support thyroid normalization. I take selenium, copper, zinc, iodine to support the thyroid. BTW, I am taking a statin (crestor).
I suspect that my protein intake is insufficient (I have been told that my intake of protein should be 150g/day). All this as background to my questions:
1. What is the recommended level of protein to support t4-t3 conversion?
2. Could an increase in protein while keep carbs 25-50g offset the need for more carbs (so the body does not go into hypothyroid 'hybernation' mode?
Thanks!
Thanks for the update, Darrin. I think I’d stick with the 1000 IU and maybe try getting a bit more vitamin A if you don’t eat much of that.
Hi Janusz,
You’re a bit below our recommended absolute minimum of 600 calories (150 g) carb+protein. This leads to glucose conservation and low T3/high rT3.
Taking T3 will lead cells to consume extra glucose, creating a crisis for the body because the food in is well below the amount being consumed. This is like late starvation. You get low in energy because you’re starving.
I think you should eat more carbs, first of all. You don’t need to be zero-carb to get sLDL down.
Recommended protein: I would aim for >400 calories carbs and >700 calories carbs+protein, so if you go 400 calories carbs, at least 300 calories protein.
Protein can only partially offset very low carb intake. If you want to bring T3 up naturally, you need to eat more carbs.
Thanks Paul,
I am less concerned now that its below 70ng/ml.
I am intentionally shedding some fat at the moment, so I think i will take 1000 IU every other day while i do that.
As i expect i will be getting some Vit D from my fat stores as well.
Hi jesús,
sorry, no i did not have LDL checked at the time.
my last LDL result was 4 mths prior to the rT3, when it was 3.3 mmol/L (127.61 mg/dl).
Thanks, Paul!
Okay on more carbs. You stated “Protein can only partially offset very low carb intake.” What about MCT oil? MCT oil goes directly to the liver, provides energy to cells, and increases metabolism — preserves glucose, reduces fatigue — and doesn’t go to fat. Seems like that would work also.
Hi Janusz,
Yes, MCT oil can partially offset glucose too.
However, it’s still good to get some dietary glucose.
Hi Paul,
I had another test for lipids yesterday and my results didn’t change much from a month ago.
I asked my doctor to retest my results to see how much variability there is between the testing.
September 20th test was:
TC: 279
LDL: 214
HDL 55
TG: 50
October 26th test results:
TC: 272
LDL: 206
HDL: 53
TG: 67
TSH: 1.5
During the course of the month, I started taking your recommended supplements and I also increased my safe carb consumption. I made a conscious effort to eat more tubers and rice. I think the rise in triglycerides is an indication of increased carb consumption. I also cut out the morning half and half in my coffee and laid off the coconut milk. I was curious if the saturated fat reduction would lower the numbers. It doesn’t seem like saturated fat is the issue.
My doctor wants me to come back in three months to retest. He insists that I go on statins but I don’t want to go that route. I told him I was going to modify my diet to lower the numbers. My numbers aren’t terrible but I am not sure what to make of it. I feel like I am playing a game on how to lower LDL without really knowing what the cause is or whether it is really worth my time worrying about it. My weight, and blood pressure are normal. I don’t smoke or drink. I eat a very balanced diet of tubers, fruits, veggies, berries, nuts, fish, etc.
I was thinking perhaps my LDL receptors may not be clearing the LDL fast enough or the amount of oxidation stress is minimal where LDL isn’t being removed by the immune system. My exercise activity is strictly walking. I wonder if increasing the intensity of exercise would stimulate the production of LDL receptors that would clear the LDL out at a faster rate thus lowering concentrations in the blood.
I had my thyroid checked and the TSH is in the normal range. Unfortunately, the test did no measure T3.
So, I am thinking of adding in more exercise, maintain the PHD diet with extra carbs and take the recommended supplements in the next three months.
Does this seem like a reasonable approach?
Many thanks for your time and help,
Erik
Hi Erik,
It does sound like a reasonable plan. I certainly wouldn’t take statins, and I would look first to nutrition for the remaining LDL reduction. Our recommended minerals (selenium, magnesium, zinc, copper, iodine, plus calcium) and vitamins A/D/K2 and C are probably most important.
Thank you, Paul.
I was curious if you know what beeturia is? I recently ate some fresh beets and my urine turned pink after consuming them. I did some searching on the web and found that 10% of the population will excrete these beetalin compounds that turn the urine pink. Apparently, it is harmless. What really poked my curiosity is that people within this population have a higher rate of iron absorption problems that lead to anemia or hemachromotosis.
I began to wonder if maybe my high LDL might be tied to iron metabolism. If I am getting too much, then this could lead to oxidation damage therefore the LDL is cleaning up the damage. It is a wild speculation. I looked at my blood tests from 2010 and my hemoglobin (13.9 GM/DL) and hematocrit (40.5%) were slightly below the normal reference range. Those numbers are pre-PHD diet and on USDA recommended diet.
I am thinking of asking my doctor to test for ferritin and other iron markers.
Do you think iron could be a factor in high LDL levels?
Thank you,
Erik
Hi Erik,
I have heard of beeturia but not experienced it.
I think it’s very possible that some iron issue may be involved with the high LDL problem. Iron is involved in glucose metabolism, thyroid function, and other aspects that seem to be involved with LDL issues.
I would have to explore more to think about mechanisms, but I do think it’s worth your while to ask your doctor to assess iron status as well as T3/rT3 status.
Hi Paul,
I don’t have LDL issues, but just noticed your comment on iron, so I am curious how one might know of an ‘ironclad’ way to know if they had an iron issue? As background, I contacted ‘The Road Back’ for a doctor referral after reading your post about arthritis. I visited a doc on the list to see about trying the antibiotic therapy. It turns out he has long since moved on from providing the protocol, and fancies himself a bit of a ‘House’ type. If you are interested, he is a bit of a pioneer in the low-carb, toxic substances kill world. In his 80’s now and quite eccentric.
Meanwhile, I did give him background on my health and he speculated that I have an iron problem that may be at the root of the cause. I got the impression he had a hammer and I was the nail, but I agreed to some tests – which included finding out the mineral status, including copper, in my blood. I haven’t seen the results yet, but I was curious if you have done much research on iron?
Sorry if the above seems to much like free association!
Nick
Hi Nick,
I haven’t done much research on iron. I’ve read papers about it’s relation to health issues, but I haven’t acquired the sort of knowledge necessary to give clinical advice about how to diagnose and treat iron-related issues.
Hi Paul,
I have high cholesterol and my TSH seems to have increased a lot in the month I’ve been taking 1mg of iodine and 200mcg selenium (with some more selenium from my multivitamin). I’m now doing zero carb to heal/alleviate proctitis, fatigue and gut issues. My TC climbed to 400 when going low carb high fat, but I’ve been feeling better at the same time. Unfortunately starch seems to cause proctitis symptoms and I seem to have developed fructose malabsorption since this all started last winter, so it’s not a viable option to increase carbs. Triglycerides seem to be slowly creeping up but are still in a healthy range. I did experience warm hands on occasion a few weeks into supplementing iodine.
My best guess is that everything will simply take time to adjust and normalize. However with the latest TSH I’m not sure about the iodine dosage, I assume I should back down? Please see this image for a more detailed timetable with various bloodwork results: http://i.imgur.com/wj2oq.jpg
I’m also suspecting slight Vitamin D3 toxicity due to K2 deficiency, which in turn may stem from my gut issues… I have stopped getting calculus which had started this year and less symptoms like bone pain since stopping D3 and upping K2 supplementation recently. Not sure how that could be involved in cholesterol and thyroid issues.
What’s your impression?
Hi Dean,
It’s a rather complex set of symptoms and I can’t attempt much doctoring. I think it would help you a lot to get some carbs, so I would try rice syrup or dextrose and see if you tolerate that.
Then you have to address the gut dysbiosis that makes starches and sugars intolerable.
The interplay of iodine with the thyroid in infectious conditions is very tricky. There’s not much evidence to guide us. However, since 100-200 mcg iodine on a higher carb diet reduced TSH to the normal range, and since I have faith in iodine, my guess is it’s really the combination with zero carb that is the problem and is raising TSH.
I would probably stick with 1 mg (don’t raise it further), finding a tolerable glucose source, and give my thyroid more time to adapt. However, you could make a case for reducing the iodine back toward the 200 mcg that worked for you before. I wouldn’t increase it until your TSH normalizes. In the meantime, the key is to fix the underlying cause of the hypothyroidism.
Best, Paul
Thanks Paul!
I don’t actually have hypothyroid symptoms, by warm hands I meant “too warm” as in hyperthyroidism. Doesn’t sound right with high TSH, that’s why I thought it might be adjusting. Most of the time my temperature is fine, weight has always been fine, energy is much better than earlier this year etc.
It’s puzzling how eating sugar might offer health benefits just because it’s a carbohydrate. It goes against a lot I read about immunity, blood sugar etc. I did a trial with dextrose while I was still taking probiotics, which ended in more fatigue. This is one of the reasons I suspect SIBO. I stopped the probiotics and later did a glucose H2 breath test which was negative, so I should be able to tolerate it. I’ll read some more and maybe try dextrose again. Mine is not a natural position to be in and might justify unnatural means like dextrose. Thanks again.
Hi Paul,
Interestingly it turns out I’ve also got a H. pylori infection which has been causing havoc in my system. I’ve started a combination of antibiotics to hopefully get rid of it.
It just occurred to me that maybe there is some link with my elevated LDL. Could that be why some people of low carb get elevated LDL and others don’t?
A quick google came up with this study:
http://jkms.org/DOIx.php?id=10.3346/jkms.2011.26.5.654
What do you think?
Thanks,
Adam.
Hi Adam,
H. pylori is cholesterol dependent (http://www.ncbi.nlm.nih.gov/pubmed/22092715) so it might be in its interest to upregulate host LDL. The Korean study is suggestive that it may be able to do that. Here’s a Japanese study: http://www.ncbi.nlm.nih.gov/pubmed/20610892.
The smoking gun: Eradicating H pylori significantly reduced LDL: http://www.ncbi.nlm.nih.gov/pubmed/20134372.
I think you’re on to something.
Best, Paul
Hi Adam and Paul,
H pylori is tought to be implicated with autoimmune thyroiditis:
http://www.ncbi.nlm.nih.gov/pubmed/18271683
http://www.ncbi.nlm.nih.gov/pubmed/15244214
http://www.ncbi.nlm.nih.gov/pubmed/19522019
Altough not all studies showed a correlation:
http://www.ncbi.nlm.nih.gov/pubmed/15745105
Erradication of H pylori apparently could led to a decrease in thyroid autoantibodies:
http://www.ncbi.nlm.nih.gov/pubmed/15521972
Hypothyroidism patiens who failed to achieve normal TSH levels with T4 supplementation greatly improved after H pylori erradication:
http://www.ncbi.nlm.nih.gov/pubmed/21435090
But, since we have been living with H pylori for ages, would be a good idea try to erradicate H pylori with antibiotics?
For me the problems with H pylori result from an altered gut microbiota and gut permeability, and resolving the gut health, without erradicating H pylori, would be a better solution.
Thanks Mario for your thoughts and great links. In the case of otherwise healthy individuals you’re probably right.
However my symptoms relating to H pylori go way beyond elevated LDL. I’ve had some recent internal bleeding. I have been developing multiple food intolerances. I’ve never had healthy digestion and have had a chronic sore throat for over 20 years and have only now worked out it is reflux which has been suggested could be H pylori related. I’ll be having a gastroscopy to find out exactly what damage has been done.
If I simply had elevated LDL and tested positive for H pylori and otherwise felt great then I would consider alternatives to eradication. But given it’s impacts on me so far and the links to stomach cancer and so many other diseases I’ll do whatever it takes to rid myself of it as fast as possible. Resolving my gut health will then continue to be my priority.
I wanted to let you know that I’m still doing better without carbs than when trying to add any, inclding dextrose. Not convinced about safe carbs at all when it comes to dysbiosis.
Congratulations Paul, you were right again.
A few weeks of trying to go as low carb as possible produced this lipid profile (i was seeing if it could get more desirable from an HCV perspective)
total C 8.9
tg 1.3
HDL 1.65
LDL 6.7
now the LDL is the only fly in the ointment here (BTW, doesn’t quite add up, I took it over the phone, but probably close enough). Meanwhile I had these symptoms – ache behind the eyes as if eye sockets were emptying, loss of energy compared to earlier on low carb, or slightly more carbs.
Came across this post and I think it describes it perfectly. Eyes bulge in hyperthyroidism, no doubt the opposite applies.
Upped carbs to 100-150g and eyes became normal and energy good. Will tell you how the next lipid panel goes in 3 months.
U da man.
Great to hear you’ve added the carbs, George! Keep me posted.
Dear Gregory,
Would it be possible for you to post another update? Your story is fascinating, not least because I seem to be dealing with a Reverse T3 problem myself. My labs have repeatedly revealed low Free T3 and adequate Free T4; when I requested Reverse T3 on my most recent workup, my value was at the 99th percentile. Yikes!
I was VLC for about 18 months before adding carbs a la the PHD, and I now consume 150-250 grams of safe starches per day. (I’m a fairly active 6’3 24yo male.) I’ve been at this level for about 9 months, so I don’t think I’ll gain anything further with dietary changes.
I’ve run my numbers by Val, and she suggested that I’m a great candidate for T3-only therapy. (My iron levels and adrenal status are actually pretty good.) Did you manage to wean yourself off of the T3, and did the effects last? Any insights or notable experiences over the past few months would be greatly appreciated.
Hi Phoenix,
Gregory sent me material for an update, as did Larry, I just have to put it together in a blog post.
It’s all consistent, Gregory did indeed need to up carbs, and Larry benefited most from micronutrient supplements including selenium and iodine, so there is still a thyroid connection.
Are you supplementing selenium and iodine?
Thanks for the prompty reply, Paul. (And greetings from Berkeley!. I’m a PhD student out here.) I look forward to Gregory and Larry updates.
I was supplementing iodine (having slowly worked up to 3mg non-kelp per day) and selenium (always 200mcg per day) until fairly recently, when Val and the thyroid groups suggested that my exceptional RT3 value was evidence that there was clearly enough selenium in my system to de-iodonize T4. Cron-o-meter tells me that I consume about 150mcg of selenium daily from natural sources. I take most of the other PHD supplements and adhere strictly to the diet. I also take 30mg zinc, Vitamin B12, and milk thistle (for reasons outlined below). No I/Se at the moment.
Interestingly, my TSH has dropped from 3 to about 1.5 over the past six months, and the removal of iodine and selenium is probably the most significant thyroid-related change I’ve made to my routine during this time. This drop started before I upped my carbs from ~150g to 200-250g, which was in response to your 2/2/2012 post. That said, I’ve had some of the healthiest-feeling days in a long time between then and now, and those followed higher-carb days. Perhaps higher-carb + I/Se would be even better? Or perhaps the iodine would just make my thyroid do more of what it does best, which seems to be “converting T4 into RT3”?
Sadly, my thyroid issues are only one of two major hormone problems I’m dealing with at the moment. I also have exceptionally low testosterone. Here are my most relevant recent numbers (24yo American active male):
Triglycerides: 62
HDL: 71
LDL: 167
Free T4: 1.4 (0.8 – 1.8)
Free T3: 2.5 (2.3 – 4.2)
RT3: 37 (11 – 32)
FT3 / RT3 ratio: 6.7 (20+)
TSH: 1.46
Thyroid antibodies: None
Testosterone, Total: 164 (250 – 1100)
Testosterone, Free: 43.6 (46, 224)
FSH was low-normal, LH was low last time we checked; checking again tomorrow
Vitamin D: 48
For some context, my problems all started 8.5 years ago when I was anorexic and overexercising for 6-9 months, with a low-dose Accutane cycle for mild acne on top. After ~6 years of absolute misery (including 4 as a vegetarian), I went VLC paleo in December 2009 a la Mark Sisson and saw some definitely improvements, though still tons of room for improvement. I switched to PHD in June 2011 and felt even better with safe starches, though still with two hormonal imbalances that haven’t resolved. These imbalances were only diagnosed six months ago, having been missed for 8 years, but we haven’t made much progress treating them.
On clomiphene citrate, I had very reasonable testosterone/LH/FSH levels at one point and felt a bit better, but hardly great. When we tried two different natural dessicated thyroid hormones (Armour and Naturethroid, not simultaneously, one in the presence of clomiphene and one on its own), I experienced fatigue, dizziness, and feeling “off”. My theory is that my body just converted all the T4 into RT3, which prompted me to request RT3 on my most recent labs. It’s interesting that RT3 conversion gets up-regulated under conditions of biological stress such as undereating and overexercising, exactly what started this whole ordeal.
I realize this is a lot of information, but there’s a lot happening to me, medically. Any thoughts or suggestions would be deeply appreciated.
Hi Phoenix,
How’s your diet? Eat lots of seafood? You’re young, probably don’t have amalgams, no?
Mercury exposition is associated with higher T4, fT4/fT3 ratio and reverse T3. And lower total testosterone (but not free T).
All this is aggravated if you have low iodine…
http://pmid.us/11180271
http://pmid.us/7951778
Thanks for weighing in, Mario. I’ve greatly enjoyed your posts on iodine and hypothyroidism.
No, I don’t have any amalgams, having enjoyed great dental health over the course of my life. Aside from about a year during which I was eating canned tuna a few times per week, mercury exposure in my lifetime has been limited; no industrial work, proximity to toxic waste dumps, or hours spent playing with broken mercury thermometers/lightbulbs.
These days, I eat about 1/2 pound of fresh seafood, usually salmon, per week. I also take a small sip of cod liver oil on non-seafood days. I was eating seaweed daily for a few months (small amounts of kombu) when I started the PHD, but I don’t do that any more to avoid bromides and heavy metals.
Other than that, my diet is fairly simple and quite PHD compliant, I think:
– Breakfast: homemade bone broth, organic veggies (kale, bok choy, red cabbage, carrot) sauteed in coconut oil, 1/3 lb grass fed ground beef, beef liver (about 1 lb per week), rice, and spices. Drink homemade kombucha. Delicious!
– Lunch needs to be fast, so I have a protein shake of shredded coconut, grass fed butter, whey protein, cinammon, and rice, mixed with water.
– Dinner: rotates between (seafood, beef, eggs) with sweet potatoes.
It may be worth looking at whether this low-carb rT3/ high LDL syndrome is mainly associated with mercury exposure. Certainly in my case I had dozens of amalgam fillings most of which ended up in my stomach as my teeth decayed. It’s possible that following toxic exposure some mercury may be stored more or less safely, say in fat reserves, and mobilised by later alterations in lifestyle or diet. It may also be relevant that mercury sequesters selenium (by formation of a stable Hg-Se compound).
Phoenix,
Another possible source of mercury are some drugs for eye (including some contact lens cleaning solutions), ears and nose:
http://tinyurl.com/knbznc
Some ideas;
1) Perhaps the strong coffee drunk by many paleo dieters may be responsible for the cortisol “stickiness” in hibernation mode.
2) Perhaps dietary PUFA is a buffer against LDL elevation (and possibly rT3 hypothyroid). This explains the “Inuit paradox’ in this regard, if there is one.
3) PUFA increases LDL receptors; what if this redirects the thyroid (what if LDL leads T3 instead of the other way around? Does the thyroid have LDL receptors?)
4) perhaps squeezing both carbohydrate and PUFA at the same time is more, not less, disruptive than only squeezing down on one? (note that I achieved my lipid results above by eating less olive oil and fish than usual, as well as a zero-carb diet, although this diet was still by no means PUFA-deficient by normal standards)
Badda Bing, Badda Boom!
Here is exactly what I was talking about – the PUFA – T3 interaction!
The “Inuit paradox”!
Next time I hit the wall with a ketogenic diet I will sup some cod liver oil.
Don’cha just love it when guesses come true?
J Nutr Biochem. 2010 Oct;21(10):935-40. Epub 2009 Sep 29.
Effects of dietary fish oil on thyroid hormone signaling in the liver.
Souza LL, Nunes MO, Paula GS, Cordeiro A, Penha-Pinto V, Neto JF, Oliveira KJ, do Carmo MG, Pazos-Moura CC.
http://www.ncbi.nlm.nih.gov/pubmed/19793640
Abstract
n-3 polyunsaturated fatty acids (PUFAs) present in fish oil (FO) potently decrease serum lipids, which is also an effect of thyroid hormones. Both PUFAs and thyroid hormones affect hepatic lipid metabolism, and here we hypothesized that a long-term diet rich in n-3 PUFAs would enhance thyroid hormone action in the liver. Female rats received isocaloric and normolipid diets containing either soybean oil (SO) or FO during lactation. Male offspring received the same diet as their dams since weaning until sacrifice when they were 11 weeks old. FO group, as compared to SO group, exhibited lower body weight since 5 weeks of age until sacrifice, with no alterations in food ingestion, lower retroperitoneal white fat mass and elevated inguinal fat mass relative to body weight, with unchanged water and lipid but reduced protein percentage in their carcasses. FO diet resulted in lower serum triglycerides and cholesterol. Serum total triiodothyronine, total thyroxine and thyrotropin were similar between groups. However, liver thyroid hormone receptor (TR) ?1 protein expression was higher in the FO group and correlated negatively with serum lipids. Liver 5′-deiodinase activity, which converts thyroxine into triiodothyronine, was similar between groups. However, the activity of hepatic mitochondrial glycerophosphate dehydrogenase, the enzyme involved in thermogenesis and a well-characterized target stimulated by T3 via TR?1, was higher in the FO group, suggesting enhancement of thyroid hormone action. These findings suggest that the increase in thyroid hormone signaling pathways in the liver may be one of the mechanisms by which n-3 PUFAs exert part of their effects on lipid metabolism.
Copyright © 2010 Elsevier Inc. All rights reserved.
J Endocrinol. 2011 Oct;211(1):65-72. Epub 2011 Jul 13.
Thyroid hormone contributes to the hypolipidemic effect of polyunsaturated fatty acids from fish oil: in vivo evidence for cross talking mechanisms.
Souza LL, Cordeiro A, Oliveira LS, de Paula GS, Faustino LC, Ortiga-Carvalho TM, Oliveira KJ, Pazos-Moura CC.
http://www.ncbi.nlm.nih.gov/pubmed/21752938
Abstract
n-3 polyunsaturated fatty acids (n-3 PUFA) from fish oil (FO) exert important lipid-lowering effects, an effect also ascribed to thyroid hormones (TH) and TH receptor ?1 (TR?1)-specific agonists. n-3 PUFA effects are mediated by nuclear receptors, such as peroxisome proliferator-activated receptors (PPAR) and others. In this study, we investigated a role for TH signaling in n-3 PUFA effects. Euthyroid and hypothyroid adult rats (methimazole-treated for 5 weeks) received FO or soybean oil (control) by oral administration for 3 weeks. In euthyroid rats, FO treatment reduced serum triglycerides and cholesterol, diminished body fat, and increased protein content of the animals. In addition, FO-treated rats exhibited higher liver expression of TR?1 and mitochondrial ?-glycerophosphate dehydrogenase (mGPD), at protein and mRNA levels, but no alteration of glutathione S-transferase or type 1 deiodinase. In hypothyroid condition, FO induced reduction in serum cholesterol and increase in body protein content, but lost the ability to reduce triglycerides and body fat, and to induce TR?1 and mGDP expression. FO did not change PPAR? liver abundance regardless of thyroid state; however, hypothyroidism led to a marked increase in PPAR? liver content but did not alter TR?1 or TR? expression. The data suggest that part of the effect of n-3 PUFA from FO on lipid metabolism is dependent on TH signaling in specific steps and together with the marked upregulation of PPAR? in liver of hypothyroid rats suggest important in vivo consequences of the cross-talking between those fatty acids and TH pathways in liver metabolism.
PMID:
21752938
[PubMed – indexed for MEDLINE]
I have to take thyroid hormones, do I have to eat more than the usual 400 carb calories because of the higher glucose utilization?
Hi JP,
400 carb calories should be enough to support thyroid function (unless you’re an athlete), but it’s always good to experiment yourself and see what makes you feel best. There’s no harm in eating a bit more unless you are diabetic / have glucose regulation issues.