One of the more mysterious conditions afflicting low-carb Paleo dieters has been high serum cholesterol. Two of our most popular posts were about this problem: Low Carb Paleo, and LDL is Soaring – Help! (Mar 2, 2011) enumerated some cases and asked readers to suggest answers; Answer Day: What Causes High LDL on Low-Carb Paleo? (Mar 4, 2011) suggested one possible remedy.
On the first post, one of the causes suggested by readers was hypothyroidism – an astute answer. Raj Ganpath wrote:
Weight loss (and VLC diet) resulting in hypothyroidism resulting in elevated cholesterol due to less pronounced LDL receptors?
Kratos said “Hypothyroidism from low carbs.” Mike Gruber said:
I’m the guy with the 585 TC. It went down (to 378 8 months or so ago, time to check again) when I started supplementing with iodine. My TSH has also been trending up the last few years, even before Paleo. So hypothyroidism is my primary suspect.
Those answers caused me to put the connection between hypothyroidism and LDL levels on my research “to do” list.
Chris Masterjohn’s Work on Thyroid Hormone and LDL Receptors
Chris Masterjohn has done a number of blog posts about the role of LDL receptors in cardiovascular disease. His talk at the Ancestral Health Symposium was on this topic, and a recent blog post, “The Central Role of Thyroid Hormone in Governing LDL Receptor Activity and the Risk of Heart Disease,” provides an overview.
His key observation is that thyroid hormone stimulates expression of the LDL receptor (1). T3 thyroid hormone binds to thyroid hormone receptors on the nuclear membrane, the pair (a “dimer”) is then imported into the nucleus where it acts as a transcription factor causing, among other effects, LDL receptors to be generated on the cell membrane.
So higher T3 = more LDL receptors = more LDL particles pulled into cells and stripped of their fatty cargo. So high T3 tends to reduce serum LDL cholesterol levels, but give cells more energy-providing fats. Low T3, conversely, would tend to raise serum cholesterol but deprive cells of energy.
Other Pieces of the Puzzle
Two other facts we’ve recently blogged about help us interpret this result:
- LDL particles are not only lipid transporters; they also have immune functions. See Blood Lipids and Infectious Disease, Part I, Jun 21, 2011; Blood Lipids and Infectious Disease, Part II, Jul 12, 2011.
- T3 becomes low when glucose or protein are scarce. Thyroid levels alter to encourage resource utilization when resources are abundant and to conserve resources when they are scarce. See Carbohydrates and the Thyroid, Aug 24, 2011.
We can now assemble a hypothesis linking low carb diets to high LDL. If one eats a glucose and/or protein restricted diet, T3 levels will fall to conserve glucose or protein. When T3 levels fall, LDL receptor expression is reduced. This prevents LDL from serving its fat transport function, but keeps the LDL particles in the blood where their immune function operates.
If LDL particles were being taken up from the blood via LDL receptors, they would have to be replaced – a resource-expensive operation – or immunity would suffer. Apparently evolution favors immunity, and gives up the lipid-transport functions of LDL in order to maintain immune functions during periods of food scarcity.
High LDL on Low Carb: Good health, bad diet?
Suppose LDL receptors are so thoroughly suppressed by low T3 that the lipid transport function of LDL is abolished. What happens to LDL particles in the blood?
Immunity becomes their only function. They hang around in the blood until they meet up with (bacterial) toxins. This contact causes the LDL lipoprotein to be oxidized, after which the particle attaches to macrophage scavenger receptors and is cleared by immune cells.
So, if T3 hormone levels are very low and there is an infection, LDL particles will get oxidized and cleared by immune cells, and LDL levels will stay low. But if there is no infection and no toxins to oxidize LDL, and the diet creates no oxidative stress (ie low levels of omega-6 fats and fructose), then LDL particles may stay in the blood for long periods of time.
If LDL particles continue to be generated, which happens in part when eating fatty food, then LDL levels might increase.
So we might take high LDL on Paleo as a possible sign of two things:
- A chronic state of glucose deficiency, leading to very low T3 levels and suppressed clearance of LDL particles by lipid transport pathways.
- Absence of infections or oxidative stress which would clear LDL particles by immune pathways.
The solution? Eat more carbs, and address any remaining cause of hypothyroidism, such as iodine or selenium deficiency. T3 levels should then rise and LDL levels return to normal.
Alternatively, there is evidence that some infections may induce euthyroid sick syndrome, a state of low T3 and high rT3, directly. And these infections may not oxidize LDL, thus they may not lead to loss of LDL particles by immune pathways. So such infections could be another cause of high LDL on Paleo.
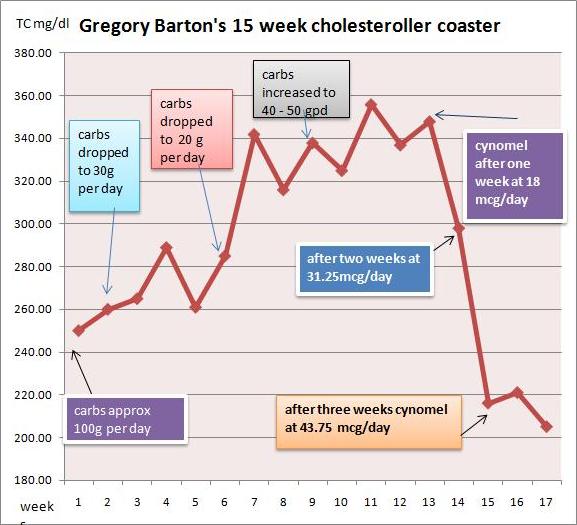
Gregory Barton’s Experience
Gregory Barton is an Australian, 52 years old, living in Thailand, where he keeps goats, makes goat cheese and manages a large garden which can be seen on http://www.asiagoat.com/.
Gregory left a comment with an intriguing story, and I invited him to elaborate in a post. Here’s Gregory’s story. – Paul
Gregory’s Writing Begins Here
One of the claims of low carb dieting is that it will normalize the symptoms of metabolic syndrome. Blood pressure, blood sugar and blood lipids, it is claimed, will all come down on a low carb diet, in addition to weight. For most people this happens. But there is a significant minority of people on Paleo and other low carb diets whose blood lipids defy this claim. (See the list of low-carb celebrities with high LDL in this post.)
Why should this happen? Why should some people’s lipids fall on low carb while other people’s lipids rise? Suboptimal thyroid might be the proximate cause for lipids rising on a low carb or paleo diet. Broda Barnes and Lawrence Galton have this to say about thyroid disorders:
“Of all the problems that can affect physical or mental health, none is more common than thyroid gland disturbance. None is more readily and inexpensively corrected. And none is more often untreated, and even unsuspected.” — Hypothyroidism: The Unsuspected Illness
I went very low carb in April in an effort to address metabolic issues, eating as little as 15grams carbohydrate per day. I had great results with blood pressure, sleeping, blood sugar and weight loss. But lipids bucked the trend.
I had expected triglycerides and cholesterol to drop when I cut the carbs, but they did the opposite: They surged. By July my total cholesterol was 350, LDL 280, and triglycerides bobbed around between 150 and 220.
I did some research and found several competing theories for this kind of surge:
- Saturated fat: The increase in saturated fat created a superabundance of cholesterol which the liver cannot handle. Also, Loren Cordain has claimed that saturated fat downregulates LDL receptors.
- Temporary hyperlipidemia: The surge in lipids is the temporary consequence of the body purging visceral fat. Jenny Ruhl has argued that within a period of months the situation should settle down and lipids should normalize.
- Hibernation: The metabolism has gone into “hibernation” with the result that the thyroid hormone T4 is being converted into rT3, an isomer of the T3 molecule, which prevents the clearance of LDL.
- Malnutrition: In March, Paul wrote that malnutrition in general and copper deficiency in particular “… is, I believe, the single most likely cause of elevated LDL on low-carb Paleo diets.”
- Genetics: Dr. Davis has argued that some combinations of ApoE alleles may make a person “unable to deal with fats and dietary cholesterol.”
I could accept that saturated fat would raise my cholesterol to some degree. However, I doubted that an increase in saturated fat, or purging of visceral fat, would be responsible for a 75% increase in TC from 200 to 350.
There are two basic factors controlling cholesterol levels: creation and clearance. If the surge was not entirely attributable to saturated fat, perhaps the better explanation was that the cholesterol was not being cleared properly. I was drawn to the hibernation theory.
But what causes the body to go into hibernation? According to Chris Masterjohn, a low carb diet could be the cause. Although he does not mention rT3, he warns,
“One thing to look out for is that extended low-carbing can decrease thyroid function, which will cause a bad increase in LDL-C, and be bad in itself. So be careful not to go to extremes, or if you do, to monitor thyroid function carefully.”
If low carb is the cause, then higher carb should be the cure. Indeed, Val Taylor, the owner of the yahoo rT3 group, commented that “it is possible that the rT3 could just be from a low carb diet.” She says, “I keep carbs at no lower than 60g per day for this reason.”
Cortisol and Getting “Stuck” in Hibernation
So what about temporary hyperlipidemia? Bears hibernate for winter, creating rT3, but manage to awaken in spring. Why should humans on low carb diets not be able to awaken from their hibernation? There are many people who complain of high cholesterol years after starting low carb.
A hormonal factor associated with staying in hibernation is high cortisol. It has been claimed that excessively high or low cortisol, sustained over long periods, may cause one to get “stuck” in hibernation mode. One of the moderators from the yahoo rT3 group said:
High or low cortisol can cause rT3 problems, as can chronic illness. It would be nice if correcting these things was all that was necessary. But it seems that the body gets stuck in high rT3 mode.
James LaValle & Stacy Lundin in Cracking the Metabolic Code: 9 Keys to Optimal Health wrote:
When a person experiences prolonged stress, the adrenals manufacture a large amount of the stress hormone cortisol. Cortisol inhibits the conversion of T4 to T3 and favours the conversion of T4 to rT3. If stress is prolonged a condition called reverse T3 dominance occurs and lasts even after the stress passes and cortisol levels fall. (my emphasis)
What I Did
First, I got my thyroid hormone levels tested. A blood test revealed that I had T4 at the top of the range and T3 below range. Ideally I would have tested rT3, but in Thailand the test is not available. I consulted Val Taylor, the owner of the yahoo rT3 group, who said that low T3 can cause lipids to go as high as mine have and, “as you have plenty of T4 there is no other reason for low T3 other than rT3.”
I decided to make these changes:
- Increase net carbs to ~50 grams per day. Having achieved my goals with all other metabolic markers I increased carbs, taking care that one hour postprandial blood sugar did not exceed 130 mg/dl.
- Supplement with T3 thyroid hormone.
- In case the malnutrition explanation was a factor, I began supplementing copper and eating my wife’s delicious liver pate three times per week.
I decided to supplement T3 for the following reasons:
- The surge in TC was acute and very high. It was above the optimal range in O Primitivo’s mortality data.
- I increased carbs by 20-30g/day for about a month. TC stabilized, but did not drop.
- The rT3 theory is elegant and I was eager to test my claim that the bulk of the cholesterol was due to a problem with clearance rather than ‘superabundance’.
What happened?
I started taking cynomel, a T3 supplement, four weeks ago. After one week triglycerides dropped from 150 to 90. After two weeks TC dropped from 350 to 300 and after another week, to 220. Last week numbers were stable.
Based on Paul’s recent series on blood lipids, especially the post Blood Lipids and Infectious Disease, Part I (Jun 21, 2011), I think TC of 220 mg/dl is optimal. As far as serum cholesterol levels are concerned, the problem has been fixed.
I believe that thyroid hormone levels were the dominant factor in my high LDL. Saturated fat intake has remained constant throughout.
My current goal is to address the root causes of the rT3 dominance and wean myself off the T3 supplement. I hope to achieve this in the next few months. My working hypothesis is that the cause of my high rT3 / low T3 was some combination of very low carb dieting, elevated cortisol (perhaps aggravated by stress over my blood lipids!), or malnutrition.
Another possibility is toxins: Dr Davis claims that such chemicals as perchlorate residues from vegetable fertilizers and polyfluorooctanoic acid, the residue of non-stick cookware, may act as inhibitors of the 5′-deiodinase enzyme that converts T4 to T3. Finally, Val Taylor claims that blood sugar over 140 mg/dl causes rT3 dominance. I couldn’t find any studies confirming this claim, and don’t believe it is relevant to my case. Val recommends low carb for diabetics to prevent cholesterol and rT3 issues but warns not to go under 60g carb per day.
Issues with T3 Supplementation
There are some factors to consider before embarking upon T3 supplementation:
- Preparation: In order to tolerate T3 supplement you have to be sure that your iron level and your adrenals are strong enough. This requires quite a bit of testing. I’ve read of people who cut corners with unpleasant results.
- Practicalities: T3 supplementation requires daily temperature monitoring in order to assess your progress. People who are on the move throughout the day would find this difficult.
- Danger: Once you get on the T3 boat you can’t get off abruptly. Your T4 level will drop below range and you will be dependent on T3 until you wean yourself off. If you stopped abruptly you could develop a nasty reaction and even become comatose.
My advice for anyone doing very low carb
As Chris Masterjohn said, in the quote above, if you are going to do very low carb, check your thyroid levels. I would add: Increase the carbs if you find your free T3 falling to the bottom of the range. It might be a good idea to test also for cortisol. A 24-hour saliva test will give you an idea whether your cortisol levels are likely to contribute to an rT3 issue. It might also be a good idea to avoid very low carb if you are suffering from stress – such as lipid anxiety!
Gregory Barton’s Conclusion
I also think my experience may help prove thyroid hormone replacement to be an alternative, and superior, therapy to statins for very high cholesterol. Statins, in the words of Chris Masterjohn,
“… do nothing to ramp up the level of cholesterol-made goodies to promote strength, proper digestion, virility and fertility. It is the vocation of thyroid hormone, by contrast, to do both.”
Paul’s Conclusion
Thanks, Gregory, for a great story and well-researched ideas. The rapid restoration of normal cholesterol levels with T3 supplementation would seem to prove that low T3 caused the high LDL levels.
However, I would be very reluctant to recommend T3 supplementation as a treatment for high LDL on Paleo. If the cause of low T3 is eating too few carbs, then supplementing T3 will greatly increase the rate of glucose utilization and aggravate the glucose deficiency.
The proper solution, I think, is simply to eat more carbs, to provide other thyroid-supporting nutrients like selenium and iodine, and allow the body to adjust its T3 levels naturally. The adjustment might be quite rapid.
In Gregory’s case, his increased carb consumption of ~50 g/day was still near our minimum, and he may have been well below the carb+protein minimum of 150 g/day (since few people naturally eat more than about 75 g protein). So I think he might have given additional carbs a try before proceeding to the T3.
Gregory had a few questions for me:
GB: What if one is glucose intolerant and can’t tolerate more than 60 grams per day without hyperglycemia or weight gain?
PJ: I think almost everyone, even diabetics, can find a way to tolerate 60 g/day dietary carbs without hyperglycemia or weight gain, and should.
GB: What if raising carbs doesn’t normalize blood lipids and one finds oneself ‘stuck in rT3 mode’?
PJ: I’m not yet convinced there is such a thing as “stuck in rT3 mode” apart from being “stuck in a diet that provides too few carbs” or “stuck in a chronic infection.” If one finds one’s self stuck while eating a balanced diet, I would look for infectious causes and address those.
Finally, if I may sound like Seth Roberts for a moment, I believe this story shows the value of a new form of science: personal experimentation, exploration of ideas on blogs, and the sharing of experiences online. It takes medical researchers years – often decades – to track down the causes of simple phenomena, such as high LDL on low carb. We’re on pace to figure out the essentials in a year.











In my first post (July 2) above, I had read Masterjohn’s explanation (link above) that LDL increases during the initial months of starting a LC paleo diet as the liver is purged of FFAs that get released into the blood stream, especially in the case of non-alcoholic fatty liver (NAFLD) which I have.
At the time of my last lipid profiles (link posted above also), I was also consuming approx. 4g of FO. Sound reasonable I could be on hepatic overload and increased cholesterol synthesis from FFA clearance and too much FO causing serum LDL to spike? What I can’t figure out is why there was an accompanying decrease in HDL. The unusual spike in my HGBA1C is also supported by Kresser’s article regarding excess FO.
There are a few ways FO PUFA can influence lipids; by increasing hepatic fat burning; by decreasing triglyceride expression; by peroxidation driving inflammation.
It seems like a pretty dose-and-time sensitive tool for lipids. Unpredictable at levels that give convincing results.
I’d rather use it as needed for other things.
If PUFAs and statins are the answer to high LDL, maybe it has been a stupid question all along…
Hi Adam,
Congratulations on getting rid of the high cholesterol. Now your cholesterol is actually a bit low. I wouldn’t worry about it unless it persists even after a long period of time on a high-fat diet. If it does, I would get checked for protozoal infections. But it’s most likely some transient effect due to all the changes you’ve been going through.
Hi Paul, I’ve switched to Paleo only a week ago. I took a blog test today, in brakets, I’m adding my last blod result from January.
Cholesterol total 2.87 g/L (2.28)
7.42 mmol/L (5.90)
Triglycerides 0.74 g/L (.78)
0.85 mmol/L (.89)
HDL CHOLESTERLO 0.72 g/L (.61)
Cholesterolol/HDL 4.00 (3.7)
LDL Dosage direct 2.01 g/L (1.44)
Also my fasting Glycemie is at 0.79 g/L compared to 0.95 of previous blood work.
I think in only a week I might have gone way to Low Carb.
I’ve always had my cholesterol higher than 200 in in the 220 range. I 38 and weight 44 kg.
This week I cut out all grains, dairy and legumes. I’m eating meat, eggs and fruit.
Should I just increase my safe starches?
Hi ItalianPaleo,
Yes, you should absolutely increase safe starches. About 1/2 kg per day is best.
Also nutritional deficiencies can matter. Include 1/8 kg beef or lamb liver per week, 3 egg yolks per day, shellfish, seafood, and seaweed among your foods.
Paul, thank you very much for you prompt response.
I should have mentioned that I do eat regularly (every week): oysters, clams and other shellfish and also offals. Foie gras it’s much more affordable where I live. And use veal stock reduction (demi glaze) to flavor my food.
From my blood work it also came out that I’m almost too high in folates 20.00 ng/mL (range 3.1 to 20.5)
and I’m at the border for magnesium 25 mg/L (range 16-26).
I’m still following your old supplement recommendations because I honestly feel bad at waisting the big supply I bought.
Given my love for offals and my tendency for high cholesterol, I feel a little uneasy eating also so many yolks and getting worried about overdoing and taking wrong supplements. I can see though-since I start supplementing- I don’t loose so many hair as before (and according to my husband white hair are less noticeable)
Thanks for all the work your putting here. Looking forward for your new book.
Meanwhile, I’ll leave in the next few days some tasty recipes for lamb liver in the recipe section.
Regards
Been low carbing for about a year and a half (though not as strict). Did not get a baseline test, but when I got my lab results I had a high TC, barely low HDL, “dangerously” high LDL.
My triglycerides were really low and blood pressure was normal. I had a high white blood cell count though. I wonder if this has to do with the LDLs oxidizing with the harmful particles and the white blood cells are floating around cleaning it up.
If triglycerides are low then a) the LDL calculation won’t be accurate (it is calculated, not measured) and b) the LDL particles will be larger thus less problematic.
But how high is your high? Doctors have very low thresholds these days. And they don’t have a “too low” level, which they ought to have.
http://healthydietsandscience.blogspot.co.nz/2012/10/patients-hospitalised-with-mental.html
Recent thinking is that your omega 6:3 ratio, vit D level, fasting triglycerides and blood glucose are directly causative disease factors that can be measured, compared to which cholesterol counts are as useful as phrenology.
Low cholesterol, that should be the disease marker.
http://www.ncbi.nlm.nih.gov/pubmed/22870570
Thanks. Everything looked good except for my total cholesterol and LDL (which would affect the total). Not too bad since I hardly do any exercise.
The white blood cell count might be a number of things though.
I’m curious as to what the actual TC and LDL counts were!
Look at this:
http://homepages.slingshot.co.nz/~geoff36/LDL_mg.htm
“For those of us on a low carbohydrate lifestyle – the “Iranian” formula used above can perhaps give a better “estimation” of LDL when our Triglycerides are nice and low. However the Iranian study was made with people with elevated cholesterol. Hopefully one day, a study may be done with “healthy” people (and thus develop a more accurate formula)”
My TC was 247 with an LDL of 193 (173 adjusted to the Iranian formula).
Could be better.
From a PHD perspective, it sounds pretty good except guessing your HDL could be higher.
http://perfecthealthdiet.com/2012/02/ris-a-la-mande/comment-page-1/#comment-54344
Also, Chris Masterjohn has been consistently indicating that a key marker is TC:HDL <3 ideally, <4 pretty good.
Hi Nathaniel,
LDL is indeed high. The most common cause is hypothyroidism or low iodine, next most common is oxidative stress and/or antioxidant deficiency (zinc, copper, selenium, iodine) leading to high production of oxLDL which isn’t cleared as easily. There are other possible causes, and both factors (or more) can be in play.
High white blood cell counts are a sign of infection and generate oxidative stress.
So I would address possible nutritional factors, get a thyroid test and treat any hypothyroidism even if it is subclinical, and get retested. It could be that a transient infection caused a transient LDL elevation and HDL depression. I would also try to track down the cause of the high WBC count if it doesn’t go away.
My personal thoughts anyway, take them for what they’re worth.
Depends whether you have risk factors for heart disease (high BP, BMI, smoking, etc) or for something else (family history of cancer or mental illness, for example), in which case it might well be quite comforting…
Probably doesn’t mean too much either way.
Getting more omega 3 – eating an extra meal of fish instead of one of pork or chicken, more leafy greens, fewer nuts – might lower it without compromising anything.
Hi all,
I suggest you listen to Chris Kresser’s latest podcast on Robb Wolf’s site:
http://robbwolf.com/2012/09/25/chris-kresser-episode-151/
He is now adopting Dr Daysrping’s thesis that it is particle number, not particle size which creates a risk for atherosclerosis:
http://livinlavidalowcarb.com/blog/the-llvlc-show-episode-585-lipidologist-dr-thomas-dayspring-explains-the-truth-about-cholesterol/14485
As for my progress, I’ll write a short note below.
Gregory
It’s now a year since I wrote the article for Paul. Here’s a brief rundown of what happened since:
I weaned off T3 taking my last dose early January this year.
I implemented Paul’s suggestion of selenium and iodine supplementation and 100g carbs per day from starch.
I had great results for the first three months post weaning:
i. Daily average body temperature went up to its highest.
ii. TC/LDL came down from post-weaning 275/190 to 220/140
iii. Trig stayed in the mid 50’s.
iv. HDL stayed in the 50’s.
I tested in three consecutive months: February, March and April of this year: results were consistent.
I was feeling good some days: good energy, lack of drowsiness. But not consistently. Some days I was lackluster and hands and feet were cold.
In July this year I retested:
TC: had returned to 280
LDL-C 190
Trig: 110
Hba1c: 5.6 (up from 5.1 previous test)
I was also putting on weight.
I tested postprandial blood sugar and found that I was getting spikes of 150 to 180 but only when eating 200g fish or meat and 100g of starch. If I ate the meat or fish with salad blood sugar was normal (less than 120) 1 hr after eating.
In mid-august I decided to go back on thyroid supplementation and cut starch to 100g rice or sweet potato with breakfast and no starch at dinner. (I only eat twice a day.) This time I chose natural dessicated thyroid.
I did so for the following reasons:
i. rising LDL, Hba1c and trig despite eating 100g carbs per day;
ii. postprandial blood glucose spikes above safe levels
iii. increased weight
iv. lingering hypothyroid symptoms: inconsistent energy and cold feet/hands
v. TSH around 2.5
After one month:
LDL-C dropped 50 points from around 190 to 140
Trig: from 110 to 85.
In reflection I think I have always been mildly hypothyroid and would probably have benefited from thyroid supplementation for years, perhaps decades.
I agree that Paul’s formula is the first strategy to try if your cholesterol is high. However, for those of us who are hypothyroid with abnormal blood sugar control I think it is more important to cut carbs to tolerable postprandial blood glucose levels, get trigs under 90 and supplement thyroid.
Hi Gregory,
Just a few cautions from my own thyroid journey and the extensive experiences of my endo (who after many years of exclusively treating hypothyroidism has found problems with both conventional and “holistic” treatment approaches).
I’d look out for a decline over time in how you feel on the thyroid extract. It seems to be much too rich in T3 for most people. Initially people feel fantastic because they’re starved for T3 (from the hypothyroidism itself or the standard T4-only treatment). But eventually they get overdosed on T3 and start to feel awful. We hypothyroids do tend to need T3 as well as T4 supplementation, but only a fraction of the amount in pig thyroid extract.
I’d also take some of the tests you’re using with a large grain of salt. My endo doesn’t even measure free T3 or rT3 anymore because he found they never added anything to simply asking patients how they feel and watching TSH and T4 levels to guard against gross underdosing or overdosing. No one has any idea what *your* T3 or rT3 (or even TSH or T4) levels should be. The only way to find out is to experiment with various amounts of T4 and T3 supplements and figure out what works best for you. My endo’s books provide a lot of guidance, but in the end trial and error is the only way.
The same goes for body temps (with apologies to Barnes). They vary for many reasons. For example, those of us on lower-carb diets have “low” body temps and free T3 levels, whether hypothyroid or not. It’s likely a healthy, physiological adaptation. As you may know, some low-carb docs such as Ron Rosedale believe it’s extremely beneficial. My early AM temp, for example, is always 96.9, even when my TSH is near zero and I’m obviously overdosed on thyroid supplements.
Regardless, just suggesting to be skeptical of *everything* you read about hypothyroidism and try to avoid being misled by tests or theories that could lead you down rabbit holes.
Good luck!
http://www.amazon.com/Functional-Approach-Hypothyroidism-Traditional-Alternative/dp/1578263875/ref=sr_1_3?ie=UTF8&qid=1349355604&sr=8-3&keywords=kenneth+blanchard+thyroid
The pig thyroid is approx 3 parts T4 to 1 part T3. What fraction do you suggest we need? Is it not a matter of suck-it-and-see?
I think your endo is right. As I mentioned below, I don’t think blood tests can determine that you are not hypothyroid. How you feel is a necessary guide. But there are long term issues in hypothyroidism that won’t necessarily show symptoms until they are well developed, such as heart disease.
I agree that experimentation with T3 and T4 is the way to go and I agree with your test “figure out what’s best for you”.
I am not persuaded that low body temperature is beneficial. If I were taking a maximum dosage of thyroid and my temperature were 96.9 I would suspect low cortisol.
I agree with your sceptical approach. Hypothyroidism seems to be one of the great mysteries of modern medicine. Thanks for the book recommendation.
Oh, please ask Dr Kenneth to publish his book in kindle form.
Hi Gregory,
“The pig thyroid is approx 3 parts T4 to 1 part T3. What fraction do you suggest we need? Is it not a matter of suck-it-and-see?”
My endo has found that, on average, people feel best with T3 dose (from either synthetic T3 or thyroid extract) about 1.5% of the T4 dose. Yes, a fraction of the amount in pig thyroid extract itself.
Part of this discrepancy may have to do with differences between people and pigs, but a lot probably results from differential absorption in the digestive system and different processing in the liver. T3 is known to be absorbed much better than T4, for example.
That said, he has found that patients differ widely. A few seem to do fine on the standard of care (T4-only therapy). A few seem to feel great on 100% thyroid extract, as the holistic docs often recommend. The great majority do best on approximately 1.5% T3, but there is still a big range and he has found no lab test that can tell him where a given individual should be in that range. Experimentation is the only way, with TSH and free T4 monitored to avoid gross mis-dosing and provide clues about directions to move does in when people feel poorly.
“I don’t think blood tests can determine that you are not hypothyroid. How you feel is a necessary guide. But there are long term issues in hypothyroidism that won’t necessarily show symptoms until they are well developed, such as heart disease.”
Yes, and another heretical aspect of his practice is to offer a trial of thyroid hormone to any patient who has symptoms or signs that could be consistent with hypothyroidism, regardless of lab values (unless of course they show frank hyperthyroidism). It’s safe, cheap, and pretty definitive. He does not want people suffering for years, and possibly getting very ill as you say, because doctors follow the standard of care and deny thyroid hormone to people because their TSH is “normal.”
As with the other labs, apart from gross abnormalities he has found no way to determine what TSH a given person’s body wants to be at. Some patients consistently feel best with TSH<1, others with TSH more like 3. Some even seem to be OK with frankly hypo TSH levels, though it is not recommended to stay there. This is one reason I think no one should recommend seeking particular TSH levels in general. Our optimal level varies too much, as with so much else.
"I am not persuaded that low body temperature is beneficial. If I were taking a maximum dosage of thyroid and my temperature were 96.9 I would suspect low cortisol."
I'm not sure either–another area where, really, no one knows anything I think. I have had my salivary and serum adrenal hormones checked and they are normal. Cortisol was a bit on the low side, but followed the normal pattern through the day. My doc thought it was clearly a good "low," showing good stress management, not one suggesting adrenal fatigue. But again I'm not really sure anyone can say for sure.
Other than possibly taking megadoses of T3 that would make me feel much worse, I'm not sure what I can do about the low body temp anyway. I consider it normal for me. And by the way while I do eat low carb, it is not VLC and my body temp has been low my whole life through many dietary changes ranging from vegetarian low-fat to VLC high fat and everything in between.
"Hypothyroidism seems to be one of the great mysteries of modern medicine."
Yes, and almost every time I seriously look into other aspects of medicine I also come away questioning how much anyone really knows. Very little of what doctors do is supported by real evidence.
I do highly recommend my doc's upcoming book. I really think he has figured a lot of this out, and he did it by careful experimentation in close collaboration with his patients over many years, not theorizing or conducting mouse experiments or hiding behind medical dogma.
Bill,
With all due respect to Ron Rosedale, low body temperature due to calorie or severe carbohydrate restriction could increase your suscetibility to infections, and chronic infection is, IMHO, THE most probable cause of Hashimoto’s.
http://www.ncbi.nlm.nih.gov/pubmed/19424864
http://www.ncbi.nlm.nih.gov/pubmed/22813720
http://www.sciencedaily.com/releases/2010/12/101222121610.htm
Can anyone comment on whether subclinical hypothyroidism might increase longevity?
Not if it increases your chances of heart disease and chronic infection.
Well, for example, running your body at a lower metabolism might slow down aging, if aging is a process your body initiates rather than resists.
No, I don’t believe it does. Carb+protein restriction, which reduces thyroid hormone levels, probably does.
Thanks, Mario. I concur. So much of our biology evolved to happen at a particular temperature, there’s no way other temperatures can be equally healthy.
Hi Paul,
“So much of our biology evolved to happen at a particular temperature, there’s no way other temperatures can be equally healthy.”
That makes sense, but like everything else body temps vary quite a lot in healthy people. How can anyone know what the right body temp is for a given person within the range of normal variation? Same with TSH or LDL or blood pressure, etc., etc.
Even two standard deviations or more from the population mean still comprises a huge number of healthy people who may or may not be at their optimal levels. How would we know?
And this does not even take into account people, like you and me, who are hugely different, in diet or other key factors, from the population that generated the “normal” mean value. This is why, for example, doctors have no evidence-based way to evaluate people like me, on low carb with high LDL-C but superb HDL, TG, CRP, etc.
HI Mario,
I’m not sure about what an optimal body temp is for me or anyone else, but to me those references don’t provide evidence of dangers to people like me with low temps. One study is about calorie restriction, the second about medically-induced hypothermia, and the third seems to be nothing more than a mathematical model.
If the low carb/low T3/low body temp combination really promotes infections, it seems surprising that so many docs use low carb with such success yet haven’t observed it. It’s always the case that people may not see if they are not looking, so it could be true and I’d be curious if there’s any better evidence of it.
I was mainly saying that I’m not sure it’s wise to use body temps as a means to evaluate hypothyroidism therapy a la Barnes. I suspect the reality is hugely more complicated and it would be very easy to be misled, as with lab values.
If you look at this paper by Broda Barnes, you see that almost all of his patients ended up with total cholesterol 180-200 by eating desiccated thyroid: http://www.ncbi.nlm.nih.gov/pubmed/13796871
So 180-200 seems to be a very common total cholesterol level in people with a healthy thyroid hormone function.
I highly recommend Broda Barnes, “Hypothyroidism: the unsuspected illness”.
Barnes speculates that 40% of the population in the US has sub-optimal thyroid function. (Correlating with a 50% drop in child mortality over the 19th century.)
His chapter on heart disease is worth reading. Barnes compared records of his patients over 20 years with the population in the Framingham study. His patients were not told to stop smoking or change their diet. All were supplementing thyroid. He found that among his patients the incidence of heart disease was only 6% of what would otherwise have been expected in a population of that size using the Framingham results as a control.
This is a powerful reason to get your sub-optimal thyroid function up to optimal.
Interesting Gregory, thanks for the update.
What is considered optimal thyroid? My oral temp tends to be around 97.5-97.9 and TSH 1.76, fT3 2.53 eating 125g starchy carbs. So not diagnosed as hypothyroid.
My blood sugar and trigs are good, but high cholesterol. Part of me thinks I should have warmer body temps independent of other symptoms.
Should I be considering desiccated thyroid and aim for 98.6 temps and better thyroid labs?
According to Barnes, optimal thyroid is that which gives a basal temperature of 97.8 to 98.2. He instructed his patients to shake down a mercury thermometer at night, leave it by the bed and take your temperature in the morning, while lying still in bed, by placing the thermometer under armpit – not the tongue for ten minutes.
The yahoo group that I visited takes the average of three readings with a mercury thermometer – under the tongue – taken at three hour intervals after rising. They aim for an average of 98.6 plus or minus 0.2 consistently from day to day.
If the oral temps that you report are taken during the day I would suggest your thyroid is not optimal. Your low fT3 would confirm it.
Barnes says that blood tests will tell you only what’s going on in the blood, not in the cells where thyroid is being used. So blood tests will not tell you that you are not hypothyroid – only that you are.
Your free T3 looks pretty low. Did you do free T4? If it’s over 1.4 you might have an rT3 dominance issue.
If you are eating 125 grams of starchy carbs (around 400g of rice per day or 600g of sweet potato) – as opposed to 400g of starchy vegetables (30 to 40g of carbs) and your freeT3 is still 2.5 I would suggest considering thyroid supplementation.
correction: last paragraph should read “- as opposed to 125 grams starchy vegetables”
I’ve been using a Vicks digital thermometer, just randomly during the day (never upon waking) and not recording. It seems Dr. Rind recommends digital:
http://www.drrind.com/therapies/metabolic-temperature-graph
I’m afraid I don’t have fT4, despite my efforts to have it included.
Yes, 125g of starchy carbs from potatoes, sweet potatoes, rice.
So, is this thyroid supplmentation a safe DIY sort of thing, or a Dr. prescription is needed?
Thanks again!
I’ve tried both digital and mercury and found a difference of 0.3. Which is right? I can’t say. I don’t have a standard to measure against. Dr Rind recommends a particular brand of digital. He claims it to be accurate. But what is his benchmark?
You have to decide for yourself whether to DIY or consult a doctor. According to Dr Barnes thyroid supplementation puts a strain on your heart. It can be fatal for people who have just had a heart attack if they take too much. For healthy people if you overdo it you’ll feel like you’ve drunk too much coffee for a day or two. No big deal. If you decide to DIY I suggest you consult a support group, such as the yahoo group I used.
And read Dr Barnes. He has a chapter on dosing.
This is all very helpful information for me. I’ve got my first endocrinologist appointment coming up in Denver. (had to schedule 6 mo. in advance to get it) I’m a 50 yr. old woman, TSH 3.8 with 4 benign thyroid nodules. In looking back at old blood tests over the last dozen years, I saw that my TSH has usually been in the 3s or even 4s but I’ve never been aware of having any major hypothyroid symptoms. I started eating low carb (about 100g/day) 1.5 years ago after realizing I had poor blood sugar control. Recent test showed TC 241, LDL 133, Trig 42, HDL 99, Hba1c 5.2.
My question is: do I need to be on thyroid even if I feel fine? Sounds like it might be better for my health.
(also – test from a year ago showed T3 at 2.5 and T4 at 1.27, will retest this before endo appt.)
Hi Mary,
Well, your lipids and blood sugar are excellent, so they give no sign of hypothyroidism either, despite the high TSH.
If it were me I might try an experiment with the lowest possible dose of T4 to see if that makes you feel better. But I wouldn’t do anything dramatic. Discuss it with your doctor.
Thanks, Paul. Your blog is such a great source of info.
I think Paul’s advice is excellent. If there’s any reason to suspect hypothyroidism (lab results, symptoms, or signs), a trial of T4 is the only way to see if you need supplementation.
Your endo will likely not agree, however. It is a heretical position now that TSH has been accepted as a definitive test for hypothyroidism.
You could also consider the Abraham iodine protocol. People with early stage hypothyroidism can sometimes completely reverse the condition with 25-50 mg of iodine per day as part of the complete protocol (don’t just take the iodine and ignore the rest, could be not so healthy).
Do any of you have a reaction to this: I finally went to the endocrinologist – she made sure the nodules were still ok and looked at my new labs: TSH 2.9, T4 1.36, T3 2.8, TPO had gone up from 78 a year ago to 111 now. She said T3 doesn’t matter because the T3 is in the cells not the blood. She also said quit taking potassium iodide (For about 6 months I had been taking 300 mcg/day, not more because of all the mixed reviews I’d seen about iodine and Hashimotos). She said I could take iodine but not potassium iodide as that’s what they prescribe to Graves patients to shut down thyroid output. Isn’t potassium iodide just a form of iodine? In any case, I quit all iodine.
Hi Mary,
I think your endocrinologist is confused. High doses of potassium iodide may on rare occasions be given to interrupt a thyroid storm, but those doses will be much higher than 300 mcg. Potassium iodide dissolves in water in the digestive tract into free potassium and free iodine, so it is the same as taking iodine and potassium separately.
Yeah, it didn’t make a lot of sense to me. How can iodine be ok but potassium iodide not be? I noticed that potassium iodide is how they put iodine into Morton’s salt. I’m going to go without any iodine supplements for 2-3 months and see if TSH or TPO changes, then decide about taking low dose of T4.
The endo doesn’t understand as much as he should about iodine, but I don’t think he’s confused about the different forms of it.
I think he meant that he thought it was OK to take iodine (i.e, molecular iodine) as opposed to iodide (in this case the potassium salt). They are not the same thing (different redox states). The thyroid needs iodide while some other tissues need molecular iodine.
They may interconvert in the body, but because we need both, traditional Lugol’s iodine as well as Dr. Abraham’s Iodoral contain both forms.
Endos are taught that iodide above tiny doses can be dangerous to those with thyroid disease. I still think that the Iodine Project has shown pretty conclusively that’s not true (apart from autonomous functioning thyroid nodules) as long as a complete nutritional protocol, i.e. Dr. Abraham’s iodine protocol, is used.
Hi Bill,
I don’t believe there’s going to be a difference. Once ions are in solution, they’ll exchange electrons until they reach an equilibrium degree of ionization. The iodine/iodide balance will be determined physiologically, not by the form of the supplement.
I don’t have access to the full paper, so I don’t know how large a difference in thyroid assimilation the iodine and the iodide form had, but it seems the difference was there: Differences in the distribution of iodine and iodide in the Sprague-Dawley rat.
here’s a later study on the Sprague-Dawley rat, “Distribution of iodine into blood components of the Sprague-Dawley rat differs with the chemical form administered”.
Conclusion “These data indicate a differential distribution of radioactivity depending on whether it is administered as iodide or iodine.
This is inconsistent with the commonly held view that iodine (I2) is reduced to iodide (I-) before it is absorbed systemically from the gastrointestinal tract”.
http://www.ncbi.nlm.nih.gov/pubmed/1433379
& here’s a later study again, where they try see if this is the same case in humans, “Comparison of the effects of iodine and iodide on thyroid function in humans”
Part of conclusion “TSH was significantly increased by the high dose of both I2 and I-, as compared to the control.
Decreases in T4 were observed with dose schedules with I- and I2, but none were statistically significant compared to each other, or compared to the control.
This human experiment failed to confirm the differential effect of I2 on maintenance of serum T4 concentrations relative to the effect of I- that was observed in prior experiments in rats.
However, based on the elevations in TSH, there should be some concern over the potential impacts of chronic consumption of iodine in drinking water.”
It should be noted that they were using ‘massive’ amounts of iodine or iodide during this study,
“A 14-d repeated-dose study utilizing total doses of iodine in the two forms at either 0.3 or 1 mg/kg body weight was conducted with 33 male volunteers.”
the link to that human study,
http://www.ncbi.nlm.nih.gov/pubmed/9761130
Thanks Darrin!
Very interesting the following from the second paper on Sprague-Dawley rats: “Twice as much radioiodine is in the form of I- in the plasma of animals treated with 125I- compared to 125I2-treated rats. No I2 could be detected in the plasma.” This seems to contradict the first study on rats: “The initial distribution of 125I to the thyroid depended sharply on chemical form, being greater when iodide rather than iodine was administered, whether animals were fed or fasted.” Perhaps it is a matter of time between administration and measuring. From the human study and simply looking at Figure 1 and Figure 2 it seems that iodine effect on thyroid is only due to “A significant but consistent amount (25%) of I2 was converted to I– in the preparation of the stock solutions.”
It still is not clear to me if there is a difference or not from supplementing iodine or iodide.
“It still is not clear to me if there is a difference or not from supplementing iodine or iodide”
I have no idea either Andrés,
Lugols has both Iodine and Iodide, supposedly for good reason (if you read up on it).
However, if you read the links below, it seems very easy for the Iodine to get converted in to Iodide. ie if taken with juice or vitamin C.
So it would seem on the face of it that any iodine would just get converted to Iodide in the body.
All far too complicated for me i’m afraid.
http://curezone.com/faq/q.asp?a=13,281,2962&q=630
http://curezone.com/forums/am.asp?i=858627
left out: TPO was 78 in test from year ago
I sometimes wonder if we pay too much attention to body temp via the thyroid only. What role does the autonomic nervous system play, especially if one has a dominant sympathetic nervous system? I find if I can activate the parasympathetic nervous system to act as vasodialater I feel warmer and my forearms/hands and feet radiate heat. It is hard to sustain though.
My use of 50mcg of SRt3 markedly improved on my thyroid labs, but I honestly felt no better for it.
Here’s a link to the site of the aforementioned Dr. Rind. The link includes a rather elaborate “matrix” for evaluating one’s thryoid health using free T3, free T4, and TSH. In my case the matrix correctly identified me as having a chronic non-thyroid infection, which I then confirmed as epstein-barr by blood test. The site does contain the major caveat that iodine supplementation may skew readings.
http://www.drrind.com/therapies/thyroid-scale
I read here
http://www.freegrab.net/Iodine%20update.htm
that “the optimal daily requirement for iodine has been estimated at 6 mg of iodide for the thyroid gland and 5 mg of iodine for the mammary glands”
I think i have also seen this interpreted as;
“the optimal daily requirement for iodine has been estimated at 6 mg of iodide for the thyroid gland and 5 mg of iodine for the rest of the body”
Just wondered if ‘Ammonium Iodide’ is just as good an Iodide form as ‘Potassium Iodide’?
I use both Iosol drops and Lugols drops.
Iosol ingredients: Iodine and Ammonium Iodide.
Lugol ingredients: Iodine and Potassium Iodide
ie. does it matter what the IodiDe form, as long as you are getting IodiDe (as well as Iodine)?
http://en.wikipedia.org/wiki/Ammonium_iodide
http://en.wikipedia.org/wiki/Potassium_iodide
I don’t know how they got that estimate.
I would think ammonium and potassium iodides would be identical in effect.
Speaking of iodine, my 24-hr. urine iodine has consistently been elevated on my last several labs.
Given this, methinks I have more than enough iodine from diet and supplementation and that I should logically not seek additional exogenous supplementation.
Anyone disagree?
Are you referring to the Abraham 24-hour iodine loading test (24 hour urine collection following a 50 mg iodine dose)? Or simply measuring iodine in 24 hour urine without the loading dose?
The latter; no loading dose.
I’m not sure what, if anything, that test result means.
I would not assume it means you are replete in iodine. Without knowing how much iodine you ingested in the previous 24 hours, it is not possible to interpret the amount you are excreting in urine. That’s why in Dr. Abraham’s loading test you refrain from iodine (from supplements or food) for 24 hours and then take a 50 mg loading dose. Then you know what percent you are retaining vs. excreting.
And even Dr. Abraham’s loading test, which was expressly designed to measure iodine sufficiency, can be misleading by itself—for example, if one is toxic in bromine, which can block iodine absorption, or if one has an iodine symporter defect
If you really want to assess your iodine sufficiency, I’d suggest the iodine loading test. If you get it a FFP Lab you can get a consult with Dr. Flechas himself to help you interpret it. I’d strongly suggest getting the bromine test as well. The test is also available, less expensively, at Hakala Labs.
Whatever iodine dose you take, you’ll eventually reach a balance at which the amount you’re losing from the body equals the amount you’re ingesting.
Since urine is a major excretion point, the urine test proves that Mark’s dietary intake of iodine is high.
After reading the revised supplement recommendations, I reduced my supplementation from 6 mg down to 1 mg. Recently had my TSH tested: 3.8 which is not ideal. And I’m having cold hands more often as well as some other hypothyroidism symptoms. I think I’ll slowly increase back up to 6 mg iodine and see if that helps, making sure I get enough selenium, of course. My cholesterol numbers are fine (total is 200). I do wonder if I messed things up by being low/very low carb for so many years.
Hi Connie,
Yes, perhaps you do better on higher iodine. Another factor is that it can take 3-4 weeks for the thyroid gland to adapt to a different iodine intake.
Thank you, Paul!
Hi Paul,
Would you explain a bit more about the ‘adaptation’ of the thyroid gland to changes in iodine intake if possible. (or provide a link if simpler)…
for instance, does an actual physical change take place…ie. will the gland expand or shrink in size depending on iodine intake. & if so, why, what is physically happening to the gland.
& would the gland possibly feel a bit sensitive to touch during times of change (adaptation).
many thanks as always
Hi Darrin,
The gland does change in size but there are also changes in expression at the cellular level in iodine-binding molecules and deiodinases.
Not sure about sensitivity to touch, which would be a sign of inflammation or thyroiditis. I don’t think that’s a necessary feature of adaptation but it may be a common occurrence.
thanks Paul,
I mentioned the sensitivity because in the past when i have increased iodine, my throat/neck has sometimes become a bit sensitive for a while.
& recently i abruptly stopped my iodine and selenium supplementation. & my throat/neck become a bit sensitive again.
However, i now think the two things are totally unrelated;
i was ‘experimenting’ with taking sodium bicarbonate for various reasons for a few weeks. In hindsight the bicarb gave me acid reflux (which i never get) & i believe ‘burnt’ my throat.
Since stopping the bicarb a couple of days ago, i think my throat is clearing up.
I probably get around 1.5mg of supplemental iodine daily, the rest from food sources, and my urine iodine remains elevated.
That’s an interesting theory, but totally wrong.
Keeping thyroid function at a nice high level only takes one high-carb meal per week. Eating 60g of carbs per day is a great way to take you out of ketogenesis, removing much of the benefit of being low carb in the first place, AND it won’t cause enough of an insulin release to get the hormonal benefits you’re looking for.
In fact you’ll probably just end up with continued hypothyroidism leading to insulin resistance. Which is probably why you only saw improvement by supplementing with exogenous thyroid hormone T3.
http://www.hindawi.com/journals/jtr/2011/152850/
You shouldn’t have to do that.
Unless someone has epilepsy or extreme intolerance to carbs, I really don’t understand this dogmatic adherence to staying in ketogenesis 24/7 even when all these “Wrong Way” signs show up — like high cholesterol and flagging energy levels and loss of fertility.
This is just as bad as raw food dogmatism. “Oh, you’re losing a bunch of muscle, you must not be eating enough fruit! You need 30 bananas a day!”
Carbs and insulin are not evil, they just need to be *applied* appropriately.
Hi Naomi,
could you clarify your definition of ‘low carb’ in this context (in carb grams or percent of calorie intake)?
it’s just that i would have thought that 60 grams (and under) of carbs is closer to vlc, at least for me anyway.
“Keeping thyroid function at a nice high level only takes one high-carb meal per week.”
Is there any evidence for this claim?
” Eating 60g of carbs per day is a great way to take you out of ketogenesis, removing much of the benefit of being low carb in the first place, AND it won’t cause enough of an insulin release to get the hormonal benefits you’re looking for.”
… assuming that everyone has the same, healthy, secondary insulin response, which is not the case.
“A” benefit of low carb is that it moderates the diet to fit the insulin response.
“In hyperthyroidism, dysregulation of this balance may end in glucose intolerance mainly due to hepatic insulin resistance. In hypothyroidism the results are less evident.” (article you quoted). The tentativeness of the conclusion speaks for itself.
I am experimenting myself with a keto diet, have hypothyroidism, and am studying Drs. Phinney and Volek’s work and book, ‘The Art and Science of Low Carbohydrate Living’. They (and Jimmy Moore) argue against Colpo and others http://anthonycolpo.com/is-a-low-carb-diet-bad-for-your-thyroid/
that it’s CR (caloric restriction) that is the issue and not VLC diets that contribute to low thyroid function. You can get plenty of dense
nutrition and calories from the 65% fat-30% protein/5% carbs keto diet.
http://livinlavidalowcarb.com/blog/do-low-carb-diets-lower-thyroid-function-lets-ask-the-experts/15305
I am still waiting to see the results of my blood work to determine if this is true in my case.
The question I STILL do not know is whether a once per week carb refeed on a CKD http://www.bodybuilding.com/fun/sclark91.htm will derail ketosis for several weeks as Phinney and Volek seem to think.
Thoughts??
Hi Mark,
Calorie restriction certainly reduces thyroid hormone levels, but so does carb and protein restriction in the absence of calorie restriction. It’s true that the most severe problems will occur when total calories are restricted as well.
A once per week carb refeed will not derail ketosis so far as I know. One goes back into ketosis fairly quickly, in a day or so.
There seems to be a ton of debate still as to solo carb restriction causing or contributing to hypothyroidism. Here’s one you hash out with the author:
http://aworldlymonk.wordpress.com/2012/04/07/low-carb-diets-and-hypothyroidism-a-false-alarm/
I would like to think we can keto-adapt as the science seems to confirm this more daily, as glucose causes more problems than it’s worth. Nonetheless, I might agree to err on the side of caution and do CKD with a big carb refeed once a week assuming it doesn’t derail ketosis. Need to confirm this with the docs in the know.
Hi Mark,
You can be in ketosis eating 50 g of starches per day if you eat MCT oil, and that’s a much healthier way to achieve ketosis. I would recommend getting some carbs every day over a weekly major refeed.
Carbsane posted this paper on pufa diets being better for ketosis.
http://jcem.endojournals.org/content/89/4/1641.full.pdf
although the actual diets in the paper are rubbish, there are anecdotal reports of it being true, and mechanisms to explain it.
While this is not optimal PHD, it could be used for a few days to trigger ketosis intially in people who find it hard to get there – I am thinking a fish, nut and coconut diet, rather than oils.
Hi George,
Well, in the study most of the SAT fats were dairy fat, which is low in MCTs; MCT oil would have been much more ketogenic than the PUFA diet vegetable seed and walnut oils.
I think the reason PUFA are more likely than SaFA to be turned to ketones is the same reason they are 3 times more likely to be turned to cholesterol: they are present in excess in most people and the body is trying to get rid of them.
So I don’t see any good reason to eat them at any stage of a ketogenic diet.
Makes sense. Also, the longer the fatty acid, the less glycerol by proportion (and the more calories per gram in real, non-Atwater terms), which might make a difference…
tho this doesn’t seem to apply to MCTs
I question whether low calories can account for high LDL – isn’t cholesterol driven by energy to some extent?
Yes, good point. Should have just said carbs.
This seems to conflict with …
Chris Masterjohn discusses how only replacing PUFA with SaFA increases cholesterol over the long term. Supported by a controlled setting of the LA Veterans Administration Hospital Study.
Also discusses the Stephan Guyenet referenced observational study and the hypothesis that increased SaFA increases cholesterol over short term, but normalizes over the long term. There are confounders with the natural setting.
Starts at 6:45:
http://www.bulletproofexec.com/podcast-16-everything-you-need-to-know-about-saturated-fat-cholesterol-with-chris-masterjohn/
PUFAs increase the requirement for cholesterol – LDL-receptors increase, serum LDL decreases, but hepatic cholesterol production is ramped up.
There is more total cholesterol in the body on a high-PUFA diet, but less in the blood.
Switching from PUFA to SFA ought to pull some of that cholesterol back into the blood, to the liver…
You can also worsen a fungal infection (like Candida and mold) on a low carb diet. That’s what happened to me just from following Wheat Belly for a few months.
And it would seem that iodine requirement may be linked to carbohydrate levels.
ie. More iodine is required as carb intake is increased, to prevent iodine deficiency.
Which i interpret as more carbs = increased thyroid activity (function?) = thyroid requires/uses/needs more iodine (due to the increased thyroid activity/function).
At least that’s my take of this study.
http://www.ncbi.nlm.nih.gov/pubmed/15142639
Tho I only have access to the abstract.
So i do not know what their definition of ‘high carbohydrate’ is.
& i do not know if they found a linear relationship between iodine requirement and carb intake ie. more carbs = more iodine needed.
“Abstract:
An increased iodine requirement as a result of significant changes in human nutrition rather than a decreased environmental iodine supply is suggested to represent the main cause of the iodine deficiency disorders (IDD).
The pathomechanism proposed is based on the fact that serum concentrations of thyroid hormones, especially of trijodothyronine (T3), are dependent on the amount of dietary carbohydrate.
High-carbohydrate diets are associated with significantly higher serum T3 concentrations, compared with very low-carbohydrate diets.
While our Paleolithic ancestors subsisted on a very low carbohydrate/high protein diet, the agricultural revolution about 10,000 years ago brought about a significant increase in dietary carbohydrate.
These nutritional changes have increased T3 levels significantly.
Higher T3 levels are associated with an enhanced T3 production and an increased iodine requirement.
The higher iodine requirement exceeds the availability of iodine from environmental sources in many regions of the world, resulting in the development of IDD.”
Interesting. Maybe going LC is why I’m throwing off a lot of iodine (don’t need much).
I agree – 50g total daily is the cutoff. That and coconut oil for the MCTs + pastured butter should work. This would be TKD (targeted keto diet) doing minimal carbs daily. 50g is only 200 calories.
What’s more important: thyroid functioning or stomach/gut functioning? I have hypothyroidism. I used to be a vegetarian. Last December / January, I went paleo. I was also told about klebsiella bacteria in a stomach analysis. I have problems with SIBO/fodmaps too. Since going low carb, my stomach has been much better. The only problem it seems is that I have less energy and can’t work out (e.g., run, CrossFit) without the carbs I cut out. So, do you think it is more important to eat enough carbs to treat hypothyroidism, and have a lot of accompanying digestive issues, or eat fewer carbs but just not be able to work out as much? I’d love to hear your thoughts as I’m nearing my wit’s end with this conundrum!
Hi Lizzie,
Well, you’d like to avoid the either-or and get both better. Have you tried simple dextrose as a carb source? It would be good to find a carb source you tolerate.
Best, Paul
If you must resort to carbs, DO NOT resort to simple ones like dextrose! That will only wreak havoc with your immune system and encourage the growth of unwanted gut bugs like the one you mentioned! Ideally, in addition to eating paleo – you should re-train your system to become keto-adapted in which your body gradually learns to become an efficient fat-burner by using ketones from fat as the main energy source as opposed to staying a glucose-burner – that is unless you’re running marathons in which boosting complex carb intake is necessary
but no man that values his health should be running marathons anyway. I am also hypothyroid and am taking T2, T3, and T4 separately in addition to experimenting with the keto diet myself. The docs that have studied this diet the most feel that with a) adequate calories, and b) no more than 50g complex carbs daily, you should maintain ketosis and not suffer the hypothyroid symptoms that have been reported empirically.
Hi Paul,
I’ve heard some essentials oils were very helpful to regulate thyroid status.
I put the link for general interest, andwould be happy to know your advice on this particular use or experience with EO and Thyroid.
http://www.jennscents.com/uploads/Aroma_Glandular_Support_Handout_11Oct.pdf
In France, D.Baudoux (a well known aromatherapist) recommends a soft massage on the neck 2 times a day (approximatively where thyroid is located)with 5 drops of this mix prepared in a bottle: 4 ml green myrtle + 1 ml clove + 30 ml Nut oil.
Best,
Maya
Image 06. Put in a $15 Blockbuster card,
movie sized candy and a bag or two of unpopped microwave popcorn.
So, oft in theologic wars The disputants, I ween,
Rail on in utter ignorance Of what each other mean; And prate about
an Elephant Not one of them has seen.
I developed LDL cholesterol of 200 being on paleo diet indulging in large quantities of coconut oil and butter with the aim of gaining weight (I did). My paleo was nowhere close to lowcarb, I have eaten lots of fruits and rice. After I significantly reduced butter and coconut oil my LDL is back to 100. No testing done but I believe I am one of the 14% of population who are Apo E4
Aha! I have been on a paleo diet for 2 months, and just had my first lipids test. My HDL is super-high (Dr didn’t share that figure) glucose is 82, BUT, my LDL has gone up from 142 a year ago to 169, and my Dr. wants to put me on statins. Yikes! Twelve years ago, I did the Protein Power Plan, and my cholesterol went way down (to 5.7 in NZ). It has crept up over the years as I added a little too much carb back into my diet.
Since starting on Paleo, my blood pressure has gone down enough that I can cautiously go off my meds. And I’ve lost 11 lbs.
Anyway, your post about coconut oil and butter being a factor rings true with me – for the first time in my life I’m eating heaps of coconut oil, and a lot more butter than ever before! I’ll post again in a few months, after cutting back / out and being re-tested. I hope that will get my LDL to go back down again.
If anyone else has any comments I’d love to hear from you!
Thanks! Anne
PJ and Gregory B,
I’ve been on a bit of a roller coaster over the last 8 months with my thyroid and cholesterol. Never great lipid profiles. I was on 1500 MG Niaspan and 4G of Lovaza up until last October. In August, I went Paleo. Meat, veggies, and small fruit. My daily carb intake is less than 50g / day.
In August, I am diagnosed as HYPERthyroid (TSH = .01 TSH), and then 3 weeks later I flop to HYPOthyroid (TSH = 73.77). I am also positive for Antibodies (+1000), so I am diagnosed as having Hashimoto’s Disease. The endo puts me on 150mcg of Levothyroxine. Cardio agrees that I could go off Niaspan and Lovaza in order to get “real” cholesterol.
I returned to endo 2 weeks ago. My TSH is .72, so technically in line. Problem is that I feel TERRIBLE. Brain fog, cold extremeties, fatigue, muscle fatigue / pain / cramping, insomnia, depression and anxiety. Endo thinks I’m fine.
Other information: Previous cardio tried me on a statin in July (in conjunction with Niaspan). I go 2 weeks, and have severe muscle impairment. I cease that one and try Crestor. Same result. I then have a VERY high CPK (1296) in early September.
Prior to starting Paleo, my lipds were:
195-230 TC
290-310 TG
110-130 LDL
22-31 HDL
Yesterday I received results, and was VERY disheartened:
TC 279
TG 140
LDL 214
HDL 37
When my thyroid went 73.77, my cholesterol went to 344, TG 160, LDL was 261 and HDL 50.
I’m thinking I might have a similiar experience as Gregory, but not sure. Can you guys help? I’m going bananas!!!!
Thanks,
Karl
Hi Karl,
It looks like there is something wrong with the thyroid and the drugs and low-carb diet probably exacerbated it.
Oxidative stress mediates thyroid damage and high-dose niacin can generate ROS. Lovaza / fish oils are easily oxidized to create toxic byproducts. Low-carb aggravates thyroid issues and stresses adrenal function. You probably have adrenal involvement now.
The normal TSH is no reassurance because thyroid hormone lives in the body for ~24 hours so you can have a normal TSH but totally disrupted circadian rhythms.
When everything’s going haywire, the sensible thing is to moderate what you’re doing:
1. Quit taking drugs.
2. Eat a more normal amount of carbs (PHD level) mainly from starches.
If you’re supplementing, make the doses moderate.
Get your diet in the middle between your pre-Paleo and current Paleo diet, along PHD lines.
Then check back in a few months. It takes time to heal the thyroid and you probably have gut involvement / dysbiosis which also takes time, but have faith, with a good diet and lifestyle and time these issues will generally heal themselves.
Paul,
Thanks for the quick response.
One thing that I forgot to mention, as it really caught my eye on this thread. I am part of the track your plaque website, and as Nancy mentions above, I am one of the APO 3/4 crowd. I’m not sure how that confounds my cholesterol either.
Best,
Karl
Karl,
First, don’t panic about the numbers. Going bananas over numbers will kill you before the numbers will. Ultimately, if you are persistent, you will work out what’s out of whack and how to fix it.
Secondly, I agree with Paul that you are taking too many drugs and getting too few results.
If you’re taking levothyroxine (T4) and you’re still having hypo symptoms, including high cholesterol, that would suggest a reverse T3 dominance. If you can increase carbs without having blood sugar issues or putting on weight, I would try that first.
If that doesn’t work, or if you have blood sugar or weight issues when raising carbs, you would probably benefit from supplementing T3 as I did in 2011. However, taking T3 only requires getting iron and cortisol tested and, if necessary, raised to optimum levels. T3 also needs to be taken a few times per day. All in all, a lot of bother. But worth it if nothing else works. The ladies moderating the yahoo rT3 group will offer guidance on how to do all of these things if you choose this route.
T3, according to the yahoo group, will also stabilize Hashimotos. You might want to research that issue since you have high antibody numbers.
T3 brought my triglycerides down dramatically. They were in the range of 150 to 220 despite being on low carb for 12 weeks. After taking the starting dose of T3 they dropped from 155 to 95 – in one week. By the end of my experiment TG was in the 50’s and 60’s.
Your HDL is consistently low. Are you eating enough saturated fat?
Greg,
Thanks for the reply. Let me make a few other clarifications / inclusions.
Since I went LC, I have lost 28 lbs.
I am currently NOT on any pharma, except the T4 supplement. I stopped the NIASPAN and LOVAZA because I wanted to get an idea of WHAT my true cholesterol is.
My typical fasting blood sugar is 95-99.
HDL – I was up to 50 in November, but has since dropped. I’ve had no excercise due to the muscle fatigue in my legs.
Saturated Fat – That’s pretty much all I eat. Along with veggies and small amounts of fruit.
TG – Considering my lack of carb intake, I’m pretty disappointed in my 140. Doesn’t make a whole of sense to me.
I got my new thyroid numbers last night:
TSH – .40 (down from .72 (2 weeks ago), so it looks like I’m headed for hyper again.
T4 – 11.3
T3 – 2.7
I don’t have RT3 yet.
I can’t thank you both enough.
Best,
Karl
Karl, TG are only improved by reducing carbs to 30% of energy. Going VLC as you have may actually worsen TG. Not sure why that happens but people have reported it. Maybe a choline deficiency.
Paul / Greg,
I just received my most recent results with the RT3. Could you interpret for me? I think this is basically what Greg describes above…..RT3 dominance.
TSH .40
T 11.3 mcg / dL (Not marked Free)
T3, free 2.7
RT3 38 Testosterone 650
Free Testosterone 84.7
Please tell me that it’s likely or at least plausible that my Cholesterol / LDL issue is due to this issue.
Thanks,
Karl
Hi Karl,
I think it’s due to eating too few carbs, and possibly other issues as well. One of the causes of RT3 dominance is that the diet is too low carb and the body is trying to prevent utilization of glucose by non-brain cells.
I think you need to normalize your carb consumption and eat a nutrient-dense, balanced diet, then see what happens. The hyperthyroidism suggests something else was involved too, besides eating insufficient carbs, but fixing the obvious carb problem will clarify symptoms and help indicate the next step.
Best, Paul
Paul / Greg,
Well, I wanted to thank both of you for your time and consideration. (I sent an email to Greg thanking him a couple of weeks ago.)
So, my recent lipid profile seems to have normalized:
TC = 217 (Down from 344 in September)
Trigs = 77 (Down from 337 last year)
LDL = 159 (Down from 261 in September)
I got off of the T4 completely. It was making me crazy. Crawling out of my skin crazy. Instead, I started using only Cytomel. The results above were achieved with only 20-25mcg of Cytomel.
Once I started on the Cytomel, I instantly felt better. I did indeed have a high RT3. That cleared in 2 weeks after initiating the Cytomel. It’s no normal.
I expect that my numbers will continue to improve as a titrate up on the Cytomel. (I’m now at 35 mcg). My goal is to get to 50-75 mcg and then retest in 4-6 weeks. I am upping 5 mcg every two weeks.
I’ve noted Greg’s warnings about Cortisol and Iron. Indeed, I did a Cortisol spit test 2 weeks ago, and I do have some adrenal insufficiency.
I was having problems with the Cytomel in the morning (my Cortisol is low is the AM and mid afternoon…..else normal ranges). So, I started splitting my doses.
My Transferrin Saturation rate is only 17%, but I want to test that again before I come to any conclusions. I did give blood 3 days before my last lipid test.
Overall I feel gobs better. Not even close.
BTW – I did know that I was ApoE 3/4, but have combined my understanding of that with what I learned here. It’s funny, for years, my doctors told me that I was a hyperproducer of cholesterol. The truth (I believe) as see it: I don’t overproduce cholesterol ….. As a 4, I hold onto it, and I don’t CLEAR it particularly well.
This does appear to confer a genetic advantage during times of food scarcity, however, in the modern day, I have food available to me at virtually every moment.
It is indeed about CLEARANCE rather than overproduction. My doctors (they just don’t get it) are confounded by all of this. I also confirmed from 23AndMe that I DO NOT have familial hypercholesterolemia.
I am a part of Dr. Davis’ Track Your Plaque Community, many of whom are what I would call statin zealots. Interfering with native cholesterol production is just crazy to me…..even as an ApoE 3/4. Some of the people on the site take their LDL down to CRAZY levels (30-50 mg).
As a 4, I really can’t think of any reason I’d want to STOP native production of cholesterol as that appears to be one of the problems of AD patients, namely crossing the BBB.
Alas, that’s a story for another day. I’ll be sure to post again after my next profile. I can’t thank you both for your time and assistance.
Chalk this one up as a success thusfar:)
Karl
Hi Karl,
That’s great news!
Your numbers are very good now and presumably would continue to improve over time if you just keep doing what you’re doing. So I question the wisdom of increasing your dose of Cytomel. 20-25 mcg might be perfect for you.
The adrenals should recover over time now that the thyroid is functioning more normally.
Thanks for sharing the good news!
Paul
Paul – I’d like to see 2 or 3 profiles before I can say that I’m good, including an advanced lipid profile so that I can get an idea of my particle count.
I’d like to see if I can get my TGs to 50, my HDL up to 50, and my LDL to fall in around 110-130. So I still have some work to do.
That would give me a very healthy 180ish total cholesterol, which is just fine. I’m NOT going below 160, which we know is a magic number for all cause mortality.
I was taking 1000mg of OTC niacin prior to this last test. I have since stopped it, because I was having fasting blood glucose of 108-100 pretty regularly. Since I stopped it, I’m 90-92 in the a.m.
So, if I depending upon what I got out of OTC niacin, I may see a slight spike up from my 159 right now, but I think that will be mitigated by my increase in Cytomel.
Your caution is noted though.
Again, I can’t thank you both enough.
The only thing I can tell your readers is that it is NOT all about hyper production. Clearance is huge, and up regulating your LDL receptors via thyroid optimization is WAY better than stopping production of something you need.
I love smart people (meaning you folks)…..Thanks again.
Best,
Karl
Re T3 dosage: The point I made to Karl is that taking 20-25 mcg of Cytomel is likely to suppress one’s endogenous production of thyroid and is unlikely to be a physiological dose. Thyroid does much more than clear cholesterol. But ultimately, we’re all different and only experimentation will reveal the optimal dose. Make sure you get Free T3 and Free T4 tests every month while upping the dosage to make sure you don’t do too much too soon. Good luck.
Greg – I am indeed under the care of a functional doctor (not an endo) who is monitoring T3, Free T3, RT3, Free T4 and T4.
I do have Hashimoto’s, so it’s really not clear to me if I want a fully functioning thyroid or not.
In September when my TSH was 73.77, my TPO antibodies were >1000. Through diet and the Cytomel, I have cut that in half.
I was told by many that I would get this “explosion” of energy once my receptors cleared T4, but it hasn’t happened.
The only trouble with the Cytomel thusfar was taking the full 25 in the a.m. I had a crazy throbbing / crushing sensation in my head. Once I split the doses I was fine.
Again, I have no desire to go backwards here, so I am monitoring closely.
Karl
Anyone interested in a cautionary view of T3 supplementation at supraphysiological doses may want to read the relevant chapter of my own endocrinologist’s new book.
After many years of experimenting with combined T4/T3 supplementation in hypothyroidism, he has found that, contrary to conventional medical orthodoxy, a little T3 is essential for most to feel well. But, contrary to much alternative medical orthodoxy, more than that is counterproductive and potentially dangerous in the long term, even though many will feel fantastic for a short time after trying it.
http://www.amazon.com/Functional-Approach-Hypothyroidism-Traditional-Alternative/dp/1578263875/ref=sr_1_1?ie=UTF8&qid=1374612196&sr=8-1&keywords=kenneth+blanchard+hypothyroidism
Thanks Bill. I just ordered the book and look forward to reading it.
hi there~
i think this article addressed my question but i just want to make sure this sounds consistent.
I’ve been on the Paleo diet for about 2 months now and i just got my labs back from my Dr. Expecting to hear good results, i was surprised to learn that my LDL’s had increased and i was showing signs of a fatty liver. In turn this freaked me out and now I’m all sorts of confused. I haven’t yet gone of a follow up but i just wanted to know if this is common? I have been fairly low carb, with the exception of some potatoes, sweet potatoes and the occasional dark chocolate . I’ve also lost around 16lbs and have been feeling better- no need to “graze” as often and more energy. My Vitamin D levels are very low too and i have been put on a 4 weeks of 50,000 units per week. Granted, we are just coming out of a long, cold winter in Utah so there is that o add to my “bad report”.
Not sure what to do other than maybe just increase some carb intake as the article suggests?
thanks for listening and hopefully putting my worries at ease!
alicia
Hi Alicia,
It is common. Probably about ~20% of very low-carb dieters develop high LDL, and if they are also choline deficient they will develop fatty liver.
So eat more carbs, about a pound per day of “safe starches” along with other vegetables; and eat more liver and eggs for choline.
Fixing the vitamin D deficiency will also help.
Don’t be alarmed, both the cholesterol and the fatty liver are easily fixed.
Best, Paul
Paul – what do you recommend for elevated APO B in terms of diet & supplements? My level is now 148, but my APO A is 160 and Lp(a) is 13, thanks to slow-release niacin and berberine. I heard sytrinol is good. But the APO B has increased consistently over the year. I have been eating LC paleo (LCHF)for the last year & have been taking T3 for 3 years (now @ 25mcg) to help with hypothyroid.
Hi Mark,
The keys are (a) sufficient carbs and (b) sufficient antioxidant minerals and vitamins to prevent LDL from turning into oxLDL inappropriately and (c) appropriate amounts of iodine and selenium to support thyroid health.
It sounds like you would probably benefit from more carbs, possibly from other nutrients depending on your diet.
I’m a 59 yr old male who has been Paleo for more than 2 years and for the most part have been doing fine. However, over the last few months, I started having a feeling like food was stuck in my throat and some tenderness near my Adam’s apple. Went in for a Dr’s visit and my Dr. ordered a Thyroid panel. (Results are below.) Saw an Endo and he wasn’t at all concerned about any of the results even though Antibodies were flagged as high.
I do know that on an older Blood test my T3 was at the bottom of the range, but on lat test came up some.
Since going Paleo, my TC has increased as has my LDL. On my most recent VAP test, TC was 256 (marked high); LDL was 187 (marked high); HDL 55; TG 52; apoB100-calc 127 (marked high); LDL-R (Real)-c 166 (marked high); LDL-P 2251 (high); and LDL-C 179 (high).
My Dr. who is very familiar with Paleo suggested Niacin (although it does upset my stomach). She had also put me on Pantethine. (Also had a Coronary calcium score done, which showed no problems). Also have been diagnosed with Silent Reflux (that is supposedly what my throat constriction/soreness was from). Anyway due for another Thyroid test next week.
One last note is that I had no real health problems before going Paleo and was not overweight. My diet is mostly grassfed meats, fish, veggies, eggs, some yogurt and I cook with butter, coconut oil, ghee and olive oil.
So any feedback would be appreciated.
Was VLC for most of my first 2 years on Paleo. Did start to increase my carbs about 3-4 months ago, but no noticeable difference in my general health (although did increase in weight a bit).
The report has TSH+Free T4; CBC with Differential/Platelet; Comp. Metabolic Panel; Thyroid Antibodies; Thyroxine; T3 Uptake; Triiodothyronine; and Sedimentation Rate-Westergren. .
Test 1: TSH+Free T4
TSH: 2.200 uIU/ml (range: .450-4.500) T4, Free (Direct): 1.38 ng/dL (range: .82-1.77)
Test 2: CBC (Too many items to list, but everything seems to be within range)
Test 3: Comp. Metabolic Panel (most things in range, but listed a couple that were high)
Glucose, Serum: 90 mg/dL (range: 65-99) BUN: 27 mg/dL (this was flagged as high. Range: 6-24) Creatine, Serum: 1.15 mg/dL (range:.76-1.27) BUN/Creatine Ratio: 23 (flagged as high. Range: 9-20) Calcium, Serum: 10.3 mg/dL (flagged as high. Range: 8.7-10.2)
Test 4: Thyroid Antibodies
Thyroid Peroxidase (TPO) Ab: 60 IU/mL (flagged as high. Range: 0-34) Antithyroglobulin Ab: <20 IU/ml (range: 0-40)
Test 5: Thyroxine (T4)
Thyroxine (T4): 9.3 ug/dL (range: 4.5-12.0)
Test 6: T3 Uptake
T3 Uptake: 30% (range: 24-39)
Test 7: Triiodothyronine (T3)
Triiodothyronine: 90 ng/dL (range: 71-180)
Test 8: Sedimentation Rate
Sedimentation Rate-Westergren 6mm/hr (range: 0-30)
PS Sorry for the long post
Hi Jeff,
Have you added or made changes to your intake of Iodine &/or Selenium (foods &/or supplements).
If so, it would be worth posting up that info as well, as it will add more info for Paul to comment on.
I have suspected in the past that increasing supplemental Iodine may have resulted in ‘changes’ to my throat/neck area. Though usually more like a swollen throat or sensitive neck.
Usually a bit sensitive to touch just below the adams apple, in the ‘V’ area above the sternum.
& I also wonder if changes to selenium intake may have similar repercussions.
…including any changes of the type or brand of iodine or selenium
No I have not taken any iodine or selenium supplements. I did start eating some liverwurst that I got from a grassfed meat place that I order grassfed meats from. Made up of beef and pork liver, plus spices and might have very small amount of dextrose. That and adding in some more carbs (sweet potatoes and white rice) and bananas were the other changes. Prior to that I did limit my carbs to what I would get from veggies. And the only fruit I ate previously were blueberries and strawberries. I do notice that bananas aggravate the constricted feeling in my throat so may wean myself off of them.
I did also consciously try to use a bit more table salt vs sea salt, figuring it would give me more iodine–had for the first year or two mostly used sea salt. But added it not as my only salt usage but just as an addition to sea salt use.
I also eat SeaSnax (seaweed snack).
Other regular foods in my diet are bacon (although much less than I used to eat), some pork products (roasts mostly but sometimes pork belly as well–all grassed); the fruit I mentioned above; chicken, fish including mussels, clams and shrimp. Towards the end of 2012 I did try to eat a bit more shellfish than in the past, but generally my diet didn’t change a whole lot since I was Paleo except for the increase in safe starches.
Hi Jeff,
The most common cause of high LDL on Paleo is being too low carb. You didn’t list any starches among the foods you eat; I would suggest making a point to eat about a pound of safe starches per day. Potatoes are a good choice. Cut down on the oils to keep calories from increasing.
After that, the key is being well nourished. Iodine, selenium, zinc, copper, magnesium are all important. Good amounts to supplement would be 225 mcg iodine per day, 200 mcg selenium per week, 50 mg zinc per week or 4 oysters per week, 100-200 mg magnesium per day, and 1/4 lb beef or lamb liver for copper and other nutrients. Also, egg yolks and duck/goose/chicken liver can supply extra choline, phospholipids, and nutrients.
With more carbs and better nutrition, the problem is likely to go away.
Best, Paul
Thanks Paul for the response. I have been eating more starches over the past few months, mostly sweet potatoes and white rice–not sure if a 1lb per day but definitely more than I had been. I’m not a big liver fan, but have tried to introduce some liver wurst into my diet (Grassfed). I eat eggs (mostly yolks) a few days per week. Would I need to use supplements to meet the other minerals goals you mention? Also what do you think about taking the niacin that one of my drs suggested. Also, could there be any influence from any of my thyroid numbers I posted?
Nobody on a Paleo or primal tyoe lo carb diet has to eat complex carbohydrates in the form of grains to get enough glucose. Everyone that is in this tyoe of diet should be getting plenty of glucose from very healthy fruits and veggies–grapefruit, blueberries, raspberries, kale, broccoli, cauliflower, mushrooms, celery, etc. If you are doing it right, if you are eating healthy, there is no reason why anyone on a lower carb Paleo/primal diet should be glucose deficient.
Great post. I have been on low carb for a few years now and recently added more saturated fat (eggs, meat, …).
in mg/l
Total CHL: 235
Tri: 81
HDL: 62
LDL: 190
Since going low carb I noticed that my Tri plummeted, HDL went up (I exercise more as well). However LDL seems to stay high unless I reduce Saturated Fat.
And why do you think that might be?
I would blame my genes! I have no real idea how to lower LDL via diet. Any idea Gregory?
I suggest you read the article and comments on this page. All the answers are here.
One thing I would say is that it is unlikely that your LDL is 190. Unless you had it tested directly, which I doubt, it is more likely around 150.
http://homepages.slingshot.co.nz/~geoff36/LDL_mg.htm
Thanks. I think the LDL was measured and not calculated (I spoke to my GP about it – he said it was measured otherwise the labs results would show “Calculated”).
Using your website I have a value of 145-155. And so I still think my measurement was 190.
I will read the post again for further information.
Greg,
I do apologize. I was using a wrong conversion formula to convert from mmo to mg.
So in mg this is what I have:
Total 235
Tri 81
HDL 54
LDL 166
LDL-P is likely elevated with these LDL, trig levels.
Here are some examples I’ve seen folks share. The agreed upon limit is LDL-P<1000.
TC 235 HDL 54 LDL-C 166 TG 81 TC/HDL 4.35 LDL-P ???? VincentB
TC 188 HDL 45 LDL-C 126 TG 87 TC/HDL 4.18 LDL-P 1641
TC 257 HDL 72 LDL-C 176 TG 46 TC/HDL 3.57 LDL-P 1437
TC 199 HDL 82 LDL-C 116 TG 61 TC/HDL 2.43 LDL-P 1147
TC 228 HDL 92 LDL-C 130 TG 34 TC/HDL 2.48 LDL-P 1012
TC 133 HDL 46 LDL-C 76 TG 56 TC/HDL 2.90 LDL-P 717
I find it interesting that so many people mimicking starvation with their nutritional ketosis seem to have elevated LDL-P numbers in the setting of low or low-normal thyroid function tests, low hs-CRP, and, almost uniformly, CT coronary calcium scores of zero. Rakesh Patel documents his LDL-P in the three thousands and REVERSAL of coronary plaque on his IMT. So, taking into consideration what we know of the “survival phenotype” associated with caloric restriction–and ketosis, at least in vivo as demonstrated by Hirschey, et. al in 2013, we expect the following:
(1) Inflammation to be low due to upregulation of cellular and mitochondrial antioxidants through the concerted effects of sirtuin-class proteins and their associates.
(2) Low or lowered levels of thyroid hormone.
(3) Absence of atherosclerosis, which can be inferred by the longevity associated with CR.
In light of these observations, perhaps the assumption that elevated LDL-P in the setting of VLC or KDs is detrimental to health is wrong.
In fact, one might hypothesize the oppposite, that it is beneficial. Perhaps the increase in LDL-P does actually reflect a “thrifty gene effect,” however not so much as Dr. Davis suggests in terms of improved energy shuttling in times of famine, but in terms of immune function. FH, for example, is thought to confer an immunologic benefit to individuals. Furthermore, it has repeatedly been shown that conserved sequences on apoB protein play an important role in innate immune function. I think it is entirely concievable that the elevated LDL-P’s in so-called “hyperresponders” might reflect and entirely normal range of expression in terms of individual polymorphisms reflective of increased immune “surveillance” in times of famine.
I think it is an interesting hypothesis that mechanistically makes sense–in times of famine, thyroid function goes down to conserve energy and LDLr expression (regulated by thyroid function) is decreased, leading to an increase LDL-P numbers and aid in the organism’s immunologic defense efforts. What does not make sense is how a diet that mimics at the molecular level the one thing known to extend life span in non-human primates and that also, in humans, improves all markers of health including radiologic studies of atherosclerosis would singularly increase the strongest marker for CAD against all the other benefits.
I haven’t quite had the time to comb PubMed to find literature to support or refute, other than to quickly find a few studies showing that cholesterol levels in CR’ed rats usually fall. Far more intersting would be to observe the LDL-P response to CR or a ketogenic diet in an animal model of FH…
“If your theory disagrees with Nature’s phenomena, if your theory disagrees with numerous A1 top quality experiments, replicated by others’ top quality experiments who achieved the same results – IT’S WRONG. It does not matter what your name is, how credentialed you are, how beautiful your theory is ….This is the key to science”
The above is the message and summary of what Richard Phillips Feynman stressed.
Whether you are a high carb person or a low carb person we need to have a bend over backwards HONESTY approaching this subject. Feynman stressed that !
I am sure this post has touched all the internet users,
its really really nice article on building up new blog.
Also visit my site … Anti Inflammatory Products