Since starting the blog, I’ve gotten a number of emails from cancer patients or their family members. When the Q&A page started last week, the second question was from Lindsay, asking for a cancer diet:
In the past 3 weeks my partner has been diagnosed with stage 3 breast cancer. She is 28 and there is no family history….
Do you have suggestions aside from vit d and green tea that might be therapeutic?…
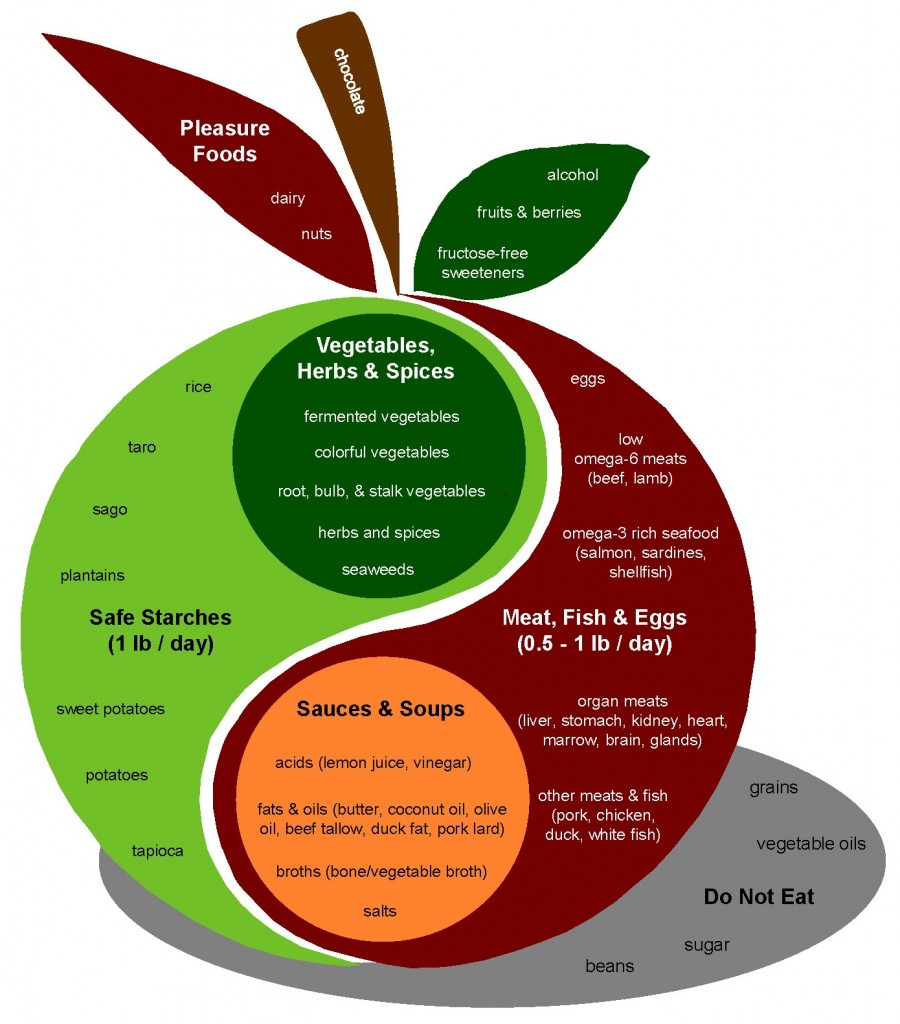
In my mind she simply needs to be extremely well nourished, but that is proving tricky due to nausea. I made a batch of chicken broth the other day and the smell alone sidelined her. Any thoughts on a way to sneak in dense nutrients without a strong odor?
I’ve delayed blogging about cancer and diet because of the complexity of the issue. Research has not yet determined the optimal diet for cancer patients, and there is reason to believe that the optimal diet may differ for different cancer patients. It is not easy to balance the many factors that should influence a cancer patient’s diet.
Today I’ll lay out my general perspective on cancer. The goal is to identify aspects of the disease that we can influence through diet. In subsequent posts, I’ll discuss foods, nutrients, and eating strategies. I hope the manner in which I’m addressing the issue will help cancer patients to understand the issues better and to design an effective personal eating strategy.
Cancer as a Progression of Diseases
Cancers often develop over long periods of time – typically decades. They usually cannot be detected or diagnosed at early stages. This is just as well, because most early cancers resolve spontaneously; they disappear or return to a normal state. Perhaps we should have a distinct name for these early and usually harmless cancers – “proto-cancers” perhaps.
Proto-cancers develop through a series of stages into life-threatening cancers. At each stage, the character of the disease changes. The purpose, and perhaps the nature, of dietary interventions may change with it.
Origins of Cancer
What characterizes these proto-cancers is that one or more cells develop an abnormal state of gene expression that I’ll call the cancer phenotype.
What causes a cell to develop the cancer phenotype? I believe the most common are:
- Infections, especially viral infections (since viruses are good at modifying gene expression).
- Toxins, especially DNA-modifying toxins such as those generated by peroxidation of polyunsaturated fats.
- Malnutrition, especially nutrient deficiencies that impair the ability to maintain epigenetic regulation of DNA.
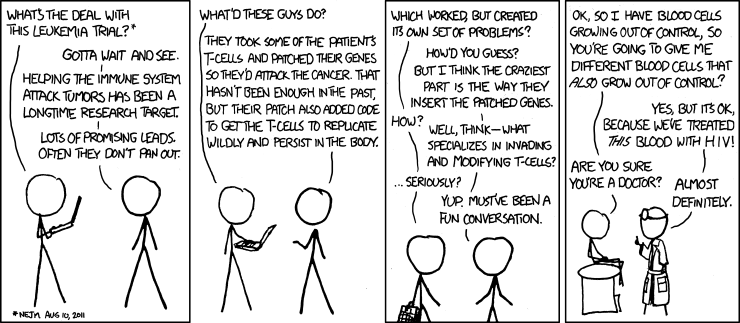
The Wikipedia page “Infectious Causes of Cancer” says that 18% of human cancers are known to have infectious causes, but I suspect the fraction will get much larger. Read through our story of XMRV and chronic fatigue syndrome (“Retroviruses and Chronic Fatigue Syndrome, Aug 24, 2010) for an example of how difficult it is to identify the viruses that cause cancers. In this instance, a new human retrovirus may (it is still disputed) have been discovered because men with genetic impairments to anti-viral immunity have much higher rates of prostate cancer, and scientists searched prostate tumors of men with this genetic impairment for viruses. If finding the cancer-causing virus is so difficult when we know it is present in the tested tissue, you can easily imagine how many other viruses may have escaped scientific notice.
Interventions to prevent the original causes of cancer are great for cancer prevention, but they may also be therapeutic. Removing cancer-causing viruses may enable the body to defeat a cancer it otherwise could not.
Proto-Cancers and the Evolution of Cancer Cells
The cancer phenotype has various characteristics, but at early stages important characteristics may include:
- Suppression of mitochondrial activity, especially apoptosis (programmed cell death).
- Metabolic changes toward metabolism of glucose and away from metabolism of fatty acids or ketones.
- Isolation of the cell from the rest of the body. Normal human cells closely coordinate their activities with the rest of the body, especially with neighboring cells, and respond to hormonal and other signals. Cancer cells tend to be more “individualistic,” less responsive to the body and to their neighbors.
Every once in a while one of these cells with a cancer phenotype will divide, creating two daughter cells. Perhaps in part because after metabolic impairment the cell has difficulty providing sufficient ATP to handle the complex motor tasks involved in cell division, these cancer cells often fail to divide properly, resulting in daughter cells with altered genetic state. Common changes include:
- Aneuploidy. Most genes have two copies, one inherited from the mother and one from the father. In cell division, genes are first duplicated, and then divided among two daughter cells, so that each cell gets two copies. In aneuploidy, chromosomes are improperly separated so that one cell gets three copies of a chromosomal strand, the other one. Genes on that strand then become expressed 1.5-fold in the cell with three copies, half-fold in the cell with one copy.
- Translocations. Chromosomes have a certain gene order. However, they can be re-assembled in an improper order, with one segment translocated to another place. This changes gene expression.
- Epigenetic modifications. DNA comes with a protein scaffold that packages and organizes it, and can be modified so that gene expression is silenced (via methylation) or enhanced (via acetylation). Epigenetic modifications are usually inherited by daughter cells – but dividing cancer cells may experience less stability in the epigenome.
These changes mean that cell division causes cells with a cancer phenotype to evolve. Let’s say aneuploidy occurs affecting a gene that stimulates cell division. One daughter cell gets 3 copies and becomes more likely to proliferate; the other cell gets only 1 copy and becomes less likely to proliferate. Of course, every time a cell divides it creates two daughters, so a decade later the first cell may have thousands of descendants while the first cell has few. A proliferative phenotype has become more common in the “tumor.”
The Middle Stages of Cancer Development
As a result of cellular evolution, the early cancer phenotype becomes a later cancer phenotype with new traits, such as:
- A tendency to proliferate. This is the trait people most commonly associate with cancer cells.
- A tendency to stay alive indefinitely. Some cancer cells become “immortal.” For instance, HeLa cells are immortal cells taken from the cervical cancer of Henrietta Lacks, who died in 1951. So resistant to death were these cells, they were the first human cells ever to survive in vitro.
Both traits are promoted by infections. Viruses and other germs want to stay alive, and to do that they need to keep their host cell alive, since cell death typically kills any germs in the cell (thus programmed cell death is a major part of human immune defense). Viruses also want to replicate, and to do that they often piggyback on human DNA replication. So viruses have evolved ways to promote proliferation and immortality of host cells. Cancers caused by viruses, therefore, often have a head start on acquiring these traits. Cancers that appear at young ages are probably almost always viral in origin.
Once these traits are acquired, the cancer cells proliferate and form a tiny tumor. These micro-tumors can reach a size of about 0.5 mm in diameter. At that point, growth stalls for lack of oxygen and nutrients. Cells inside the tumor cannot get enough resources to continue their growth.
Often this is the end of the cancer; it never develops beyond this point. It’s been estimated that most adults have thousands of these microtumors, and most never go on to develop clinical cancer. It is generally impossible to diagnose the presence of these microtumors.
However, cells in the microtumor are still evolving. Cells, when nutrients are available, divide, and one daughter cell survives to divide again while another cell in the tumor dies to make room. There is a “survival of the fittest” contest in which cells become more adapted to the environment of the tumor.
Progression to Diagnosable Disease
At some point, one or more cells may gain the ability to manipulate neighboring cells to their own benefit. This is a crucial stage in the development of cancer: when the cancer phenotype extends to give the tumor new abilities to exploit its human host. A key capability is:
- the ability to induce the formation of blood vessels. This process is called angiogenesis.
This process involves manipulation of the immune system, which is responsible for wound healing as well as defense against foreign bodies. Angiogenesis is part of the normal wound healing process, and when it becomes angiogenic, a tumor (in the famous phrase of Hal Dvorak) becomes a “wound that never heals.” That is, it acts like a wound to call forth the blood vessel generation process, but it never allows the wound healing process to terminate.
Once cancer cells can call forth new blood vessels from surrounding tissue, they have access to all the body’s nutrient and oxygen resources. There is no longer any limit to the tumor’s growth. This evolution of an angiogenic capability could be said to create the disease of cancer.
One of the interesting findings of recent research is that foods can significantly influence the likelihood that tumors will develop an angiogenic capability. A number of plant compounds from foods such as garlic, tomato, green tea, and turmeric have been shown to inhibit angiogenesis. If you read the excellent book Anti-Cancer by David Servan-Schreiber, you’ll find that these anti-angiogenic foods form the essence of his dietary advice.
Once tumors can induce angiogenesis, they can grow quite large. But even large single tumors are usually not deadly.
Progression to Deadly Disease
Cancers become deadly when another change evolves:
- Some cancer cells become metastatic.
Metastatic cells migrate away from the tumor, interact with non-cancer cells, and may travel through the blood to distant sites where they establish new tumors. When cancer metastasizes, many tumors can develop and the cancer can become a devastating drain on the host.
Immune Suppression and Co-Infections
Other new cancer capabilities may also evolve. For instance:
- Suppression of anti-cancer immunity.
When the immune system successfully attacks and destroys cancers, it is usually through an innate immune response involving natural killer cells and macrophages. Interestingly, this is also the same immune response which defends against fungal infections.
One of the interesting aspects of the evolution of cancer cells is that they often end up with many genes silenced, such that they lose many distinctively “human” genes and probably come to resemble our primitive evolutionary ancestors. In other words, cancer cells evolve to look more like fungal cells, so that a tumor may biologically resemble a mold colony.
Suppose cancer cells evolve a capability to suppress the NK cell and macrophage immune response. Then the tumor will flourish more readily – but so also will fungal infections.
It happens that late-stage cancer patients commonly develop systemic fungal infections.
It also works the other way: fungi that have evolved into obligate parasites of human hosts, like Candida, are good at suppressing human anti-fungal immunity. In doing so they also suppress human anti-cancer immunity. Thus, fungal infections are a risk factor for cancer. I saw a study recently in which a large fraction of people treated for systemic fungal infections were diagnosed with cancer in the following five years.
There is evidence that fungal infections of cancer cells increase the rate of metastasis. So the combination of cancer and fungal infections may be particularly deadly. This suggests that cancer patients might benefit from anti-fungal therapies.
There may be great variability in human immunity against cancer. Biologist Zheng Cui has found such variability in mice, and estimates that 10-15% of humans may be highly resistant to cancer. It is likely that diet can modulate this resistance, which suggests looking for dietary tactics that promote anti-cancer immunity.
Cachexia and Anorexia
Cachexia is the wasting syndrome that afflicts late-stage cancer patients. The tumors become a large drain on resources, their nutrient consumption is not met by diet, and the rest of the body is cannibalized in order to provide resources to the tumors. Muscle and other tissue wastes away until they can no longer sustain life.
Cachexia is often what kills cancer patients.
Now, if the cancer patient could eat sufficient food, even very large tumor burdens might be tolerable. Olympic swimmers eat 12,000 calories a day; pregnant women support 8 pound growths in their abdomen without risk.
Unfortunately, cancer also tends to diminish appetite. One of the consequences of cancer’s interactions with the immune system is that late-stage cancer generates a lot of inflammatory cytokines which can be imported into the brain where they affect the food regulatory systems that Stephan Guyenet has written about, causing anorexia.
Cancer-related anorexia makes food distasteful and causes cancer patients to cease eating. Lindsay mentioned her partner’s anorexia as one of the problems she hoped I could help her address.
Exercise and dietary strategies that promote muscle and tissue growth (“anabolic” strategies) such as those employed by bodybuilders and strength athletes might increase appetite, protect tissue, and delay the negative effects of cachexia. They might also have an anti-cancer effect by depriving the cancer of resources.
Interaction with Chemotherapies
Yet another complexity is that the standard therapies for cancer involve poisoning the body with chemotoxins.
This raises a conundrum. A healthy diet makes the body, and all its cells including cancer cells, more resilient to toxins. So a healthy diet may undermine the effectiveness of chemotherapies.
Some diet-chemotherapy interactions are well documented. Supplementation of vitamin C, glutathione, and omega-3 fats are all known to protect cancer cells against chemotherapies.
If beneficial foods reduce the effectiveness of chemotherapy, it might also be the case that toxic foods could increase their effectiveness. Thus, the optimal diet during chemotherapy might be quite different from the optimal diet when off chemotherapy.
I will not say much about these interactions, other than to advise that before undergoing chemotherapy cancer patients discuss their diet and supplement regimen with the oncologist.
Summary: Our Path to an Anti-Cancer Diet
So, we’ve identified a number of possible levers for attacking cancer. We can look for dietary steps to:
1) Defeat viral or other infections that originally caused the cancer.
2) Remove toxins and improve nutrition in order to promote DNA and epigenome stability.
3) Deprive cancer cells of their favored glycolytic metabolic pathways, slowing their growth.
4) Restore mitochondrial function, promoting apoptosis (programmed cell death) of cancer cells.
5) Inhibit angiogenesis.
6) Inhibit metastasis.
7) Promote anti-cancer and anti-fungal immunity.
8) Mitigate anorexia and cachexia.
Those who are trying to prevent cancer will want to focus on (1)-(5); those with early stage cancers on (1)-(7); those with late stage cancers on (1)-(8).
Our mission: understand how diet and nutrition can affect each of these; and then try to integrate various dietary tactics into an optimal anti-cancer strategy.
Conclusion
I think this gives us plenty to work on. Next week, I’ll provide short provisional answers. Over the next year, I’ll examine each type of cancer-diet interaction in detail and see if we can refine and improve our anti-cancer strategy.
































Recent Comments