Our May 2015 Perfect Health Retreat has just concluded. It was a rousing success: we had a great time, the program was better than ever, and we appear to have had excellent health outcomes.
But, thanks to a busy winter, I have barely begun to blog about the October 2014 retreat. I have many testimonials to share from October. One of them came from a celebrity guest: low-carb podcaster and author Jimmy Moore.
Why I invited Jimmy to the Retreat
Jimmy and I first met in person at the first PaleoFX (in 2011). There we had a long conversation about starches, and I encouraged him to try them. He seemed open to the idea and we agreed that he would do a “PHD” trial at some future time.
The years passed and we never did the trial, but at AHS 2014 we continued our conversation. Jimmy was more committed to a low-carb (now ketogenic) approach than ever, and I was more persuaded than ever (in part due to my friend Seth Roberts’ death; I’ll blog about that soon) that such a diet risked an early death from cardiovascular disease. I again encouraged Jimmy to try PHD and see if he felt better on it. Jimmy said that he didn’t feel he could give PHD a fair test on his own, because he didn’t fully understand it.
If you meet a man dying of thirst, you have an obligation to lead him to water; even if he has an irrational aversion to water, and you know he is unlikely to drink. Still, if you refuse to show him the water, you share the guilt for his suffering. If you show him the water and he refuses to drink, his suffering is his fault alone. In the same way, I felt an obligation to show Jimmy the way to a healthier diet, even if I knew it was unlikely he would drink from that pool. We weren’t quite sold out, so I invited Jimmy to do the PHD experiment for one week at our retreat. Jimmy and his wife Christine accepted the invitation.
Jimmy’s Praise of the Retreat
On the final day of the retreat, Jimmy generously recorded a video testimonial for us. After seeing the final edited video in January, Jimmy signed an authorization for us to use it. Here is the video:
For those who don’t like to watch videos, here are some quotes:
- “We had such a great time”
- “It was such an amazing time”
- “The camaraderie among the attendees was better than I have seen with any other group”
- “I enjoyed the food better than anything … It surprised me that it was not only tasty, delicious, and nourishing which I expected it all to be but I wasn’t quite as hungry as I thought I’d be eating more carbohydrates than I’m used to.”
- “This setting is absolutely spectacular.”
- “I’ve considered myself a pretty good exerciser … but you challenged me…. I learned quite a bit.”
- “I was very pleased [with the science classes]…. I really hope you pack this place out … The circadian rhythm stuff dude that is the best stuff you’ve done … that has helped my sleep and helped me get back on track with that more than anything.”
- “I actually was surprised [by how beneficial the health coaching was] … You provided information that no doctor ever has.”
- “This would shock a lot of people but I would absolutely recommend the retreat because I think if you’re interested in your health, you deserve to know all the evidence…. I think you owe it to yourself to give PHD a chance, learn about it, see if it works for you, and give it a go.”
- “Very glad I did it, and highly, highly recommend it for anyone else”
For those who are wondering, there was no quid pro quo between us. Jimmy had no obligation to give us a testimonial, and I’m grateful for his enthusiastic endorsement of the retreat.
Jimmy’s Recent Blog Post
Although they enjoyed their week at the retreat, it didn’t change their minds about their own diets. Jimmy and Christine told me when they left the retreat that it was clear PHD was bringing health benefits to many people, but they themselves, and many of their readers, were different and needed a lower-carb diet to be healthy.
Their conviction that eating moderate levels of carbs would harm their health came out in a blog post Jimmy published on May 2, the first day of our May 2015 retreat. “Paul Jaminet’s Perfect Health Retreat: The Good, The Bad, The Ugly” is a discussion of “my thoughts of the good, the bad, and the ugly about what this event was like for us.”
The important words here are “for us.” Those who only read headlines might obtain the impression that the retreat itself was “bad” or “ugly”; but in fact most of what Jimmy refers to as “bad” and “ugly” are statements about the biological reactions he and his wife had to eating carbs.
Although Jimmy may not have intended to denigrate the value the retreat brings to those who actually want to eat carbs, I feel that casual readers will interpret his post as a denigration of the retreat, so I’d like to correct the record. Also, I disagree with his interpretations of his experiences, and I think my commentary on the science may be helpful to many – even Jimmy, if he is open to it. So I’d like to respond in detail.
The “good” in his post repeated statements from his video testimonial above; so I’ll discuss only the “bad” and “ugly.”
The Bad #1 – Disorganized Schedule
This was his sole criticism of the retreat itself. Jimmy wrote:
There was a general schedule of waking up, attending a morning seminar, morning workout time, doing a kitchen class, eating lunch, afternoon free time, afternoon workout time, afternoon cooking class, evening meal, meditation class, and then sleep. But it would have been nice to have some semblance of a written schedule to at least know what we’re doing next…. This is easily resolved with a schedule.
We did in fact have a schedule, it was emailed to guests as part of a larger information packet in advance of the retreat and written on a whiteboard in our dining area. Jimmy himself took a picture of the whiteboard (from his Instagram):
In future retreats, the welcome kits that guests receive when they arrive will include a printed handout of the schedule, a map to help them find class locations, and a detailed description of the topic of each class, so that those who prefer to skip a class in favor of hot tub, pool, ocean, beach, or Internet browsing may know what they are missing.
For May this year, we revised the schedule, moving the start of science classes back from 9 am to 8:30 am and giving more time to movement and cooking classes. This helped prevent slippage of start and end times, something we experienced in October 2014.
It takes some experience to make everything move like clockwork. We’re getting there.
Overall, I think our organization deserves a great deal of credit. We delivered an ambitious program successfully. Our staff of 11 in October 2014, 13 in May 2015, was well coordinated. Many guests complimented us on what we had achieved. One October 2014 guest, CEO of a $100 million per year company who frequently stays in 5-star hotels, told us that he was very surprised by how well we had managed to deliver luxury hospitality rivaling the best he had experienced. (Credit where credit is due: We benefited from having David Spence, the principal of a luxury hospitality business, come as our guest to the May 2014 retreat and provide us with detailed advice on how to improve our hospitality. Susan Savery of Savery Services has been outstanding as our concierge.)
The Bad #2a – Christine was hungry
Jimmy writes:
[A]lthough we were told to eat at least two pounds of food per meal and as much as we wanted to satiety, Christine was constantly hungry throughout the retreat.
Although this experience is uncommon, it’s quite possible for this to occur.
A full plate of PHD food in PHD proportions weighs about 2 pounds and has about 900 calories. We serve two meals per day so “two pounds” per meal works out, including a glass of wine, to about 1900 calories per day. However, calorie needs vary based on body size, age, activity levels, and health considerations, so we don’t provide calorie or food weight guidance. Rather, our guidance is, “Eat as much as you want in the first days of the retreat. Then, as you get experience with intermittent fasting, calibrate your food intake during the feeding window so that you just begin to experience mild hunger at the end of the next day’s fast. ‘Mild hunger’ means that you notice it if your attention is unoccupied, but forget it if you give your attention to something else, such as exercise, an interesting conversation, or interesting work.”
For most guests, PHD food is highly satisfying from the first day of the retreat, and there is little to no hunger during the fast. For most others, there may be hunger during the fast for a few days, but by the end of the week, they feel satiated and begin eating less and having no hunger during the fast.
However, occasionally someone may remain hungry for a full week. Invariably this is someone who has been undereating either total calories or carbs before coming to the retreat. So far we have only seen this occur in women.
We had one such person in May, out of 27 guests. I would say that this phenomenon of week-long hunger affects no more than 3% of the people who come to our retreat.
Why does this happen? As we discuss in our book (Chapter 17), nutrient deficiencies drive appetite. A dearth of a key nutrient, such as carbohydrates, will drive appetite.
The exception to this is that, if a missing nutrient is chronically unavailable, hunger disappears. The brain does not want hunger to distract us from critical activity – the search for food. Thus, starvation itself is anorectic – it tamps down hunger.
However, once the starving person finds the food or nutrient she needs, the hunger returns, amplified. The brain acts as if the starving person, after a long trek through the desert, has found an oasis that may be only transiently available. Therefore, it makes the person ravenously hungry, to get her to eat as much as possible while food (or the missing nutrient) is available.
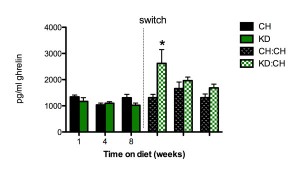
Ketogenic diets are generally carb-starved diets, and carbs are a critically important nutrient; so it is not surprising that ketogenic diets lead to exactly this pattern. Here is an animal study which measured hunger through serum levels of ghrelin, the “Hunger Hormone.” [1]
Rats were put on a ketogenic diet (KD) or chow diet (CH) for 8 weeks, then the ketogenic diet rats were switched to a chow diet. The ketogenic diet suppressed ghrelin a bit – consistent with tamped-down hunger – but when the ketogenic diet rats switched to a diet with carbs, ghrelin levels soared. At one week post-switch, ghrelin levels were more than double their levels on the ketogenic diet. Ghrelin levels dropped steadily with continued time on the chow diet, returning close to normal around 8 weeks post-switch.
What does this prove? It’s not that surprising that someone coming from a ketogenic diet might be hungry for the first week after adopting a higher-carb diet. It may take more than a week to improve carbohydrate status, reassure the brain that starvation is not imminent, and bring appetite back to normal.
Let me emphasize – such hunger is a rare occurrence at the retreat. People coming to the retreat from SAD diets are generally hunger-free throughout. People coming from low-carb or ketogenic diets typically see their hunger disappear in one to three days. In only two cases – Christine’s and one other – have we seen hunger persist for a full week.
The Bad #2b –Jimmy developed acne
Jimmy wrote:
I was surprisingly NOT hungry eating all of that (but I was pretty well fat-adapted and used to regular periods of extended intermittent fasting of 18-24 hours between meal on keto prior to the retreat). My issue was the sudden outbreak of acne all over my face that was not there before.
The video above was recorded at the end of the retreat, so you can clearly see the quality of Jimmy’s complexion. Judge for yourself whether acne is “all over [his] face.” I see one pimple on his face and one on his neck.
We have had 64 paying attendees at the retreat (15 in May 2014, 22 in October 2014, 27 in May 2015). As far as I know no one but Jimmy has developed pimples while at the retreat. I have a long history of severe acne and while it is far better than it was, I sometimes do develop pimples during the Boston winter. However, they quickly go away when I go to the retreat. So I don’t think the retreat is an acne-promoting environment – far from it.
On the rare occasions pimples do appear on PHD, they can usually be quickly cleared with some nutritional supplements and sunshine. Vitamin A, zinc, and pantothenic acid are typically the supplements most likely to eliminate pimples.
Why might Jimmy have gotten pimples at the retreat? My best guess is that it was a combination of (1) a depleted mucus layer in the gut caused by his carb-starved pre-retreat diet, (2) a sudden rise in his gut bacteria population at the retreat due to a suddenly increased carb and fiber intake, leading to (3) inflammation triggered by direct contact between gut bacteria and intestinal cells, coupled with (4) some nutrient deficiencies that made his skin sensitive to the inflammation.
I’ve blogged on how very low-carb diets can deplete the mucus layer of the gut (see “Dangers of Zero-Carb Diets, II: Mucus Deficiency and Gastrointestinal Cancers,” Nov 15, 2010). This happens because mucin-2, the primary constituent of mucus in the gut, is 80% carbohydrate, and when the body is carb-starved glucose is triaged for the benefit of the brain, starving other tissues like the gut.
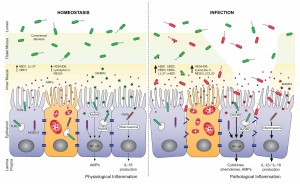
The mucosal layer of the gut generally shields the gut and immune cells lining the digestive tract from direct contact with bacteria. The bacteria they do see are beneficial probiotic mucin-degrading microbes like Akkermansia. A good mucus layer assures an absence of inflammation and a non-permeable gut barrier.
However, when the mucosal layer is depleted, the cells lining our gut are exposed to direct contact to gut bacteria that feed on food. This is inflammatory and also tends to lead to a leaky gut barrier and endotoxemia (entry of bacterial cell wall components into the body). Here’s a picture, from [2]:
My guess is that when Jimmy arrived at the retreat, he had a depleted mucosal layer of the gut, similar to the “INFECTION” side of the image above. However, on his very low carb diet, his gut bacterial population was low, so there wasn’t a lot of inflammation.
When he started eating carbs, his population of gut bacteria soared – bacteria can double their numbers in 20 minutes. It took a week or so to restore a normal mucosal layer. So he had a temporary period that was characterized by a relatively high level of inflammatory signaling coming from the gut.
As our guest Seppo Puusa wrote (“What Causes Acne? An Overview,” Feb 27, 2013), inflammation is the trigger for acne:
[M]ore than anything [acne] is an inflammatory problem. Many researchers now believe that inflammation in the skin is the trigger that kicks off the whole process. Studies have shown that inflammation is present in the very earliest stages of a pimple, even before P. Acnes bacteria colonizes the skin pore.
Antioxidant and immunomodulatory nutrients like vitamin A, zinc, and copper help to prevent pimple formation, while fat disposing nutrients like pantothenic acid help to prevent pore blockage. Jimmy was probably lacking in some of these nutrients, increasing the impact of the inflammation upon his complexion.
Of course this is just speculation, but the general picture is consistent with other aspects of Jimmy’s health. For example, his high LDL is suggestive of a leaky gut and endotoxemia, and recent lab tests indicate a number of nutrient deficiencies.
If I’m right, then Jimmy’s two pimples would have gone away in a little more time on PHD.
The Bad #3 – No info on ketogenic version of PHD
Jimmy wrote:
One thing I was especially looking forward to at the Perfect Health Retreat was learning more about the ketogenic version of Paul’s Perfect Health Diet. He has often noted that there are certain situations where ketones can play a therapeutic role in health–but there was nary a mention of ketosis at all in the hours upon hours of lectures…. [W]hy not share the information about how you recommend going keto for those who do need it?
When we did longer retreats – 30 days and 2 weeks – a discussion of ketogenic diets was part of the curriculum, but with a 1-week curriculum some content had to be dropped. We do health coaching pre-retreat, which allows us to identify any guests who would benefit from a ketogenic diet. So far no such person has come to the retreat. Since none of the guests would benefit from a ketogenic diet, there’s little reason to include it in the curriculum, when we have so much material of general interest.
(Interestingly, Paul would not allow me to give a guest lecture about ketosis as a bonus class for the attendees, but he did let me share a half-hour presentation on cholesterol based on my 2013 book Cholesterol Clarity).
With two days left in the retreat, Jimmy asked me if he could give a talk to the guests. I said sure; but it would have to be in the afternoon – the only free time in the schedule – and I wouldn’t be able to attend because that is when I do one-on-one health coaching. He said he could speak from either of his two books – Keto Clarity and Cholesterol Clarity – and asked which I would prefer. I said I would prefer he do the cholesterol talk, because many of our guests were not familiar with our differences of opinion, and might be confused to hear non-PHD diet recommendations being given with the apparent imprimatur of the retreat, and without me being present to clarify disagreements. Jimmy seemed fine with that at the time, delivered his cholesterol talk, and I heard it was well attended and well received.
I think it is misleading to summarize this conversation with the phrase “Paul would not allow me to lecture about ketosis.” Had I been able to be present and chime in to discuss points of difference, I would have been fine with Jimmy giving his ketogenic diet talk.
Jimmy also states that it is “unfortunate” anyone would think the ketogenic variant of PHD was as good as his no-starch, essentially carb-less diet. (Our ketogenic diet recommends including some starches to avert a deficiency of carbohydrate, fiber and medium-chain triglycerides as sources of ketogenic fatty acids, and a shift of protein toward ketogenic amino acids.) It’s no surprise that we differ on this point, since I think eating some carbs is desirable for everyone, while he thinks carbs are harmful in any dose.
The Ugly #1 – Jimmy Gained Weight
Jimmy wrote:
Many have wondered what would happen to my weight if I truly gave these “safe starches” a go in my diet. Like I said earlier, I told Paul we would do his plan as prescribed just to see what would happen. And the results on the scale were pretty shocking after eating this way for just one week–I gained a whopping 13 pounds!
Let me start my reply to this with a picture:
This picture was taken October 19, 2014, the day after Jimmy left the retreat. (Jimmy was at the retreat October 11-18.) You can see from the comments that Jimmy’s fans think he looks unusually good (“Woohoo! You’re killing it, Jimmy!” “lookin’ handsome Jimmy!! Great job!!” “Lookin’ spiffy!”).
Also note Jimmy’s last statement: he doesn’t know how his weight changed at the retreat. We keep no scales at the retreat, so it was impossible to measure his weight there; and his visit to the retreat was in the middle of a Keto Clarity book tour. He had a series of events in North Carolina following the retreat, and did not have an opportunity to measure his weight until his return home Tuesday, October 21. There must have been a minimum of 11 days between weight measurements, and possibly much longer. Any weight gain he could quantify did not occur in just one week.
If someone did gain 13 pounds in one week, I would expect his face to appear puffy. There is no sign of that in either this image or the video recorded the last day of the retreat.
I looked for a few other full-body images of Jimmy bracketing the retreat. Here is an image dated August 20, 2014 (pre-retreat) from an Asheville, NC Low-Carb meetup:
By eye, I would guess he was not lighter on August 20 than he was on October 19.
Soon after leaving the retreat, Jimmy undertook a long trip, first to San Francisco and then to Australia. Jet lag is a major circadian rhythm disruptor, and as I noted in my AHS talk on weight loss, circadian rhythm disruption is a major cause of obesity. So I wasn’t surprised that in photos from Australia, Jimmy looked heavier. Below is an image from a video of a talk Jimmy gave in Australia in November 2014 placed alongside the above image from October 19.
He looks significantly heavier in November. Immediately after the retreat, his suit jacket hangs straight down at the sides. In November, it bulges out sideways around the waistline.
I find it hard to reconcile this photographic evidence, plus my memory of what I saw in October, with Jimmy’s claim to have gained 13 pounds at the retreat.
Nor did Jimmy eat an inordinate amount of food while at the retreat. He went up for seconds at nearly every meal, but 1.5 to 2 plates per meal adds up to 3000-3500 calories per day, which should be roughly a weight maintenance intake for someone of Jimmy’s size (6’3”).
As my AHS talk on weight loss noted, we’ve had excellent results for weight loss at the retreats. Even in one week, we often see significant weight loss, even with ad libitum eating and wine consumption. For example, in May 2015, our two heaviest guests told me on departure that their pants had become loose and they were cinching their belts in one to two notches.
No guest at the retreats has gained significant weight. I think it would be difficult to do so, since we optimize so many of the weight loss factors.
I think Jimmy is mis-remembering when he gained his weight. He may have gained 13 pounds late last year, but it was probably during his cross-time-zone travels, not the week he spent at our retreat.
The Ugly #2 – Jimmy’s Blood Sugars Over 100
Jimmy wrote:
Measuring in a fasted state and then measuring postprandial at 30-minute intervals was not a pretty picture. I regularly saw spikes that jumped well above 140 after an hour which is a sign that your body is not tolerating the level of carbohydrates you just consumed. Of course, I was documenting all of this on social media and Paul decided to chime in about it with the following:
“I saw your blood glucose was 149 after lunch. That’s a normal reading, I actually thought it would be higher so I take that as a good sign. It takes a few days to a week to increase insulin sensitivity so it should be better by the end of the week, but even now it is in the normal range.”
I’m sorry, but 149 is NOT normal for me. My postprandial blood glucose readings typically NEVER go above 110-120 at the very most. Generally, the rise in blood sugar is about 20-25 points. But after every meal I consumed on the Perfect Health Retreat, the jump was more like 60-80 points. Not good at all. It took me a few weeks to get my blood sugar back down and under control again after the starchy meals ended. Promoting a starch-based diet to someone with significant insulin resistance is a recipe for disaster.
Jimmy was posting his blood glucose numbers on Instagram and so we have an enduring record.
Jimmy posted about two dozen blood glucose readings from his week at the retreat – I believe, nearly every reading he took – and only one was above 140 mg/dl. Jimmy has always been eager to show that he couldn’t tolerate starches, and if there were any other instances of a blood glucose reading above 140, Jimmy would have posted them to Instagram lickety-split. So I am confident that Jimmy is misremembering when he states, “I regularly saw spikes that jumped well above 140 after an hour.”
His postprandial glucose readings improved steadily throughout the retreat. I’ll just show his earliest and last reports, with links to Instagram:
- The first two postprandial glucose readings Jimmy posted from the retreat were 127 mg/dl one hour after lunch on Sunday October 12, and 149 mg/dl after lunch on Monday October 13.
- After lunch on Friday October 17, the last full day of the retreat, Jimmy’s 90 minute postprandial glucose was 87 mg/dl, and his 120 minute postprandial glucose was 100 mg/dl.
- After our farewell dinner on the evening of Friday October 17, Jimmy recorded his blood glucose every 15 minutes. They were:
- 15 minutes postprandial: 112 mg/dl
- 30 minutes postprandial: 126 mg/dl
- 45 minutes postprandial: 97 mg/dl
- 60 minutes postprandial: 116 mg/dl
- 75 minutes postprandial: 110 mg/dl
- 90 minutes postprandial: 125 mg/dl
- 135 minutes postprandial: 115 mg/dl
- 150 minutes postprandial: 111 mg/dl
- 180 minutes postprandial: 111 mg/dl
These numbers represent a dramatic improvement over the course of the week. Jimmy’s lowest reading on the first two days of the retreat was higher than his highest reading on the last day.
This improvement in insulin sensitivity was expected. Low-carb ketogenic diets are notorious for inducing insulin resistance, leading to high postprandial glucose when carbs are consumed.
This is one of the earliest reported side effects of a ketogenic diet. Recently Sarah Ballantyne and Denise Minger did a literature review on ketogenic diets and offered this image from a 1931 paper [3]:
The deeper the ketosis, the higher blood glucose rises after a carb rich meal. A mere 20 grams of carbs (versus about 125 g in Jimmy’s retreat meals) caused a nearly 30% rise in blood glucose.
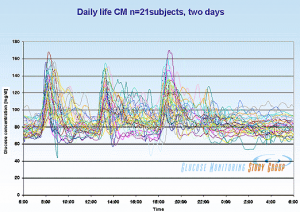
What is a “normal” postprandial glucose reading? Here is a view of postprandial blood glucose levels in healthy (HbA1c 5.4 or less) young people as measured by Professor JS Christiansen (from Ned Kock):
Although most postprandial glucose readings peak about 125 or so, a significant fraction of normal people experience postprandial readings of 149 or higher.
It is within that context that I told Jimmy that it was “normal” for him to have a postprandial reading in the range 127-149 on his first two days at the retreat (coming from a ketogenic diet), and normal to have postprandial readings in the range 97-126 after a week of carb consumption had improved insulin sensitivity.
At the retreat, I estimate that Jimmy was eating about 3000 calories per day, about 1/3 of them carbs; about 500 carb calories per meal and 1000 carb calories per day. It is gratifying to see that he is not diabetic, that a week of carb consumption restored his insulin sensitivity, and that he is fully capable of handling PHD levels of carbs.
More disturbing were Jimmy’s fasting glucose numbers. Jimmy posted these fasting glucose numbers: 130 mg/dl on Monday, 126 mg/dl on Wednesday, 133 mg/dl on Thursday, and 129 mg/dl on Friday. These are pathological numbers, and worse they showed no improvement during the week.
Jimmy’s fasting glucose numbers are lower on his ketogenic diet, but I do not find this pattern reassuring, for several reasons:
- Jimmy’s numbers are changing for the worse. In his recent “Potpourri of Health Tests,” he reported his history of medical lab tests of fasting glucose: 80 on February 28, 2013; 85 on August 22, 2013; 91 on October 17, 2013; 94 on April 3, 2015; 100 on May 15, 2015.
- Ketones substitute for blood glucose in feeding the brain, and it is the brain that controls blood glucose levels. So it is normal for blood glucose readings to be lower when in ketosis. However, what is important for health are total circulating energy levels (glucose + ketones + free fatty acids); elevated circulating energy poisons the pancreatic beta and alpha cells through “glucolipotoxicity.” [4] To be in ketosis, Jimmy has to have elevated levels of free fatty acids and ketones. So it is alarming that his fasting blood glucose levels while in ketosis are as high as 100 mg/dl.
Note that the loss of pancreatic alpha and beta cells, presumably due to poisoning by glucolipotoxicity, is an observed adverse effect of long-term ketogenic diets [e.g. 5, titled “Long-term ketogenic diet causes glucose intolerance and reduced β- and α-cell mass but no weight loss in mice”]. So possibly Jimmy’s elevated fasting levels of circulating energy substrates is a harbinger of the future development of diabetes.
UPDATE: Another explanation may be more likely. Apparently Jimmy was supplementing 50 mg melatonin. Melatonin is known to raise blood glucose levels in both evening and morning; just 5 mg of melatonin increased maximum night time plasma glucose by 27%. If this is the explanation, then Jimmy’s poor fasting glucose was a result of not following the Perfect Health Retreat program. We have specific supplementation recommendations and melatonin is not among them, except in rare cases where our RD may recommend a therapeutic supplement, in which case we recommend doses below 1 mg.
All this has come about due to Jimmy’s carb-phobia, but ironically Jimmy shows no metabolic signs of an intolerance of carbs. In a Facebook post on May 4, 2015, Jimmy prescribed a test for the healthfulness of “safe starches”:
Try eating a white potato to see how YOU do. Whether it’s truly safe for you will be determined by the impact it makes in your body, especially blood glucose. Measure at fasting (baseline), eat the potato, and then check at 30-minute intervals for at least two hours. At one hour, it should not go higher than 140. At two hours, you should be back close to your baseline. If either of these is awry, you might want to reevaluate your love for white potatoes.
By this test, by Friday at the retreat his “baseline” (fasting glucose) was 129, but eating about 500 calories of carbs in a PHD meal caused his blood glucose to drop postprandially to readings between 97 and 126 – all below his baseline. So white potatoes, if eaten as part of PHD meals, are “truly safe” for Jimmy by his own criterion.
The Ugly #3 – Dogmatic Approach
Jimmy wrote:
[O]ne of the ugliest parts of the Perfect Health Retreat to me was the completely dogmatic approach that it and it alone is the one and only true way to attain optimal health. There was no consideration given to any other means of getting there …
It is hard for me to fathom why it should be “ugly” for me to teach only advice I believe in, and not approaches that I don’t believe in, such as no-starch ketogenic diets.
I know of no health retreat that says, “We not only teach you the ways to achieve health that we believe in; we’ll also teach you the ways we don’t believe in.” I think guests would rightly respond, “Why should I spend time and money to hear you teach me things you believe are health-damaging? I’d rather you make a shorter, cheaper retreat and teach me only what you believe in.” I’m pretty sure Jimmy doesn’t teach the Ornish Diet on his Low Carb Cruises.
Our retreat makes a simple promise. It offers our best advice on how to be healthy. It covers every “ancestral” input to health — diet, nutrition, lifestyle, environment, movement / physical health — and some modern aspects, like understanding lab tests and managing doctors. There is neither time nor interest on my part (or the guests) for me to teach anything other than our best advice.
If someone wants to learn multiple approaches, they can come to our retreat to learn ours, and other events, like Jimmy’s Low Carb Cruise, to learn alternatives.
[Paul holds] staunch, dogmatic views on diet. While there is a lot of good in his plan, the abject close-mindedness to consider anything outside of what he has prescribed is truly unfortunate.
To borrow the Princess Bride line, I’m not sure “dogmatic” and “close-minded” mean what Jimmy thinks they mean.
First, I give evidence for all my recommendations – logical arguments and evidence for every assertion with citations to the literature. Guests at the retreat are given pdf copies of our slide decks, and each slide has its citations printed on it.
Second, I change my mind and update recommendations as I learn. When I first started Paleo I believed in a very low-carb approach, but when it led to health problems I changed my mind. Between the first edition of our book (2010) and the second (2012), a vast number of our recommendations changed — for example, the recommended macronutrient ratios changed from 20% carb 65% fat to 30% carb 55% fat, and nearly all the micronutrient recommendations were revised — based on research I’d done in the meantime, plus experiences of our readers. As an example of changing micronutrient suggestions, I toyed for several years with the possibility that high-dose iodine might be beneficial, before committing to a steady low dose (225 mcg per day) as a firm recommendation. The history of this blog is replete with explorations of issues to which I did not know the answer, and kept an open mind until sufficient evidence and experience gave a reliable answer.
If our dietary advice has recently been stable, it is because we have great confidence in it. We are hearing lots of success stories from people on PHD, essentially no negative outcomes, and new articles in the scientific literature continue to be supportive of our recommendations.
In contrast, I have not seen Jimmy change his mind about anything of substance, in spite of strong evidence which should have led to a reconsideration of his low-carb advice.
Recently, Tom Naughton changed his mind about starches (Safe Starches and The Perfect Health Diet, April 28, 2014):
I noticed more and more people saying they developed problems on a strict very-low-carb diet – low thyroid function, cold hands and feet, high fasting glucose, dry eyes, etc. – which went away when they added some “safe starches” back into their diets as prescribed in the Perfect Health Diet…. So I figured there had to be something to it…. Is the Perfect Health Diet truly the perfect diet? I don’t know, but I was persuaded to move my own diet more in that direction.
We’ve gotten thousands of reader reports of health improvements after switching to PHD from low-carb. Tom and every other prominent person in the ancestral community must have seen hundreds – Jimmy too. And every prominent ancestral leader (unless you count Loren Cordain as a leader) has responded to these experiences by endorsing starches and carbs to some degree. But Jimmy remains as anti-carb as ever.
As his low-carb ketogenic experiment winds on, Jimmy and Christine seem to be developing more of the “Zero Carb Dangers” that I blogged about in 2010-11. For example:
- Kidney stones. In April 2015, Jimmy revealed in a comment on Instagram that Christine was dealing with kidney stones. On November 23, 2010, I noted in “Dangers of Zero-Carb Diets, IV: Kidney Stones,” that low-carb ketogenic diets increase the risk of kidney stones 100-fold. (Ironically, Jimmy devoted a chapter of Keto Clarity to rebutting my critiques of “zero-carb diets,” and stated on page 199, “Kidney stones are the result of a high-carb diet, not a low-carb one.”)
- High LDL. On April 23, 2013, Jimmy revealed in a blog post that his LDL had ranged between 228 mg/dl and 332 mg/dl over the period 2008-2013. In a recent test dated May 15, 2015, Jimmy had an LDL of 194 mg/dl (still very high) despite an iron deficiency anemia (ferritin of 7, serum iron of 23) which is probably depressing his LDL by 30 to 60 mg/dl. I would say that an LDL over 160 is a reliable indicator that something is wrong, and a risk factor for cardiovascular disease. In 2011 I made a detailed investigation into why low-carb diets often lead to high LDL levels; see Low Carb Paleo, and LDL is Soaring – Help!” (Mar 2, 2011); Answer Day: What Causes High LDL on Low-Carb Paleo? (Mar 4, 2011); High LDL on Paleo Revisited: Low Carb & the Thyroid (Sep 1, 2011).
Experience shows that there is no amount of evidence that can persuade Jimmy that he is eating too few carbs. Is not his opposition to carb consumption dogmatic?
Summary of the Health Effects of the Retreat on Jimmy
Jimmy’s post suggests that I have overlooked another zero-carb danger: memory loss. After spending the last seven months on an almost carb-free ketogenic diet, Jimmy has forgotten:
- Most of the good aspects of the retreat.
- That his 2014 weight gain occurred after the retreat ended, not during it.
- That his acne at the retreat consisted of one facial pimple, not pimples “all over his face.”
- That his blood glucose went over 140 mg/dl once, not regularly.
- That a week at the retreat made him more insulin sensitive and made eating potatoes and rice “truly safe” for him by his own definition.
In truth, I think the retreat benefited Jimmy’s health. He probably left at his lowest weight, best insulin sensitivity, lowest blood pressure, and lowest LDL cholesterol of the last year. And he left in a joyful, generous mood. Thank you, Jimmy, for your video testimonial.
If his recent blog post about the retreat was less generous, well, I would take that as another indicator that his health has been worsening. Poor health can make one cranky and uncharitable.
More on Jimmy’s Situation
Earlier this week Jimmy posted a comprehensive set of medical labs (“Potpourri of Health Tests,” May 16, 2015). He had a host of abnormal numbers. Follow the link and look at all the red and yellow results.
In interpreting these test results, I think it should be recognized that the various individual issues – such as the iron deficiency anemia, the high anion gap metabolic acidosis, the “euthyroid sick syndrome” pattern of low T3 thyroid hormone (see my post “Carbohydrates and the Thyroid,” Aug 24, 2011), and the low cortisol with a disrupted circadian pattern – are probably reflections of deeper problems caused by malnutrition (starvation of carbs, protein, and assorted micronutrients) despite excess fat intake (a source of metabolic stress). Jimmy is posing metabolic stresses to his body that it is incapable of managing. As a result, his body is failing to perform basic functions like maintaining the circadian rhythm of cortisol or the normal pH (slightly alkaline) of blood.
I hope Jimmy will recognize that his labs (dyslipidemia, glucolipotoxicity, high anion gap metabolic acidosis) suggest that his low-carb ketogenic diet may be putting him at risk of cardiovascular disease, diabetes, and kidney disease.
I like Jimmy and consider him a friend, so I hope he recognizes that this post, and my earlier invitation to our retreat, have been friendly interventions intended to help him.
References
[1] Honors MA, Davenport BM, Kinzig KP. Effects of consuming a high carbohydrate diet after eight weeks of exposure to a ketogenic diet. Nutr Metab (Lond). 2009 Nov 19;6:46. http://pmid.us/19925676.
[2] Muniz LR, Knosp C, Yeretssian G. Intestinal antimicrobial peptides during homeostasis, infection, and disease. Front Immunol. 2012 Oct 9;3:310. http://pmid.us/23087688.
[3] Ellis RW. Some Effects of a Ketogenic Diet. Arch Dis Child. 1931 Oct;6(35):285-92. http://pmid.us/21031858/.
[4] Srinivasan VA, Raghavan VA, Parthasarathy S. Biochemical basis and clinical consequences of glucolipotoxicity: a primer. Heart Fail Clin. 2012 Oct;8(4):501-11. http://pmid.us/22999235.
[5] Ellenbroek JH, van Dijck L, Töns HA, Rabelink TJ, Carlotti F, Ballieux BE, de Koning EJ. Long-term ketogenic diet causes glucose intolerance and reduced β- and α-cell mass but no weight loss in mice. Am J Physiol Endocrinol Metab. 2014 Mar 1;306(5):E552-8. http://pmid.us/24398402.














Carbs caused me to gain weight, have acne, and experience emotional erraticism when I added them to a very low-carb, fat-based diet (I too used to pose biting into sticks of butter just like Jimmy and Dave Asprey). It confirmed my suspicion about carbs being the root of all evil.
But really, the right way to interpret all of this is that Jimmy’s diet and poor health resulting from it (I’m not saying Jimmy would be healthier on any other diet, I think the dude is screwed no matter what–propensity to have these problems can be traced mostly back to early developmental factors), causes him to experience a great deal of malaise eating a more or less normal diet (combining the three macronutrients).
It caused me to experience malaise when reverting back to mixing the macronutrients back together, so I can feel his pain. Recovering from years of highly-restricted eating regimens is a real bitch, and is very fattening.
Matt,
Can you give some examples of what you consider the prime early developmental factors that make weight maintenance problematic in adults?
I don’t have much time to hang out and comment, but most obesity researchers consider “genetics” to be anywhere from 50-80% responsible for one’s proneness to develop obesity. One example that have trouble overlooking is the fact that identical twins, even when separated at birth to live in different households, grow up to have very similar weights, body fat percentages, and even fat distribution as adults–much more similar to their identical twins than to their birth parents or even step siblings that grew up in the exact same household/environment.
Of course, most attempt to remedy the accumulation of fat with dietary restriction and/or increase in physical activity, and the effectiveness of that approach seems to be short-lived. After 6 months, few continue to lose weight. After 12 months, most are starting to regain weight, and by 24 months all lost weight is regained for the vast majority of people–even if they are still religiously following the same protocol that induced weight loss in the first 6 months of trying it out.
As far as evidence of the “genetic” differences between individuals, I think there’s some strong evidence that it isn’t purely genetic, but that it may be hereditary (in the sense that a nutritional deficiency could be passed from mother to child) or that it could be tied to the diet in the first couple of years of life.
Gerard Ailhaud’s research has shown some interesting things in rodents and humans–showing that the amount of omega 6 in proportion to omega 3 in the developmental diet influences probably the most significant factor of all (the number of fat cells), which goes on to be very predictive of future weight gain and body composition.
Guyenet and I have both written about this, but here’s a link to one of Ailhaud’s studies in particular.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2474903/
“I too used to pose biting into sticks of butter just like Jimmy and Dave Asprey” – but did you try deep fried butter?
https://www.youtube.com/watch?v=8o7E3ioJ9Ek
Thank you, Paul. Another generous post. I can feel your warmth from the writing. Good luck to Jimmy and Christine.
I think this is a sensitive and caring post, too.
Just as a point of information about my experience on PHD. I gained weight on PHD as I restored the nutrients I desperately needed and my body got used to the carbs I never ate during my 20s. I began the diet clinically deficient in b12, vitamin D, magnesium and iron with the high cholesterol that pointed to hypothyroid as a cause and a fungal rash and hives that cleared immediately with removing gluten and adding safe carbs.
I paid attention to how I felt (dramatically better) and to my labs (consistently much better) and now I am beginning to lose weight after about a year on the diet. I was a normal weight on low carb and still within the healthy range after the 15 pounds I gained on PHD and I was willing to live with being slightly bigger than I wanted for my own health. I knew I could not think about weight loss until my body had reached equilibrium.
I am now losing weight from a place of strength and satiety I have never experienced. I grew up with an anorexic mother and I worked in the fashion industry so believe me when I say that. I think in the US especially we are an instant gratification culture and repairing health is anything but instant gratification. I am so glad I am doing this in my 30s when I still have a great deal of resilience. I was making myself quite sick.
So, just wanted to add that the process of returning to equilibrium after adding the safe starches can feel like a long one but you will get there. Two years seems right to me.
Dr. Diane Schwarzbein also states that in order to lose weight you have to be healthy, not the other way around. She focuses on adrenal exhaustion plus insulin resistance/sensitivity. Her warning that you probably WILL gain some weight as you heal, before your body reaches equilibrium, is interesting.
I agree with her 100% on that.
That has definitely been my experience — I knew I would gain weight as I learned to really eat again and I did. One really just has to have the wherewithal to get through that stage and see it as healing.
I had no idea how little I was eating on a very low carb diet.
How very sad he felt the need to be so negative. However, he was in the middle of his own book tour. So. Your response took much time out of your busy schedule and it was very well done. Back to helping those of us in the majority who desperately need your help. And, thank you for your balanced, honest approach. You are trusted, respected and very needed.
For the record, “iron deficiency anemia” in an obese person is known as “hypoferremia of obesity.” The thing is that obese people likely have “anemia of chronic disease” which makes it so that not only does their body not absorb iron very well, but they are also withholding iron in their adipose tissue. This is done to keep excess iron out of the blood, away from pathogens and cancers and the hormone responsible for it is hepcidin.
In a review paper that was published last month (April 2015), researchers hypothesized how obesity may be related to iron overload, even if the patient appears to be anemic.
An inability to handle carbohydrates is also a sign of metabolic disfunction from iron overload.
Obesity and insulin resistance has been linked to an iron-enriched diet. Obese people have iron in the hypothalamus of their brains (possibly increasing their appetite), iron in their urine, in their adipose tissue, they do not absorb iron well and iron blood levels can be low. Researchers believe their bodies may very likely be using adipose intentionally to keep excess iron out of the blood so that pathogens and cancer cannot thrive (i.e. anemia of chronic disease). As those studies point out, adipocytes use hepcidin to regulate the iron status of the blood.
Jimmy may appear to be anemic, and probably isn’t absorbing much iron, but evidence suggests that his adipose tissue and hypothalamus have depositions of iron in them. Eating anything with Vitamin C in it would improve his absorption, but that would likely be counterproductive given the possibility of iron overload in anemia of chronic disease.
Jimmmy had iron excess in 2012 before embarking on his NK experiment.
“With my high iron levels I have to avoid red meat. So I’m abundantly aware of chicken which I consumed for half of the time in this experiment.”
http://livinlavidalowcarb.com/blog/jimmy-moores-n1-experiments-safe-starch-sweet-potato/13976
Jenny,
Those are some really good and interesting studies you linked to. However, I disagree with the entire idea of “hypoferremia of obesity.” Obese people tend to be iron loaded, plain and simple. Serum Iron is not a good marker for whole body iron stores. It can often fluctuate wildly during the day, especially in response to a meal (although I’m sure the measurements where taken fasting). Ferritin and Transferrin Saturation are superior, and ideally should be measured together.
As for poor absorption of iron, that is one of the body’s natural defenses to high iron stores, and also one of the defenses to a high iron diet. Popping vitamin C at meals to increase absorption isn’t a great idea if you have high ferritin. Lowering iron intake and blood donation would be better.
Also, when people hear “anemia,” they tend to think of iron deficiency, and while iron-deficiency anemia certainly does exist, many things can produce anemia, even in the face of high iron stores. Deficiencies of certain B Vitamins (like B6, B12 and Folate) are most common, and also most easily corrected, but it can also happen with more serious conditions, like sickle cell and thalassemia. Also, I didn’t see hemoglobin measured in the studies, which is what anemia is all about.
Still, I’m glad people are paying attention to the iron issue. Iron intakes are higher than ever (thanks to misguided fortification efforts), while things like a more sedentary lifestyle and eradication of hookworm have forced people to retain more iron. It’s especially problematic for men and post-menopausal women.
Jimmy needs him some spuds!
This was a very generous post on your part Paul. If you’ve listened to Jimmy’s podcasts over the years, you’d know that Jimmy has become more and more dogmatic about his persistence to sticking with a low carb diet despite his worsening health and weight gain. He always says on his podcast that he believes in doing what “works”. But if you look at his results, it isn’t working. I hope that he can benefit from this post before his health declines even more.
Paul, I got your back on this. Jimmy means well I guess, but a lot of what he said in his article is outright BS. Long-term ketosis is not good for everyone, it has harmed people like Dave Asprey and even Jimmy Moore permanently. Long-term ketosis should mainly be used medically as a diet, and there are few people who may be able to tolerate it genetically as a long term diet if done properly. Jimmy Moore’s health issues have gotten a lot worse over the years and I think a lot of it has to do with the same low carb dogma and the drastic links that he tries to go to be “healthy.” Not every diet is perfect for everyone, but I believe that the PHD is the best diet for most people (it might cause issues in people with SIBO,) and I both recommend and follow your diet. As someone I look to as a mentor I agree with you most of the time, and I believe truly that your heart is in the right place. Keep it up!
sheesh… I can’t believe anyone would bother to take Jimmy Moore seriously. The guy’s a pig. He knows he did better eating those carbs and doesn’t have the guts to admit it. Sorry, he’s got guts, just take a look at him. So what system would YOU prefer? Hint … the before and after shots should help you decide. Sheeple.
Good of you to try to help Jimmy and others, Paul. No good deed goes unpunished.
High anion gap metabolic acidosis numbers have also been reported for Gary Taubes http://garytaubes.com/2011/04/before-sugar-were-talking-about-cholesterol and an Atkins LCer http://www.medscape.com/viewarticle/788312 and a South Beach LCer http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2263061.
I hope that the functional medicine practitioner will be able to help Jimmy. I wish Jimmy good luck in health recovery.
Thank you so much for this post! I was a die-hard low-carber for six years, during which I gave birth to three children. I destroyed my thyroid and adrenal function by forcing my body to forego the starches it needed to grow and nourish children. It took anemia, adrenal fatigue, obesity, and hypothyroidism to show me that low-carbing was not the way. I’m finally losing weight and finding my way back to health, thanks to the Perfect Health diet, but it involved abandoning six years of preconceptions and assumptions to do so.
I feel sorry for Jimmy who I understand has gained a lot of weight back. I know what it feels like when your way of eating stops working for you, especially when you’re livelihood depends on it. I used to teach vegetarian cooking classes and was a vegetarian for 20 years. When I developed food allergies to every imaginable source of non-meat protein — dairy, eggs, soy, beans, nuts, etc. I had to face facts that my diet was no longer working for me. It forced me to change my diet AND my livelihood.
It will be very hard for Jimmy to change his ways. For him to call you dogmatic is beyond unreasonable. One thing that attracted me to the PHD diet is that it’s based on evidence and is never “done” but continues to evolve as new knowledge comes to light. This is the least dogmatic eating plan I can think of!
Deane, I would encourage you to join the PHD facebook group and post this message there. You have succinctly said what I believe, as well. I wondered at the outset how Jimmy’s participation in the retreat would turn out. He has numerous books that he surely hopes will continue to sell. To change his perspective so dramatically would surely be costly in a few ways. Would you mind if I added you to our group?
Hi lana, Yes, please add me to your group. 🙂
Hi Paul
I posted here way back when your blog was new about some problems I was having on low carb and you had me jog in the early a.m. and add back some carbohydrate. My T3 corrected and I am still running every morning and feeling wonderful
I am an RN and now in a Master’s program at Northwestern and I try to engage others in academic debates by emulating your gracious style.
You are really a role model of mine and I thank you.
The thing that jumps out at me in this post is the PHD acceptance of high blood sugars. The plot of ‘normal’ blood sugars you show are folks eating high carb diets. The beauty of a low carb diet is that if you don’t eat glucose, you maintain a normal blood sugar, 83 mg/dL, before, during and after a meal. Attached is MY blood glucose for a day. I don’t spike my glucose because I don’t eat glucose. I have a healthy a1c: in the mid 4s. It is A1c that is the fundamental determined of health. If I eat potato glucose, I’m going to raise my blood sugar and them you get the myriad negative health impacts of glycation. https://docs.google.com/file/d/0B7nTJuQ6HdueQk91a0dXRGhrbHc/edit?usp=docslist_api
@RD
On my blog with about 100,000 total comments at this point, many thousands are from LC and VLCers over the year who report:
1. Elevated fasting BG. This is physiological insulin resistance and is well established.
2. Whenever they do eat carbs (rice, potatoes, bread, etc.) they experience huge spikes, sometimes up to 180-200.
Here’s the problem, many people who experience this use it to confirm an unwarranted bias that they can’t handle carbohydrate. It’s very much like a couch potato finding the elevator in his building out of service, has to climb 6 flights of stairs, his heart races to 250bpm and he confirms his bias that he can’t tolerate any exercise.
Carbohydrate is a natural, ESSENTIAL part of a human omnivore diet and if you reply with the old saw that “there’s no such thing as an essential carbohydrate,” then explain why a human infant’s exclusive food is 40% carbohydrate.
The ability to exist without it is a survival adaptation (gluconeogenesis) in order to spare glucose for the brain. BTW, since no essential carb, please explain why brains run on glucose primarily with an absolute low-end requirement of about 130g per day.
In fact, both I, my wife, and my dad experienced that same thing. I went years without ever measuring fasting BG under 100. And, I had post meal spikes if I “indulged” in significant carbs of 180. Now, my fasting is 85ish and I never spike over 130ish, even with a big plate of mashed potatoes or rice. And the way I re-developped a health metabolism instead of touting a broke-dick metabolism like you’re doing (out of ignorance) is that I added back significant starch to my diet and ignored my glucose meter for a month as I EXERCISED my metabolic pathways back to that of a health human.
…And that was also about 15 lbs ago and counting.
Tons of my former LC and VLC commenters have experienced similar results once they realized they were being cleverly manipulated through obsessive BG testing that they had a metabolic problem and had to be a lifelong LC dieter and supporter.
When babies are nursing aren’t they in ketosis?
No, breast milk contains lactose and GOS’s, and a good amount of them at that. There is more by percentage carbs in breast milk then fat. Babies are not in ketosis, except possibly after birth and while they are getting colostrum. http://www.ncbi.nlm.nih.gov/pubmed/392766
Colostrum is mainly water, protein, and GOS’s with a little lactose and fat thrown in and differs from mature milk. Either way babies are not in ketosis for very long after birth, if they even are at all.
They can go into ketosis between feedings, especially longer intervals overnight…which is why the CPT1a mutation in Inuit is most dangerous for Infants and care must be taken to feed in short intervals, because they can’t produce ketones at sustainable levels.
RN is right. I had no problems with blood sugar until after some years eating VLC/LCHF. Gradually my FBG rose from the low 80’s to the upper 90’s and low 100’s and continued to rise and my postprandial spikes from occasional carby meals worsened and it took less and less carbs to cause bigger and bigger spikes.
RD, Your verbiage sounds like that of Dr. Richard K. Bernstein. I was unfortunately influenced by him (and other VLC advocates) and recommended his book to a relative and am grateful that they didn’t follow his advice 100%. I do give him and Dr. William Davis credit for influencing me to obtain a glucometer, which eventually helped me recognize that VLC was having bad effects, though it initially caused a new problem in the way that Richard described (in guiding me to continue eating too few carby foods for too long, which made matters worse).
Instead of giving up on my metabolism and consigning myself to coddling my system with endless carb avoidance, and thereby further weakening it in the long run, I found ways to improve my insulin sensitivity, carb metabolism and thus metabolic flexibility. In the process, I experienced other unexpected health benefits, such as resolution of cold extremities and excruciatingly painful tetany that I didn’t know was connected to VLC diets via low serum CO2 (not just low electrolytes), which both Jimmy Moore and Gary Taubes have reported. I did not see warnings in the LC community about low serum CO2. Jimmy and Gary seem unaware of the issue.
Excellent, Ex-VLCer.
So gratified you shared your story because from where I sit it’s literally a “broken record” with so many folks, and not only have I seen it first hand, but in close family members.
I’m even more glad that you eventually recognized that the solution was not in ever more carb restriction, but in adding in more, exercising your metabolic pathways and returning them to the strength that is the birthright of every human—to be able to consume, enjoy, and find Perfect Health with carbohydrates from real food as an important contribution to an overall real food diet.
Bravo!
Thanks Richard.
An additional explanatory note: by “low” serum CO2 for Jimmy and Gary I meant suboptimal. Christopher Kelly listed the “optimal range” for serum CO2 as 25-30 mmol/l, which Jimmy just barely reached with 25. Gary reported 19 in 2011 (http://garytaubes.com/2011/04/before-sugar-were-talking-about-cholesterol). Jimmy unfortunately has multiple worse health markers.
your analysis is very reasonable!
you think Jimmy has hypothyroid. his diet sounds pretty boring to me.
he called you dogmatic? 🙄
perhaps next time when i’d accrued enough vacation to join your retreat.
regards
pam
Hello Paul Jaminet,
Why oh why invite this delusional individual to your retreat ?? JM deserves NO attention whatsoever. It boggles the mind to see him parading as an “expert” (sic) in nutrition when a simple look at his idiotic diet and health evolution over the years reveals how phony his “livin-la-vida-low-carb” actually is and what an attention whore he is. He strongly appears as a kind of dangerous religious zealot who ignores science and hard evidence. What a pure waste of time, and the noise he tends to create (whether directly or via well meaning people like you) is potentially harmful.
I am amazed! wow! You’d better call a spade a spade and trash this dude and his books for what they are once and for all.
“So it is normal for blood glucose readings to be lower when in ketosis”
I was surprised to read this. You’ve regularly claimed on this blog that fasting blood glucose is HIGHER on ketogenic diets. A FBG of 100 on ketosis isn’t alarming – it’s quite normal, whether you believe it’s healthy or not.
In support of my previous post, here’s a quote from your blog post “Safe starches symposium: Dr Ron Rosedale” of Nov 1st 2010:
“In general, very low-carb diets tend to raise fasting blood glucose and 2-hr glucose levels in response to an oral glucose tolerance test.
This is a well-known phenomenon in the low-carb community. When I ate a very low-carb diet, my fasting blood glucose was typically 104 mg/dl. Peter Dobromylskyj of Hyperlipid has reported the same effect: his fasting blood glucose is over 100 mg/dl.”
So why do you argue the opposite in this blog post?
Hi Harry,
There’s no contradiction in any of my statements:
– Lowering carbs without ketosis raises fasting glucose, but
– Ketones lower glucose.
Here I am making the point that ketosis lowers his glucose, and he has some pathology raising his fasting glucose. Exactly what it is requires medical investigation.
OK, the distinction between low carb and ketosis. Glad I was proved wrong as it seemed such a glaring contradiction. However, I thought Peter D was always in ketosis and he has high FBG.
With regard to Jimmy – if only he could be persuaded to try the PHD for a couple of months instead of 1 week…
“When I say I avoid ketosis because Kwasniewski says avoid ketosis, that’s religion. … I’ve always stayed just on the edge of ketosis.” – Peter D., http://high-fat-nutrition.blogspot.com/2009/11/brief-discussion-of-ketosis.html
What a slimeball. Mr. LLVC preacher extraordinaire dare calls someone else, “dogmatic?” Jimmy Moore’s essence of being is the very definition of dogma. How amusingly hypocritical. Such a shame Paul. He has zero honor.
Please, folks – don’t call names or make ad hominem attacks on Jimmy. He faces an extraordinarily difficult problem: to accept carbs, he not only has to give up long-held beliefs, but he also may lose his livelihood, and the persona of “lowcarbman” that has become his personal identity. This must be like being on Calvary for him, a sort of death. Now I think he’s a talented guy and would do well after being “born again,” but it probably doesn’t look that way from where he stands. In order to make that leap you need faith and a willingness to die for truth. Not many could do it. I hope Jimmy can.
Have some sympathy for the man, and be courteous.
Thank you, Paul, for saying this. What Jimmy Moore has done is actually a good thing. Every experiment he did on himself furthered our knowledge of how nutrients affect us. Without him, and his outgoing attitude, the others who disagree with him might not have been noticed (you, as well as others). In addition, he did a lot of great podcasts and interviews. Not everyone he interviewed he agreed with, either. I wish him love and luck. Personally, I’m still trying to figure it all out for myself.
I agree with that too. Jimmy’s done a lot of good. I wish he would be willing to be “lowcarbman” at a higher level of carbs. I make a point of criticizing “very low carb” rather than “low carb” because I think a little re-definition would make it so much easier for people like Jimmy to improve their diets.
Once again you show yourself to be the most gracious and kind person around, Paul. I just had to let you know that, as it is extraordinary.
And, on topic, that was a great and thorough discussion and explanation of the criticism you received. If only we all could handle such a thing so well.
The world would be so much better off if more people responded to criticism with such graciousness and generosity. I know that I wouldn’t have responded this way, but I hope to remember Paul’s example if I’m faced with a similar situation in the future.
I thoroughly appreciate that Jimmy Moore has brought so many interesting and helpful guests on his blog through the years, but debating him on science is like me (who flunked chemistry in high school) debating Stephen Hawking e.g. why bother.
It had to be done, Paul, and you did it honestly, kindly, and thoroughly, as usual.
What a thoughtful, enlightening post. I wish Jimmy Moore well and hope he’ll give the PHD another, longer try and head off his budding metabolic problems before he has to suffer too much more.
It feels like the community knows Jimmy is headed for a major health disaster, and everybody wants to get something down in writing to say that they tried while he was still alive.
So far, Paul’s done it with the most class. But will it be enough to save his dear friend?
Props to you, in a hostile, hated filled attack web world, you concern is heartfelt.
Looking at those lab results he needs help. Those look like precursors of some very bad things to come.
I think that a 13 lb weight gain would not be surprising in a man of that size. Switching from a very low carb diet to a diet with carbs would cause glycogen and water to be stored in muscle as a one time, overnight “weight gain”. It’s a gain, but in a good kind of way.
It’s probably not a good idea to model much of anything on how it affects Jimmy. He’s a good guy with a big heart, but it seems clear he has a uniquely damaged metabolism. The damage may or may not be reversible at this point, but he is very much an N=1 experiment with little application to the experience of others. And even if it were reducible by adding more carbs, as Paul says, that would require changes to pretty much his entire life. Not an easy leap of faith. But if he did give it a chance, and saw positive changes, the benefits to the entire community would be immense.
“require changes to pretty much his entire life” – you said it right there. How long was the n=1 keto experiment, 8-9 months? Why not try something else for 8-9 months instead of 1 week.
Hi Paul,
thanks for this blog post. For the last six years I’ve been eating 50-100grams of carbohydrate a day. I go to the gym four days a week am generally healthy and a good weight. About five years ago I developed a problem of waking up at 4am every night feeling ravenously hungry, it is quite distressing as I usually can’t get back to sleep, and often feel quite sleep deprived. No answers from doctors. Definitely a link with carb consumption, as increasing the amount I eat makes the problem worse (multiple wake ups rather than one). Maybe I just need to gradually increase my carb intake and stick with it for more than a week? Any thoughts you might have would be appreciated.
Hi David,
Yes, I’d try eating more carbs longer (look at the plot of ghrelin in rats coming off the ketogenic diet — it probably takes as long to fix sleep as it does to fix hunger). Also, tend to electrolytes — you may have developed adrenal insufficiency and be waking due to lack of electrolytes. Cherry tomatoes and a bit of salt and water before bed and upon waking may help a lot.
thanks kindly for your answer Paul, much appreciated.
david for what its worth i had same problem which is slowly getting better.I have concentrated montmorency cherry juice with water and it helps,along with stopping alcohol 🙁
marcus
thank-you Marcus for your ideas.
Paul,
Thanks for the informative post. I looked at that link to Jimmy’s health tests. He posted his meal diary for 3 days – Quest protein chips for dinner every night (with cheese, cream, raw cacao powder and stevia).
Jimmy said: “I regularly saw spikes that jumped well above 140 after an hour which is a sign that your body is not tolerating the level of carbohydrates you just consumed.”
Paul said: “Jimmy posted about two dozen blood glucose readings from his week at the retreat – I believe, nearly every reading he took – and only one was above 140 mg/dl.”
Why is P Jaminet saying Jimmy Moore only had one reading over 140?
When I tried the Perfect Health Diet for 3 days, I regularly saw spikes to the 150s.
question 1: which single nucleotide polymorphism (SNP) within the TCF7L2 gene, is, to date, the most significant genetic marker[3] associated with Type 2 diabetes mellitus (T2DM) risk?
question 2: what is the prevalence of this SNP in the general population?
question 3: so people possessing one of both of the T risk alleles in this SNP usually insulin sensitive or insulin resistant?
question 4: is this snp associated with a insufficient production of insulin?
Paul:
v has commented on my blog since 2008 or 9. There is literally nothing you can say that will change an electron signal in a single brain cell.
So just ignore.
My advice.
Paul-
You and your team are class acts. And smart as hell. It was an honor having y’all on the podcast, come back anytime.
Thanks Robb, I had a great time on your show, I’d love to do it again.
Paul,
Very nice comments. I haven’t been on your blog for a while, but it seems that you never tire of using sound logic, reasoning, and evidence to support your conclusions.
I’ve been doing a variation of PHD for about 4 years now, and haven’t looked back.
I hope others in the AH community will eventually come around and endorse your ratio of starches/carbs.
hello paul change of subject
have you a view on stephan guyenets website discussing
the PCSK9 inhibitor trials strengthening case that LDL can cause heart disease
subject is beyond my intelligence
thanks marcus
Hi Marcus,
There’s no doubt high LDL promotes risk of heart attacks, strokes, and other cardiovascular events. We know the mechanisms and the evidence is very strong.
But, low LDL increases mortality from cardiovascular events, infections, and cancer. So you want an optimum LDL, it’s not the case that “lower is better.”
thankyou paul very kind
It doesn’t take rocket science to understand who is of the better understanding here. An astrophysicist or a gentlemen who simply assumes things as he tries new endeavors. I respect a lot of things Jimmy has done over the years for the Nutrition industry, but the bottom line is Paul is a scientist and a researcher and has a greater understanding of the science behind why the body responds the way it does. This blog post was highly informative, yet anyone who has read Paul’s book, and has seen all the countless hours of research he puts into everything he writes will clearly be on the side of research and science rather than a biased view of someone who has clearly not stepped aside from a mis-understood view about carbohydrates.
Wow. Selective “memory loss” indeed! I imagine you might’ve been blind-sided by Jimmy’s post, Paul. Good on you for responding with the thoughtful, respectful class I’ve come to know you for.
I do wish JM well, and hope he makes it safely out of his dietary Mobius loop. Beliefs are powerful!
(I also hope Mr. Moore has done the honorable thing, and offered to pay for his and Christine’s stay!)
Best regards,
KM
This would be relevant if JM was actually following a Keto diet. It’s obvious he cheats like crazy.
How is that obvious?
” A dearth of a key nutrient, such as carbohydrates, will drive appetite.”
This is false. There is no such thing as an essential carbohydrate.
People like you post this garbage because you don’t want to part with your precious potatoes and pasta.
Brilliant observation, Colin. Paul has written an entire book discouraging wheat consumption, and your explanation for why he finds carbs essential is that he doesn’t want to give up pasta? Yeah, ok.
Keep swallowing down all that zero-carb b.s. When you find yourself stubbornly overweight, approaching prediabetic FBG, and squeezing out kidney stones, you can assure yourself it’s all due to metabolic damage that occurred over a decade ago.
Colin, you do realize that you sound just like a vegan when you say that, don’t you?
Self-awareness, it’s tough, but it’s a good thing.
Oops, hit the wrong reply button. Sorry Bret, meant for Colin, of course.
Interesting. When I first starting questioning the SAD diet myself and my family were eating back 2008’ish his was one of the websites I frequented until his website was compromised and was never the same. Regardless, I wish him well. Since then I’ve read many of this big names in this new way of eating, including both version of your book and I keep coming back here. Classy rebuttal and well done.
Jimmy was a member on my Facebook group until recently. He has left because he was asked why he thinks his diet isn’t working for him. He is in denial due to the fact that he now cannot do a u-turn and admit that too much fat causes these problems. When you are so entrenched in the LCHF world money talks…
I’m sure excess fat is causing problems, but also the lack of carbs. I think of it like a muscle that goes months without exercise. When someone is bedridden for months, he can’t walk for some time after. It should be no surprise that after months of VLC/ZC ketosis-induced atrophy, our carb metabolism is dysfunctional and our blood sugar skyrockets on a glucose test, as Richard wrote about here (see second graph).
Jimmy clearly does not see things this way. For him, a carb-phobic ketogenic diet seems to be the end-all, be-all. Oh well. Good luck, Jimmy.
To be fair, Jimmy isn’t the only person who believes carbs are inherently harmful for everyone and ketosis is the most beneficial metabolic state to be in. There are many out there who believe this, and there are continual anecdotal reports of dramatically improved health as a result of ketosis-based dieting.
And heck, I start doing ketosis in the 70s, and over the past few decades it has helped me keep my weight under control. So it’s not like he’s some whack job shouting on a street corner with no evidence. As a short-term approach, I think it still has merit. It’s only long-term that the negative effects start to show up in many (if not most).
And if you’ve ever been really fat (and sick and tired, etc.) the fear of being that way again, and being out of control of your metabolism, is strong, really strong. And being in ketosis gives you a sense of control. So Jimmy’s in a tough position right now, and I don’t claim to know what’s best for him. PHD has a better chance than most approaches to help people in conditions similar to his, but maybe not. I just wish him the best…
So many are weighing in with what they think of JM’s test results — what, if anything, is he saying? Is he alarmed, as well?
Charles wrote: “It’s only long-term that the negative effects start to show up in many (if not most).”
That’s basically my point (though I would say “mainly,” rather than “only”–plenty of people also report minor short-term issues like “ketosis/LC flu”), and I think that Paul, Richard and most other people who warn about potential risks of keto are also mainly warning about the longer-term risks of doing keto or VLC chronically that we experienced and that Jimmy appears to be experiencing.
Also, the claim that “carbs are inherently harmful for everyone and ketosis is the most beneficial metabolic state to be in” goes way beyond saying that keto can have some merit short-term. I’m not convinced that either is true for most people.
Jimmy is in trouble. Jack Kruse explains that Jimmy is sick on a quantum level, because that is his thing.
I believe every living being suffers and becomes ill because of fallacies and contradictions, and ultimately it is only logic that kills everything that is alive.
Confusion will be my epitaph…
But we all fool ourselves. There is a serious mismatch between cognition and experience. Physiology is far more complicated that physics, chemistry, biology, economics, mathematics, paleontology, theology and psychology.
I think it is time for everyone in the field of trying to find the correct science of nutrition and health to re-read Thomas Kühn’s “The Structure of Scientific Revolutions”, visualizing when you read it that the mainstream, official theory is your particular theory. That is, imagine that you are the Emperor, rather than a random Guerrilla Leader.
In the case of Jimmy Moore, I would ask: does he take supplements regularly? What supplements, and in what quantity? CoQ10, Mg, Zn?
Does he have an underlying infection?
Does he receive electrical muscle stimulation?
When he went to the retreat, he changed biomes, which implies other level of radiation, different enviromental bacteria and fungi, different subconscious mind stress. Does these things actually
Does he practice earthing regularly and did not on the retreat, or vice versa? What about the water composition? Does he drink normally only distilled water, or does he drink normally this solution of salts in water that we call “water”?
A conjecture. There is this theory that gaining weight, when asociated with an increment of fatty tissue, occurs because adipocytes can’t receive the signal to stop accumulating fat, either by not being able to produce leptin, or by not being able to reject the influence of insulin. What if individuals who gain weight by means of fat easily, actually have an excess of adipocytes, which their physiology cannot eliminate, and these cells are constantly demanding fatty acids, independently of having hormones well under control.
I’m talking of numbers versus procedural dysfunction. It does not matter how good technically is your army, when your enemy outnumbers you 1000 fold. The illness might be caused by a deformation, rather than a insufficiency or an excess of some chemical.
The brain is in control, but what if that which is controlled cannot be actually controlled, no matter how much the brain tries?
I like you all. But I would love to see Jimmy better, and Kruse less freaky, and Jaminet less mesianic, and Rosedale less dogmatic, and Noakes less commie… and I could go on.
Let’s try some “functional medicine”, and see what those guys have. Let’s leave, for a while, this trying to find a perfect health theory that explains everything. Let’s get to the specifics. A real doctor is needed here, not a pure theorist, not a researcher, not a half doctor, half scientist. To overcome this problems, we need the exhaustive and imaginative work of a real artist, and there are very few, sadly.
A real artist is one who does not believe any theory, yet makes thing right.
Sorry for writing too much.
“What if individuals who gain weight by means of fat easily, actually have an excess of adipocytes” – but what does it mean to have excess adpipocytes? If it means just having 20% body fat, no 6-pack, no chance to win sport competitions etc. – this is not a scary scenario for the majority of people.
What Steve said, in terms of numbers. That’s a really interesting thought. I have seen research stating that when you are fat when you are young, you have developed a large quantity of fat cels. And as Steve says, numbers may overcome all sorts of other things, like willpower, dietary interventions, etc. It’s worth considering. Maybe we can’t fix everything?
Jimmy owes me an apology – does Robb Wolf and about two-thirds of the Paleosphere. I was right about Jimmy when it was wasn’t cool to be right about Jimmy. Ya’ll better recognize… And as Jimbo would say, THANK YOU to the haters -for just making me more famous. 😉
Yes, Evelyn, you were one of the early ones to figure out that Jimmy and Gary were misguided. I think you’ve got the accolades already covered, with this and many other self-pats on the back, making further recognition redundant. 🙂
Evelyn will never understand how to be a good iconoclast, you must do it with style, flair, gusto, minimize long boring posts…and laf and shit on your own self now & then.
Most importantly, you have to give people glimpses of your own real life.
It’s a shame. I never really hated her. If I did, I’d have never spent a second on her.
Call me selfish if you like, but I’m less interested in who has the worst style or who is the biggest jerk than in what the facts are and how they can help me (and others). When it does come to style, I’ll vote my preference for Paul’s polite, humble, reasonable, fact-focused style (putting aside questions of who is more correct for now).
Please don’t get me wrong, I do value the useful information that you and Evelyn share, I could just do without the drama. The biggest downside of a “take-no-prisoners” approach, shall we say, is that it’s not uncommon that when someone tries to warn about the potential dangers of versions of VLC/keto, that someone replies by saying something along the lines of “Oh no, it’s another crazy Carbsane/Richard Nikoley” and it gets dismissed.
I don’t expect perfection from anyone and I try to cut people some slack when they are sharing info for free like you two are, commendably. FWIW, I just vote for a truce between the two of you and for more focus on sharing information and helping others than on credit or vengeance, for the good of all. Lately it seems like you both have been less into drama and I’m hoping that continues. It’s becoming increasingly clear (if it wasn’t already) that the long-term dangers of extreme chronic VLC/keto are too serious to let get drowned in personal drama.
If anyone actually thinks this is Evelyn … lol … not too swift.
If you know her and she disagrees with the comment attributed to her, then by all means let her know so she can set the record straight.
Whoever it is, it’s a fair point that Evelyn saw through the VLC and keto dogma before many.
And if it was you, just fess up. 🙂
Yes Trina. Everyone is well aware that Evelyn doesn’t slum. Two failed show ups to AHS showed that (or, didn’t want to put her science-based fat ass on display take your pick).
What’s the real laf is that you think anyone really cares. She’ll get wind of this guaranteed, so you expose yourself as a typical fool who doesn’t understand, but finds room to laf.
Which is actually good yin -yang wise, but still not very perceptive.
Well, it’s good to know that it was a troll impersonating Evelyn, so thanks to Trina for that tipoff. I wasn’t familiar with this troll’s tactics, as I tend to ignore trolls. So since it wasn’t Evelyn praising herself, I take back the redundant comment and give her credit where credit is due.
If anyone actually knows Evelyn, I think it’s clear that’s not how she writes. Funny nonetheless 🙂
Not sure why Richard is getting so cranky.
Well Trina, I’ll tell you. I’m down here in Baja, wife up in San Jose and I’d just learned she passed me in the daily Fitbit challenge with just over 16k steps so I had to go out walking from 11-midnight in order for the win at 17.5k steps.
I’m much better now. 🙂
Yes Trina, I think I know what you’re referring to and will be on the lookout in the future. Thanks again for the tipoff.
What time do you serve the 2 meals/day?
noon and 6 pm.
Hey Paul,
Bill Lagakos is quite insisting on his caloriesproper.com blog that breakfast and morning light are important because you get a good synchronization of our biological clocks (one that is influenced by food intake, the other by light exposure). So if one gets his/her caloric bulk at breakfast and lunch while soaking in daylight, evening food becomes just a matter of a light snack so as not to go to bed hungry.
I believe the PHD recommendations have the rest in place (blue blockers, good night sleep, physical activity). So what say you about early food intake ? And why delay food intake by skipping breakfast ?
Hi Man,
A consistent morning light trigger is important, and we recommend also getting some light physical activity at onset of day as well to coordinate the activity zeitgeber. But I’m not convinced that you need to simultaneously provide a morning trigger for the digestive-metabolic clock. It is influenced by the central (light-driven) and systemic-metabolic (activity-driven) clocks, and if you keep your peak food intake at the peak time of the digestive-metabolic clock (early afternoon), then it will have the right phase.
I’ve looked at most of the papers he’s cited and there are many ill effects to the digestive-metabolic clock being out of phase with respect to other clocks, but no evidence that you need a breakfast trigger in order to be in phase.
So we’re 98% in agreement but I think the benefits of intermittent fasting outweigh any circadian advantages to a breakfast trigger at start of day.
Paul,
Thanks for chiming in. One can intermittent-fast by skipping evening food I presume 🙂
If I remember correctly what Bill mentioned, there is a time dependence on insulin sensitivity in different tissue types: muscles are IS in the morning, fat isn’t, and opposite in the evening: fat is more IS while muscles not as IS as in the morning …
But maybe all of those details are 2nd order things. If one keeps good sleep and respect circadian rhythm without excessive blue light and other stressors in the evening, then provided that you eat good quality foods and move, you’re OK.
Why have the carbs do high. I have read your reasons but they do not convince me. I use to eat higher carbs but m glucose insulin a1c etcetera do better with a doctor Richard k bernstein level or lower.
Bear Stanley ate eggs meat cheese and butter from 1959 till his detain 2011. Many peoples like the plaines peopl of North America or headers in Africa
Eat a very low carb diet.
I prefer to keep my blood sugar between 65-80 and enjoy these health benefits
Great for those who like your diet BUT for many it maybe less than optimal but much better than the sad American diet or radical vegetarian diets.
Eric
Is that the same Bear Stanley who claimed his heart attack was “the result of some poisonous broccoli his mother made him eat as a youth”? 🙂
No, that was throat cancer, I believe, which I think he got over. Don’t think he had a heart attack.
The most notable thing about the Bear is that back in the day, he cooked the purist LSD available.
I see that others say the media got it wrong and that the Bear had heart surgery for a blockage, rather than a heart attack, and that he claimed he had the blockage since before his meaty diet and blamed it on the carby diet of his youth and just hadn’t bothered to get it treated until much later. Whatever the reason for the heart blockage, his broccoli retort was funny. 🙂
Even if Bear told the truth, we know his diet didn’t clear his blockage like some of the most positive claims about VLC/keto might lead one to expect, and like some studies report and claims for other types of diets and therapies, such as those of Dr. Dean Ornish http://www.webmd.com/heart-disease/features/can-you-reverse-heart-disease, and Dr. William Davis and others http://www.peaktestosterone.com/Clear_Your_Arteries.aspx.
I read before that Bear said his throat cancer was due to HPV, rather than his diet, and that his diet prevented it from getting worse, though it didn’t cure the cancer like some keto claims might again lead one to expect. He was also treated with chemo, which left him looking a wreck.
Wish I could remember Kurt Harris’ comment about the wisdom (lack thereof) of following the diet recommendations of an LSD cooker. 🙂
A study suggests that Dr. Bernstein’s obsessive focus on keeping BG very low may be misplaced, at least for T2D patients: “no improvement was seen in the rate of overall survival” for T2D patients assigned to “intensive glucose control for 5.6 years” http://www.nejm.org/doi/full/10.1056/NEJMoa1414266
That finding is in line with the Jaminets’ advice to eat starch.
VLC “experts” tend to regard glucose unequivocally as a toxin, whereas Paul stresses that it is a nutrient. Carb phobia, including an obsession with repressing BG, is a road to insulin resistance.
Eh…
The problem there is that ‘intensive glucose control’ is in conventional medicine achieved entirely with drugs, some of the commonly prescribed ones (depending on the time period they were studying) are now known to cause heart issues. And that’s out of possible toxicity otherwise.
So that’s not really a critique of what Bernstein is doing, which has diet as a first line, with drugs used to fix what the diet can’t. He advocates as small amount of drugs as possible.
That’s also a lot less tight control than he advocates.
It MAY be that Bernstein is wrong or misguided, but the ACCORD and ADVANCE trials don’t really show that.
Did you bother to read the study treatment guidelines before commenting? The “intensive glucose control” wasn’t restricted to being “achieved entirely with drugs.”
I still currently follow a relatively LC approach and I’m not a fan of “conventional advice,” but even I’m aware that conventional advice typically includes more than just drugs. If your physician limits himself to only drugs, it’s time for a new physician.
Yes, the study did not analyze Dr. Bernstein’s protocol, so it of course isn’t solid proof regarding that one way or the other. It does nonetheless raise questions about his recommendations on keeping blood glucose chronically well below levels for which research studies have found benefit and it would be unscientific to simply dismiss the research entirely because it isn’t exactly apples to apples.
Without subscribing to the NEJM to read their article, I went to the clinical trials website about it.
What it extensively mentions is a drug regimen, and briefly mentions diet and exercise.
It doesn’t specify what these are, but it mentions that they are what is routinely available to diabetologists.
https://clinicaltrials.gov/ct2/show/study/NCT00032487?show_desc=Y#desc
I am going to assume, then, with the caveat that this indeed an assumption, that the diet and exercise intervention is what the ADA recommends.
Which means that in effect, assuming the patient ate what they ate, blood glucose control was entirely achieved with drugs. Because the ADA diet flat out will not do so.
So unless you can show me evidence that isolates blood sugar control per se as the factor, and not the drugs, then this study isn’t evidence of much beyond the fact that blood sugar control in and of itself isn’t necessarily useful for all cause mortality.
I could do a study where I use a chainsaw to reduce overweight people to normal weight, and then conclude normalizing weight doesn’t improve health, but it’d be a poor way of showing dieting to lose weight doesn’t improve health.
But it’s possible I missed something in the publicly available stuff on this or that the article in the NEJM is more specific about diet.
“this study isn’t evidence of much beyond the fact that blood sugar control in and of itself isn’t necessarily useful for all cause mortality.”
Add the qualifier “intensive” or “strict” or “semi-strict” or whatever you want to use to describe the lower-than-usual BG targets in the study and you have the gist of my original point, and we therefore appear to basically agree on that. The point wasn’t that the study proves anything, just that it raises questions about whether aiming for chronically very low BG #’s is the right focus (and please note my use of the qualifier “may” in my original comment on the topic). More study and analysis is of course needed. I’m also skeptical of whether Bernstein’s even tighter BG control would be any more beneficial re: overall mortality, and I say that as someone who used to be quite persuaded by him. If you have good evidence on that (and I don’t mean just anecdotes, like Dr. Bernstein’s longevity, which is an interesting aspect of his n=1, but even less solid evidence than the study), feel free to share it.
“I could do a study where I use a chainsaw…”
I could also throw red herrings at you, but I’ll refrain. 🙂
“assuming the patient ate what they ate, blood glucose control was entirely achieved with drugs. Because the ADA diet flat out will not do so.”
Do you also flat out deny the possibility of any BG control from exercise, which is included in the of recommendations of both the VADT and Dr. Bernstein?
Perfect.
Yes, ultimately one ought question this obsession with chronically ultra low BG, when spikes to 140ish are perfectly physiologically normal.
It’s like trying not to exert yourself in order to never let your bpm get above some arbitrary number that’s substantially less than physiologically appropriate and arguably, healthy EXERCISE.
The more I contemplate it, the whole Keto/VLC thing is no more than an “exercise” in “training” one’s metabolism to be a total whimpy ass couch potato (insulin resistant), where any significant amount of carbs send BG to 200 and above. That’s where I was. Now I can drink a 12oz Mexican Coke (sugar, not HFCS, though probably no difference) now & then and have a normal BG response.
“Yes, ultimately one ought question this obsession with chronically ultra low BG, when spikes to 140ish are perfectly physiologically normal.”
I hesitate to use “perfectly/perfection” to describe any natural phenomenon, but I get your gist–that peak numbers up to thereabouts or even a bit more haven’t been found to be associated with any harm in studies. I don’t see the point of avoiding multiple common foods and socially ostracizing oneself with a severely restricted diet in order to meet far lower BG targets that so far haven’t shown evidence of significant benefit and are increasingly being connected to unintended consequences.
Coincidentally, such an extreme approach smacks of perfectionism, which when carried too far can be counterproductive, which I confess I know all too well, and perhaps may help explain how I ended up trying VLC for years and even ZC for a time, whereas most people regard it as extreme and even crazy (and they let me know that, which only encouraged me to dig my heels in further 😛 ).
“The more I contemplate it, the whole Keto/VLC thing is no more than an “exercise” in “training” one’s metabolism to be a total whimpy ass couch potato (insulin resistant)”
You hit the nail on the head, Richard, and I realized that this is what I was unintentionally doing, but I find that this is an off-putting concept for most people, and I haven’t yet found a way to communicate it that isn’t off-putting. No one likes to think they are coddling themselves, least of all Americans, we who tend to like to think of ourselves as tough, independent, hard working, self sufficient, individualistic, pull ourselves up by the bootstraps, don’t need the guvment/handouts and such. For some, it’s only when they’ve hit rock bottom and realize that something is seriously wrong that they’re willing to consider that maybe what they’re doing isn’t “perfect”/”infallible”/”maverick” after all, but actually “coddling”/”weakening”. I consider myself lucky that I didn’t wait until I reached Jimmy’s level (and in some ways he started out in much worse shape than I, so I’m not criticizing him at all), and I kept at it longer than most, so I’m no genius, that’s for sure.
I also try to stay humble and keep in mind that I may still be doing things badly and there may be much more for me to learn. If I was wrong before, I could be wrong again.
Nassim Taleb’s elaboration on Richard’s point about avoiding the “whimpy ass couch potato” approach — Avoiding Stressors by Coddling vs Building Antifragility: https://www.youtube.com/watch?v=MMBclvY_EMA&feature=youtu.be&t=2273
I’m confused, a little. I was diagnosed with T2D in 2008, and lowering my carbs (and getting rid of a lot of junk) helped me control my blood glucose. This year, and in recent past, I ate a lot of sugar and gluten free stuff. I have been off wheat for 4 years. My blood sugars were way out of control!
Since March, I gave up sugar and have only a little stevia, xylitol, or erythritol. My sweet tooth is mostly under control, and I use berries for my sweet. I was following a grain free/starchy veggie free diet. My blood sugar went down some, but not enough. And then I added back in white rice (that one is very recent), pinto beans (also recent), and potatoes. Not eating tons, but my blood sugars are still high (over 200, altho this is better…they were in the 300s).
Do I keep on with this WOE? I eat plenty of butter, coconut oil, and other saturated fats, along with some olive oil on salads. Protein and veggies that grow above ground, plus some ‘safe starches’? I really don’t want to take the drugs the doc prescribed (metformin, glimeperide, lisinopril) because the metformin gave me horrible diarrhea.
Suggestions?