Hippocrates famously said, “All disease begins in the gut.” I think we can narrow it down further: much modern disease begins in the mucus.
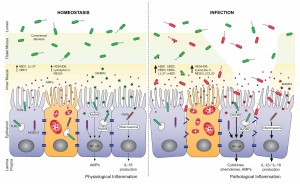
In a recent post, I put up this picture:
It’s from a paper on the role of antimicrobial peptides in maintaining gut health. [1] The point of the left panel is that a healthy gut is characterized by a thick mucosal layer that shields our intestinal and immune cells from direct contact with bacteria. The inner mucus layer is infused with antimicrobial peptides to minimize its bacterial content. The outer mucus layer contains a population of friendly mucin-degrading bacteria – symbionts like Akkermansia who evolved to feed on our mucus. These friendly bacteria provide another layer of defense against infectious pathogens; bacteria tend to be quite good at keeping out competitors. Akkermansia has been found to prevent obesity.
In an unhealthy gut, on the other hand, the mucosal layer often gets stripped away. The image (right panel) attributes this to infection, which is one possibility, but nutritional factors also matter. For example:
- Deficiencies of vitamins A or D will reduce production of antimicrobial peptides, making it easier for pathogens to reach our gut cells;
- On very low-carb diets, production of mucin-2, the primary constituent of gut mucus, may be limited in order to preserve glucose for the brain (see “Dangers of Zero-Carb Diets, II: Mucus Deficiency and Gastrointestinal Cancers,” Nov 15, 2010);
- Deficiencies of dietary fiber, vinegar, choline, and other nutrients may impair gut motility, leading to concentrations of partially digested food and bacteria at specific points in the intestine.
Regardless of why it happens, once bacteria come into direct contact with our gut and immune cells, they trigger inflammation and tend to loosen the gut barrier. This allows live bacteria and cell wall components from dead bacteria to enter the body from the gut.
Endotoxins – toxic compounds released when bacteria die, such as lipopolysaccharides from the cell walls of gram-negative bacteria – are immunogenic and inflammatory. A large influx of endotoxins into the body is “endotoxemia” – poisoning by endotoxins. As little as 2 nanograms LPS per kilogram body weight will induce fever, and 1 microgram LPS per kilogram of body weight will induce shock. [2]
Diseases caused by endotoxemia include:
- Hepatitis [3]
- Diabetes [4]
- Heart disease [5]
- Obesity [6]
- Pulmonary hypertension [7]
- Dyslipidemia [8]
- Chronic kidney disease [9]
Many of today’s most prevalent diseases are caused by chronic endotoxemia.
So it behooves us to avoid it. If endotoxemia is fundamentally caused by the loss of a protective mucosal layer in the gut, how do we assure healthy production of mucus?
A recent paper sheds valuable light on that question.
Natural Whole Foods, High-Fat Diets, and Gut Health
It’s well known that in mice, “high-fat diets” induce endotoxemia. But these diets aren’t necessarily high in fat – any pelleted rodent food in which fat provides more than 20% of calories may be called “high-fat.” The critical difference of “high-fat diets” from chow is that they are composed of purified nutrients – starch, sugar, oil, vitamins, and minerals – whereas chow is composed of natural whole foods such as wheat, corn, and seeds.
A recent study tried to distinguish whether the cause of endotoxemia is the fat, or the purified starch, sugar, and oil. It made up three diets of varying fat content (8%, 48%, and 74% of energy respectively), but composed of natural whole foods. [10]
The result was remarkable:
[U]sing complex [i.e. natural whole foods] HFD, no associations were observed between dietary lipid amounts and the magnitude of endotoxemia, inflammation, and physiological alterations developed.
It turns out the endotoxemia that typically develops on high-fat diets is due to getting the calories from purified sources – starch, sugar, oil – rather than from whole foods. On a whole foods diet, the amount of endotoxin entering the body is more or less independent of the amount of fat consumed.
This is surprising in one respect. Lipopolysaccharide is fat-loving and enters the body along with dietary fat. So it stands to reason that a higher-fat diet would carry more endotoxin into the body.
But it turns out the body has mechanisms to regulate how much endotoxin enters the body. It wants a small amount so that the immune system can sample the gut microbiome, but not so much as to cause inflammation.
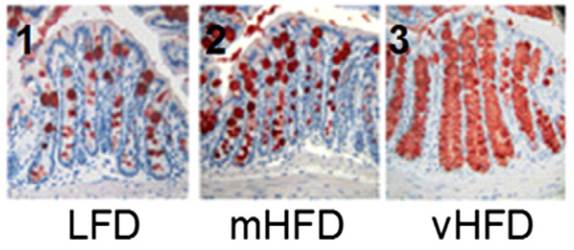
The primary mechanism for controlling endotoxin influx? Mucus production. The study noted that the mice eating higher-fat “had an increased number of goblet cells … [and] an increased MUC2 production.” MUC2 is mucin-2, the primary component of mucus in the gut.
Here is a picture with mucin-2 in the mucin-producing goblet cells stained red:
It’s obvious that mucin production goes up dramatically as the fat content of the diet increases.
The study concludes,
“We show that, in complex HFDs based on chow ingredients and milk fat, there was no association between dietary lipid amounts and the magnitude of metabolic endotoxemia or low-grade inflammation.”
If high-fat diets are healthy, we can thank our mucin-producing goblet cells.
One last note: the fact that mice can produce healthy amounts of mucus on a 74% fat diet does not necessarily mean that humans can do the same. Humans have much larger brains than mice, and as a result our carbohydrate needs are larger. It’s possible that mice can maintain mucus production on a low-carb diet better than humans can.
References
[1] Muniz LR, Knosp C, Yeretssian G. Intestinal antimicrobial peptides during homeostasis, infection, and disease. Front Immunol. 2012 Oct 9;3:310. http://pmid.us/23087688.
[2] Warren HS et al. Resilience to bacterial infection: difference between species could be due to proteins in serum. J Infect Dis. 2010 Jan 15;201(2):223-32. http://pmid.us/20001600.
[3] Parlesak A, Schäfer C, Schütz T, Bode JC, Bode C. Increased intestinal permeability to macromolecules and endotoxemia in patients with chronic alcohol abuse in different stages of alcohol-induced liver disease. J Hepatol. 2000 May;32(5):742-7. http://pmid.us/10845660.
[4] Moreno-Navarrete JM et al. Circulating lipopolysaccharide-binding protein (LBP) as a marker of obesity-related insulin resistance. Int J Obes (Lond). 2012 Nov;36(11):1442-9. http://pmid.us/22184060.
[5] Lepper PM et al. Association of lipopolysaccharide-binding protein and coronary artery disease in men. J Am Coll Cardiol. 2007 Jul 3;50(1):25-31. http://pmid.us/17601541.
[6] Cani PD et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007 Jul;56(7):1761-72. http://pmid.us/17456850.
[7] Dschietzig T, Alexiou K, Richter C, Bobzin M, Baumann G, Stangl K, Brunner F. Endotoxin causes pulmonary hypertension by upregulating smooth muscle endothelin type-B receptors: role of aldose reductase. Shock. 2008 Aug;30(2):189-96. http://pmid.us/18091567.
[8] Lassenius MI et al. Bacterial endotoxin activity in human serum is associated with dyslipidemia, insulin resistance, obesity, and chronic inflammation. Diabetes Care. 2011 Aug;34(8):1809-15. http://pmid.us/21636801.
[9] McIntyre CW et al. Circulating endotoxemia: a novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J Am Soc Nephrol. 2011 Jan;6(1):133-41. http://pmid.us/20876680.
[10] Benoit B et al. Increasing fat content from 20 to 45 wt% in a complex diet induces lower endotoxemia in parallel with an increased number of intestinal goblet cells in mice. Nutr Res. 2015 Apr;35(4):346-56. http://pmid.us/25687164.











Very interesting post! But I couldn’t help but notice that the researchers used dairy fat. Dairy fat is very high in butyrate, a short-chain fatty acid that is known for its immunomodulatory and gut-strengthening properties.
Here’s a relevant article: http://wholehealthsource.blogspot.com/2009/12/butyric-acid-ancient-controller-of.html
Many different health practitioners have used butter and ghee to heal the gut in the case of inflammatory bowel disease, fistulas, ulcers, and leaky gut. So it appears more research needs to be done!
Hi Paul,
For someone who probably suffers from endotoxemia would it be wise to keep fats low? Or just eat the standard Perfect Health Diet?
Hi Matthew,
Standard PHD. If you are trying to lose weight, cut down the fats/oils a bit.
I do not think this is good advice Paul, for 3 reasons (amongst others).
1) Endotoxaemia can’t be divorced from inflammation and diets low in carbohydrates (amongst other features) substantially improve inflammatory markers. See multiple PubMed studies & basic textbook mechanisms for this.
2) It contradicts many rigorous clinical studies showing LCHF diets to be more effective for losing excess fat mass (obesity). See PubMed & recent meta-analyses.
3) It contradicts basic physiology where surplus carbohydrate is converted to palmitic acid (a saturated fat) by the liver and is then exported into VLDL particles which lose their cargo (to adipose tissue), eventually becoming sdLDL particles. The fate of dietary fat (like mono & saturated fats) goes the chylomicron route which does not suffer the same fate nor gets stored in adipose tissue with such ‘ease’. These have profound implications for our metabolism & satiety response. See here for a more complete explanation: http://drmalcolmkendrick.org/2015/06/23/what-happens-to-the-carbs/?utm_medium=twitter&utm_source=twitterfeed
Matthew, I would advise you not concern yourself primarily with calories but with:
1) the macronutrient ratio of your diet, namely lowering total carbohydrate load, whilst
2) also focusing on maximizing the nutrient density (which means making it a high-quality diet – avoiding process foods goes without saying). An example of how to maximize nutrient density/diet quality would be to focus on organ meats, sea food & eggs, while using a variety of fibrous vegetables as an nutritive adjunct (contributing very few calories) that doubles as a fantastically delicious vehicle for fats!
Enjoy your food & good luck with
Hi raphaels7,
The LC studies in the literature are much closer to PHD levels of carbs and fat than to what Paleo community people consider LCHF.
The obesity evidence is complex but doesn’t indicate that LCHF is special as far as weight loss is concerned. Again, most of the LC studies are closer to PHD than to current LCHF Paleo. They are also short-term oriented which means they don’t address the critical questions regarding long-term sustainability of the weight loss.
On low-carb diets there is negligible conversion of carbohydrate to palmitic acid. You have to get over 40% carb before this process becomes significant.
The problem is that the endotoxins are not broken down by bile acids – http://www.psoriasisdietplan.com/2013/09/bile-acids-facts/
High fat intake induces high fat absorption what makes the body absorb also the LPS. Significantly increasing the blood endotoxins levels – http://care.diabetesjournals.org/content/35/2/375.full
Hi Paul,
In your book, you gave precise recommendations about quantities of vitamin A, vitamin D, and choline. Do you now have more precise ideas about how much vinegar and how much fiber would be optimal?
Thanks!
Eric
Hi Eric,
It’s hard to say what the optimum is but it appears that nearly everyone is currently getting too little. The too are related because fiber becomes vinegar (acetic acid) in fermentation.
Hi Paul,
I don’t believe you said how the mucus and muc2 gets to the gut and into the proper position shown in the diagram? Is it secreted in all cells of the body or just in some areas of the digestive track like the sinuses or stomach and intestines? Is it secreted right on point at the critical intestinal lumina lining or does it land there?
Hi Perry,
It is generated in the goblet cells lining the gut. http://www.ncbi.nlm.nih.gov/pubmed/20703838
Hi Paul
My understanding from the abstract of the study is that the 8% and 74% fat diets were healthier than the 48% fat diet as only the mice on this diet developed endotoxemia and inflammation. Have you any ideas about why this might be?
As a consumer of the PHD, which could also be considered a moderate high fat diet, I’m a little confused. Some say high a high saturated fat diet should be coupled with few carbs for blood lipid reasons and I’m wondering if this might be evidence for that? Hopefully not
In the meantime I’ll still be eating my potatoes, rice and plantains!
Hi Harry,
It all comes down to maintenance of a healthy gut. The middle diet was challenging because it had enough carbs to build a large bacterial population and enough fat to carry large quantities of endotoxins. But the mice still did much better with seeds and cereal grains than purified nutrients. If they’d eaten PHD foods, I bet they’d do even better.
Thanks Paul!
Amazing, thank you Paul! I came to the PHD website this morning to search the archives for anything you might have posted of VLC diets and the integrity of the gut lining, and here it is!
For someone on a VLC diet due to SIBO, where do you think one should draw the line? I am fairly active during the day, do HIIT and/or weight training every other day and have already started experiencing dry eyes and decreased cognitive ability (word- finding problems, poor recall of number codes etc). I have probably stayed around 50 g of carbohydrate for the past month, and in general on a LC diet for years ( again, due to SIBO and some fungal overgrowth). Any advice on how to balance this? I do add a teaspoon of Dextrose to my water bottle for workouts.
Thank you so much!
Hi Webraven,
If you are experiencing dry eyes, then you will definitely be underproducing mucus in the gut and elsewhere. So you are definitely too low carb. Fungal overgrowth is also a sign of being too low carb.
I believe that PHD is the best for most people, and probably for you too. Starch is better than dextrose. SIBO should be addressed by other methods than carb restriction, e.g. nutrition for immunity and gut motility, acidification of the diet, intermittent fasting, circadian rhythm entrainment.
Thank you much for the reply, Paul!
Around the time of the publication of your first edition you recommended dextrose in the case that starch exacerbated symptoms. Have you amended that recommendation, or are you saying that starch is more beneficial specifically for the mucous layer because the goblet cells utilize the starch as it passes through the GI tract, before absorption into the blood stream?
Unfortunately the only thing that’s decreased symptoms so far has been carb restriction combined with anti-microbials (unless there is a lot more to acidifying the gut than making sure there are adequate levels of HCl and using vinegar?) and I seem to be stuck with the LC angle, albeit worried about its many negative consequences.
Do you think a small, slow trickle or starch or “carb cycling” would be more beneficial in terms of mitigating potential damage? Currently I’m basically eating my small amount of carbs (berries mostly) only at night.
Warm thanks!
Like Webraven, I am very interested to read you write you think starch is better than dextrose for SIBO as I too read you suggest previoulsy dextrose for those trying to eliminate sibo as I presumed though both glucose dextrose is absorbed quicker than starch which is a polysaccharide? Many thanks
Hi Annie,
Dextrose is for symptom management in extreme circumstances. Starch is better for those who can tolerate it. In general, the digestive tract works better on natural whole foods like starchy plants than it does on purified nutrients like dextrose.
Best, Paul
Hi Paul,
Could the lectins be a cause of endotoxemia ? And what about the ones in potatoes and tomatoes for example ? What do you recommend to flush them ?
http://www.greenmedinfo.com/article/potato-lectin-has-chitin-binding-properties-indicating-it-may-have-inflammatory-properties
Thanks for your incredible and so useful work.
Best,
Penelope
Most lectins are destroyed by ordinary cooking. (Although the lectins found in wheat and peanuts survive cooking.)
In particular, from (http://www.fao.org/docrep/t0207e/T0207E08.htm#Potato):
“Lectins or haemogglutenins are also present in potato. These toxins are… of minimal nutritional significance as [they] are also destroyed by heat, and potatoes are normally cooked before they are eaten.”
Warm Thanks for your answer Eric !
lectins are not destroyed by heat… some beans are limited by soaking overnight, never by heat, unless you pressure cook them
Hi Paul,
MCTs, which constitute the majority of the triglycerides in Coconut oil, don’t require the formation of chylomicrons, therefore should not facilitate the absorption of LPS.
Am I missing something?
3rd paragraph of the Introduction:
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0008442
Is butter safe in your opinion?
Have a great day!
MCTs can carry LPS to the liver where it can cause inflammation. LPS is safest in chylomicrons. Yes, butter is safe if your gut is healthy and your diet balanced.
Hi Paul,
Just a quick question on this last post.
I eat 1 desert spoon of coconut oil everyday at breakfast. If MCTs can carry LPS to the liver where it can cause inflammation should I stop eating it?
Sorry I am not a scientist – so please forgive me if my question is a bit misinformed.
Thanks so much for all your work!
Thank you, Paul.
Do you have any suggestions for specific reliable material to research this subject further?
Paul- I just love your posts, and your information- full of science but accessible!!!
And I can not tell you how much it has helped my clients and me personally in the search for healthy living and rich eating
A big thanks to you and Shou- Ching and looking forward to your cook book someday along with a dream to attend your retreat!!!
Katie
A lot of fat and vinegar sounds like a recipe for acid reflux.
Paul
How does stress affect the gut and the mucos lining. I have lost weight in the last few days. Some foods cause me extreme diarrhea and other foods not. I’m in the middle of moving so I’m wondering if it’s the stress. I’m still eating phd.
Would appreciate any thoughts.
Thank you
FYI I’m drinking water w/ potato starch and vinager. Also ate a few onions and garlic raw. People think I’m crazy for doing this home remedy.
I would eat potatoes instead of potato starch. Stress can disrupt the gut; stress in the daytime is not bad but stress at night is a major problem.
So what would you suggest at night? I woke up with anxiety in the middle of the night. Thank you for answering my cry for help.
Paul,
I’ve been on a nutritional journey for over 5 years. I dropped 120 pounds 5 years ago purely from hitting a rock bottom and being scared straight. Mainly cardio and inadvertent intermittent fasting. However, for the past 3 years I’ve been chasing body composition and optimal brain health, as I’m a medical student.
I started carbohydrate cycling and have been doing it for two years. However, my protein consumption had been way too high and my fats (or carbs) not high enough and I have developed (what I believe to be) a putrefaction dysbiosis. Any amount of protein I eat over 20g in one meal will give me horrible hydrogen sulfide gas within 20-30 minutes of eating, bad brain fog, and even depression and the feeling of being uncomfortable in my own skin until the protein is metabolized.
I just finished reading your book (and it’s the best I’ve read on the subject of nutrition and I have been doing the PHD for 2 weeks now. I’ve decreased my protein intake dramatically and have seen GI improvement, but at this point I can’t sustain the level of weight lifting that I’m used to and am sore all the time. Gastro doc just wanted to run me a strong course of antibiotics, but I want to hold off on that. Any recommendations?
I really appreciate the time you put into answering questions and am considering the perfect health retreat as I live in Greensboro, NC, so Wilmington wouldn’t be such a trek!
Try lowering your workout load. Go with 1 set to failure for every muscle group trained that day. Work out 3 times a week or less. You should gain just as much lean mass this way.
You can supplement with branch-chain amino acids to compensate for the decrease in protein, which should boost your protein synthesis.
Paul – what do you think of bitters?
http://www.westonaprice.org/health-topics/abcs-of-nutrition/bitters-the-revival-of-a-forgotten-flavor/
Paul
I have read the material on higher carb diets and still do not see the net advantages
When compared to lower carbohydrate ketogenic diet. Carbs increase palmatalic acid (not good)
Compare insulin glucose hba1c and PALMATALIAC acid.
Still your take on diet is better than the SAD way of eating.
I am sure many would object to my eating ketone salts to lower glucose and insulin while increasing my ketone levels.
Maybe I missed the part where moderate protein and electrolyte resulted in problems. How many per 100 or 1000 people had this problem?
Eric A
Hi Eric A,
The liver will only convert carbs to palmitic acid when given carbs in excess of its capacity to store carbs as glycogen.
Since the liver can store about 125g of carbs as glycogen, and Paul only advocates a daily intake of 150g of carbs (distributed throughout the day so some will be burned before the final carb feeding), production of palmitic acid from carbs should be negligible on the perfect health diet.
Best,
Eric (a different Eric from above)
Parities acid
And your post did not address this.
Also Phiney, Voleck, Fung, nor Richard K Bernstein have not seen this.
So we have years of research and many many
Patients vs what???
palmitic
Dear Paul,
usually I read about a link between high saturated fat intake and inflammation and insuline resistance (for example here: http://atvb.ahajournals.org/content/30/4/692.full).
What do you think about?
Hi ML,
This is a rather complex topic, but I doubt that such an abundant component of the human body is inflammatory in all dietary contexts. I believe the problems with saturated fats are largely restricted to energy-excess diets. Also, don’t put much faith in molecular mechanisms like TLR4 interactions – there are homeostatic mechanisms regulating inflammation, so even if SFA stimulate inflammation by one pathway, other pathways will tend to bring it back to normal. So I wouldn’t expect an observable negative health impact, and the large-scale studies don’t show one.
However, this is a large literature and I haven’t read all of it; and biology is very complex.
Do you have specific recommendations for recovering this mucus layer once it’s gone? Is that covered in your book?
Yes, follow our diet and lifestyle advice. It can always come back.
Hi Paul
As part of healing compromised gut mucin, would you recommend taking probiotic SB to increase SIgA to prevent infections?
Maybe but not necessarily, it depends. A clinician should use professional judgment on that one.
Paul,
The other part of the abstract of the paper you cited seems to indicate negative effects of high fat. I am a bit confused.
“Only vHFD mice significantly increased body weight and fat mass vs LFD mice. This was associated with increases of plasma concentrations of triglycerides, leptin and adiponectin, and liver lipids. No such differences were observed between LFD and mHFD mice. However, mHFD developed metabolic endotoxemia and inflammation, unlike vHFD mice.”
Hi W, Yes, the mice diets were hardly perfect. Getting 2/3 of calories from milk fat will lead to undernutrition and an excess of calories leading to weight gain. The diet needs to be balanced and complete in every nutrient to avoid negative effects. The main point was that a whole foods diet, even an unbalanced one, prevents the endotoxemia.
Hi Paul,
I was wondering if you could provide a rationale for why you think a lack of vinegar may lead to motility problems in the gut. I am considering adding apple cider vinegar to my diet, but I would love to see a study before going out and buying it.
Two reasons, acetate supports acetylcholine which supports motility, and the acid helps clear SIBO which interferes with motility.
Hi Paul, I have very slow motility, which is probably why I don’t tolerate vinegar (acidic things in general) well. Lemon juice in small amounts is better tolerated. Does lemon juice have the same benefits as vinegar in terms of motility?
Paul,
What do you suggest for those who are intolerant to vinegar. I have an issue with histamine and all vinegars cause a severe reaction. Hives and tachycardia. Should I just eat more fiber so that the bacteria ferment it into more organic acids?
Hello Paul!
What is your opinion about this study, where they found that serum endotoxin concentration was highest when meal consumed with saturated fats (coconut oil) compared to meal with PUFA (fish oil and grapeseed oil)?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5097840/
Hi Nani,
That’s a short-term effect, but if your diet is consistent, the gut adapts to control endotoxin influx to the desired level. In the long run, eating a consistent diet high in saturated will give you better health overall through better control of gut microbes and a tighter intestinal epithelial barrier. I blogged about this here: https://perfecthealthdiet.com/2015/06/disease-begins-in-the-mucus/. Note also that the higher endotoxin influx with saturated fat is primarily found from junk foods, not natural whole foods.
Best, Paul