Last week’s post (Is It Good to Eat Sugar?, Jan 25, 2012) addressed what I see as the most problematic part of the thought of the health writer Ray Peat – his support for sugar consumption.
Apart from this difference, “an extreme amount of overlap is evident,” Danny Roddy notes, in our views and Peat’s. Both perspectives oppose omega-6 fats, support saturated fats, favor eating sufficient carbs to normalize metabolism, support eating nourishing foods like bone broth, and oppose eating toxic foods like wheat.
If there is another difference between our ideas and Peat’s, it’s that “Peat-atarians” often eat more carbs. Danny puts it:
Paul and Peat have similar recommendations for carbohydrate consumption. Paul’s recommendations hover around 150 grams while Peat usually recommends 180-250 grams, but he himself eats closer to ~400 grams.
So I thought it might be worth looking at the issue of overall carb consumption.
Carbs for Hypothyroidism
In Is There a Perfect Human Diet? (Jan 18, 2012) we noted that diseases can change the optimal diet. In some diseases it’s better to lower carb consumption, but in others it’s better to increase carb consumption. The example we gave is hepatitis; hepatitis B and C viruses can exploit the process of gluconeogenesis to promote their own replication, so high-carb diets which avoid gluconeogenesis tend to slow down disease progression.
Another disorder that might benefit from more carb consumption is hypothyroidism. A number of people with hypothyroidism have benefited from Peat-style carb consumption. Here is ET commenting on last week’s post:
As someone following the PHD with a good dash of Peat, I really enjoy this post and the comments. Thank you Paul….
Paul says that “I’m not persuaded that it’s a desirable thing to keep liver glycogen filled at all times, but for some health conditions it may be good to tend that way, like hypothyroidism.” Well, according to Chris Kresser, 13 of the top 50 selling US drugs are either directly or indirectly related to hypothyroidism. If going by either the low body temperature/low pulse diagnostic, and/or some kind of pattern on the serum tests (Anti-TG, TPO, TSH, free T-3, free T4, total T3, total T4), we are talking a significant proportion of the population, especially women, being hypothyroid in some form….
Many with low T3 have a conversion problem from T4 in the liver (80% of T3 is converted from T4 in the liver and kidneys – only a small portion is coming from the thyroid gland).
Is it a good idea to NOT try to fill the liver glycogen in such a pattern? For those who have lived with the consequences of low T3 (adrenaline rush, waking up in the middle of the night, fatigue, tendency to orange-yellowish color i the face etc.), and had improvements on a more Peat like diet, I do not think so.
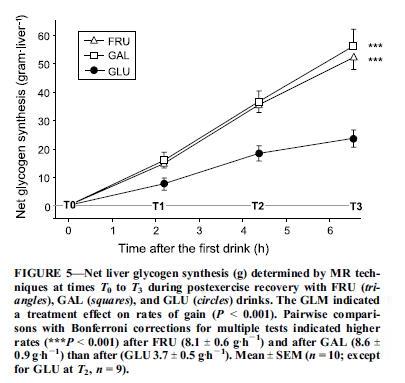
The way to fill liver glycogen, of course, is by eating more carbs.
I’ve previously noted that increased carb consumption upregulates the levels of T3 thyroid hormone (Carbohydrates and the Thyroid, Aug 24, 2011):
T3, the most active thyroid hormone, has a strong effect on glucose utilization. T3 stimulates glucose transport into cells, and transport is the limiting factor in glucose utilization in many cell types. In hyperthyroidism, a condition of too much T3, there are very high levels of glucose utilization. Administration of T3 causes elevated rates of glycolysis regardless of insulin levels.
The body can reduce T3 levels by converting T4 into an inactive form called reverse T3 (rT3) rather than active T3. High rT3 levels with low T3 levels lead to reduced glucose transport into cells and reduced glucose utilization throughout the body.
This means that eating more carbs raises T3 levels, and eating fewer carbs lowers T3 levels.
For a hypothyroid person, then, eating more carbs is an alternative tactic for increasing thyroid hormone activity. It may provide symptomatic relief similar to that achieved by supplementing thyroid hormone directly.
Perhaps the two are complementary tactics that should be done together. Taking thyroid hormone pills will increase glucose utilization, creating a need to eat more carbs. A mix of the two tactics may be optimal.
UPDATE: Mario points out that most cases of hypothyroidism in advanced countries are due to Hashimoto’s, an autoimmune disease probably triggered by infections or gut dysbiosis, and eating more carbs will tend to flare any gut dysbiosis and thus aggravate the thyroiditis. Meanwhile, supplemental thyroid hormone tends to reduce antibody activity.
Carbs for Mood
Another interesting comment came from Jim Jozwiak:
Paul, this discussion gets to the crux of what I do not understand about the Perfect Health Diet. You are speaking as if refilling liver glycogen is a good thing, and it undoubtedly is, because mood is so much better when there is sufficient liver glycogen because then the brain is confident of its power supply. Also, you acknowledge that safe starch would eventually replenish liver glycogen after muscle glycogen is topped off. So why not eat enough starch to replenish liver glycogen? It is not so difficult to figure out how much that would be. Have some sugar, feel what replenished liver glycogen is like, then titrate safe starch gradually meal-by-meal to get the same effect. When I do it, and I am not an athlete, I get 260 grams of non-fiber carb per day, which is considerably more than you usually recommend. Have you tried this experiment and found the result unsatisfactory in some way?
Jim has experimented to find the amount of carbs that optimize his mood, and found it to be 260 g (1040 calories). On a 2400 calorie diet, typical for men, this would be 43% carbs.
If Peat typically recommends 180 to 250 g carbs, as Danny says, then on a 2000 calorie reference diet that would be 36% to 50% carbs.
Those numbers are strikingly similar to another statistic: The amount of carbs people actually eat in every country of the world.
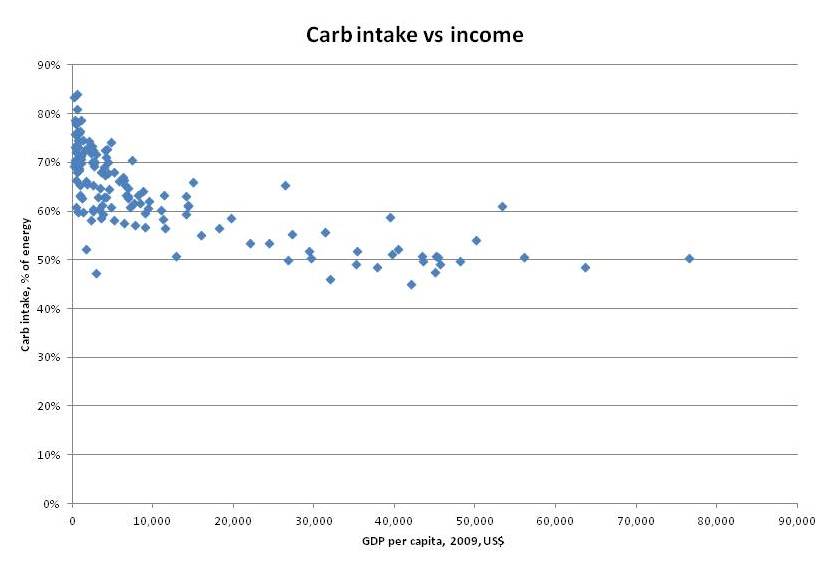
Here is a scatter plot of carb consumption vs per capita income by country. Dietary data comes from the FAO, income is represented by GDP per capita from the IMF:
At low incomes people eat mainly carbs, because the agricultural staples like wheat, rice, corn, and sorghum provide the cheapest calories.
As incomes rise, carb consumption falls, but it seems to approach an asymptote slightly below 50% carbs. The lowest carb consumption was France at 45%, followed by Spain, Australia, Samoa, Switzerland, Iceland, Italy, Austria, Belgium, and Netherlands.
We can guess that if money were no object, and people could eat whatever they liked, most people would select a carb intake between 40% and 50%.
This is precisely the range which Jim found optimized his mood.
The Longevity vs Fertility and Athleticism Trade-off
I won’t enumerate studies here, but animal studies indicate that higher carb and protein intakes promote fertility and athleticism, while restriction of carbohydrate and protein promotes longevity.
In our book, we calculate the daily glucose requirements of the human body at around 600 to 800 calories, or 30% to 40% of energy on a 2000-calorie diet.
So a 30-40% carb diet is a neutral diet, which probably places minimal stress on the body.
A 40-50% diet is a carb-overfed diet, which probably promotes fertility and athleticism.
A 20-30% diet is a mildly carb-restricted diet, which probably promotes longevity.
Do we see diminished longevity with higher carb consumption in human epidemiological data? I think so.
It’s useful to compare European countries, since they are genetically and culturally similar. There is a correlation between carbohydrate intake and longevity. Here is a list of life expectancy among 46 European countries. Neglecting little countries like Monaco, San Marino, and Andorra, that are not in my carb database, the countries with the longest life expectancy are also the ones with the lowest carb consumption: Italy first, France second, Spain third, Switzerland fourth, and Iceland sixth are all countries with carb intake below 50%. Sweden, at 50.8% carbs, placed fifth in longevity.
Did Evolution Hardwire a Preference for Carbs?
We know that the brain has an innate food reward system which tries to get people to eat a certain diet. What carbohydrate intake is it likely to select for?
Experiments on the food preferences of insects and rodents give us clues. The paper “Macronutrient balance and lifespan,” by Simpson and Raubenheimer, cited some time ago by Dennis Mangan, summarizes evidence from animals for the influence of macronutrients on lifespan. A good example is the fruit fly; protein has the dominant effect on lifespan, with low protein favoring longevity and high protein favoring fertility. The flies eat so as to maximize fertility:
The response surface for lifetime egg production peaked at a higher protein content than supported maximal lifespan (1:4 P:C, Figure 1A). This demonstrates that the flies could not maximize both lifespan and egg production rate on a single diet, and raises the interesting question of what the flies themselves prioritized – extending lifespan or maximizing lifetime egg production. Lee et al. [3] answered this by offering one of 9 complementary food choices in the form of separate yeast and sugar solutions differing in concentration. The flies mixed a diet such that they converged upon a nutrient intake trajectory of 1:4 P:C, thereby maximizing lifetime egg production and paying the price of a diminished lifespan.
This seems to be the evolutionary preference in mammals as well as flies. When unlimited food is available, animals tend to overfeed slightly on carb and protein, sacrificing lifespan for increased fertility and athleticism.
Jim reported improved mood on a 43% carb diet. Is it due to the filling of liver glycogen raising metabolism? Due to a sensation of enhanced fertility, libido, and athleticism? Or simply due to greater satisfaction of the brain’s reward system?
Yet another factor may also be involved.
Might Stress Be Mistaken for Enhanced Energy?
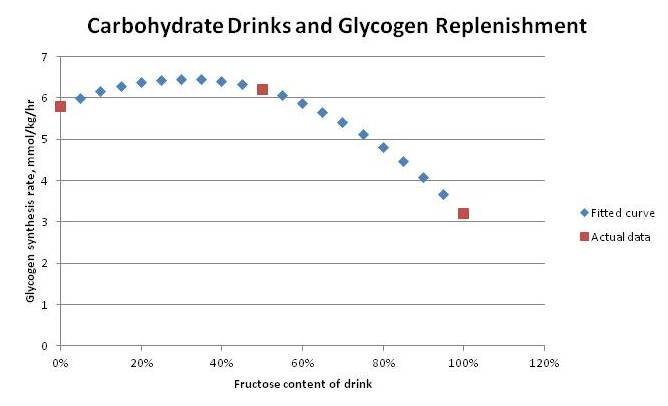
Peat favors sucrose as a carb source, which is why Danny Roddy recommended orange juice and Travis Culp soda. I argued in last week’s post that it would be better to eat a starchier diet so that the carb breakdown would be at least 70% glucose, less than 30% fructose and galactose.
Eating a higher-carb diet fills up liver glycogen, removing the most rapid fructose disposal pathway. This makes a high-carb sucrose-based diet rather stressful for the body; it has to dispose of fructose rapidly to avoid toxicity, but has limited ability to do so.
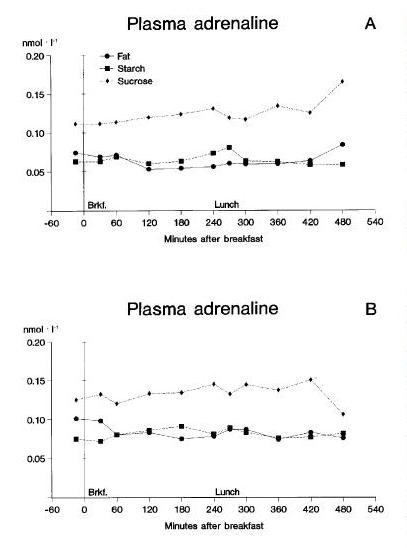
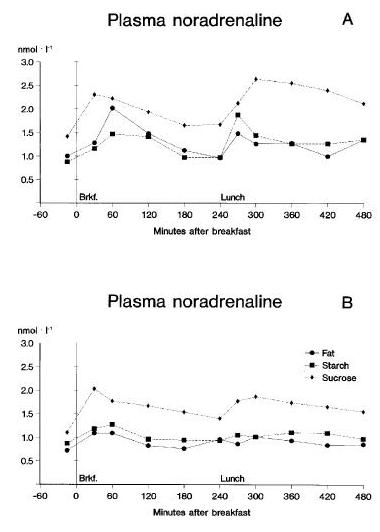
We can see the stressfulness of sucrose by its effects on the “fight-or-flight” stress hormones adrenaline (epinephrine) and noradrenaline (norepinephrine). Here is a study that fed high-fat, high-starch, and high-sucrose diets for 14 days to healthy non-obese subjects, and measured the hormonal response [1; full text]. This paper was discussed by the blog Proline (hat tip: Vladimir Heiskanen). The results:
On high-fat and high-starch diets, adrenaline and noradrenaline levels are low; they are consistently elevated — almost doubled — on the high-sucrose diet.
This makes sense; as Wikipedia notes,
epinephrine and norepinephrine are stress hormones that underly the fight-or-flight response; they increase heart rate, trigger the release of glucose from energy stores, and increase blood flow to skeletal muscle.
These hormones trigger the release of glucose from liver glycogen, thus freeing up room for fructose disposal.
Note that this result contradicts an assertion by Danny Roddy:
I consider the ability to refill glycogen (minimizing adrenaline & cortisol release) to be an important factor in health.
Refilling glycogen is not the same thing as minimizing adrenaline release. The requirement to dispose of fructose may trigger adrenaline release.
The reason I bring this up is not to renew the starch vs sugar discussion; but rather to ask if this “fight-or-flight” response to sugar consumption may not be partially responsible for the perceived mood and energy improvements on a Peat-style diet.
Indeed, one of the peculiar aspects of Ray Peat’s health advice is his recommendation to increase pulse rates well above normal levels. In his article on hypothyroidism, Peat states:
Healthy and intelligent groups of people have been found to have an average resting pulse rate of 85/minute, while less healthy groups average close to 70/minute.
I would have thought 60 beats per minute was normal, and when I was more athletic my pulse was typically 48 beats per minute.
One of the effects of adrenaline and noradrenaline is to speed up the pulse rate. If Peat really does eat 400 g of carbs per day, predominantly from sucrose, then he may be achieving his high pulse rate from an “adrenaline rush” that helps dispose of an excess of fructose.
If, indeed, this is a source of improved sense of well-being on Peat-style diets, it may be a double-edged sword. Chronic stimulation of the “fight-or-flight” hormones to aid in fructose disposal may have long-run negative consequences.
UPDATE: I’m reminded of this video, showing the adrenaline-promoting effects of sucrose consumption:
Starch would not have had the same effect, and would surely be healthier in the long run.
Summary
It is possible that higher carb intake may increase thyroid hormone levels, fertility, and athleticism, and enhance mood in some people. These gains do not come without cost. Notably, they probably involve a sacrifice of longevity.
If the benefits of higher carb intake are sought, it is best to achieve them by eating starches primarily, not sugar.
Conclusion
In our book, we recommend a slightly low-carb diet of 20-30% of calories. If we were re-writing the book now, we would probably be a bit less specific about what carb intake is best. Rather, we would say that a carb intake around 30-40% is neutral and fully meets the body’s actual glucose needs; and discuss the pros and cons of deviating from this neutral carb intake in either direction.
For most people, I believe a slightly carb-restricted intake of 20-30% of calories is optimal. Most people are not currently seeking to have children or engaging in athletic competition. There is good reason to believe that mild carb restriction maximizes lifespan, and most people desire long life. As we’ve noted, supercentenarians generally eat low-carb, high-fat diets.
But the spirit of our book is to educate, and let everyone design the diet that is best for them. And there is room for difference of opinion about the optimal carb intake.
References
[1] Raben A et al. Replacement of dietary fat by sucrose or starch: effects on 14 d ad libitum energy intake, energy expenditure and body weight in formerly obese and never-obese subjects. Int J Obes Relat Metab Disord. 1997 Oct;21(10):846-59. http://pmid.us/9347402. Full text: http://www.nature.com/ijo/journal/v21/n10/pdf/0800494a.pdf.














Recent Comments