Jan Kwasniewski developed his Optimal Diet something like 40 years ago and it has become extremely popular in Poland.
Kwasniewski recommended that adults should eat in the ratio
(Source).
In terms of calories this is roughly 240 calories protein / 1640 calories fat / 120 calories carbohydrate on a 2000 calorie diet.
The Perfect Health Diet proportions are more like 300 calories protein / 1300 calories fat / 400 calories carbohydrate. So the diets would be similar if about 300 calories, or 15% of energy, were moved from fat to carbohydrate in the form of glucose/starch (not fructose/sugar!).
Note that we recommend obtaining at least 600 calories per day from protein and carbs combined. This ensures adequate protein for manufacture of glucose and ketones in the liver. But the Optimal Diet prescribes only 360 calories total (less in women), suggesting that gluconeogenesis cannot, over any long-term period, fully make up for the dietary glucose deficiency.
In the book, we note that a healthy body typically utilizes and needs about 600 glucose calories per day. On the Bellevue All-Meat Trial in 1928 Vilhjalmur Stefansson ate 550 protein calories per day, which is probably a good estimate for the minimum intake needed to prevent lean tissue loss on a zero-carb diet.
With only 360 carb plus protein calories per day, the Optimal Diet forces ketosis if lean tissue is to be preserved. Since at most 200 to 300 calories per day of the glucose requirement can be displaced by ketones, the Optimal Diet is living right on the margin of glucose deficiency.
Gastrointestinal Cancers in Optimal Dieters
I learned over on Peter’s blog that Optimal Dieters have been dying of gastrointestinal cancers at a disturbing rate. Recently Adam Jany, president of the OSBO (the Polish Optimal Dieters’ association), died of stomach cancer at 64 after 17 years on the Optimal Diet. Earlier Karol Braniek, another leader of the OSBO, died at 68 from duodenal cancer.
A Polish former Optimal Dieter who has now switched to something closer to the Perfect Health Diet noted that gastrointestinal cancers seem to be common among Optimal Dieters:
The impression we get is that there’s rather high occurrence of gut cancer, including stomach, duodenum, colon … [source]
I want to talk about why I think that is, since the danger that the Optimal Dieters are discovering was one of the key factors leading us to formulate and publish the Perfect Health Diet.
Zero-Carb Diets Can Induce Mucus Deficiency
I ate a high-vegetable but extremely low-carb diet from December 2005 to January 2008. At the time I thought I was getting about 300 carb calories a day, but I now consider this to have been a zero-carb diet, since I don’t believe carb calories are available from most vegetables. Vegetable carbs are mostly consumed by gut bacteria, whose assistance we need to break down vegetable matter, or by intestinal cells which consume glucose during digestion.
Throughout my 2 years on this zero-carb diet, I had dry eyes and dry mouth. My eyes were bloodshot and irritated, and I had to give up wearing contact lenses. Through repeated experiments, I established that two factors contributed to the dry eyes – vitamin C deficiency and glucose deficiency. After I solved the vitamin C issue, I did perhaps 50 experiments over the following few years, increasing carbs which made the dry eyes go away and reducing them which made them immediately come back. This established unequivocally that it was a glucose deficiency alone that caused the dry eyes.
Rebecca reports similar symptoms in herself and her low carb friends.
This is also a well-known symptom during starvation. As a review cited by LynMarie Daye (and referenced by CarbSane in the comments) notes,
Since hepatic glycogen stores are depleted within 24 h of fasting, blood glucose concentrations are maintained thereafter entirely through gluconeogenesis. Gluconeogenesis is mainly dependent on protein breakdown (a small amount comes from the glycerol released during lipolysis) and it thus results in protein wasting. It is the effects of protein malnutrition that lead to the eventual lack of ability to cough properly and keep the airways clear, in turn leading to pneumonia and death during prolonged starvation; hypoglycaemia does not occur. [1]
Another common symptom of very low carb diets is constipation. This is often attributed to lack of fiber, but I am skeptical. I will get to the various possible causes of constipation in a future post, but for now I’ll just point out that a deficiency of gastrointestinal mucus would create a dry colon and cause constipation.
What connects a zero-carb diet to dry eyes, dry mouth, dry airways, and dry gastrointestinal tract?
Tears, saliva, and mucus of the sinuses, airways, and gastrointestinal tract are all comprised substantially of glycoproteins called mucins. Mucins are primarily composed of sugar; they typically have a number of large sugar chains bound to a protein backbone.
For instance, the main mucin of the gastrointestinal tract, MUC2, is composed of a dimerized protein – each protein weighing 600,000 Daltons individually, so 1.2 million Daltons for the pair – plus about 4 million Daltons of sugar, for a total mass of 5 million Daltons. In the mucus, these large molecules become cross-linked to form “enormous net-like covalent polymers.” (source)
If, for whatever reason, mucin production were halted for lack of glucose, we would have no tears, no saliva and no gastrointestinal or airway mucus.
Mucin Deficiency Causes Cancer
There is a strong association between mucus deficiency and gastrointestinal cancers.
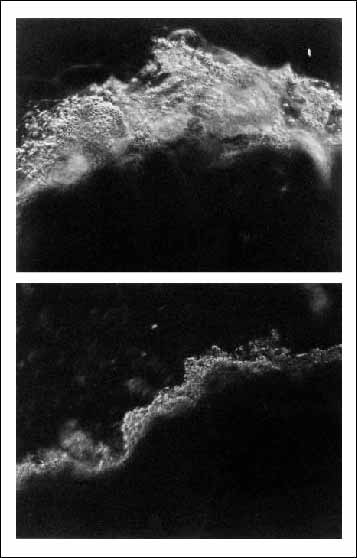
H. pylori is the strongest known risk factor for stomach cancer. [2] H. pylori infection is found in about 80% of gastric cancers. [3] One reason H. pylori promotes stomach cancer so strongly may be that it diminishes mucus in the stomach, as this photo shows:
Top: Normal stomach mucosa. Bottom: Stomach mucosa in an H. pylori infected person.
Scientists have created mice who lack genes for the main digestive tract mucins. These give us direct evidence for the effects on cancer of mucin deficiency.
Experiments in Muc1 knockout mice and mice with Muc1 knockdown have shown that under Helicobacter infection, mice deficient in Muc1 develop far more cancer-promoting inflammation than normal mice. [4]
The main mucin of the intestine is Muc2. The group of Leonard Augenlicht of the Albert Einstein Cancer Center in New York has studied mice lacking Muc2. They develop colorectal cancer. [5]
Tracing backward one step toward the source of mucin deficiency, the sugars in mucin are built from smaller pieces called O-glycans. It has been shown that mice that are deficient in O-glycans are prone to colorectal cancer: “C3GnT-deficient mice displayed a discrete, colon-specific reduction in Muc2 protein and increased permeability of the intestinal barrier. Moreover, these mice were highly susceptible to experimental triggers of colitis and colorectal adenocarcinoma.” [6]
Nutrient Deficiencies Can Also Play a Role
Some micronutrients are required for mucin production – notably vitamin D. [7, 8] Poland is fairly far north, and many of the Optimal Dieters could have been low in vitamin D.
Other important micronutrients for cancer prevention are iodine and selenium. Poland in particular had the lowest iodine intake and among the highest stomach cancer death rates in Europe. After Poland in 1996 began a program of mandatory iodine prophylaxis, stomach cancer rates fell:
In Krakow the standardized incidence ratio of stomach cancer for men decreased from 19.1 per 100,000 to 15.7 per 100,000, and for women from 8.3 per 100,000 to 5.9 per 100,000 in the years 1992-2004. A significant decline of average rate of decrease was observed in men and women (2.3% and 4.0% per year respectively). [9]
So among the Polish Optimal Dieters, the elevated gastrointestinal cancer risk caused by mucin deficiency may have been aggravated by iodine and sunlight deficiencies.
Conclusion
A healthy diet should be robust to faults. The Optimal Diet is not robust to glucose deficiency.
There’s good reason to suspect that at least some of the Optimal Dieters developed mucin deficiencies as a result of the body’s effort to conserve glucose and protein. This would have substantially elevated risk of gastrointestinal cancers. Thus, it’s not a great surprise that many Optimal Dieters have been coming down with GI cancers after 15-20 years on the diet.
We recommend a carb plus protein intake of at least 600 calories per day to avoid possible glucose deficiency. It’s plausible that a zero-carb diet that included at least 600 calories per day protein for gluconeogenesis would not elevate gastrointestinal cancer risks as much as the Optimal Diet. But why be the guinea pig who tests this idea? Your body needs some glucose, and it’s surely less stressful on the body to supply some glucose, rather than forcing the body to manufacture glucose from protein.
Fasting and low-carb ketogenic diets are therapeutic for various conditions. But anyone on a fast or ketogenic diet should carefully monitor eyes and mouth for signs of decreased saliva or tear production. If there is a sign of dry eyes or dry mouth, the fast should be interrupted to eat some glucose/starch. Rice is a good source. The concern is not only cancer in 15 years; a healthy mucosal barrier is also essential to protect the gut and airways against pathogens.
Related Posts
Other posts in this series:
- Dangers of Zero-Carb Diets, I: Can There Be a Carbohydrate Deficiency? Nov 10, 2010.
- Danger of Zero-Carb Diets III: Scurvy Nov 20, 2010.
- Dangers of Zero-Carb Diets, IV: Kidney Stones Nov 23, 2010.
References
[1] Sonksen P, Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth. 2000 Jul;85(1):69-79. http://pmid.us/10927996.
[2] Peek RM Jr, Crabtree JE. Helicobacter infection and gastric neoplasia. J Pathol. 2006 Jan;208(2):233-48. http://pmid.us/16362989.
[3] Bornschein J et al. H. pylori Infection Is a Key Risk Factor for Proximal Gastric Cancer. Dig Dis Sci. 2010 Jul 29. [Epub ahead of print] http://pmid.us/20668939.
[4] Guang W et al. Muc1 cell surface mucin attenuates epithelial inflammation in response to a common mucosal pathogen. J Biol Chem. 2010 Jul 2;285(27):20547-57. http://pmid.us/20430889.
[5] Velcich A et al. Colorectal cancer in mice genetically deficient in the mucin Muc2. Science. 2002 Mar 1;295(5560):1726-9. http://pmid.us/11872843.
[6] An G et al. Increased susceptibility to colitis and colorectal tumors in mice lacking core 3-derived O-glycans. J Exp Med. 2007 Jun 11;204(6):1417-29. http://pmid.us/17517967.
[7] Paz HB et al. The role of calcium in mucin packaging within goblet cells. Exp Eye Res. 2003 Jul;77(1):69-75. http://pmid.us/12823989.
[8] Schmidt DR, Mangelsdorf DJ. Nuclear receptors of the enteric tract: guarding the frontier. Nutr Rev. 2008 Oct;66(10 Suppl 2):S88-97. http://pmid.us/18844851.
[9] Go?kowski F et al. Iodine prophylaxis–the protective factor against stomach cancer in iodine deficient areas. Eur J Nutr. 2007 Aug;46(5):251-6. http://pmid.us/17497074.











Hi Devi,
Yes, coconut oil is among the harder things to digest. 4-5 tbsp is enough if you’re just trying for some antibiotic effects in the gut.
Candida is concentrated in the colon. Since glucose feeds both yeast and the immune system, you want to give as much as possible to the immune system and as little as possible to the yeast. That calls for digestible starches that are broken down by human enzymes and absorbed as glucose in the small intestine. Resistant starch reaches the colon and can feed yeast.
According to this, cooking at 100 C or less may make cranberries even more helpful: http://pmid.us/19241540.
Paul,
I guess what I was trying to say that it is hard for the average person to find high quality high fat animal products that one would want to consume.
Many of the products out there don’t have much fat or the type of fat we want — ie chicken and most fish — even a lot of fat from pork seems to be too omega 6 heavy (pigs that are not corn fed).
The only meat id feel happy consuming a lot of fat from would be grass fed cows– and even then, most of the meat is pretty low in fat so you would have to discard a lot of the protein to make sure you don’t eat too much (of the protein). Do you know other sources of high quality fat that I can use that aren’t the typical butter or coconut or palm oils?
This is the type of stuff I’m trying to resolve because I don’t think it’s smart to have a lot of olive oil or butter for the reasons you listed in the choline post– and I also dont like to waste good protein (because most grass fed products are low in fat).
Hi Aaron,
Yes, I see your issue now.
The “Paleo” solution would be to eat fat-rich parts of the grass-fed animals like brains and bone marrow. Of course, that could be very expensive.
I think supermarket meats are mostly OK, since the animals largely detoxify their food and we can handle the rest. We tend to concentrate on beef and salmon, since they are naturally low in omega-6 even when fed bad diets.
Our Asian supermarket sells beef fat slabs, which we use for cooking. That’s better than plant oils as far as nutritional value.
Hi Paul.
I think gastrointestinal cancer of Optimal Dieters may be due to high red meat consumption:
http://medicine.journalfeeds.com/gastroenterology-hepatology/am-j-gastroenterol/meat-consumption-and-risk-of-esophageal-and-gastric-cancer-in-a-large-prospective-study/20101028/
http://news.bbc.co.uk/2/hi/health/4662934.stm
“In the latest study the same Dunn team examined cells from the lining of the colon taken from healthy volunteers eating different diets.
They found higher levels of DNA damage in the cells taken from people eating red meat.
Work by the Open University team suggests the reason could be the presence of substances called N-nitrosocompounds, which form in the large bowel after eating red meat.”
Hi Kratos,
The trouble with that explanation is that Optimal Dieters eat less protein than other Poles, so they probably eat less red meat, not more.
So ODers should have lower risk if that was the explanation.
A further issue is that the problem seems to be with processed meats, not red meats.
The study blames N-nitroso compounds, but these are formed in cured meats (treated with nitrites) that are cooked at high temperatures. So we’re looking at toxins that aren’t present in natural red meats.
Other studies have also found that all the cancer danger comes from processed meats, not red meats.
Hi Paul,
Re. Digestion of coconut oil:
I was pleased to read in one of your comments above, “…coconut oil is among the harder things to digest.”; pleased because it jibes with my experience, and because I’ve been meaning to ask you about it.
I’ve been trying hard, but find myself unable to get the daily six ounces (on the ketogenic variant of your diet) down my gullet. If I take any substantial amount with breakfast or lunch, it lives with me for the rest of the day (repeating/burping/tasting the coconut oil). At the next meal, my body says, “Nope, you’re gonna feel sick if you eat this”, and I find I’ve been obeying.
So, if coconut oil is difficult to digest, I’m assuming it would be even more difficult for someone with low thyroid and leaky gut, and their attendant digestive issues? Could excess difficulty digesting coconut oil indicate a general problem with bile production/fat digestion? (I don’t seem to have problems with other recommended fats). Any tips to help digest it, so that I can take the recommended dose? (i.e. digestive enzymes, betaine-hcl, bile salts, etc.???).
p.s. I’m currently using Nutiva brand; have also used Orphee.
Sammy, I’m having the same problem with coconut oil. I took 2T/day for two months, but the taste and smell of it is distasteful and distressing and seems to stay with me all day no matter how I take it.
In fact, like you, I’m listening to my body and stopped it yesterday. It hasn’t helped my bloating and gas problems and I can’t help thinking that taking something that produces such a violent reaction can’t be doing me much good.
Otherwise, I’m following Paul’s diet and supplement suggestions with no problem.
Aaron, in the US, at least, there are a number of grass-fed meat vendors (e.g. Slankers) that sell bags of fat. When I cook meat I throw a few tablespoons of beef fat into the pan. It renders as it cooks and I end up eating it with a spoon along with the meat. You can also order grass-fed tallow but I prefer the raw fat.
Sammy and Erp, I feel the same way about coconut oil. It didn’t make me nauseous and it didn’t cause any digestive problems. After I finished about half of the first bottle I bought, there was just a intense intuitive feeling, as if my body was telling me, “Do not eat that, it’s bad.” I can’t remember any other food that ever affected me that way.
Hi Paul and All,
erp and Robert Sacks, thanks very much for your replies and commiseration re. coconut oil.
To avoid confusion for Paul or anyone else reading my post, I should clarify that I don’t find the “taste and smell distasteful and distressing”, nor do I feel that my body is telling me, “Do not eat that, it’s bad.”
For me it’s simply that I seem to have challenges digesting it, and I am looking for ways to overcome those challenges so that I am able to consume a therapeutic dose each day.
Sammy, sorry to have misinterpreted your comment.
However, I do feel that if after a reasonable amount time, one’s body is not reacting well to something, it’s probably right to stop it until a solution or explanation can be found. BTW – my reaction to coconut isn’t new. It’s one of only two foods I can’t tolerate — the other being okra. :-{
Hi Sammy,
Fat in general is hard to digest, because the same enzymes that digest dietary fats can digest human cell membranes, so there are a lot of moving parts that have to be coordinated for fat digestion to occur safely. In people with small bowel diseases, this coordination often fails and fats are troublesome.
Then the medium-chain fats in coconut oil are even harder to digest, because they are damaging to cell membranes and have to be routed to the liver for disposal. So one more thing that can go wrong, or bring fat-digesting enzymes into the wrong place.
I think if they’re giving you trouble you should cut them down. Maybe later they’ll be more tolerable.
I have to agree with CO giving GI distress. I did mess up my portion sizes somewhat in the beginning but it is hard to consistently maintain 12 tbsp per day.
I can also relate to the “do not eat” feeling where even the thought of another spoonful turns my stomach.
Out of interest, I also get a similar GI distress with too much lard via pork belly. If I eat too much that’s very fatty I feel quesy and my stomach soon removes it!
Beef dripping not so much, but that does give me a very “full” feeling stomach-wise.
Butter seems to be the fat I can tolerate best in large doses; it’s easy for me to eat 100g at a time, especially melted. Maybe because it’s not all fat with the milk-proteins?
I think it’s always easiest for digestion to eat fat with other foods – e.g. in mashed potatoes or the like.
For someone who can’t tolerate dairy, getting the recommended levels of macronutrients is a challenge. I do use coconut milk in coffee and recipes and cook with coconut oil (not a big fan of eating it straight) but the main source of fat is fatty meat.
However, even the fattiest meat carries a lot of protein along. It seems like the best method to address this would be to stay at the higher protein levels but reduce the carbs, perhaps by carb cycling. I am trying that right after Thanksgiving. I’ll be near zero carb during the week and then eat high starch (safe starches, not carby crap) on the weekend, with reduced protein.
Paul,
I have also started to experience a little nausea and general feeling of yuckiness when taking coconut oil by spoon. This wasn’t present before but now that I have upped intake (usually two tablespoons a day) I have noticed it. Do you see this as evidence of some sort of toxicity that is building up? Why would so many people have this experience in the absence of toxicity?
Hi Todd,
I don’t know. It’s conceivable there could be a buildup of lauric acid in the body and that that induces distastefulness. However, Kitavans and Tokelau islanders have significant amounts of lauric acid in the body, but they still eat a lot of coconut milk – in fact it’s their largest dietary fat. But then maybe that’s what’s available.
Apart from assisting with fasts, there isn’t much need for coconut oil – I recommend it for antimicrobial actions in the gut, for raising HDL, and for ketosis – but if it’s distasteful, that seems like a good reason not to eat it.
Here are some thoughts on coconut digestion — I had a bit of trouble with it when I first started consuming it in high quantities, but I seem to have adjusted. I also take a high lipase plant-based digestive enzyme supplement before fatty meals, which seems to help. I now on occasion will drink whole cans of coconut milk without much trouble.
Taking coconut oil after a meal of solid food should help, since it will close the pyloric sphincter and greatly slow down the digestive process. The pyloric sphincter should then open every once in a while to allow bits of food into the small intestine, where the fats get emulsified and absorbed. Without the solid meal, the coconut oil may just pass immediately into your small intestine in one big bolus. Hilarity ensues.
As coconut oil is a pure fat, it needs to be emulsified by bile salts, which are injected from your gall bladder into your duodenum. If your gall bladder is not up to snuff, you could have problems, because emulsification is a prerequisite to lipase activity and fatty acid absorption. Un-emulsified fats end up in the large intestine, where they can feed bacteria (producing gas and bloating) and produce fatty stools (steatorrhea).
One alternative is to try coconut milk instead, since it is already emulsified and should work better for someone with a spotty gall bladder or insufficient hepatic bile production. If you have an easier time digesting emulsified fats like butter, cheese and eggs, your gall bladder could be implicated. Good luck!
Thanks Greg!
I second Greg’s recommendations. I was able to ingest coconut oil by the spoonful in the summmer (it was in the melted form–I live in Greece), but now that it’s in the congealed form, I find it a little nauseating. Although I still have some coconut oil by spoon, I also drink coconut cream as I would a glass of milk with a meal. Very easy, very satiating without the nausea. If some feel the carb content of the cream is too high for them (it really isn’t), then there are ways of fermenting the coconut cream with kefir grains to get rid of the carbs.
Another great way of getting a ton of coconut oil/cream is through stir fries/curries. I cook these with a ton of coconut oil and mix in a box of coconut cream at the end–guaranteed to turn a ketostix pink!
So, the recommendation to mix with foods is a great one, IMO. I’m fasting today and will have a box (250 mL) of coconut cream for lunch–makes a 24 hours fast super easy (I do one weekly).
I’d like to try digestive plant enzyme (lipase) to see if the help me with fats digestion.
Paul do you think lipase can be harmful for the gut?
You before said that fat-digesting enzymes into the wrong place are not good.
Hi Kratos,
If you do try lipase, I would break the plastic pill covering and mix them in with your fatty food before eating. And try it in very small doses.
The trouble is they can digest your cell membranes. So personally, I think there may be more to lose than to gain. But as a diagnostic experiment, to see lack of pancreatic enzymes may be the problem, I don’t mind it. But I don’t think you should do it routinely.
Hi, thanks for reply.
Can I ask why do you think lipase can digest cell membranes? If so also proteases should be dangerous.
I know lipase is present in high doses in raw butter.
Hi Kratos,
In a healthy gut lipase wouldn’t do much harm, because there is a sound mucus barrier and good bile flow and micellation of fats so the lipase congregates with the bile and eaten fats. But with a healthy gut fat digestion would be fine and you wouldn’t need lipase. If you are having trouble digesting fats, then the situation may be different — maybe mucus deficiencies because of infections or dehydration, maybe lack of bile, maybe other issues — and these may make the lipase dangerous.
The cell membranes prevent proteases from entering the cells, so at most they would cleave some membrane proteins. So proteases aren’t as dangerous.
One web site I found mentioned this: “Doses above 6000 Units of lipase per kilogram meal have been associated with colonic stricture: the ascending colon becomes blocked, sometimes requiring a surgical solution. This has occurred predominantly in young males during the warmest summer months, and may be associated with dehydration.”
There are some conditions like cystic fibrosis where lipase supplementation is needed. But I think most people should be cautious about it.
I don’t want to say categorically that you shouldn’t experiment. It might help – try it and see. But use low doses and be aware of potential dangers. Take it only with dietary fat.
Middle school biology fans will remember the lipid bi-layer, which forms our cell membranes. This is why lipase can eat through them. Lipase is one of the nasty things that will digest your insides if you ever get acute pancreatitis. A gall stone can block the pancreatic duct, causing enzymes to back up in the exocrine pancreas and spill out into neighboring tissue. A healthy pancreas will dump lipase directly into the lumen of the small intestine while keeping it away from your bloodstream and internal organs.
So be careful with it, probably fine for a short term experiment, but discontinue immediately if it is having any negative effects. It may be necessary to try different brands before you find one that works and that you tolerate, and cycling is probably also going to be much better than cronic use.
Hi Paul,
I have a question for you.I have access to fresh beef suet from a butcher.Could these hard chunky pieces be used for getting the recommended levels of macro nutrient? Or are they too high in saturated fat?
They contain only 1-2g protein per 100 grams.
Thanks.
Hi Nada,
Beef suet is an excellent source of fat. It’s great as a cooking fat. The low omega-6 levels are an advantage.
Best, Paul
Thanks for clarifying Paul and Greg.
I’m using since 3 months ago a broad spectrum enzyyme product that does contains 200 FCCLU (1700 LU) of lipase.
There shouldn’t be too much lipase but do you think it’s better to discontinue it after some time of use?
Hi Kratos,
Well, in general I would recommend enzyme products that don’t contain lipase.
I guess the question is: do you think the lipase is helping you? You have to decide.
You might want to break a capsule and let the enzymes sit on your tongue for a moment before adding food, so you have a sense of how harsh it is to your tissue. Also switch it off and on with a product that doesn’t have lipase. Is there a difference?
Either way, keep the lipase dose low.
This is really an interesting post.
Did anyone here with dry eyes also notised an odd kind of sore nosetip? It seems to come and go with the eye-problem.
I´ll try the vitamin C tips, so thank you all.
Hi Paul, I read your post about constipation and I started eating 3 brazil nuts every morning (for selenium).
The next 3 days I have had perfectly formed BM every morning for the first time from being low carb!! (1+ years)
Now I don’t know if it is due to selenium or to fiber (but I don’t think 0.7g of fiber in 10g of nuts can do the trick). I used to eat a lot of vegetables but never worked.
Why do you think selenium and gluthatione can lessen constipation? I have never read such thing.
Have you also suffered of constipation during low carb?
Hi Kratos,
My wife had constipation 5 years ago, so I researched causes. Glutathione/selenium deficiency is a known cause. I never had it myself.
Glad you’re feeling better!
Best, Paul
Thanks.
But why do you think selenium/gluthatione deficience can cause constipation?
Did selenium worked also for you wife?
I don’t know the mechanism. I’ll have to research it. My wife’s constipation was caused by hypothyroidism.
Dr Jaminet, earlier you referred to a
” comment about a paper showing that people who DON’T develop IgA antibodies to wheat have worse health outcomes than those who do. The antibodies help clear the wheat toxins, which would otherwise build up.’
This is very interesting to me, as my tests were ‘clear’ except for a very small antibody “reaction to somethign” and the GI surgeon suggested “more fiber” !!! However my own experiment with a strict wheat-free diet has proven that I have a wheat allergy of some kind – it’s very obvious, when I eat it, I have GI issues in response. But both the specialist and my doctor were skeptical.
So I’d be curious to see what sort of study this was – was it simply non-diagnosis resulting in continued wheat consumption? Do you have any further links or information to hand?
I find it quite absurd that I’ve effectively had to self-diagnose a potentially life-threatening condition (quite apart from the chronic effects that pain, bloating and so on were having on my wellbeing!)
Once again I’m impressed by the quality of scholarship on your blog. I look forward to reading the book.
Helen, you’re not alone with having to self-diagnose a debilitating condition. So many of us had to do that. For years I saw GI specialists and had many tests, but my gluten/casein intolerance went undiagnosed until a friend suggested I get tested at Entero Lab, which does specialized testing. I could have saved myself years of pain, suffering, time, and money if I’d been diagnosed earlier. About a year before my Entero Lab testing, one GI specialist told me it was “a coincidence” that I felt much better when I was on a low-carb diet, and that the reason I had GI issues was because I had a “sensitive stomach” and was “stressed,” – and to avoid spicy food!
Hi Helen,
This paper: http://www.ncbi.nlm.nih.gov/pubmed/11720003 discusses the consequences of IgA deficiency for wheat tolerance and disease. I can do a blog post on it if you’d like.
It’s scandalous that your doctors don’t know the dangers of wheat! The medical literature is full of discussions of celiac disease and other wheat-derived autoimmune diseases. Many doctors assume that if you don’t test positive for antibodies then you don’t have these diseases, but that is a mistake, as we discuss in the book.
As suzan says, unfortunately contemporary medicine is no good at chronic illness. So we have to diagnose and treat ourselves. That’s why this blog came into existence – to help others learn about and follow the path it took us years to trailblaze!
Best, Paul
Paul,
Any thoughts on antibiotic use for acute infections? I’m struggling with a sinus infection that came on at the end of a cold I thought I was getting over. I feel terrible and am about to throw in the towel and head to the doctor. I know the standard treatment is antibiotics, sometimes with a course of steroids – something I’m inclined to avoid if at all possible.
I used to get several sinus infections every winter before I went low-carb paleo, which seemed to cure them for a while. They’ve recently started happening again, which is one of the reasons I was drawn to your blog. Anyway, I’m hoping that my recent switch to the Perfect Health Diet will make these sort of infections a thing of the past, but what to do in the meantime?
Hi suzan, are you sure your illness were due to casein and gluten?
If you are doing a low carb diet without gluten free starches you can’t be sure.
I tell you this because I know a lot of people who healed their disease only going low carb without eliminating gluten.
Hi Eric,
I support the use of antibiotics for acute bacterial infections.
Sinus infections can be caused by fungal or viral infections too – something to be aware of. Recurrent sinusitis is more likely to be fungal than occasional acute conditions.
Extra vitamin D, vitamin C, and glutathione or its precursors (like N-acetylcysteine) are highly desirable during infections.
“Feed a fever, starve a cold” is good advice – it’s basically feed extracellular infections (provide glucose for immune activity) and starve intracellular infections (promote autophagy).
With good diet and supplements infections should become rare. I haven’t had an acute infection in years. Once or twice I’ve felt like I was dealing with one, but it didn’t hinder me from doing anything, didn’t produce overt symptoms, and my wife didn’t know unless I told her. I think the body can deal with most infections effectively if you’re sufficiently healthy and well-nourished.
Best, Paul
Back in 2007, I asked my MD at the time to order the GI-2 test from Diagnos-Techs labs. This test kit requires stool samples, as well as saliva samples. It tests for the presence of dysbiosis, various parasites, inflammation, etc.
http://www.diagnostechs.com/TestPanels/GIHealthPanels.aspx
One of test parameters is Gliadin Ab, SIgA. My score was 9, negative. [borderline: 13-15, positive: >15]. When my MD went over the test results, he did not mention gluten being a problem for me. I was negative after all, right?
Wrong. I consulted with a different practitioner a few weeks later to get a second opinion since I had the feeling I was not in good hands with this MD’s advice.
This second practitioner reviewed the test results, and told me I needed to go gluten free. He went on to explain that my Total Intestinal SIgA score was rock bottom, at 33, with normal being 400-880.
He said that even with poor antibody production (low Total Intestinal SIgA), I managed a Gliadin Ab, SIgA score of 9. He said if my antibody production was strong, I surely would have a much higher Gliadin score, and a very strong positive.
He told me this pattern is quite common. If practitioners don’t take the time to learn how to interpret test results with the MDs at the lab (it’s free!), patients will be ill advised & told there is no gluten problem.
Since then, several of my friends and/or their children have taken this test to look for gut problems. Nearly all of them have shown the same pattern, very low Total Intestinal SIgA, and then negative, borderline positive, or positive Gliadin Ab, SIgA. All have greatly benefited from giving up gluten. Many admit they needed to see it on paper in order to make the change.
There are other parameters on the test which are dependent on antibody production. I’m not confident that many practitioners understand this.
Just sharing!
Thanks, Michelle! That’s a very helpful story.
I have some sympathy for the doctors, since biology is so complicated it’s hard to remember everything. But that only means that it’s very important for patients to push and keep looking for answers and for doctors who can help. You’re a model patient! Independent and persistent.
Thanks for the link to the testing service.
Thank you, and you’re welcome. 🙂
With regards to sinus infections (or throat, ears, and bad breath) I highly recommend BlisK12 – my husband had a nasty smelling sinus / post nasal drip and it fixed it. I had bad breath and it fixed that too.
It is a mouth and throat probiotic – very effective.
I did a post on it, has links and where to buy:
http://paleozonenutrition.wordpress.com/2010/11/20/bad-breath-frequent-strep-throat-ear-infections-try-mouth-and-throat-probiotics/
Thanks Julianne!
I noticed your blog post on that a few weeks ago, and have been planning to post about it. I hadn’t heard of mouth probiotics before your post!
My only concern is a negative customer review at Amazon: http://www.amazon.com/Life-Extension-Advanced-vegetarian-lozenges/dp/B002R3CGHI/
Best, Paul
Wow,
I hadn’t seen that, interesting. It is certainly not our experience – neither of us experienced any gum issues or negative side effects.
I only used it a couple of times – for the first month and then again a few months later. I haven’t needed it since it killed my bad breath a couple of years ago.
It would be interesting to see if Professor John Tagg (who developed it) has had any negative side effects reported? It would be interesting to see how he responds to this person’s negative experience.
Yes, I was excited when I read your post, it made a lot of sense, oral probiotics, how smart. But it would be nice to get a bigger sample and make sure it’s generally beneficial. One complaint could just be a coincidence … but I don’t want to ignore it either.
Paul, what dosage of glutathione do you recommend. I’ve had a sinus problem for 15 years and numerous ent exams, endoscopies have shown nothing. The pressure is painful and the constant headache is a real headache.
Hi erp – You can take up to ~3 grams of N-acetylcysteine or glutathione per day, but you might start with 500 mg or 1 g NAC, 2 g vitamin C, and 4,000 IU vitamin D3.
Yes, I was tested for both gluten and casein intolerance by http://www.enterolab.com, and was positive for both. I’ve been on and off low carbing for years, so not consistent with low-carb until last year. I’ve had gastro issues most of my adult life. (my first 20 years of life I had recurring colds and viruses, then for the next 30+years, gastro issues) I also had a DNA test from Entero Lab and both my parents carried the gene for Celiac disease, though neither had were diagnosed with it.
Thanks Paul.