Mario Renato Iwakura’s guest series on the place of iodine and selenium supplementation in treatment of hypothyroidism continues. This is part 2. Thank you Mario! – Paul
UPDATE November 2023: Since this article was written, PHD recommendations for iodine have become firm. We recommend consistent daily supplementation in the range of 150 to 225 micrograms (not milligrams) per day, plus frequent seafood consumption. The supplementation (a) ensures a healthful supply of iodine and (b) accustoms the thyroid to the presence of iodine which minimizes the risk of thyroid injury from intake of a large amount of iodine at once, possibly at a time of selenium deficiency, for example from an all-you-can-eat crab buffet. Supplementation of >1 mg high doses of iodine carries a high risk of thyroid injury, making some parts of the thyroid hypothyroid and possibly also creating nodules with hyperthyroid activity. … Although our recommendations are not in line with Mario’s, nevertheless Mario’s article is fascinating, and a few people have reported benefit from high-dose iodine. Please read his article and judge for yourself! Best, Paul
In Part I (Iodine and Hashimoto’s Thyroiditis, Part I, May 24, 2011) we looked at evidence from animal studies that iodine is dangerous to the thyroid only when selenium is deficient or in excess, and that optimizing selenium status allows the thyroid to tolerate a wide range of iodine intakes. In fact, there were some hints (such as an improved CD4+/CD8+ T cell ratio) that high iodine, if coupled with optimal selenium, might actually diminish autoimmunity.
If that holds in humans too, we should expect that populations with healthy selenium intakes should see a low incidence of thyroid disease and no effect from iodine intake on the incidence of Hashimoto’s thyroiditis. Is that the case?
Korean Study
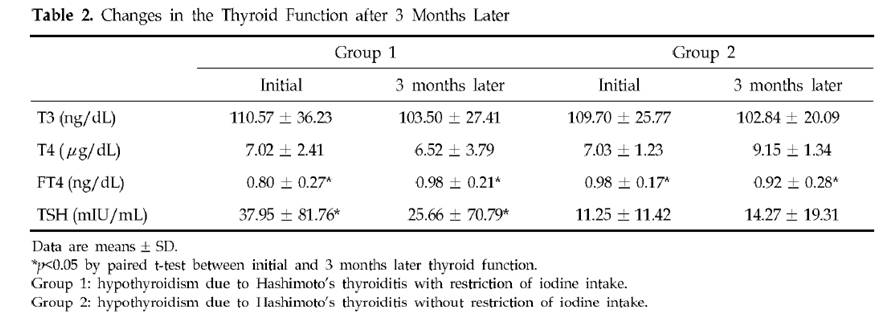
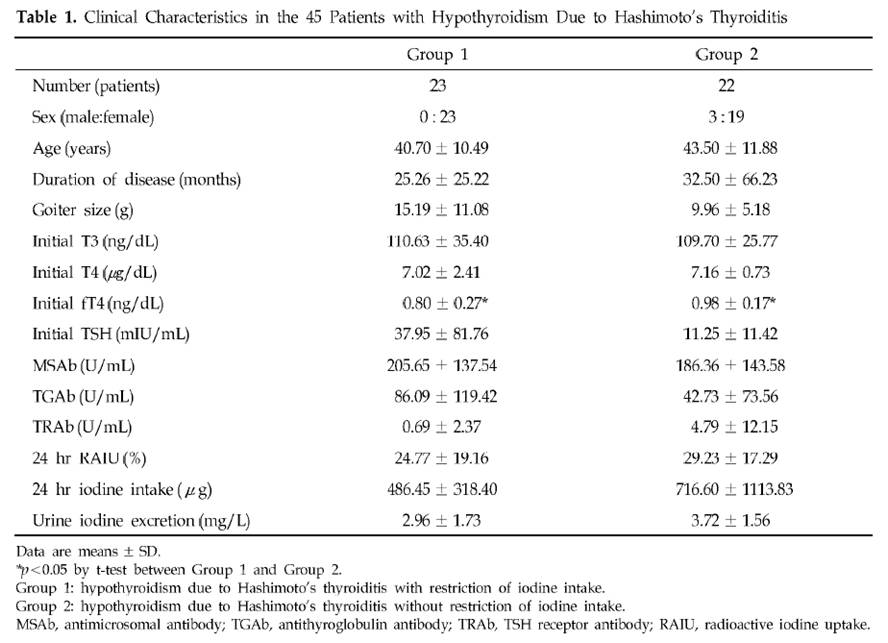
Dr. K [1] quotes a Korean study [3] of Hashimoto’s patients. Half restricted iodine intake to less than 100 mcg/day, the other half ate their normal seaweed and iodine. Of the 23 patients who restricted iodine, 18 (78%) became euthyroid in the sense of having TSH below 4.43 mIU/L, while only 10 (46%) of the 22 that did not restrict iodine became euthyroid. There was no measurement of symptoms at all, and no report of thyroid antibody titers after iodine restriction, so we don’t know if the iodine restriction relieved the underlying autoimmune disorder.
The selection of subjects for the two groups was odd. Group 1, the iodine restricted patients, had an extremely wide range of starting TSH, averaging 38 mIU/L but with a standard deviation of 82 mIU/L. Since all subjects began with TSH above 5 mIU/L, it’s clear that many of the Group 1 members had TSH near 5 and others had TSH well over 100 mIU/L. In comparison, Group 2, the controls, averaged a TSH of 11 mIU/L with a standard deviation of 11 mIU/L – less than 1/7 the standard deviation of Group 1. Few Group 2 members had a TSH above 30.
Table 2 presents the results. Mean TSH in Group 1 was reduced a little, but it did not even come close to normal. Since 78.3% of Group 1 had TSH below 4.43 mIU/L after 3 months, the other 21.7% had to have averaged a TSH above 102.2 mIU/L at the conclusion of the study. The standard deviation of Group 1 TSH at the end of 3 months of iodine restriciton was 71 mIU/L.
Meanwhile, Group 2 members still had a much lower standard deviation at the end of the study: 19 mIU/L.
A conclusion of this study was that “the initial serum TSH concentration was significantly lower in the recovered patients than in the non-recovered patients, which suggests that the possibility of recovvery is increasingly rare as the initial hypothyroidism becomes more severe.” Since Group 1 originally had a much larger fraction of members with very low TSH than Group 2 (plus a few with extremely high TSH to raise the average TSH), and the definition of recovery was a reduction of TSH to 4.43, perhaps it is not surprising that a higher fraction of Group 1 recovered.
Further calling into question the conclusion that lower iodine intake is beneficial is another observation. Looking at Table 1, we see that Group 2 (controls) had, at baseline, much higher iodine intake and higher urinary iodine excretion. Despite this, goiter size, TSH, antimicrosomal (MSAb) and antithyroglobulin (TGAb) antibodies were all lower!
A Japanese Study
A similar study with similar results was done in Japan [4].
In Asia, high iodine intake is due to high consumption of seaweed. Seaweed is high in naturally produced bromine compounds [5][6][7], arsenic [9][12][13], and mercury [9], and can accumulate radioactive iodine [8][9][10][11]. All these substances are known to interfere with thyroid function.
Bromide levels in urine in Asia are very high and are associated with seaweed consumption [6][7]. Values of 5 to 8.1 mg/l have been observed among Japanese, and 8 to 12 mg/l among Koreans.
It is quite possible that any benefits from “iodine restriction,” i.e. seaweed restriction, were due to reduced intake of bromine, arsenic, mercury, and radioactive iodine.
A China Study
Dr. Kharrazian [2] cites a study done in China [14] comparing three different areas: one with iodine deficiency (Panshan), another where iodine is more than adequate (Zhangwu) and a third where iodine is excessive (Huanghua). More than adequate and excessive iodine was associated with increased risk for subclinical and overt hypothyroidism.
But, another study [15], done in the same regions, showed that, coincidentally, Huanghua, the region with excessive iodine, and Zhangwu, the region with more than adequate iodine, had lower median serum selenium concentrations than Panshan, where iodine was deficient. Blood selenium concentrations were 83.2, 89.1 and 91.4 microg/L, respectively. So iodine consumption was inversely related to selenium consumption. Was it lower iodine, or higher selenium, that was beneficial?
TPOAb antibody levels were inversely associated with selenium levels. Patients with the highest TPOAb antibodies (>600 UI/ml) had lower selenium levels than patients with moderate and lower TPOAb antibodies (respectively 83.6, 95.6 and 92.9 UI/ml). [15]
Studies from Brazil, Sri Lanka, Turkey, and Greece
Dr K also cites a rise in Hashimoto’s incidence in Brazil, Sri Lanka, Turkey and Greece after salt iodinization began. Are these countries deficient in selenium? Well, lets see:
Brazil: The study was done in São Paulo, a city with a large Brazilian-Japanese population. Brazilian-Japanese have significant lower levels of Se than Japanese living in Japan [16].
Greece: Selenium status is one of the lowest of the Europe [17].
Turkey: Selenium status of Turkish children is found to be unusually low, only 65 ng/ml in boys and 71 ng/ml in girls [18]. Turkey is characterized by widespread iodine deficiency and marginal selenium deficiency [19].
Sri Lanka: Significant parts of the Sri Lankan female population may be selenium deficient [20].
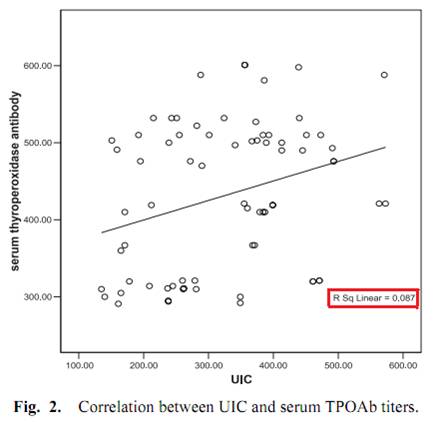
One study, done in Egypt, measured iodine excretation in urine and its relation with thyroid peroxidase antibody (TPOAb) [21]. Although the abstract said that a significant correlation was found, this is far from reality, as we can see from Fig. 2.
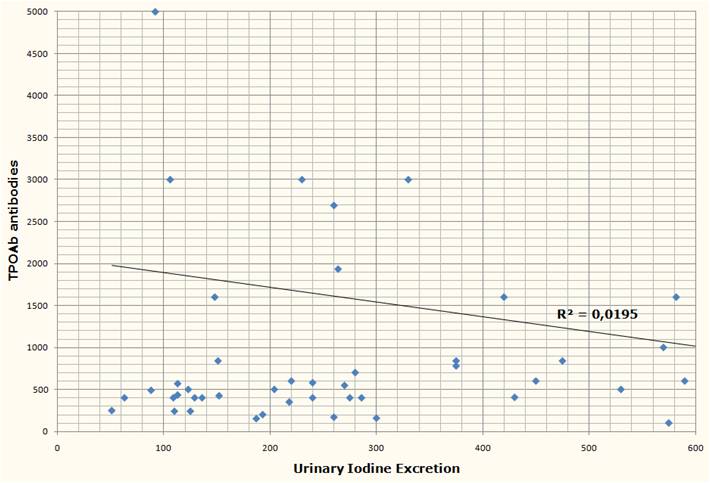
Another study from Brazil [2] measured urinary iodine excretation and serum TPOAb and TgAb antibodies from 39 subjects with Hashimoto’s, none of whom were receiving treatment at the time of the study. Both antibody titers had no obvious correlation with urinary iodine.
Two discordant epidemiological studies
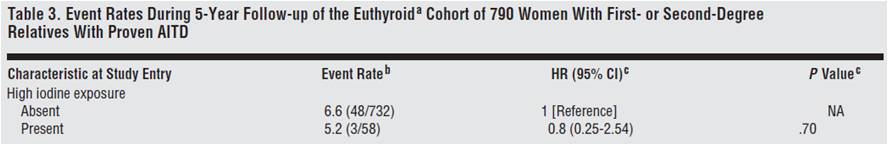
From the Netherlands, we have a prospective observational study looking at whether the female relatives of 790 autoimmune thyroid disease patients would progress to overt hypothyroidism or hyperthyroidism [22].
Although the relationship was not considered statistically significant, they found that women with high iodine intake (assessed through questionnaires) were 20% less likely to develop thyroid disorders.
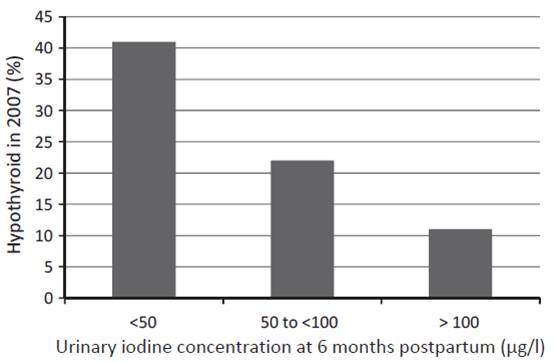
Another study from western Australia (a region that has previously been shown to be iodine replete) measured urinary iodine concentration (UIC) of 98 women at 6 months postpartum and checked their thyroid status both postpartum and 12 years later [23]. UIC at 6 months postpartum predicted both postpartum thyroid dysfunction and hypothyroidism 12 years later:
The researchers concluded:
The odds ratio (OR) of hypothyroid PPTD with each unit of decreasing log iodine was 2.54, (95%CI: 1.47, 4.35), and with UIC < 50 lg/l, OR 4.22, (95%CI: 1.54, 11.55). In the long term, decreased log UIC significantly predicted hypothyroidism at 12-year follow-up (p = 0.002) … The association was independent of antibody status.
In short, the more iodine being excreted (and thus, presumably, the more in the diet and in the body), the less likely were hypothyroid disorders – not only at the time, but also 12 years later.
Dangers of selenium supplementation in iodine deficiency.
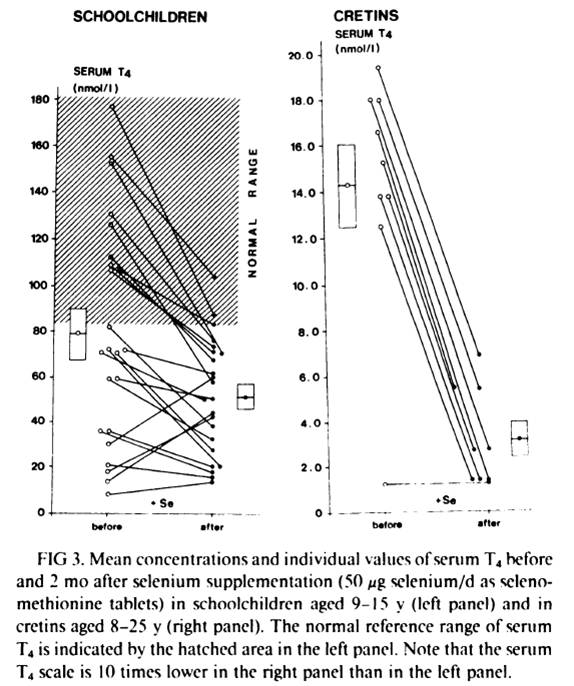
Selenium supplementation when iodine and selenium deficiencies are both present can be dangerous, as the experience in northern Zaire, one of the most severely iodine and selenium deficient population in the world, shows [25].
Schoolchildren and cretins were supplemented for 2 months with a physiological dose of selenium (50 mcg Se per day as selenomethionine). Serum selenium was was very low at the beggining of the study and was similar in schoolchildren and in cretins (343 +- 190 nmil/L in schoolchildren, n=23, and 296 +- 116 nmol/L in cretins, n=9). After 2 months of selenium supplementation, the massive decrease in serum T4 in virtually every subject can be seen in fig. 4 below:
In schoolchildren, serum free thyroxin (fT4) decreased from 11.8 +- 6.7 nmol/L to 8.4 +- 4.1 nmol/L (P<0.01); serum reverse triiodothyronine (rT3) decreased from 12.4 +- 11.5 nmol/L to 9.0 +- 7.2 nmol/L; mean serum T3 and mean TSH remained stable. In cretins, serum fT4 remained the same or decreased to an undetectable level in all nine cretins; mean serum T3 decreased from 0.98 +- 0.72 nmol/L to 0.72 +- 0.29 nmol/L, and two cretins who were initially in a normal range of serum T3 (1.32-2.9 nmol/L) presented T3 values outside the lower limit of normal after selenium supplementation; mean serum TSH increased significantly from 262 mU/L to 363 mU/L (p<0.001).
Another previous similar trial, this time done in 52 schoolchildren, reached the same results: a marked reduction in serum T4 [26][27]. This previous trial “was shown to modify the serum thyroid hormones parameters in clinically euthyroid subjects and to induce a dramatic fall of the already impaired thyroid function in clinically hypothyroid subjects” [27].
What stands out is the difference in the results between euthyroid schoolchildren and cretins/hypothyroids. Two months of selenium supplementation was probably not enough time to affect significantly the thyroid of the euthyroid schoolchildren (althougt already impacted T4 and fT4). But, in cretins and hypothyroids, where the thyroid was already more deficient, the impact was evident.
Conclusion and What I Do
Iodine and selenium are two extremely important minerals for human health, and are righly emphasized as such in the Perfect Health Diet book and blog. I believe they are fundamental to thyroid health and very important to Hashimoto’s patients.
A survey of the literature suggests that Hashimoto’s is largely unaffected by iodine intake. However, the literature may be distorted by three circumstances under which iodine increases may harm, and iodine restriction help, Hashimoto’s patients:
- Selenium deficiency causes an intolerance of high iodine.
- Iodine intake via seaweed is accompanied by thyrotoxic metals and halides.
- Sudden increases in iodine can induce a reactive hypothyroidism.
All three of these negatives can be avoided by supplementing selenium along with iodine, using potassium iodide rather than seaweed as the source of iodine, and increasing iodine intake gradually.
It’s plausible that if iodine were supplemented in this way, then Hashimoto’s patients would experience benefits with little risk of harm. Anecdotally, a number have reported benefits from supplemental iodine.
Other evidence emphasizes the need for balance between iodine and selenium. Just as iodine without selenium can cause hypothyroidism, so too can selenium without iodine. Both are needed for good health.
A few months after I was diagnosed with Hashimoto’s I started 50 mg/day iodine plus 200 mcg/day selenium. If I were starting today, I would follow Paul’s recommendation to start with selenium and a low dose of iodine, and increase the iodine dose slowly. I would not take any kelp, because of potential thyrotoxic contaminants.
Currently I’m doing the following to try to reverse my Hashimoto’s:
- PHD diet and follow PHD book and blog advices to enhance immunity against infections, since infections seems to be implicated in Hashimoto’s pathology [28][29][30]. I give special attention to what Chris Masterjohn calls “traditional superfoods”: liver and other organs, bones and marrow, butter and cod liver oil, egg yolks and coconut, because these foods are high in minerals, like iodine, zinc, selenium, copper, chromium, manganese and vanadium, all of which seems to play a role in thyroid health [31];
- High dose iodine (50mg of Lugol’s) plus 200 mcg selenium daily. These I supplement because of their vital importance to thyroid and immune function;
- 3 mg LDN (low dose naltrexone) every other day to further increase immunity. LDN resources are listed below [32][33][34][35][36];
- Avoiding mercury and other endocrine disruptors. When I removed 9 amalgams (mercury), my TPO antibodies increased for 3 months and took another 6 months to return to previous values. I also avoid fish that have high and medium concentrations of mercury. Cod consumption increased my TPO antibodies;
- 1g of vitamin C daily. Since it seems to confer some protection against heavy metal thyroid disfunction [37], improve thyroid medication absorption [38] and there is some evidence that it could improve a defective cellular transport for iodine [39];
- Donating blood 2 to 3 times per year. In men, high levels of iron seems to impact thyroid function [40].
Final Thanks
I would like to make a special thanks to Paul Jaminet for giving me the opportunity to write this essay, for gathering many, many papers for me, and for having the patience to revise both posts and suggest many changes that made the text clearer; and to Emily Deans who kindly sent me one key study that Paul could not get.
References:
[1] Dr Datis Kharrazian. Iodine and Autoimmune Thyroid — References. http://drknews.com/some-studies-on-iodine-and-autoimmune-thyroid-disease/.
[2] Marino MA et al. Urinary iodine in patients with auto-immune thyroid disorders in Santo André, SP, is comparable to normal controls and has been steady for the last 10 years. Arq Bras Endocrinol Metabol. 2009 Feb;53(1):55-63. http://pmid.us/19347186.
[3] Yoon SJ et al. The effect of iodine restriction on thyroid function in patients with hypothyroidism due to Hashimoto’s thyroiditis. Yonsei Med J. 2003 Apr 30;44(2):227-35. http://pmid.us/12728462.
[4] Kasagi K et al. Effect of iodine restriction on thyroid function in patients with primary hypothyroidism. Thyroid. 2003 Jun;13(6):561-7. http://pmid.us/12930600.
[5] Gribble GW. The natural production of organobromine compounds. Environ Sci Pollut Res Int. 2000 Mar;7(1):37-47. http://pmid.us/19153837.
[6] Zhang ZW et al. Urinary bromide levels probably dependent to intake of foods such as sea algae. Arch Environ Contam Toxicol. 2001 May;40(4):579-84. http://pmid.us/11525503.
[7] Kawai T, Zhang ZW et al. Comparison of urinary bromide levels among people in East Asia, and the effects of dietary intakes of cereals and marine products. Toxicol Lett. 2002 Aug 5;134(1-3):285-93. http://pmid.us/12191890.
[8] Leblanc C et al. Iodine transfers in the coastal marine environment: the key role of brown algae and of their vanadium-dependent haloperoxidase. Biochimie. 2006 Nov;88(11):1773-85. http://pmid.us/17007992.
[9] van Netten C et al. Elemental and radioactive analysis of commercially available seaweed. Sci Total Environ. 2000 Jun 8;255(1-3):169-75. http://pmid.us/10898404.
[10] Hou X et al. Iodine-129 in human thyroids and seaweed in China. Sci Total Environ. 2000 Feb 10;246(2-3):285-91. http://pmid.us/10696729.
[11] Toh Y et al. Isotopic ratio of 129I/127I in seaweed measured by neutron activation analysis with gamma-gamma coincidence. Health Phys. 2002 Jul;83(1):110-3. http://pmid.us/12075675.
[12] Miyashita S, Kaise T. Biological effects and metabolism of arsenic compounds present in seafood products. Shokuhin Eiseigaku Zasshi. 2010;51(3):71-91. http://pmid.us/20595788.
[13] Cleland B et al. Arsenic exposure within the Korean community (United States) based on dietary behavior and arsenic levels in hair, urine, air, and water. Environ Health Perspect. 2009 Apr;117(4):632-8. Epub 2008 Dec 8. http://pmid.us/19440504.
[14] Chong W, Shit Xg, Teng WP, et al. Multifactor analysis of relationship between the biological exposure to iodine and hypothyroidism. Zhongua Yi Za Zhi. 2004 Jul 17:84(14):1171-4. http://pmid.us/15387978.
[15] Tong YJ et al. An epidemiological study on the relationship between selenium and thyroid function in areas with different iodine intake. Zhonghua Yi Xue Za Zhi. 2003 Dec 10;83(23):2036-9. http://pmid.us/14703411.
[16] Karita K et al. Comparison of selenium status between Japanese living in Tokyo and Japanese brazilians in São Paulo, Brazil. Asia Pac J Clin Nutr. 2001;10(3):197-9. http://pmid.us/11708308.
[17] Thorling EB et al. Selenium status in Europe–human data. A multicenter study. Ann Clin Res. 1986;18(1):3-7. http://pmid.us/3717869.
[18] Mengüba? K et al. Selenium status of healthy Turkish children. Biol Trace Elem Res. 1996 Aug;54(2):163-72. http://pmid.us/8886316.
[19] Hincal F. Trace elements in growth: iodine and selenium status of Turkish children. J Trace Elem Med Biol. 2007;21 Suppl 1:40-3. http://pmid.us/18039495.
[20] Fordyce FM et al. Selenium and iodine in soil, rice and drinking water in relation to endemic goitre in Sri Lanka. Sci Total Environ. 2000 Dec 18;263(1-3):127-41. http://pmid.us/11194147.
[21] Alsayed A et al. Excess urinary iodine is associated with autoimmune subclinical hypothyroidism among Egyptian women. Endocr J. 2008 Jul;55(3):601-5. Epub 2008 May 15. http://pmid.us/18480555.
[22] Strieder TG et al. Prediction of progression to overt hypothyroidism or hyperthyroidism in female relatives of patients with autoimmune thyroid disease using the Thyroid Events Amsterdam (THEA) score. Arch Intern Med. 2008 Aug 11;168(15):1657-63. http://pmid.us/18695079.
[23] Stuckey BG et al. Low urinary iodine postpartum is associated with hypothyroid postpartum thyroid dysfunction and predicts long-term hypothyroidism. Clin Endocrinol (Oxf). 2011 May;74(5):631-5. doi: 10.1111/j.1365-2265.2011.03978.x. http://pmid.us/21470286.
[24] American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Evaluation and Treatment of Hyperthyroidism and Hypothyroidism. https://www.aace.com/sites/default/files/hypo_hyper.pdf.
[25] Vanderpas JB et al. Selenium deficiency mitigates hypothyroxinemia in iodine-deficient subjects. Am J Clin Nutr. 1993 Feb;57(2 Suppl):271S-275S. http://pmid.us/8427203.
[26] Contempré B et al. Effect of selenium supplementation on thyroid hormone metabolism in an iodine and selenium deficient population. Clin Endocrinol (Oxf). 1992 Jun;36(6):579-83. http://pmid.us/1424183.
[27] Contempré B et al. Effect of selenium supplementation in hypothyroid subjects of an iodine and selenium deficient area: the possible danger of indiscriminate supplementation of iodine-deficient subjects with selenium. J Clin Endocrinol Metab. 1991 Jul;73(1):213-5. http://pmid.us/2045471.
[28] Benvenga S et al. Homologies of the thyroid sodium-iodide symporter with bacterial and viral proteins. J Endocrinol Invest. 1999 Jul-Aug;22(7):535-40. http://pmid.us/10475151.
[29] Wasserman EE et al. Infection and thyroid autoimmunity: A seroepidemiologic study of TPOaAb. Autoimmunity. 2009 Aug;42(5):439-46. http://pmid.us/19811261.
[30] Tozzoli R et al. Infections and autoimmune thyroid diseases: parallel detection of antibodies against pathogens with proteomic technology. Autoimmun Rev. 2008 Dec;8(2):112-5. http://pmid.us/18700170.
[31] Neve J. Clinical implications of trace elements in endocrinology. Biol Trace Elem Res. 1992 Jan-Mar;32:173-85. http://pmid.us/1375054.
[32] David Gluck, MD. Low Dose Naltrexone information site. http://www.lowdosenaltrexone.org/.
[33] LDN Yahoo Group. http://groups.yahoo.com/group/lowdosenaltrexone/.
[34] LDN World Database. Where LDN users share their experience with various diseases. http://www.ldndatabase.com/.
[35] Those Who Suffer Much Know Much. A colection of LDN users testimonies. http://www.ldnresearchtrustfiles.co.uk/docs/2010.pdf.
[36] Elaine A. More. The Promise Of Low Dose Naltrexone Therapy: Potential Benefits in Cancer, Autoimmune, Neurological and Infectious Disorder. http://www.amazon.com/Promise-Low-Dose-Naltrexone-Therapy/dp/0786437154.
[37] Gupta P, Kar A. Role of ascorbic acid in cadmium-induced thyroid dysfunction and lipid peroxidation. J Appl Toxicol. 1998 Sep-Oct;18(5):317-20. http://pmid.us/9804431.
[38] Absorption of thyroid drug levothyroxine improves with vitamin C. The Endocrine Society. News Room. http://www.endo-society.org/media/ENDO-08/research/Absorption-of-thyroid-drug.cfm.
[39] Abraham, G.E., Brownstein, D.. Evidence that the administration of Vitamin C improves a defective cellular transport mechanism for iodine: A case report. The Original Internist, 12(3):125-130, 2005. http://www.optimox.com/pics/Iodine/IOD-11/IOD_11.htm.
[40] Edwards CQ et al. Thyroid disease in hemochromatosis. Increased incidence in homozygous men. Arch Intern Med. 1983 Oct;143(10):1890-3. http://pmid.us/6625774.












Hi Will,
Great find, thanks for pointing that out.
As usual in small studies with limited data, it’s hard to interpret the results. Selenium without iodine can cause hypothyroidism which is a risk factor for diabetes, but they didn’t measure thyroid status. The increase in diabetes in the selenium group barely reached statistical significance (4 extra cases).
The line in the Discussion about overexpression of catalase promoting diabetes is interesting. The effect may be diet-specific, eg enhancement of glucolipotoxicity on obesogenic diets.
A commentary on the paper has a good discussion: http://www.annals.org/content/147/4/271.long. 200 mcg per day may be too much in some cases, especially if the diet is selenium rich. If a multivitamin is taken, which would add 50 to 100 mcg, and food is selenium-rich then toxicity might even become likely.
We’re going to be revisiting supplement recommendations soon and this looks like a candidate for reconsideration. I think it’s reasonable to dial back selenium dose a bit.
Best, Paul
Hi Paul,
My LEF Se supplement (the one you recommend) just arrived in the mail today. I’m waiting to start iodine supplementation until being on selenocysteine “for a while.” My multi has 200mcg s-methionine, so I’m going to stop taking it while on the LEF Se + iodine protocol.
But after reading the discussion you linked to above, I’m wondering if Se is still necessary during iodine supplementation, or if I will be covered if I’m sure to get adequate dietary Se? (Although dietary is s-methionine and not s-cysteine, the preferable kind, right? So confusing.)
Thanks for your help!
Hi Bella,
It is tricky. Selenomethionine is in plants, selenocysteine is in animals. Animal sources are better.
That’s a lot of selenium for a multi, I think you’re right to stop it.
I think you can take the LEF Se supplement every other day, the iodine daily.
Best, Paul
I read the comment on the paper that you linked to, and they mention the SELECT trial that was being conducted at the time. Sure enough here are the results:
http://www.ncbi.nlm.nih.gov/pubmed/19066370
Insignificant 7% increase in T2DM incidence in the selenium group after 5.5 years (p=0.16), but not the selenium+vitamin E group. Seems like there may be some risk, but less severe than indicated by the previous study.
That comment does mention the epidemiological evidence that we have, and those larger surveys do find plasma selenium levels correlate with worse glycemic control. Oddly enough the study using toenail selenium levels showed the reverse effect, though they point out that smokers have reduced toenail levels and there may be residual confounders even after adjustment…
OMG…I see light under the tunnel!
It is almost 20 years that I have been diagnosed with Hashimoto’s thyroiditis (I had also nodules in the thyroid which slowly disappeared with the time).
Since then I have been taken quite regularly tiroxin (chemical) around 75mg per day. TSH, FT3 and FT4 have been always in the range with TSH around 2 (I know it is a bit higher but I never wanted to take more hormones). However I had always lots of side-effects or anyhow not healthy conditions: mainly very difficult digestions (I understand only now it is because of low acidity in my stomach), non regular evacuations, constipation, dizziness, candida overgrowth, bacterial infections, skin rushes, unable to concentrate/focus, tiredness, etc, etc.
Around 7 years ago I started to have a complete different diet: substantially reduced chemical food (if not at all), no milk products. At that time I thought my main problem was candida. Despite that my health conditions were not improving.
Three years ago I discovered the root cause could have been heavy metals intoxication (I had for tree years!! yes 3! vaccination for dust mites allergy).
I did test and bingo! Very high mercury, high lead, high nickel.
I did the detoxification for two years with EDTA + DMPS, and now levels are very low. In this two years I have been taken supplements, mainly vitamin C, Zink, Selenium, and probiotics, amd also DHEA for 9 months.
Despite that I still had (not so often like in the past, and not so strong) difficult digestions, and bacteria and fungi infections. My tyroid antibodies were still high.
I was so desperate that I wanted to become a fruitarian! I stopped taken all supplements for two months and progressively turning into this diet.
I could not manage. Body reactions were too strong. I slowed down and now trying to go back to normality (I do not eat anyhow milk products and fish at all since three years).
Since 20 days I take again vitaminc C in the morning (at the moment only natural with oranges and kiwi from a juice extractor), zinc 30mg, tiroxin hormon 50mg, selenium 200mcg.
Then I found this website!!
Now I am very much confused and I do not know where to start.
My first question: how can I reduce a bit the issue of the low stomach acidity which is causing me the worst symptoms?
nd then the rest….what have I to do? What should I read? Can you suggest a doctor who could follow me from the distance. I am Italian and live in Germany (so maybe only skype). Thanks for all the help you can give me.
Ciro
If you review the iodine research completed by Dr. Guy Abraham you will see that low stomach acid seems to be related to low iodine. Acid reflux can be cause by low stomatch acid (opposite of what you would think). Sure enough my own acid reflux mostly went away after starting iodine. Also, it totally went away in a young lady why had acid reflux and I suggested this to.
Hi Ciro,
Our book is a general program for good health and healing. If you’re not on our diet it’s hard for me to advise you since there can be so many dietary sources of trouble.
For stomach acid, be sure to eat enough salt and drink enough water. You can also supplement betaine hydrochloride with meals, that may help. Also, you can be checked for H pylori infection, H pylori suppresses stomach acid.
Best, Paul
Hi Paul,
thanks for the answer.
Actually I have often all type of infections: H pylori, E. Coli, Salmonella, Staph, Strept.
I help myself with bio-resonance (which I use also to diagnose) and good immune system (so far so good), but I still have lots of side-effects as wrote in my previous message.
I believe my diet is ok. It is all organic. I eat mainly dinkel bread and pasta (no yeast), live tomatoes, fresh live vegetables, fresh fuits, red and white meat (grass grown). I eat no sugar at all, no milk products, no fish.
I have several food intolerances (banana, apples, avocado, mint, tea, coffee, lactose, and many others). I try to avoid all this food.
My question was more related to the guidelines to follow (better with a doctor) to fix the issue of correct intake of selenium and iodine, and which are the tests I should carry out to determine my exact condition.
Shall I eat salt with added iodine?
Bacteria infection are a problem but not the root cause of all this. So I just wanted to help my body to kill bacteria when eating, waiting for a final solution with my thyroid disorder.
Thanks again for your help.
Ciro
I would supplement iodine. I’d also give up wheat products, replacing them with our “safe starches.”
Forgot to mention that I bought your book earlier today. Looking forward to read it 🙂
i just read something on your website about the diet you recommend.
What do you mean exactly with vegetable oil? I suppose olive oil is not good… 🙁 Which one could instead be eaten?
Thanks
Olive oil is OK. Avoid vegetable seed oils like soybean oil, corn oil, safflower oil, canola oil.
Thanks! Going to buy salt with iodine right now 😉
forgot to ask about Buckwheat. It is not a cereal 🙂
Paul, Mario
Have a few questions:
For someone with Hashi’s:
Do you recommend doing a comprehensive “autoimmune Paleo protocol” like the one Robb Wolf and Matt Lalonde describe on Wolf’s podcast episode 68?
That would exclude dairy (High Vitamin Butter Oil, ghee and non-dairy probiotics) and egg yolks.
Would balsamic vinegar be a problem?
Dr. K has said the “goitrogen model” is outdated (Underground Wellness podcast). Chris Masterjohn says that is not the case (Kresser’s cholesterol podcast pt. 3, comments section).
Any thoughts?
What should those with enlarged thyroids and their endocrinologists recommending a removal of their thyroids take into consideration?
http://robbwolf.com/2011/02/22/the-paleo-solution-episode-68/
Hi Paul,
My multi also has 200 mcg of Selenium as l-selenomethionine and 150 mcg of Iodine as potassium iodide. I also eat eggs every day and a couple of brazil nuts. Is this ok? My only concern is thinning hair and dry skin.
Thanks!
Karen
Hi Karen,
Yes, it is a concern. Try cutting out the multi for a few weeks or a month and see if you feel better.
Thank you!
Hi Paul,
Sorry to ask another question but I’m trying to follow all of this information. If I stop the multi and continue “Primal” eating but without organ meats (yuk!) and limited grass fed meat($$$) – should I supplement with something like Lugols? I think my selenium level is good because of eggs and nuts, but without processed foods and table salt with iodine, I’m wondering if I have enough in my diet. I do eat fish occasionally.
Thanks Again.
Yes, I think you should supplement iodine, but do not change the dose while you’re experimenting with selenium intake. If you haven’t been supplementing iodine, then start very low, like 225 mcg per day, and increase no faster than one doubling per month.
Hi Paul,
I just decided to start supplementing with 200 mcg selenium and some iodine. I bought Iosol and the dose seems to be kind of high to start. My lipid panel came in great but the NMR LipoProfile shoes I have LDL-P over 3000 and LDL-C over 300 (all other numbers are great). So I think I may have a problem with clearance, so I’m going to increase carbohydrate just a tiny bit probably. Definitely increase calories, and supplement with selenium and iodine. I’m afraid of autoimmune thyroid as a result of going too high in iodine though. Are there progressive symptoms that may signal if I’ve gone too far so I can ease off? Or is it once it I’ve gone too far, it’s too late?
Iosol is 1.8 mg per drop. I know you said to start low. Like 250-500. And then increase over time (weekly? monthly? which is it? I’ll have to reread). Is it incredibly dangerous for me to just start at 1.8? Will there be warning signs so I can back off? If anything, I can poor it into a big bottle, shake it up, and split it among 3 bottles to get 500 mcg to start and increase.
When i ‘over-dose’ iodine, i get a sore throat/neck after about 2 or 3 days on that ‘high’ dose.
Though, for me, this only happens when using the potassium iodide form.
I have never actually had any issues with any dose of Iosol (which does not contain potassium iodide).
Though, because of this, it does make me wonder if the Iosol is ‘doing the job’?
…oh, & i can also come out in little red spots on my stomach (usually the next day) with potassium iodide.
I think 1.8 mg is a very large dose to start with, and is likely to induce a reactive hypothyroidism for a while.
I do favor starting at 225 to 500 mcg, and doubling no faster than once a month.
With selenium, every once in a while go off it for a few weeks and see if you feel better or worse. Adjust dose accordingly.
I think increasing carbs is the first thing to do with the high LDL on Paleo problem.
Thanks! Will one day of 1.8 cause an issue? I started with about that much after misreading the bottle. I’ll back off of it for a day and get some kelp pills instead.
Should one wait until happy with their weight to increase carbs? I’m about 5 pounds from my goal (and frankly I’ve slowed down but just started adding exercise to speed it up more) and if course being so carb phobic, I’m afraid it’ll slow me down even more. But then again, if thyroid function increases then it could be helpful…
I made the mistake of starting iodine at too high a level, 1mg. A few months later at my annual physical exam, I came out hypothyroid, and the doc recommended that I discontinue the iodine. At a followup blood test one month later, my levels went back down into the normal range, or at least what mainstream docs call normal. Now I’m scared to try iodine again, because I can’t ask the doctor to test my blood every month. I did notice that the iodine was causing insomnia and that when I stopped taking it, my sleep got better. I didn’t have any other obvious symptoms of hypothyroidism. Do you think that tracking my sleep quality would be a good way to test whether my iodine levels are getting too high?
Why not try a very low dose, 225 mcg, and see if you get insomnia or any negative symptoms?
I believe iHerb sells a 225 mcg tablet.
“I made the mistake of starting iodine at too high a level, 1mg. A few months later at my annual physical exam, I came out hypothyroid, and the doc recommended that I discontinue the iodine.”
Did the doc call you “hypothyroid” simply because your TSH spiked? That could be quite wrong, as TSH often rises for some months after iodine supplementation as the body upregulates the iodine-starved thyroid’s ability to utilize it. TSH ultimately normalizes when this process completes, and in the meantime there aren’t hypothyroid symptoms or signs and T4 levels remain normal. This a phenomenon of improving health, not illness.
Since most docs, even endocrinologists, believe the simplistic idea that TSH by itself reveals the presence or absence of hypothyroidism, this is a common mistake.
Could this be what happened to you? Or were you really hypothyroid based on symptoms, signs, and T4 levels?
The benign spiking of TSH with iodine administration was described in the earliest work by Dr. Guy Abraham, the creator of the modern “Iodine Protocol,” and has been noted by all the docs using iodine.
It is also the case that many people supplement iodine without following Dr. Abraham’s protocol completely (e.g., supplementing selenium, magnesium, vitamin C, unrefined salt, screening for autonomous functioning thyroid nodules). That can lead to thyroid problems, and other serious issues.
The full protocol, however, done with the careful thyroid monitoring recommended, has proved itself extraordinarily safe, even when begun at 50 mg/day or more with no gradual ramp up. I continue to be surprised at how much commentary about iodine takes place without consideration of the remarkable scientific and clinical record of the Iodine Project pioneered by Dr. Abraham and continued by a group of open-minded docs who have reported their findings with thousands of patients in great detail.
If interested, see, for example:
http://www.optimox.com/pics/Iodine/opt_Research_I.shtml
When you say supplement with Iodine with Calcium, mag, selenium, etc, what is the proper balance? Is there a specific supplement that is whole food/natural that achieves this “balance” especially designed for Hashi’s?
Also, another piece of the puzzle in hashi’s is Adrenals. My cortisol shows low in the morning. I was told to take Hydrocortisone to deal with this “dips” in cortisol. I heard that Licorice extract can help deal wiht these dips and take stress of the adrenals. Has anyone read “Stop the thyroid madness”? There’s several protocols in there to address adrenals. I was curious if anyone tried any specific strategies.
hopefully someone ‘in the know’ can answer this one…
I have seen studies that suggest an association between mercury and thyroglobulin autoantibody (anti-Tg) positivity. (google ‘mercury thyroid antibodies’ for refs).
And Mario also writes above;
“When I removed 9 amalgams (mercury), my TPO antibodies increased for 3 months and took another 6 months to return to previous values. I also avoid fish that have high and medium concentrations of mercury. Cod consumption increased my TPO antibodies”.
So my question is…
If thyroid antibody results are low for both anti-Tg and anti-TPO.
Could you safely say that you do not have any mercury related thyroid issues?
“Removal of dental amalgam decreases anti-TPO and anti-Tg autoantibodies in patients with autoimmune thyroiditis”
http://www.ncbi.nlm.nih.gov/pubmed/16804512
Are there best labtest for Hashi’s to monitor “progress”? How does one know what they are doing is working? Is the goal simply to decrease the Antibodies?
As far as the mercury, I heard Zeolite was best for that if that is indeed an issue.
I want to try to take Iodine/Iodine with Selenium after reading this convincing information. The issue I’m having is not knowing how much is in my food. Do you normally “test” to make sure your not provoking an immune response with the Iodine? Sorry guys I’m new to all this and just found out I had Hashi’s after taking Iodine/Iodine for 3 months.
Hi Andrea,
I think the goal is to reduce your thyroid antibodies.
But i am no expert on the subject, so hopefully someone who knows for sure can answer that one…& your other queries.
Out of interest, how do you know you have Hashi’s, was it from blood tests? if you have all the results, it would be good to post them up so people can have a look and comment.
(include the lab ranges and units, as the units used vary between countries).
Hi Andrea,
Yes, you can say that one of the goals is to reduce antibodies, specially if you have very high levels (>1000).
But, a reduction of symptoms are, IMHO, even more important, since they are what impact the quality of your life. A reduction in symptoms could be also a indicator of thyroid recovery.
I know because I did a TPO and TG lab using Direct Labs. My TPO is in the 400’s. My TG was within normal ranges. I was told by a chiro (Dr. Geronimo) that worked under Datis Kharrazin that the TPO “#” does not matter. If it’s over normal ranges you just have Hashi’s and thats it. In fact, he mentioned that if the number is high (like in the 1,000’s) it says that your immune system is doing it job. But unfortunately you have Hashi’s. Has anyone tried to balance their Th1 and Th2 dominance yet? Is says that is vital in Dr. K’s book.
Hi,
I know for sure because I did a TPO and TG lab using Direct Labs. My TPO is in the 400’s. My TG was within normal ranges. I was told by a chiro (Dr. Geronimo) that worked under Datis Kharrazin that the TPO “#” does not matter. If it’s over normal ranges you just have Hashi’s and thats it. In fact, he mentioned that if the number is high (like in the 1,000’s) it says that your immune system is doing it job. But unfortunately you have Hashi’s. Has anyone tried to balance their Th1 and Th2 dominance yet? Is says that is vital in Dr. K’s book.
Hi Mario
Hope you are well. I’m curious to know if your antibodies are still continuing to decline? If so is there anything in particular that you attribute the decline to or is it an all round treatment.
For example you mentioned you are using LDN, dessicated thyroid, Lugols, selenium and on the PHD.
In my case my TG and TPO antibodies have stayed the same for 6 months (around 600 and 40 respectively) although recently my TG antibodies decreased to 450 after a trial of dessicated thyroid. I have my next test in a week after slightly increasing my dose.
It’s difficult to say whether the reduction is down to amalgam removal, a better diet (no gluten) or the introduction of dessicated thyroid but hopefully the next test will shed some light.
Out of interest have you seen any evidence that dessicated thyroid increases your antibodies or is that just scare tactics? The same controversy surrounds iodine which will be the next part of my trial.
Hi David,
I’m doing very well, thanks!
It seems that when you have very high levels of antibodies (>1000) it’s much easier to reduce them.
When you get values lower than 1000, further reductions are harder and I really don’t know if it really matters that much. If you look at table 3, of the first part of this series, the number of people that progressed from subclinical to overt hypothyroidism with TPO 1000) doesn’t progressed.
My antibodies levels are about the same as yours (TPO is around 500 and TG around 80). But, I’m not worried and . For now, I will keep enjoying some seafood now and them and taking dessicated thyroid.
If you are open to experiments and trials, this may interest you:
http://pmid.us/22718472
http://pmid.us/20662037
http://pmid.us/16356148
I’m using a cheap chinese red dot laser (50 mW). Once or twice a week.
Hey Mario,
I’m VERY interested in how you are doing now? I am truly starting to think that Hashimoto’s, as well as MOST auto-immune type conditions have a ROOT cause of some type of underlying infection (like Paul is so on top of and educates us about) as well as an uneducated/malnourished immune system. I know that in my case, after 3 years of intense pain and 20+ doctors later, I finally found out that I’ve had a bad LYME infection. I’ve done a LOT of things to combat/correct it, including Sauna, Frequency Devices (similar to the lazer thing you’re talking about), probiotics, herbs, high dose iodine (50-100mg, which I no longer believe is optimal for me…), medicinal mushrooms, ADRENAL/jing building etc… and i’m finally starting to get all the way better. I’ve found that NASCENT iodine works MUCH BETTER for me than any type of potassium-iodine product (and i’ve tried Iodoral, Iosol, Electridine and Nascent). I also adhere to a gluten free, low nightshades and low dairy diet (only raw cheese and butter). It wasn’t until this past week though that I discovered the critical importance of dietary SELENIUM in the diet. I’ve been rotating 2 brazil nuts several days in a row and then Jarrow’s Selenium Synergy (200mcg) for several days in a row. The selenium has greatly cleared up my skin and strengthened my hair. Can you shoot me an e-mail when you get the chance? I’d love to talk to you more about this. Thanks! Matt
With respect to the type of IODINE to supplement a HYPOTHYROID condition, I came across a brand called “IOSOL IODINE” from Wellness Resources in Minnesota.
Just wondering if anyone has an opinion to its’ claims in comparison to potassium iodide? LINK =
http://www.wellnessresources.com/products/iosol_iodine.php
Hi Ramon, I’ve tried Iosol (1.8mg/drop), And it does better for ME than Iodoral (12.5mg/tablet). I THINK, and my feeling is that the potassium in the iodoral somehow clogs up my thyroid and/or I get a “full throat” feeling when I take the Iodoral. It might be because it’s a larger dose and/or it is attached to the potassium. BUT I know that I can take an equal amount of the Iosol and I do NOT get the “full throat” / Hashimoto’s attack type feeling. Nascent agree’s with me the best (400mcg/drop). 1-2 drops of Nascent in the morning, either just before or right after breakfast. I also make sure to take 2 brazil nuts OR Jarrow’s Selenium Synergy (200mcg) just before breakfast. I know that potassium needs to be balanced with sodium (SALT), or it can throw things out of balance. I make sure to also include plenty of celtic sea salt in my diet. Hope this helps.
Ramon I would like the answer to a brand of iodine as well? ❓
Hi Paul
Great essay, I am so glad I finally found it.
Please bare with me as I know it is a little long winded before I get to the question.
7 months ago due to recurrent miscarriage and some research I did, my wife started taking a selenium and Zinc tablet daily, 100ug selenium and 15mg Zinc and a Kelp Tablet containing 150ug Iodine (I know kelp is bad) . She has tested pos for TPOAb 12 months previous to this (110), we conceived again but this ended in ectopic and convince the thyroid had some impact I again insisted on it being retested, this time (March TPOAb was 130). I thought this a disaster and something I suggested giving her had made things worse. She stopped taking the Kelp, and switched to a purely selenium tablet strength 200ug.
This appears to have had a disastrous affect, her TPOAb measured in June to be 660, after only 3/4 months on the new regime. For the past 15 months she has also been taking 50mg thyroxine.
I am now looking for some advice on the following; my thoughts now are to supplement zinc seperately (not really for TPO) nightly LDN (1.5mg) and keep taking 200mg pure selenium but now combine with the iodine of 150ug as before, and also switch from T4 meds to a T4 and T3 med.
Does this look like a sane thing to do?
Hi Colin,
First, stop the selenium. That’s the biggest problem I think. I’ve had problems myself with selenium and I’m going to blog about it next.
I think the 150 mcg iodine and 15 mg zinc are good.
Wow Paul
First time I have ever commented on a blog, I was expecting days before a reply, thanks!
Funny you say that as I was wondering if Selenium was not the “wonder mineral” it was being touted as, and as I was notified of your reply I was reading an article titled “Selenium Supplements May Harm Not Help”.
Is there not a danger of over supply of iodine problems due to low selenium if we stop the selenium but keep the iodine? Zinc seems to be of some undiscovered importance here, as almost every time I read about the others there is a “soft” suggestion or mention of zinc.
Colin
I think 150 mcg iodine will almost invariably be helpful in hypothyroidism. It’s really the minimum amount needed to avoid outright deficiency.
A healthy diet rich in beef/lamb, shellfish, seafood, eggs, and low-calorie plants should provide sufficient selenium. It’s true that most Americans are deficient, but that’s because they eat grains and sugars and oils for most of their calories.
well now I am super confused. I started iodine .75mg (got the tablets recommended on this site but they are 3mg and I have hashimotos so starting by cutting them into fours). and selenium at 200mcg. I was taking the selenium before and noticed my temperatures dropped but was also reading on your site that taking BOTH is very important with hashimotos. That iodine alone can be harmful and selenium alone can be harmful but BOTH together can help hashimotos and hypothyroidism? I have been off all gluten and grains except rice since October of 2011. I still can’t lose the tummy fat and temps won’t rise. I take divided dosing t3 (total of 35mcg) and one 20mcg t4 every 3 days after fixing a reverse t3 problem. Any advice on iodine and selenium would be great. Also…any side effects to be on the lookout for with iodine supplementing if you are already having hypo symptoms? thank you!
Hi Carmen,
Having selenium in its “plateau range” or “peak health range” is very important. The question is: how much do you get in food? Depending on that question, the selenium supplementation could either put you into the peak health range (standard American dieters) or put you above it with negative effects. I now think the latter may often be the case with whole foods PHD dieters.
A complication is that selenium intake is highly variable depending on the place where your food was grown/fed.
There’s also evidence that selenium from food is less dangerous than selenium from supplements, so I now think it’s best to get selenium from food.
Re iodine, you can try altering the dose to see if it helps, but I would expect selenium to be a more likely source of trouble. If selenium is wrong then high doses of iodine will be problematic.
ok…so to be clear. since I eat a paleo style diet with good carbs (basically YOUR diet is what I have been following since Februaru bc low carb paleo dieting put me in a state of RT3 issues)…I should STOP taking selenium and stay on the small dose of .75mg iodine and up the dose according to your guidelines specified in the articles on iodine etc. my main complaints are cortisol issues (fatigue and low exercise tolerance ) when T3 is off and fat around the tummy and nowhere else and hair falling out.
Hi Carmen,
Yes, I would stop the selenium; eat selenium rich foods like shellfish, beef, eggs, and maybe kidneys once in a while; stay at the .75 mg iodine dose indefinitely until your thyroid situation has stabilized — you need to know selenium status is right before raising it further. You might try regularly inducing sweating (either exercise or sauna, drink plenty of water) which helps excrete excess selenium.
Best, Paul
Thank you Paul. I am a personal trainer so sweating is NO problem (except when my temps drop into the 96’s which hasn’t happened in awhile). Your diet is awesome..I recommend the book to my wellness clients and personal training clients. Thank you for all you do!!!
Anyone have any links to good (reliable) info on symptoms of long term selenium deficiency and toxicity.
So we know what to look for.
thx
I’m curious to know what reliably evidence Paul will present of selenium toxity in presence of iodine sufficiency, because I don’t know any.
Iodine group in Yahoo has more than 6,500 members. And I don’t remember anyone with selenosis. Searched for selenosis and selenium toxity and found no one complaining about it.
If you look at the principal supporting studies in the EPA toxity risk information for selenium at:
http://www.epa.gov/iris/subst/0472.htm
You see that, for example, Yang et al. (1989b), analyzing a chinese population with high levels of selenium, only found 5 cases of selenosis in 349, with dietary selenium as high as 1438 ug/day. Longnecker et al. (1991) analyzed 142 residents of South Dakota, a region with high concentration of selenium in the soil, and found no cases of selenosis, including individuals whose selenium intake was as high as 724 ug/day.
Selenium toxity symptoms are basically the same for hypothyroidism, except the garlic odor.
I have the same question.
It’s not just the Yahoo iodine group (which I also follow, and I agree with Mario that one never reads of selenium toxicity problems despite everyone there being advised to take 200–400 mcg of selenium along with 12.5–100+ mg iodine per day).
There’s also the thousands of patients in the Iodine Project, under very close medical supervision for years and doing the same thing. I don’t recall reading of any cases of selenosis. And these are holistic docs, so I have to believe that many of the patients were also eating very good whole foods diets. Certainly Dr. Brownstein does not advise fat avoidance or any other conventional nutritional nonsense, for example.
Beyond the Ioidine Project, more and more docs have been using Dr. Abraham’s iodine protocol, with the aforementioned 200–400 mcg selenium/day. Again I can’t recall reading about any finding of or concerns about selenium toxicity despite careful medical supervision .
All this doesn’t prove it can’t happen, but it’s an incredible record of safety for the whole Abraham iodine protocol, including both the iodine and selenium supplement doses it includes.
I would be curious to know what evidence can stand against this to support warnings against this protocol, whether from selenosis or anything else beyond the cautions that are already a part of the iodine protocol itself.
I have to agree with you guys for the most part. Doesn’t mean that it can’t happen… and i’m sure that there are cases where one would want to avoid supplemental selenium, but for the most part, it seems that as long as you BALANCE selenium/iodine and other key minerals/nutrients, then it won’t pose much of a problem, and could in fact be beneficial (I know that supplementing w/ 200mcg/day for me OR a brazil nut, has cleared up my skin, increased my body temp and made my nails/hair stronger. I also take a SMALL dose of iodine (1 drop Nascent) and one sublingual b12 tablet daily as well.. but it wasn’t until I added the selenium that I got the results). I also fully agree with Paul’s stance though, that Selenium should primarily be attained from the diet when possible. BTW, I follow PHD very closely, except I add more types of Rice (Wild and Forbidden) and properly prepared oats to my diet as well. I also drink 1/8tsp celtic sea salt w/ water first thing in the morning.
I think for me it might be the intolerance to “too much for me” selenium….not necessarily a toxicity thats measurable. I have hypothyroid symptoms I can’t get rid of despite treatment with T3 and T4 protocols etc. what is the iodine group link if you please? thanks!
Iodine group at Yahoo:
http://health.groups.yahoo.com/group/iodine/
Like Colin’s wife, I also have antithyroid antibodies, which I just recently found out.
TPO/ Antithyroid Peroxidase- 131
Thyroid Antithyroglobulin Ab- 106
After reading here and there on the Internet, I also got the idea to make sure I take my selenium 200 mcg supplement, thinking that it will decrease my antithyroid antibodies (but I don’t remember where I got the idea). I will get tested again in the next month or so, but after Colin’s email I’m a little worried. Of course there could be other factors involved to cause her antibodies to increase…? One thing I did notice in the days I took the selenium supplement was some area of my throat seemed to swell a little (not visibly so, but just how it felt internally)… not sure but I think it was the lymph nodes in my neck, maybe they swelled. don’t know if that’s good or bad, but I definitely noticed it. ?? What was that?
I had the neck swelling “feeling” too.. i attribute it to a reaction of the hashimotos or a flare if you will…to something that didn’t work for my body or the need for more T3. I am not taking selenium today to see if that helps that sensation.
I’m just now starting to learn about all this, so my limited experience probably doesn’t say much yet, but I did notice that “lump in the throat” kind of feeling only on the days I took the selenium, which was only a few days so far. I usually approach all of these things cautiously and don’t really jump on the bandwagon so I’ve only taken it sporadically, every few days. Other than those days, I cant recall ever feeling a lump in throat other than when I’ve been sick a long time ago.
Also, I noticed a lot of multivitamins do have iodine and selenium. I have a few different multis now and I kind of rotate them around, just in case (of what, I don’t know, just seemed like a wise idea in case one of them is no good) but all of them have 150mcg iodine and the selenium varies- 70mcg, 100 mcg and 200mcg.
The days I took the selenium supplement (Now brand), I took the low-selenium multi and might have only taken half the multi dose, so I shouldn’t have gotten more than 235mcg or 270mcg maximum selenium those days (well, except for what’s already in my nutritious PHD). Maybe I am getting enough from diet…
Can you have selenium blood levels easily tested?
Swelling of the throat could be a bromine related symptom. The most effective for bromine detoxing is salt loading.
http://www.breastcancerchoices.org/bromidedetoxsymptomsandstrategies.html
Both iodine and selenium, taken alone or together, reduce bromine levels of the thyroid:
http://www.ncbi.nlm.nih.gov/pubmed/16601782
Hello,
Does salt loading (e.g. consuming Celtic Sea salt or iodine supplementation) require fat for optimal absorption?
thanks,
Henry
I have read that one symptom of selenium toxicity is white blotchy nails.
I have been trying to find an image on the web of white blotchy nails caused by selenium toxicity without any success.
I do not have any white marks on my own nails but am interested to see what these white blotchy nails look like.
Any one have a link to such an image, related to selenium toxicity?
All i have been able to find are images of white marks or spots on nails, which seems to relate to either nail damage or zinc deficiency.
Hi Paul
A very quick question. I am having some troubles with iodine due to excessive supplementation. I am experiencing rapid heart rate and hunger on ingestion of any foods with high amounts of iodine. I have stopped supplementation and reduced intake from natural foods. I also supplement with selenium.
Will it take long for symptoms to wear off?
I know your busy Paul. But im a bit concerned. Thanks so much for your time.
Kevin
Hi Kevin,
I would stop the selenium. The iodine is not likely to cause a problem unless selenium is off. The selenium is most likely too high. So go off it completely for a month at least.
Be sure your copper status is OK, if you don’t eat 1/4 lb beef or lamb liver per week supplement 2 mg/day copper.
Afternoon all
It’s been just over a year that I found out that I Hashimotos, albeit sub-clinical.
As part of my experimentation to reduce my antibodies (Thyrogobulin was very high at 639) I have done the following:
1. Eliminated about 95% of my gluten intake and tried to maintain a perfect health diet.
2. Removed all my mercury amalgams (11 of them)
3. Supplement Thyroid-s (1 grain) since April
4. Supplemented Co-Q-10 and cortisol
5. Supplemented selenium at various times
My last result showed that my TG antibodies had decreased quite significantly and I’m hopeful that my next test will continue that trend although I had my last amalgam replaced last week.
I’m still debating whether to try LDN and see if that has an effect but also the use of iodine (with selenium) as that seems to be key although there is much debate over that.
On the subject of debate has anyone seen their antibodies decrease through cutting out gluten? I keep reading about it but I do not think it has made a great deal of difference to me. It seems to be that the evidence is based on the research that shows that around 20% of people with Hashimotos have some form of celiac disease ( http://www.celiac.com/articles/1135/1/Connection-Found-between-Celiac-Disease-and-Hashimotos-Thyroiditis/Page1.html)
Whilst 20% is a high figure that suggests that 80% of people with hashimotos do not have a problem with gluten.
Has there been any more recent or conclusive research that shows a definite connection?
Hi David,
Good questions, and also good plan of attack for your Hashimoto’s. Congratulations on your progress.
I’d consider LDN as a one of a suite of circadian rhythm strategies. I’d do a variety of circadian rhythm improvements — daytime sun exposure, 30 minutes of daytime exercise, concentrating food intake in an 8 hour window concluding around sunset, dim lights at night, sleep in a darkened room and waken naturally. Then consider LDN on top of that if that’s not enough.
Gluten-free dieting probably helps a significant number of people (it works in atypical celiac disease: http://www.ncbi.nlm.nih.gov/pubmed/22238404) but you’re right, we don’t know what fraction it helps.
Best, Paul
Hi Mario and Paul
Following on from my last email I’m in a bit of a panic about my last results as my T4 was 48.6 nmol/L (range 77-154) is looking low as well as my TSH (0.245). Meanwhile my TPO antibodies have doubled from 45 IU/mL to 94.
At the moment i’m on one grain of dessicated thyroid (thyroid-s) which might be too high as my TSH is so low, yet I would expect my T4 to be higher. I wonder if I should just cut try cutting out the dessicated thyroid for a month and see what happens or if I should supplement some T4 and stick on the dessicated thyroid?
Funnily enough my FT4 was OK at 11.1 pmol/L (range 10-22)and FT3 was also OK at 4.7 pmol/L (range 2.8-6.5).
My lab notes did mention the possibility of a heavy metal burden which could be significant as I had my last amalgam removed a week ago and it was a big one on my wisdom tooth.
Any ideas on the best approach? I have to say that I still feel fine although am worried. 😯
Hi David,
Mario has answered this well. The T3 in the dessicated thyroid will suppress TSH and T4 generation. If you want your numbers to be more normal, then you would have to cut the T3 dose and could consider taking a bit of T4 to compensate. Cutting the dessicated thyroid in half might be a useful experiment. But how you feel is a much better guide to what you should do than the T4/TSH numbers.
David,
When supplementing with T3 or dessicated thyroid extract, TSH is useless, as it will be very low or suppressed. If you don’t have symptoms of hyper, it means nothing.
Decreased levels of T4 and FT4 is sometimes seen in dessicated thyroid users. IMHO, If you fell fine, there’s nothing to worry. Just keep doing what you’re doing!
Ps. antibodies fluctuate, and your TPO antibodies are still low and the increase was minimal. I don’t know when you removed your amalgams, but that can cause a transient increase in antibodies.
Hi Mario
Thanks for the quick reply. It has set my mind at ease although I did have a hunch that my body is processing the T3 part of the dessicated thyroid and therefore has no need to convert the T4 into more T3.
I am curious to know what would happen if I stopped taking the dessicated thyroid as i’ve been on it for 6 months. I don’t feel any different on it except for the fact that my skin is not as dry.
In your experiments have you ever come off dessicated thyroid to see what happens? I wonder if you get your diet sorted and with correct supplements if your thyroid will regain it’s health, assuming it has not been destroyed?
Re the amalgam it was removed last week and had 3 cavities in one wisdom tooth. I read that your antibodies were elevated after amalgam removal which is not surprising given the heavy metal toxcity.
Thanks
David
David,
I don’t want to experiment with getting off dessicated thyroid, since it is not detrimental to my health. Low levels of thyroid hormones are much more of a concern to me.
If you get your thyroid problems sorted out, and it begins to heal, you will know when to stop or reduce it. But, one grain is a low dose, anyway.
Interesting abstract that high carbohydrate intake is linked (or leads to?) iodine deficiency.
http://www.ncbi.nlm.nih.gov/pubmed/15142639
I only have access to the abstract, so i do not know what their definition of ‘high carbohydrate’ is.
& do not know if they found a linear relationship between iodine requirement and carb intake ie. more carbs = more iodine needed.
“Abstract,
An increased iodine requirement as a result of significant changes in human nutrition rather than a decreased environmental iodine supply is suggested to represent the main cause of the iodine deficiency disorders (IDD).
The pathomechanism proposed is based on the fact that serum concentrations of thyroid hormones, especially of trijodothyronine (T3), are dependent on the amount of dietary carbohydrate.
High-carbohydrate diets are associated with significantly higher serum T3 concentrations, compared with very low-carbohydrate diets.
While our Paleolithic ancestors subsisted on a very low carbohydrate/high protein diet, the agricultural revolution about 10,000 years ago brought about a significant increase in dietary carbohydrate.
These nutritional changes have increased T3 levels significantly.
Higher T3 levels are associated with an enhanced T3 production and an increased iodine requirement.
The higher iodine requirement exceeds the availability of iodine from environmental sources in many regions of the world, resulting in the development of IDD.”
Darrin,
Interesting theory. It does strike me as an over-simplification to say high carb (in general) causes iodine deficiency. I think of the very high carb traditional folks that seem healthy. It seems we need the details on the diet and carb sources (was it modernized refined wheat, starchy tubers, fruit, etc.) and then investigate further … maybe the main factors are not macronutrients.
I just recently read Dr. Brownstein’s Iodine: Why You Need It, Why You Can’t Live Without It (4th Edition) and he offers some additional dietary sources to consider on page 45:
So, maybe it’s the bromide content of the carbs – Dr. Browstein’s point about bromide in bakery products is that bromide is a halide that interferes with iodine utilization in the body.
Note that Dr. Brownstein recommends unrefined sea salt and not refined iodized salt, but recognizes it as a source of iodine.
It’s interesting that the abstract states this as if it is a fact:
Do we really know?
No, we don’t know how much protein “cavemen” ate
Even so, it does make sense agricultural would increase dietary carbs …
i agree with all of that.
it seems reasonable to assume there has been an increase in exposure to competing halogens; bromine, fluorine & chlorine.
We do need some chlorine (chloride) but not too much.
Bromine & Fluorine have no known biological role according to wiki
http://en.wikipedia.org/wiki/Halogen#Biological_role
here’s another link to the same study,http://www.sciencedirect.com/science/article/pii/S0306987704001690#
still just the abstract, but this one includes a Figure
I took iodine for the first time 6 months ago. Maybe 1-2mg of iodine. I got an extreme ‘rush’ and a tinnitus that I’ve had since then. (e.g. when I move my head) My eyes start burning and get red for no reason sometimes.
I think it was the Jod-Basedow phenomenon.
Thinking it was ‘detox’, I started taking Lugol’s in high dosages (>50mg). I got sinus headaches and a metallic taste in the mouth.
I finally realized that I was poisoning myself and stopped it altogether. (tip: don’t trust alternative health sites with people that think evidence-based science is a hoax)
Unfortunately, the symptoms got worse recently. Pulsatile tinnitus, dizziness especially in the morning.
Taking selenium for a while didn’t help either. (200 mcg – but I had side effects. My head got really hot when I took it sometimes, so I stopped it)
After several months, I decided to take iodine again because I was so desperate. I started three days ago. I eat at least three eggs per day now, so I’m quite confident that I get enough selenium. I take 50mg of iodine with Lugol’s over the day. (I avoid taking one big dose)
Again,
I have some symptoms that I also had before: Itchiness in my neck region (not really bad – just sometimes, like 1-2 times per day. It’s weird, but it doesn’t bother me); runny nose; I also have to clear my throat quite often.
The symptoms after taking that dose of iodine half a year ago are so bad that I’m willing to do anything. I’m just not sure what. I’m kinda afraid to go to a doctor. I think they would think that I’m insane or something or a hypochondriac. Also, I had going to the doctor.
Does anyone have any tips for me? Could the dose of up to 50mg with sufficient selenium from diet hurt me? Are the symptoms (strange feeling in the neck) worrisome? Am I possibly poisoning myself? Did I give myself an autoimmune disease by taking iodine back then?
Any help would be appreciated.
I’m 22, male. I have TMJ disorder and had problems with depression. Generally, I’m in a good state of health, though. I hardly eat any processed foods and hardly any sugar. My weight is ‘okay’ (in the normal range – that wasn’t always the case). I exercise several times a week. Generally, I’m in a good state of health. My diet is pretty much a Weston A. Price diet. I haven’t eaten gluten in a while, but started eating sourdough bread again because I didn’t see any significant improvement.
When I took iodine for the first time, I also realized how my voice changed. (apparently, it was hoarse before)
I know I can’t expect a diagnosis here 😉
Any ideas would be greatly appreciated, though.
Hi Kevin,
My first tip is don’t try iodine with such huge doses. Even 1 mg is an extremely high starting dose. Try getting the 225 mcg tablets and cutting them in quarters with a razor blade so you start at 50 mcg (not mg); or try eating shellfish and seaweed and see if you get hyperthyroid symptoms from that.
I tend to suspect a chronic infection in situations like yours — something that affects the thyroid, sinuses, and ear.
Selenium is a nutrient for eukaryotic pathogens as well as for human cells so if you overdose easily on it that could be a clue to the nature of an infection. 3 eggs is important but you also want beef/lamb, shellfish, and seaweed, possibly kidneys, to assure good selenium status.
I think seeing a doctor is the logical step. They are not good at diagnosing these conditions, but you should give yours a chance.
Hey Kevin,
Just so you know… I had VERY SIMILAR symptoms to you back when I was 23 years old (i’m 27 now). I had blood shot eyes and full blown TMJ and major fatigue, super stiff neck, coordination problems and sinus pressure. I ended up spending $5,000 cash for a nueromuscular orthotic and tensing sessions to supposedly fix the TMJ. It ended up being a total waste of time/money. The only thing that worked somewhat was the tensing unit. And I THINK that it was working because it was knocking back the infections in the area where the unit was at (I know that sounds weird, but electrically shocking an area can knock back infections in that area). Anyways, eventually I ended up finally figuring out that infections and my immune/nervous system where at the root cause of my problems. I tested positive for Lyme’s disease and coinfections (through IGeneX labs) and I tested positive for several other gut bugs (D. Fragilis & a slight overgrowth of candida) through Parasitology Center (Dr. Omar Amin).
To make a very long story short… I think that my immune system, nervous system and HORMONAL system got MAJORLY out of whack… it got hammered by living in a house that had Black mold AND from not including good probiotics/fermented foods in my diet AND from completely taxing my system working a job 60-70 hours a week and competing in triathlons. I literally went from placing 2nd in a triathlon to not being able to walk up stairs without major shortness of breath in a matter of 2 weeks. I’m almost back to 100% now and plan on detailing more about my journey as soon as possible. I really got turned onto Paul Jaminet’s work because of his interest in pathogens as a major problem in many autoimmune type conditions. To sum up what got me back to where I am… I’d say it was:
1) Paleo type diet (very close to PHD, but with properly prepared wild rice/forbidden rice and oats added)
2)A major focus on fermented foods (to get ENZYMES and proper absorption of nutrients going again)
3) Adding acids to near every meal (lemons w/ breakfast… lemons/olive oil with dinner)
4) Focusing on BALANCING hormones, ESPECIALLY cortisol. Getting cortisol UP in the morning and leveling it off throughout the day). That’s what i’m still working on, but I feel like i’ve got it almost back. Circadian rhythm balancing, glandulars, select adaptogens, etc…
Best of luck man! I know it’s crazy hard finding answers when something like that is going on with your body. Just keep adding in the good…
BTW, I also totally got that metallic taste in my mouth after taking Iodine. It also felt like it released pressure around my thyroid/neck area for some reason. I stopped supplementing it (I was doing in upwards of 62.5mg a day for a while, 3 tabs in the morning & 2 at night)… started going to whole food sources like seafood and seaweeds. Might be good to take a break from it for a while
Hi Paul!
My naturopath says that when selenium levels are what they should be, I’ll be able to try iodine supplementation for weaning down my dose of Armour (for Hashi’s). I’ve been “supplementing” selenium for 2 years with Brazil nuts (he considers 200 mg too much to take in anything other than food sources). After 2 years I’m getting a bit discouraged, as on hair analysis I continue to decrease in selenium and increase in iodine. (Thought they would begin to converge!) Do you think hair analysis is a good way to measure progress (as I’m not seeing a lot of progress in symptoms)?
Hi Kathy,
Brazil nuts don’t necessarily have large amounts of selenium. The selenium content of plants depends on the selenium content of the soil they’re grown in, Brazil nuts can have almost zero selenium, though most do concentrate selenium and selenium content can become very high. The USDA database happened to use Brazil nuts grown in selenium-rich soil, that’s why it’s assumed that Brazil nuts are high in selenium.
See http://honey-guide.com/2012/11/19/brazil-nuts-and-selenium/ for variability in selenium content of Brazil nuts.
If you want to get selenium from food, you should eat kidney weekly, preferably beef or lamb kidney. Also good are shellfish, seafood, beef, lamb, and eggs.
I think you should supplement 200 mcg maybe twice a week. Make sure it’s an organic form of selenium, not selenite/selenate.
I think hair analysis is probably a good indicator for selenium.
Dear Paul,
I was wondering if you can point me to studies on the disadvantages with inorganic selenium supplements. The studies using inorganic selenium that I have read so far indicate that it is effective in counteracting excessive iodine consumption. The citations for that are mainly in part I of this iodine report.
P.S.: At least the selenate (SeO4–) form seems to be quite safe and effective and potentially even better than Selenomethionine. The best form appears to be Se-Methyl L-Selenocysteine, which is naturally contained in garlic and broccoli. Unfortunately this form is not available in supplement form in Europe. Thus, Europeans are left with either selenate or selenomethionine. the former appears to be better according to this well referenced site:
http://www.ilifelink.com/selenium_supplementswhy_selenate_rates_and_selenite_bites.html
Hey Paul
Had many great improvements on your diet which I switched to from very low carb paleo. I’v had a few ups and downs with iodine. Started iodine at 225mcg about a month or two ago. Upped to 450mcg after a month but started getting dizziness, throat pain and very bad low back pain after only three days, so I went back down to 225mcg. Its been about three weeks since then and thankfully the throat, back pain and dizziness has gone away. But iv now developed a very itchy rash/bromoderma on my elbows and upper arm on the triceps, side hips and around my lats. I completely stopped the iodine supplements and its been about four days, with no improvements in redness, itchiness. Iv been taking all the other nutrients like liver, eggs, starches, about a quarter pound of kidney as well, and upped my C to 5g instead of 2g. Also I try salt loading by having half a tsp in water twice a day, excluding the amount I put on food which i feel I’m getting high blood pressure from. The rash seems to be spreading though and not going away, I don’t know what to do or if I should stick with the iodine to help the bromine detox away faster 🙁
Do you know how long it will take to go away, i don’t want it to spread to my forearms or anywhere visible because my parents will get worried if they find out, it’s hard to make them understand why iodine’s important. I’m 20 years old, living in UK, and I’m confused on whether I should give up Iodine because I’m a bit worried about the detox period or if I’m getting enough selenium from UK soils and maybe start at a later age when I have more free time to look into it and have doctor supervision or something. Would eating salmon, yogurt, some seafood, and sushi or nori sheets be enough to relieve a deficiency. I may stick with that until some later stage.
Would love to hear from you on this!
Hi Adam,
I guess I would continue to refrain from iodine until it goes away, then find a dose small enough that nothing happens to your skin.
You might want to have your thyroid hormone levels measured to see if those have been disturbed.
I think your selenium status should be good with the kidney you are eating. But it won’t do any harm to take a selenium supplement 1 or 2 times a week.
Yes, just eating seafood and seaweed is sufficient to maintain normal thyroid and immune function.
Aright, Sounds good. So 150mcg is the minimal to avoid a deficiency rite? You can get that by eating 3 eggs daily and a cup of yogurt and strawberries. And if you wanted to increase iodine further just include some seaweed and seafood weekly?
Hi,
Anyone familiar wih the dried urine iodine test from ZRT labs? I just had this test done for about $90 and it came back very low at 23mcg/g creatinine, normal range being 100-300mcg/g creatinine. Any advice? I have Hashi’s.
Thanks!
Hi Jay,
I’m not familiar with the test, but if you don’t supplement iodine I think it would be a good idea to supplement with 225 mcg/day.
Best, Paul