One of the more mysterious conditions afflicting low-carb Paleo dieters has been high serum cholesterol. Two of our most popular posts were about this problem: Low Carb Paleo, and LDL is Soaring – Help! (Mar 2, 2011) enumerated some cases and asked readers to suggest answers; Answer Day: What Causes High LDL on Low-Carb Paleo? (Mar 4, 2011) suggested one possible remedy.
On the first post, one of the causes suggested by readers was hypothyroidism – an astute answer. Raj Ganpath wrote:
Weight loss (and VLC diet) resulting in hypothyroidism resulting in elevated cholesterol due to less pronounced LDL receptors?
Kratos said “Hypothyroidism from low carbs.” Mike Gruber said:
I’m the guy with the 585 TC. It went down (to 378 8 months or so ago, time to check again) when I started supplementing with iodine. My TSH has also been trending up the last few years, even before Paleo. So hypothyroidism is my primary suspect.
Those answers caused me to put the connection between hypothyroidism and LDL levels on my research “to do” list.
Chris Masterjohn’s Work on Thyroid Hormone and LDL Receptors
Chris Masterjohn has done a number of blog posts about the role of LDL receptors in cardiovascular disease. His talk at the Ancestral Health Symposium was on this topic, and a recent blog post, “The Central Role of Thyroid Hormone in Governing LDL Receptor Activity and the Risk of Heart Disease,” provides an overview.
His key observation is that thyroid hormone stimulates expression of the LDL receptor (1). T3 thyroid hormone binds to thyroid hormone receptors on the nuclear membrane, the pair (a “dimer”) is then imported into the nucleus where it acts as a transcription factor causing, among other effects, LDL receptors to be generated on the cell membrane.
So higher T3 = more LDL receptors = more LDL particles pulled into cells and stripped of their fatty cargo. So high T3 tends to reduce serum LDL cholesterol levels, but give cells more energy-providing fats. Low T3, conversely, would tend to raise serum cholesterol but deprive cells of energy.
Other Pieces of the Puzzle
Two other facts we’ve recently blogged about help us interpret this result:
- LDL particles are not only lipid transporters; they also have immune functions. See Blood Lipids and Infectious Disease, Part I, Jun 21, 2011; Blood Lipids and Infectious Disease, Part II, Jul 12, 2011.
- T3 becomes low when glucose or protein are scarce. Thyroid levels alter to encourage resource utilization when resources are abundant and to conserve resources when they are scarce. See Carbohydrates and the Thyroid, Aug 24, 2011.
We can now assemble a hypothesis linking low carb diets to high LDL. If one eats a glucose and/or protein restricted diet, T3 levels will fall to conserve glucose or protein. When T3 levels fall, LDL receptor expression is reduced. This prevents LDL from serving its fat transport function, but keeps the LDL particles in the blood where their immune function operates.
If LDL particles were being taken up from the blood via LDL receptors, they would have to be replaced – a resource-expensive operation – or immunity would suffer. Apparently evolution favors immunity, and gives up the lipid-transport functions of LDL in order to maintain immune functions during periods of food scarcity.
High LDL on Low Carb: Good health, bad diet?
Suppose LDL receptors are so thoroughly suppressed by low T3 that the lipid transport function of LDL is abolished. What happens to LDL particles in the blood?
Immunity becomes their only function. They hang around in the blood until they meet up with (bacterial) toxins. This contact causes the LDL lipoprotein to be oxidized, after which the particle attaches to macrophage scavenger receptors and is cleared by immune cells.
So, if T3 hormone levels are very low and there is an infection, LDL particles will get oxidized and cleared by immune cells, and LDL levels will stay low. But if there is no infection and no toxins to oxidize LDL, and the diet creates no oxidative stress (ie low levels of omega-6 fats and fructose), then LDL particles may stay in the blood for long periods of time.
If LDL particles continue to be generated, which happens in part when eating fatty food, then LDL levels might increase.
So we might take high LDL on Paleo as a possible sign of two things:
- A chronic state of glucose deficiency, leading to very low T3 levels and suppressed clearance of LDL particles by lipid transport pathways.
- Absence of infections or oxidative stress which would clear LDL particles by immune pathways.
The solution? Eat more carbs, and address any remaining cause of hypothyroidism, such as iodine or selenium deficiency. T3 levels should then rise and LDL levels return to normal.
Alternatively, there is evidence that some infections may induce euthyroid sick syndrome, a state of low T3 and high rT3, directly. And these infections may not oxidize LDL, thus they may not lead to loss of LDL particles by immune pathways. So such infections could be another cause of high LDL on Paleo.
Gregory Barton’s Experience
Gregory Barton is an Australian, 52 years old, living in Thailand, where he keeps goats, makes goat cheese and manages a large garden which can be seen on http://www.asiagoat.com/.
Gregory left a comment with an intriguing story, and I invited him to elaborate in a post. Here’s Gregory’s story. – Paul
Gregory’s Writing Begins Here
One of the claims of low carb dieting is that it will normalize the symptoms of metabolic syndrome. Blood pressure, blood sugar and blood lipids, it is claimed, will all come down on a low carb diet, in addition to weight. For most people this happens. But there is a significant minority of people on Paleo and other low carb diets whose blood lipids defy this claim. (See the list of low-carb celebrities with high LDL in this post.)
Why should this happen? Why should some people’s lipids fall on low carb while other people’s lipids rise? Suboptimal thyroid might be the proximate cause for lipids rising on a low carb or paleo diet. Broda Barnes and Lawrence Galton have this to say about thyroid disorders:
“Of all the problems that can affect physical or mental health, none is more common than thyroid gland disturbance. None is more readily and inexpensively corrected. And none is more often untreated, and even unsuspected.” — Hypothyroidism: The Unsuspected Illness
I went very low carb in April in an effort to address metabolic issues, eating as little as 15grams carbohydrate per day. I had great results with blood pressure, sleeping, blood sugar and weight loss. But lipids bucked the trend.
I had expected triglycerides and cholesterol to drop when I cut the carbs, but they did the opposite: They surged. By July my total cholesterol was 350, LDL 280, and triglycerides bobbed around between 150 and 220.
I did some research and found several competing theories for this kind of surge:
- Saturated fat: The increase in saturated fat created a superabundance of cholesterol which the liver cannot handle. Also, Loren Cordain has claimed that saturated fat downregulates LDL receptors.
- Temporary hyperlipidemia: The surge in lipids is the temporary consequence of the body purging visceral fat. Jenny Ruhl has argued that within a period of months the situation should settle down and lipids should normalize.
- Hibernation: The metabolism has gone into “hibernation” with the result that the thyroid hormone T4 is being converted into rT3, an isomer of the T3 molecule, which prevents the clearance of LDL.
- Malnutrition: In March, Paul wrote that malnutrition in general and copper deficiency in particular “… is, I believe, the single most likely cause of elevated LDL on low-carb Paleo diets.”
- Genetics: Dr. Davis has argued that some combinations of ApoE alleles may make a person “unable to deal with fats and dietary cholesterol.”
I could accept that saturated fat would raise my cholesterol to some degree. However, I doubted that an increase in saturated fat, or purging of visceral fat, would be responsible for a 75% increase in TC from 200 to 350.
There are two basic factors controlling cholesterol levels: creation and clearance. If the surge was not entirely attributable to saturated fat, perhaps the better explanation was that the cholesterol was not being cleared properly. I was drawn to the hibernation theory.
But what causes the body to go into hibernation? According to Chris Masterjohn, a low carb diet could be the cause. Although he does not mention rT3, he warns,
“One thing to look out for is that extended low-carbing can decrease thyroid function, which will cause a bad increase in LDL-C, and be bad in itself. So be careful not to go to extremes, or if you do, to monitor thyroid function carefully.”
If low carb is the cause, then higher carb should be the cure. Indeed, Val Taylor, the owner of the yahoo rT3 group, commented that “it is possible that the rT3 could just be from a low carb diet.” She says, “I keep carbs at no lower than 60g per day for this reason.”
Cortisol and Getting “Stuck” in Hibernation
So what about temporary hyperlipidemia? Bears hibernate for winter, creating rT3, but manage to awaken in spring. Why should humans on low carb diets not be able to awaken from their hibernation? There are many people who complain of high cholesterol years after starting low carb.
A hormonal factor associated with staying in hibernation is high cortisol. It has been claimed that excessively high or low cortisol, sustained over long periods, may cause one to get “stuck” in hibernation mode. One of the moderators from the yahoo rT3 group said:
High or low cortisol can cause rT3 problems, as can chronic illness. It would be nice if correcting these things was all that was necessary. But it seems that the body gets stuck in high rT3 mode.
James LaValle & Stacy Lundin in Cracking the Metabolic Code: 9 Keys to Optimal Health wrote:
When a person experiences prolonged stress, the adrenals manufacture a large amount of the stress hormone cortisol. Cortisol inhibits the conversion of T4 to T3 and favours the conversion of T4 to rT3. If stress is prolonged a condition called reverse T3 dominance occurs and lasts even after the stress passes and cortisol levels fall. (my emphasis)
What I Did
First, I got my thyroid hormone levels tested. A blood test revealed that I had T4 at the top of the range and T3 below range. Ideally I would have tested rT3, but in Thailand the test is not available. I consulted Val Taylor, the owner of the yahoo rT3 group, who said that low T3 can cause lipids to go as high as mine have and, “as you have plenty of T4 there is no other reason for low T3 other than rT3.”
I decided to make these changes:
- Increase net carbs to ~50 grams per day. Having achieved my goals with all other metabolic markers I increased carbs, taking care that one hour postprandial blood sugar did not exceed 130 mg/dl.
- Supplement with T3 thyroid hormone.
- In case the malnutrition explanation was a factor, I began supplementing copper and eating my wife’s delicious liver pate three times per week.
I decided to supplement T3 for the following reasons:
- The surge in TC was acute and very high. It was above the optimal range in O Primitivo’s mortality data.
- I increased carbs by 20-30g/day for about a month. TC stabilized, but did not drop.
- The rT3 theory is elegant and I was eager to test my claim that the bulk of the cholesterol was due to a problem with clearance rather than ‘superabundance’.
What happened?
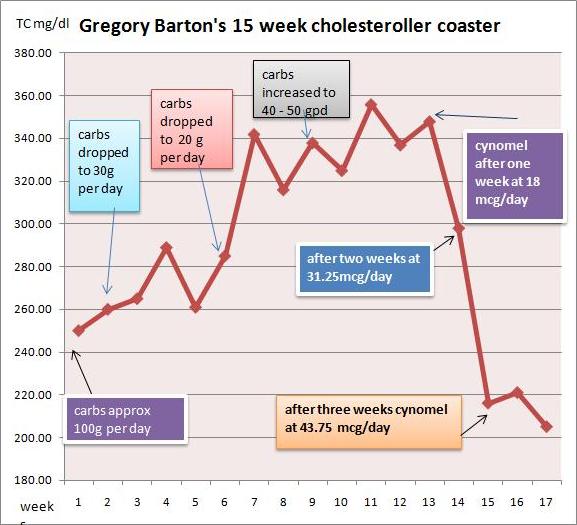
I started taking cynomel, a T3 supplement, four weeks ago. After one week triglycerides dropped from 150 to 90. After two weeks TC dropped from 350 to 300 and after another week, to 220. Last week numbers were stable.
Based on Paul’s recent series on blood lipids, especially the post Blood Lipids and Infectious Disease, Part I (Jun 21, 2011), I think TC of 220 mg/dl is optimal. As far as serum cholesterol levels are concerned, the problem has been fixed.
I believe that thyroid hormone levels were the dominant factor in my high LDL. Saturated fat intake has remained constant throughout.
My current goal is to address the root causes of the rT3 dominance and wean myself off the T3 supplement. I hope to achieve this in the next few months. My working hypothesis is that the cause of my high rT3 / low T3 was some combination of very low carb dieting, elevated cortisol (perhaps aggravated by stress over my blood lipids!), or malnutrition.
Another possibility is toxins: Dr Davis claims that such chemicals as perchlorate residues from vegetable fertilizers and polyfluorooctanoic acid, the residue of non-stick cookware, may act as inhibitors of the 5′-deiodinase enzyme that converts T4 to T3. Finally, Val Taylor claims that blood sugar over 140 mg/dl causes rT3 dominance. I couldn’t find any studies confirming this claim, and don’t believe it is relevant to my case. Val recommends low carb for diabetics to prevent cholesterol and rT3 issues but warns not to go under 60g carb per day.
Issues with T3 Supplementation
There are some factors to consider before embarking upon T3 supplementation:
- Preparation: In order to tolerate T3 supplement you have to be sure that your iron level and your adrenals are strong enough. This requires quite a bit of testing. I’ve read of people who cut corners with unpleasant results.
- Practicalities: T3 supplementation requires daily temperature monitoring in order to assess your progress. People who are on the move throughout the day would find this difficult.
- Danger: Once you get on the T3 boat you can’t get off abruptly. Your T4 level will drop below range and you will be dependent on T3 until you wean yourself off. If you stopped abruptly you could develop a nasty reaction and even become comatose.
My advice for anyone doing very low carb
As Chris Masterjohn said, in the quote above, if you are going to do very low carb, check your thyroid levels. I would add: Increase the carbs if you find your free T3 falling to the bottom of the range. It might be a good idea to test also for cortisol. A 24-hour saliva test will give you an idea whether your cortisol levels are likely to contribute to an rT3 issue. It might also be a good idea to avoid very low carb if you are suffering from stress – such as lipid anxiety!
Gregory Barton’s Conclusion
I also think my experience may help prove thyroid hormone replacement to be an alternative, and superior, therapy to statins for very high cholesterol. Statins, in the words of Chris Masterjohn,
“… do nothing to ramp up the level of cholesterol-made goodies to promote strength, proper digestion, virility and fertility. It is the vocation of thyroid hormone, by contrast, to do both.”
Paul’s Conclusion
Thanks, Gregory, for a great story and well-researched ideas. The rapid restoration of normal cholesterol levels with T3 supplementation would seem to prove that low T3 caused the high LDL levels.
However, I would be very reluctant to recommend T3 supplementation as a treatment for high LDL on Paleo. If the cause of low T3 is eating too few carbs, then supplementing T3 will greatly increase the rate of glucose utilization and aggravate the glucose deficiency.
The proper solution, I think, is simply to eat more carbs, to provide other thyroid-supporting nutrients like selenium and iodine, and allow the body to adjust its T3 levels naturally. The adjustment might be quite rapid.
In Gregory’s case, his increased carb consumption of ~50 g/day was still near our minimum, and he may have been well below the carb+protein minimum of 150 g/day (since few people naturally eat more than about 75 g protein). So I think he might have given additional carbs a try before proceeding to the T3.
Gregory had a few questions for me:
GB: What if one is glucose intolerant and can’t tolerate more than 60 grams per day without hyperglycemia or weight gain?
PJ: I think almost everyone, even diabetics, can find a way to tolerate 60 g/day dietary carbs without hyperglycemia or weight gain, and should.
GB: What if raising carbs doesn’t normalize blood lipids and one finds oneself ‘stuck in rT3 mode’?
PJ: I’m not yet convinced there is such a thing as “stuck in rT3 mode” apart from being “stuck in a diet that provides too few carbs” or “stuck in a chronic infection.” If one finds one’s self stuck while eating a balanced diet, I would look for infectious causes and address those.
Finally, if I may sound like Seth Roberts for a moment, I believe this story shows the value of a new form of science: personal experimentation, exploration of ideas on blogs, and the sharing of experiences online. It takes medical researchers years – often decades – to track down the causes of simple phenomena, such as high LDL on low carb. We’re on pace to figure out the essentials in a year.











Iodine supplementation: Should I start with 500mcg or 1 mg/day?
Hi JP,
Start with 500 mcg. If you’re sensitive, drop it down to 200-300 mcg. If you’re OK, stay with it a month and then increase to 1 mg. Be sure to take it with selenium.
“When a cell requires cholesterol, it synthesizes the necessary LDL receptors, and inserts them into the plasma membrane” http://en.wikipedia.org/wiki/LDL
How does thyroid status alter the cellular need for cholesterol?
PUFA levels affect it thusly; with more PUFA in the diet, cell membranes become less rigid and require more cholesterol for stiffening. Cells make more LDL-receptors, take in more cholesterol, and serum levels drop.
However, to fuel this need, the liver is synthesizing more cholesterol than before, and there is now more cholesterol content in the body.
Presumably if PUFA intake drops again the cholesterol will go back into circulation before the liver clears it, so there will be a rebound hypercholesterolaemia.
George, I’ve been thinking about the role of LDL receptors, and have been paying close attention to the cholesterol dialogue going on Attia’s site.
This is a very interesting idea, but does it rely on the view that cholesterol is being manufactured in the liver and shipped to peripheral cells that need it? I used to think like this and it does happen to an extent, but based on Thomas Dayspring’s lecture (and some of stuff I had read in the past but couldnt completely digest), the newer view is that cholesterol is mostly synthesized outside the liver and shipped back to the liver. The LDL-particle is actually mostly involved in Reverse Cholesterol Transport, mediated by another receptor that doesnt involve endocytosis and thus does not result in particle clearance from the bloodstream.
So if PUFA causes upregulation in LDL-R, then presumably the primary effect is in the liver, since 85% of LDL-R activity is in the liver. So maybe its the liver that needs the cholesterol for cell stiffening?
Ann Clin Lab Sci. 2007 Autumn;37(4):343-8.
Low serum LDL cholesterol levels and the risk of fever, sepsis, and malignancy.
Shor R, Wainstein J, Oz D, Boaz M, Matas Z, Fux A, Halabe A.
Source
Department of Internal Medicine, The Edith Wolfson Medical Center, Sackler School of Medicine, Tel Aviv University, Holon, Israel.
Abstract
Lipid lowering therapy of serum LDL cholesterol (LDL) has proved beneficial in reducing cardiovascular morbidity and mortality. Lately the recommended target LDL level in very high risk patients was reduced to <70 mg/dl, raising the question of what the price of such a low level will be. To elucidate this concern, we investigated the associations of low serum LDL cholesterol levels (< or = 70 mg/dl) and the incidences of fever, sepsis, and malignancy. Retrospective analysis of 203 patients' charts was carried out. Patients were divided into 2 groups: Group 1 (n = 79) had serum LDL levels 70 mg/dl. The first group demonstrated increased odds of hematological cancer by more than 15-fold (OR 15.7, 95% CI 1.78-138.4, p = 0.01). Each 1 mg/dl increase in LDL was associated with a relative reduction of 2.4% in the odds of hematological cancer (OR 0.976, 95% CI 0.956-0.997, p = 0.026). Low LDL levels also increased the odds of fever and sepsis between the groups (OR 5.3, 95% CI 1.8-15.7, p = 0.02). In summary, low serum LDL cholesterol level was associated with increased risks of hematological cancer, fever, and sepsis.
PMID:
18000291
[PubMed – indexed for MEDLINE]
Hi George,
Very interesting idea about how PUFA-SaFA affect LDL receptor levels. Might be the main factor.
It’s absurd to lower LDL levels below 70 mg/dl. LDL has important immune functions and this is just wrecking immune function.
It’s very interesting that blood cancers were increased 15-fold with low serum cholesterol. That’s a huge effect.
Thanks!
The beauty of it is, such simple mechanical overviews do not require any knowledge of hormones or gene expression to understand and apply to one’s diet.
Am J Clin Nutr. 1997 Aug;66(2):438-46.
Regulation of cholesterol biosynthesis by diet in humans.
Jones PJ.
Abstract
Biosynthesis of cholesterol represents a major input into whole-body pools; however, its regulation has been difficult to study in humans because of limitations in methodologies. The present objectives are to compare available techniques for measuring this process and examine how dietary factors alter human cholesterol biosynthesis. Review of existing techniques suggests that mass isotopomer distribution analysis and deuterium incorporation approaches offer advantages over other methods. Dietary factors influencing human cholesterol synthesis include energy restriction, meal frequency, dietary fat type, and cholesterol and phytosterol content. Food deprivation for as short as 24 h results in almost complete cessation of cholesterol biosynthesis. Similarly, increased meal frequency patterns are associated with a substantial depression in synthesis. In contrast, consumption of oils rich in polyunsaturated fatty acids, despite reducing circulating concentrations, increases the cholesterol synthesis rate compared with other fats. Stepwise addition of dietary cholesterol is associated with only a modest decline in cholesterogenesis while raising plasma concentrations slightly. It can be concluded that synthesis, as a contributor to circulating cholesterol concentrations, is sensitive to many dietary factors. Energy deprivation results in the greatest decline in synthesis, likely accounting for the beneficial decline in circulating cholesterol concentrations observed with weight loss.
PMID:
9250128
[PubMed – indexed for MEDLIN
Seems like prior patient death from hematological cancer, fever, or sepsis as a result of lowering LDL to <70 mg/dl could account for some of the reported reduced cardiovascular mortality correlated with "lipid lowering therapy of LDL".
re: PUFA vs. SaFA
Chris Masterjohn discusses how only replacing PUFA with SaFA increases cholesterol over the long term. Supported by a controlled setting of the LA Veterans Administration Hospital Study.
Also discusses the Stephan Guyenet referenced observational study and the hypothesis that increased SaFA increases cholesterol over short term, but normalizes over the long term. There are confounders with the natural setting.
Starts at 6:45:
http://www.bulletproofexec.com/podcast-16-everything-you-need-to-know-about-saturated-fat-cholesterol-with-chris-masterjohn/
Thanks,
Mark
Thanks for that link.
The interesting thing is that with high-PUFA diets there is more total cholesterol in the body, just less in the blood.
This could mean there is more in your artery walls, as this wouldn’t be picked up by lipid testing.
SaFA increases cholesterol over the short term – that would be consistent with rebound hypercholesterolaemia when PUFAs are replaced (gradually) and the cells don’t need so much cholesterol.
This might last weeks or months.
Here is the paper on PUFA (and low cholesterol diets) increasing cholesterol production as well as LDL uptake. MUFA lowers it (and presumably SaFA)
http://www.ajcn.org/content/66/2/438.full.pdf+html
Robb Wolff cited a study in a recent post which makes a similar claim about the danger of low HDL:
http://www.ncbi.nlm.nih.gov/pubmed/16096442
In the post Robb cites the cholesterol numbers of a person who was hospitalized with sepsis to show how the cholesterol was depleted.
Before hospitalization:
Total – 226
HDL – 58
TG – 60
Cholesterol while hospitalized, Jan 2012:
Total – 98
HDL – 15
TG – 97
He also describes how cholesterol binds to lipopolysacharides (LPS) – a component of the outer membrane of gram negative bacteria:
“…one of the first lines of defense against the effects of LPS is actually LDL/HDL cholesterol, which binds to LPS and helps to remove it from circulation. Hence the inclusion of LDL/HDL cholesterol as part of innate immunity.”
http://www.robbwolf.com/2012/03/09/paleo-diet-inflammation-metformin/
Paul , I am very worried about my son, he is 46 years old and he has addisons disease. His Dr. put him on cortisone but he never gives him blood or saliva tests. He is never feeling well and I wondered if his thyroid is normal
TSH 4.09 mIU/L range 0.34-5.60
T4 Free 9 pmol/L range 7.5 – 21.1
T3 Free 4.4 pmol/L range 3.8 – 6.0
Chol- H8.43nmol/L range 3.80-5.20
Trig H2.66mmol/Lrange 0.60-1.70
HDL 1.73 mmol/Lrange 1.00-1.80
LDL H5.49 mmol/L range 2.00-3.40
Cholesterol/HDL ratio 4.87 0.00-5.00
Can you give me any advice about what tests he should ask for and how he can improve his health.
Thank You
Hi Shomna,
The most important thing is to eat a good diet. With Addison’s he can’t cope with carb intake that deviates much from what his body needs, so he should try to eat close to those needs — 30% to 40% carbs, 15% protein, about 50% fat by calories. His diet should follow our food plate. Keep omega-6 fats down.
Those thyroid numbers are consistent with a mild hypothyroidism. Does he have symptoms, such as cold intolerance? He might well benefit from a low dose of levothyroxine.
High cholesterol can be caused by hypothyroidism, also by other factors. Fix the diet and address the hypothyroidism and hopefully that will improve.
Re additional testing, I prefer not to compete with doctors in dealing with specific cases. However, Wikipedia can give you ideas: http://en.wikipedia.org/wiki/Addison%27s_disease. Scroll down to the “Testing” section. Also look at “Causes” with a focus on infectious causes and think about possible tests for infections. From that perspective, I highly recommend PCR-based DNA stool tests, eg http://www.metametrix.com/test-menu/profiles/gastrointestinal-function/gi-effects-microbial-ecology. This may often reveal a treatable infection.
Best, Paul
Hi Paul – I’m trying to take as much as possible from all this incredible information to understand my own situation, but it is a bit overwhelming! I’m very concerned by my recent test results and was hoping that you might be able to provide me with some direction. I’ll make this as brief as possible…
Female, 33yrs old, 5 ft tall, active
History: “healthy by conventional wisdom” diet – low to fat-free, mod-high protein, mod carb Seemingly healthy with weight around 110lb and avg TC 175, LDL 85, HDL 75.
2011-Jan 2012: Paleo VLC, high fat from meat, avo, fish, olive oil. Seemingly healthy with weight down to 95 and TC 224 LDL 91 HDL 129. IBS and Amennhorea.
Jan 2012: Stopped BCP (after 15 yrs) and added liver to the diet. Everything started going wrong! 2 months later (3/15/12), had some Metametrix testing:
TC 371 LDL 226 HDL 132
T3 1.6, T4 92.26, TSH 1.18, FT3 4.39, FT4 15.96
Blood Sugar 76
H Pylori, Candida, fatty acid oxidation, DNA oxidation, among others
As of 3/15, I started GAPS (lots of sat fats, butter, sour cream, bone broth, etc.) and supp with C, E, Selenium, APA and herbal liver support, and chol is getting worse! (although digestion feels better) testing:
TC 463 LDL 351 HDL 96
TSH .51 FT4 1
borderline low testosterone, DHEA and low etradiol (14), borderline high SHBG
I would greatly appreciate your advice. I’ve done some research and am just hoping it is not FH. Could it be thyroid related? Iodine or copper deficiency?
Thanks in advance for your help!
Hi JF,
I’m a bit confused. What is BCP?
High LDL on low carb is most often hypothyroidism. FT4 is low (correct? you know the reference range?) but TSH is also low – that suggests a central hypothyroidism perhaps, or something odd. I think this needs investigation by a specialist.
In the meantime, you could consider treating the H pylori. It contributes to various diseases including autoimmune thyroid disease (http://www.ncbi.nlm.nih.gov/pubmed/22426167), dyslipidemia (http://www.ncbi.nlm.nih.gov/pubmed/19522019), and diabetes (ibid).
Best, Paul
Hi Paul,
Olive leaf extract seems to be effective against H pylori, while preserving the gut flora:
http://www.ncbi.nlm.nih.gov/pubmed/19135874
Best,
Mario.
Hi Paul – Sorry for the confusion, was trying to keep it short. I was referring to Oral Contraceptives as this, along with an increase in liver consumption, was the only change made prior to the high LDL readings.
As for thyroid hormones, the range for FT4 seems to be .7-1.8. Mine was 1.24, then 1.00. (Do these contstitue as low?) The range for TSH seems to be .25-5.00. Mine was 1.18, then .61.
I actually just got tested to see if the H. Pylori is active and will definitely address this if need be.
Thanks for your time. I look forward to any other thoughts/recommendations you might have. Sincerely, Jaclyn
Hi Jaclyn,
Well, it doesn’t seem like you are hypothyroid. I would try increasing carbs with “safe starches” and sugary foods like beets, and treat the H pylori.
I wonder if the contraceptive pills might have suppressed liver fat clearance for 15 years and now you’re getting a lot released.
It’s an odd pattern. Let me know how things progress.
Best, Paul
I am so scared b/c of new lab values. I started PHD in Jan hoping to help my Hasi’s and high lipids, but instead of goind down everything went up. I am looking for solutions besides pharma meds, which the MD not doubt will put me on. Any input from anyone would be worth exploring, though I have tried many, have had 15+ yrs with high lipids. Current TC 416,HDL 54,LDL 300 Tri 308,VLDL 62, TSH 3.300 and glucose 122 which is a new high for me. On most PHD supplements and iodine/iodide and do feel better. I have read that if you take care of your Hasi’s first then everything else might fall into place? Thank you for any thoughts. Donna
Hi Donna,
Feeling better is important.
First, are you taking replacement thyroid hormone? Is the dose correct? Normally TSH will be lower with thyroid hormone replacement.
Second, are you eating enough carbs? About a pound a day of safe starches is what we recommend. That will typically be 400 to 600 calories. Low carb intake can exacerbate hypothyroidism, and cause elevated fasting glucose. See our hypothyroid category.
Third, I would chase possible infections. Dyslipidemia, hypothyroidism, and poor glucose regulation are all caused by infections. You might get a stool test to start with, google Metametrix Microbial Ecology for one I would recommend. Then look to treat whatever you find.
Did you start the iodine at a low level and increase slowly? Too much iodine too soon can cause or exacerbate hypothyroidism. Also, too much selenium can do it. You might try cutting out selenium supplements for a while. Our diet is fairly selenium rich so it shouldn’t be an issue.
I think you want to keep investigating potential causes and chipping away at them. Keep me posted.
Best, Paul
Thank you for giving me more leads to follow. No thyroid hormone taken, have in the past but MD took me off. Yes, I believe on carbs 1 1/2 cup white rice a day or 1 potatoe. Yes, iodine on a slow start up, I am not even up to 1 full tab yet, will cease selenium. I am on the path to your infection lead.
Warm regards, Donna
Hi Donna,
I think you should add more carbs. 1.5 cups rice weighs about half a pound and has about 270 carb calories, 1 potato – depends on the size, but a large 300 g potato has about 250 carb calories.
You might stick with whatever iodine dose you’re at right now for a while as you experiment with other things. You don’t want to change too many things at once or it gets confusing.
I would definitely ask for thyroid replacement hormone.
Best, Paul
Hi Paul — I’m looking for a connection between raising carbs (to PHD levels) and better thyroid lab work. Should higher carbs increase serum T3 levels? I would love to find a way to improve my thyroid functioning.
Hi Kathy,
Yes, on low carb diets adding carbs will tend to raise T3 levels. This is because the body lowers T3 to conserve glucose when it is scarce.
If you look back in our Hypothyroidism series or search on “Low Carb and the Thyroid”, you’ll see some posts discussing this.
Best, Paul
Anyone have any thoughts about the appropriate testing frequency for lipids and thyroid and the length of time which a dietary milieu will lead to a stable reading?
I recall reading somewhere that the standard deviation of daily cholesterol readings could be in the order of 5% (perhaps a bit less), but the SD of serum TG (triglycerides) readings was much higher. With respect to the variability in thyroid level testing, I have no clue.
But I haven’t seen any data about the time frame required for a dietary change to cause stabilization in a test reading. Seems like LDL takes 3 weeks to stabilize at a different T3 level, at least in 1 patient.
For practical purposes, how long should you try a dietary change before you retest, to see if you are going in the right direction? For example, if you wanted to measure your response to changes in increased carbs, or changes in saturated fat, or consumption of plant phytosterols (a VERY BAD IDEA, BTW), how long should you wait before you retest?
In my experience anything from a week to a month will reflect changes in diet. The caveat would be Chris Masterjohn’s advice that if you are losing weight rapidly you should wait until your weight stabilizes before testing.
I will post a short comment in the next week or two detailing:
i. what happened when I weaned off T3 and
ii. what happened when I followed Paul’s suggestion of eating 100g carbs from starch per day.
gb
Thx Greg-
Your case study was incredibly helpful. It inspired me to collect a bit more data and I plan to offer up my own experiences in the hopes that it might help someone else down the road. Thx again for sharing!
Ditto what Ed said about the helpful info, Greg. Looking forward to your followup comment. I have mild Hashimotos and wondering if I need to be on any thyroid hormone. I’m guessing it will be impossible to find a doc who is tuned in to all this stuff.
I see there is a comment from Mario Iwakura earlier today. I appreciated his posts on hypothyroidism (Iodine and Hashimoto’s Thyroiditis, parts 1 and 2, May 2011) and am curious – Mario, how are you doing with your hypothyroidism and have you changed anything in your treatment plan? Thanks.
Mary,
I’m doing fine and have not changed anything.
Best,
Mario.
Lower LDL with reintroduction of carbs (100g/day)
in new lipid results – previous figures (ZERO CARB) in brackets.
Total-Ch 261.3 (347.1)
LDL 183.3 (261.3)
HDL 63.57 (64.35)
TG 71.2 (115.7)
Great improvement George!
George,
Very encouraging… I had my TC go from mid-200’s up to 400 on a VLC diet. After frantically looking for explanations I found this link and started some carb introduction. I had no idea what my thyroid levels were, so I went to my doc to get a prescription. By the time I got the necessary paperwork, 2 weeks had passed since my 400 TC reading, and thankfully my TC had already started going in the right direction… 340. My thyroid panels all came within reference range (so of course my doctor completely dismisses the notion that carbohydrate restriction can induce low thyroid-mediated LDL-receptor downregulation), but my FT3/rT3 was a bit lower than most people recommend (14.5 vs >20 recommendation). I’m hoping that with a little more time on carbohydrates plus a little thyroid supplementation (selenium+iodide), I can get my lipids back to a more reasonable range.
I’ve promised Paul to provide a nice case writeup after I get a few more data points, but your data is another confirmation that adding some starches can help get the LDL-receptors activated again.
Thanks for sharing.
I also wonder if more olive oil in place of hard fats would have made a difference. MUFA is supposed to promote LDL-R.
George,
Wonderful results. After a long time VLC, did you have any trouble reintroducing the carbs? Did you go gradually or all at once to 100g/day? Did you monitor blood sugar?
I ask because after almost a year of VLC and many of the common problems (low T3, high rT3, high LDL), I would very much like to reintroduce carbs, but my blood sugar spikes whenever I try. Not sure if this is a hump to get over or a sign to back off.
Thanks!
MM-
Cant speak for George but I was a bit paranoid starting some carb introduction, but I gradually increased over a period of 1 week and it didnt seem to cause a problem or any weight gain.
For me, sweet potato doesnt seem to spike my glucose readings as much as an equivalent amount of white rice, and it does seem to make a difference if you eat it in combination with something… I typically just add some sweet potato to my lunch salad.
Also, I suspect the introduction of some starches actually may have increased my insulin sensitivity. My morning fasting readings on average seem to have gone down after a few weeks since carb introduction.
I think this is probably a predictable effect. There are many who have written after prolonged periods of carb restriction, their FBG tends to rise and people say you should eat carbs for a few days if you are thinking of getting an Oral Glucose Tolerance test.
Hope this helps… good luck!
Yeah, I found rice too much at first. Potatoes and especially taro were better. Dhal was OK too. (hulled dhal soaked, rinsed and very well cooked is I think the best dried legume)
You can expect about 2 days of physiological insulin resistance at first, so gradually is probably best.
Thank you, Ed and George!
I will proceed slowly with sweet potato or taro and let you know how it goes.
p.s. Has anyone noticed better/worse carb handling at different times of day? My blood sugar control is worse earlier in the day, perhaps due to higher cortisol. Because of this, my inclination is to add the carbs at dinner.
@mm-
Interesting idea about timing glucose handling… but if you are worried about post-prandial spikes, maybe you should consider insoluble fiber (psyllium or glucomann)? Look at the glucose/insulin curves under this study (there are others that seem to confirm these effects):
http://www.ajcn.org/content/53/6/1431.full.pdf
For laughs, look at the controlled diet they are feeding T2D’s… white bread, corn flakes, orange juice…. makes my blood proteins glycate just thinking about it!
@mm
Probably wisest at first to add carbs at dinner. They can be in booth meals if eating in an 8-hour window. I think with intermittent fasting it’s a good idea to work out where you want your body clock set. For me 10am – 6 pm is eqidistant from my sleeping times and seems to work well.
Look at the illustration here:
http://www.cell.com/cell-metabolism/abstract/S1550-4131(12)00189-1
article here:
http://www.salk.edu/news/pressrelease_details.php?press_id=560
How I cook taro: this has oxalic acid so needs to be cooked well; I cut into small (1cm2) cubes and boil down till the water is thick and starchy, with a little salt. Takes up to 45 minutes. Done like this it is the tastiest of starches.
@George-
Wow….where do you pull this stuff from? Perhaps you should start a blog too! Perhaps I should start skipping breakfast.
Regarding your lipid improvement, was your only diet change a starch addition, implying the LDL-lowering effect was primarily due to T3-mediated upregulation in LDL-R activity, or some other change such as substitution of SFA for PUFA or MUFA?
I also find it interesting that your TG went down while increasing carbohydrates. If you have any good sources to read up on TG and VLDL formation that would be helpful. Thx!
And pretty much where I’d want to be! Also no more peripheral sensations or eye discomfort.
A little less protein, as you say, is a good thing. And intermittent fasting (8 hour window) – fantastic.
The lower TG could be because I’d started the intermittent fasting, and the second test was later in the day.
The LDL effect was due to more carbs, less protein and fat to accomodate it, I’m sure.
There’s an interplay between thyroid and PUFA (and possibly MUFA) both upregulating LDL-R.
So I’d be careful using oils to lower LDL if you were already in a T3r state; it could theoretically either raise or lower T3. But the carbs, by providing a substrate for increased metabolic rate, free up the T3.
Unfortunately I am not yet adept enough at using my computer to host a blog better than this: http://hopefulgeranium.blogspot.co.nz/
I mean to get with it one day, but have busy life(http://www.youtube.com/watch?list=HL1338332735&feature=player_detailpage&v=lRk-ZeCefec), one finger typing skills, and low tolerance for screentime.
Paul and Shou-Ching
You may almost get tired of people thanking you, but reading and re-reading your book and your blog, as well as the intelligent comments from your readers, has to be one of the most rewarding things I’ve ever encountered. I’ve been looking for 25 years for this information, and here it is, complete with ongoing refinements as more nuances become understood.
I’ll continue to follow closely, and with great appreciation. Thank you so much.
This was very interesting for me. I have low t3 (lowest number of the range, almost out) and t4 on the higher side of the range. I have been very low carb for a few years, as low as 10-20g per day. I have a hard time increasing carbs to even 25-30g, as I don’t eat any grains and very little dairy. I eat protein and healthy fats, some veggies, hardly ever any fruit. I try to increase veggies but how many cups of broccoli can someone eat for dinner? And it doesn’t raise my carb grams that much. What can I do? I think I need to increase carbs as you say. Can anyone help with suggestions on doing that without grains, sugar, and fruit? I eat a couple of brazil nuts a day for selenium. Is that enough? And I have a dulse powder for iodine. I add it to my water every other day. Just started doing this after I found out about the t3.
Potatoes and sweet potatoes and winter squashes and taro work well. We recommend white rice also.
Yes; the whole squash family, pumpkin, kumi kumi, courgette, etc. are probably the easiest way to re-introduce carbs at first, they are a relatively low carb source with plenty of fibre and water and it is hard to go over 50g in a meal.
Thank you. Forgot to add that I have high cholesterol, too, and didn’t before when I was low fat (3 years ago). Here are my numbers for thyroid and chol, in case you might shed some light:
:
Free t4 1.45 (range 0.82-1.60)
TSH, 2.530 (0.270-4.200)
T-3 total 0.81 (0.80-2.00)
Total Chol: 244 (range <200)
TRiglycerides 52 (<150)
Total non HDL Chol 169 (<160)
Lp(a) Chol 17.0 (<10.0)
Real LDL CHol 133 (<100)
Total LDL-C 155 (<130)
Large Buoyant Pattern A LDL (good, right?)
Hi Claudia,
Yes, as George says, your cholesterol is now normal. See http://perfecthealthdiet.com/2011/06/blood-lipids-and-infectious-disease-part-i/ and other posts in our LDL/HDL/cholesterol category.
Your thyroid numbers are consistent with eating too few carbs.
Hi Claudia,
A comment from Paul that summarizes it:
http://perfecthealthdiet.com/2012/02/ris-a-la-mande/comment-page-1/#comment-54344
Ideal profile: Total cholesterol, 200-240 mg/dl; HDL, >60 mg/dl; trigs, <80 mg/dl. LDL can cover a broad range consistent with health, but LDL numbers that are healthy in some people can be unhealthy in others, so I don’t see it as having a well-defined “normal” range, but generally speaking 80 to 160 mg/dl can be consistent with good health.
Also, Chris Masterjohn has been consistently indicating that a key marker is TC:HDL <3 ideally, <4 pretty good.
Thanks,
Mark
Did you say HIGH cholesterol?
Imagine that there are many possible causes of death and heart attacks is just one of these.
Imagine that the cholesterol level associated with the lowest incidence of each cause of death is slightly different.
I’ve heard that cholesterol of 244 is perilously close to the figure associated with the lowest odds of early death from all causes.
One study showed that keeping
(LDL – HDL)/LDL lower than 1 – [.005(SystolicBloodPressure – 50)]
provides safety against heart attack and stroke.
@George Henderson
You might find my question and subsequent answer at Paleohacks interesting :
http://paleohacks.com/questions/117484/ldl-high-increase-your-cholesterol-intake-the-elephant-in-the-room#axzz1vtoyLMPT
I’ve now replicated the results on more than six occasions by both regular lab tests and my Cardiochek PA meter.
Latest results from yesterday are:
TC 270 (7.01)
HDL 97 (2.52)
TG 51 (0.58)
LDL 163 (4.23) calc.
Reduced by eating 850mg of cholesterol in yesterday’s diet (eggs, butter, salmon)
Good stuff Dave B
It occurs to me that if there is cholesterol in chylomicrons (from diet) any need is partially met from that and liver needn’t contribute as much.
The same may be true for phospholipids (also lower LDL), vitamin A and D, and other lipids produced or released by the liver.
Cholesterol inhibits HMG-CoA reductase
– it’s nature’s statin.
@George Henderson
Thanks for this – I researched your comments and discovered this at http://www.realfooduniversity.com
“New research published in November of 2007 at the University of Connecticut indicates that a diet low in carbs with a cholesterol challenge (addition) of 640 mg per day, or 3 eggs worth, significantly reduces HMG-CoA reductase, mimicking statins. According to the researchers, “The findings indicate that dietary cholesterol during a weight loss intervention alters the expression of genes regulating cholesterol homeostasis.”(3) The same researchers later showed, in two separate studies, that adding cholesterol to a low carb diet raises HDL (4) and modulates inflammation in overweight individuals (5).”
This morning I was trying to discuss my findings with my GP who looked at me in total disbelief when I suggested that eating more cholesterol had reduced my “bad” numbers. She’s referred me to a “lipid expert” who I’ll be seeing in early July.
Incidentally, my inflammatory markers have all reduced since the decrease in LDL:
ESR:3 (was 6), Hs-CRP:0.2 (0.4), Homocysteine:5.5 (11.6)
I had posted this on wheatbellyblog not too long ago in light of the info I got from my NMR LipoProfile test. It shocked me how high my LDL-P is. The blog post on Wheat Belly was about how weight loss can make your LDL increase just because fats are being released into blood as you burn it so it is nothing to worry about while you lose weight if your lipid profiles are all crazy.
This is what I wrote:
“I got my NMR LipoProfile test results in. And I thought they were going to be superb numbers. I had been eating LC strictly for 5 months and lost 30 lbs mostly fat. The last month though, I was leveling out on weight loss. Then the LDL-P count came in at over 3000. That’s 1000 over the highest risk and 2000 over the lowest risk category! Every other numbers seems to be excellent or decent. Including LDL particle size (pattern A).
[…]
Regardless though, the number still scares me and makes me want to get additional testing to find out my thyroid function levels and what not (which I’m just learning about today). I was reading that perhaps my T3 levels were low so my LDL was having a hard time clearing out of the blood.
Here is a copy and paste from that thread. I know I probably shouldn’t worry too too much, but it is just hard to once you start worrying.
LDL-P 3132 !!!! (>2000 is highest risk)
LCL-C 323 (>189 highest risk but not concerned about this number)
HDL-C 63 (This is really good >40)
Trig 62 (Also very good 30.5)
Small LDL 217 (average is 20.5 for large pattern A)
Insulin Resistance
Large VLDL-P 0.9 (Very good. 7.3 is highest percentile in favor of sensitivity so this is good)
VLDL Size Unknown – “VLDL concentration too low to allow determination of VLDL Size. Low VLDL concentration contributes minimally to the LP-IR score.”
LDL Size 21.7 (>21.2 best percentile)
HDL Size 9.2 (50th percentile)
LP-IR Score 15 (best score is less than 27, worst is over 63 – so this is excellent)”
Dr David replied:
“Unfortunately, this is not the pattern of weight loss, but of other issues.
Yes, thyroid might be an issue, but it would be unusual to be the sole cause. Consider apo E4 and/or heterozygous familial hypercholesterolemia. You will require an intelligent assessment for ongoing decision-making. Beware of the conventional thinkers.”
Which scared the living heck out of me. I was hoping it was something I would just be able to fix with supplementation (iodine, selenium, etc) and more calories and maybe more carbs to increase my T3 after reading your blog. But he is right, it isn’t like my triglycerides and such are going crazy. In fact, most of my numbers are superb. Or at least in the average range for the not so amazing ones. But the LDL-P scares me to death. LDL-C is something I ignore due to research suggesting LDL-P is the culprit in heart disease not LDL-C.
What are your thoughts on my lipids and what Dr David said about this probably not being just a case of bad thyroid? Any insight would be amazing. I’ve been freaking out all day (which isn’t helping my stress/cortisol levels!). I really was expecting fantastic numbers to be kicked in the but with these results.
Thanks!
PS. I just got blood drawn out of panic today for TSH and free T4. I had also requested free t3 but I think he misheard me. So I emailed my doc and asked him if he could call the lab and add free t3 to my tests using the same specimen. Hopefully he does! If he does and I get results back, I’ll post them here.
The wheat belly post here: http://www.wheatbellyblog.com/2012/06/i-lost-weight-and-my-cholesterol-went-up/comment-page-1/#comment-10565
Hi Derek,
Try adding carbs, 1 lb of safe starches per day, and supplementing selenium (100 mcg/day) and iodine (low dose first, say 225 mcg, double the dose once per month) and zinc (15 mg per day) and copper (beef liver, 1/4 lb/week).
Then get retested in a month or two – just LDL, not the expensive profile.
It will probably be much better.
Best, Paul
Thanks Paul! Are my numbers in line with something having to do with thyroid? Dr David seems to think that isn’t the only culplrit with how my numbers look for whatever reason (suggesting maybe apo E4 and/or heterozygous familial hypercholesterolemia). Do you see this correlation with my numbers?
Also, My doctor ordered tests. I asked for free T3 but he apparently didn’t add it. Here are the numbers… I have no idea what to make of them since Free T3 is what I REALLY wanted to see:
Free T4 1.3
TSH 1.88
He also tested sodium among other things in a “Chem-7”. Is that ANY indication of iodine by any chance?
Sodium 140 (133 – 145)
@Derek-
Had to chime in… just read your posts on wheat belly and the lcforum. You and I had the same experiences… eerily similar. Judging from the breadth of comments on this thread and others in the paleo/lc spheres, rising LDL on a LC diet may be unusual, but clearly NOT AN ISOLATED phenomenon.
I’ve read a TON of stuff over the last month or so; and Attia’s cholesterol discussion along with his references were extremely timely for filling in some of my cholesterol knowledge gaps. I’m not sure if I agree with his conclusions, but I am in agreement that LDL-P is a far better risk marker than LDL-C.
I’ll have more to say in a week or two… I’m getting a new set of tests this weekend (after about 5 weeks of adding safe starches + more recent efforts to consciously get more iodine and selenium via food).
First off, as a gesture to Jaminet and this great thread, I would suggest $10 spent on his book. Frankly, it’s an excellent read… I wouldn’t have been ready to start my nutritional journey with his book, but after being LC for over a year and having learned so much already, I can say it’s one of, if not the best nutrition books I have read. It’s also a far better $10 kindle health investment than a $100+ investment on 1 NMR or VAP profile.
That being said, let me share a few of my findings so far:
1) there is ample evidence (gathered outside of Jaminet’s book) that carb restriction will mimic the calorie restriction effects on thyroid hormone balance.
2) T3 and rT3 levels can directly influence LDL-P and LDL-C levels because they mediate LDL-Receptor activity.
3) LDL-R activity is what you want to focus on… anything that down regulates that, in terms of expression, catabolism, or binding affinity to your apoB is something that will influence your LDL-P. The production side of the apoB particles can be investigated, but since your TG and VLDL is low, it doesnt seem that you have excess particle production… it seems more plausible that you have an apoB clearance problem; and thats all via the LDL-R.
4)Thyroid panels seem difficult to interpret. My TSH, FT4 (which are almost identical to yours), as well as FT3 and rT3 are all within reference range. My doctor says my thyroid is fine. Yet my FT3/rT3 ratio is 14.5, which is lower than recommended by various thyroid blogs. I have not seen any published, or more credible literature that supports the notion that a ratio of 20 is the magical number to shoot for, so this is all I have to go on for now. If anyone out there can provide some useful ratio guidelines supported by medical literature, let me know!
5) by the time i had my thyroid tested, 2 weeks had gone by and I had already started adding safe starches. So my “normal” ranges may have been a result of some improvement. Incidentally, my lipid panel improved by 60… almost entirely in LDL subfraction, in those 2 weeks (5 more weeks have since passed so I am anxious to get another reading).
6) Although I have no new lab results, anecdotally I can share the following: a) my weight has remained stable; perhaps +/- 1-2 lbs… i was so carbophobic after my LC success that i couldnt ever imagine eating a banana again… turns out it wont kill ya!
b) my body temp seems higher; i spent the whole winter feeling cold (my wife didnt want to snuggle). signs of improved thyroid.
Anyways, if you want to take this discussion offline with someone with very similar labs, I’m at mail.edward.lee@gmail.com.
Here’s some info i dug up on rT3 that may be of interest to some;
….on the question of the half life of rT3;
This article quotes 3 hours “This might be explained by a short half-life of rT3 (around 3 h vs. around 24 h for T3)”, http://jcem.endojournals.org/content/90/8/4559.full
& this article quotes 4 hours, http://www.pathologyoutlines.com/chemistry.html
& something else to be aware of, is that Serum TSH, T3 and FT3 follow a diurnal rhythm (T4 & FT4 has a similar rhythm but it is not statistical significance). Therefore it may be feasible that rT3 may also follow a diurnal rhythm.
References:
Serum TSH levels exhibit a diurnal variation with the peak occurring during the night and the nadir, which approximates to 50% of the peak value, occurring between 1000 and 1600 hours.[123,124] http://www.medscape.com/viewarticle/452667_4
Serum TSH, T3 and FT3 values in the early morning were significantly higher than during the daytime, but such change was not observed in serum T4 and FT4. http://sciencelinks.jp/j-east/display.php?id=000020021002A0288084
A practical consequence is that blood samples for TSH measurements in patients with moderately elevated TSH levels are best taken after 1100 h, when the low day levels are reached. http://www.ncbi.nlm.nih.gov/pubmed/985825
Ten normal young males were investigated in order to examine diurnal and short-term variations in serum TSH and serum thyroid hormones. In five subjects blood samples were obtained every 30 min during a 24 h period of daily life. A synchronous diurnal rhythm was found for free T3 and serum TSH with low levels in the day-time and higher levels at night. The mean increase from day to night was 15 and 140 per cent, respectively. There was a tendency to a similar rhythm in free T4, but the increase of 7 per cent fell short of statistical significance.
In the other five men blood samples were obtained every 5 min in a 6 to 7 h period starting within the interval from 19.15 to 22.00 h. A significant regular variation with a cycle-length of half an hour was found in TSH, free T3 and free T4. This rhythm accounted for a significant part of the total variation in the levels of TSH, free T3 and free T4. The mean amplitude of the short-term variation is 13, 15 and 11 per cent of the mean level of the respective hormones. The data suggest a pulsatile release of hormones from the thyroid gland governed by a pulsatile TSH secretion. http://www.eje-online.org/content/89/3/659
Very Useful Information. Thanks.
Gives me reason to re-evaluate whether its worth the expense for a full set of thyroid panels. rT3, in particular, seems expensive, as it doesnt normally come in any packaged panel.
So the bottom line is that if you are trouble shooting your rising LDL with the hypothesis that your T3 and rT3 levels are downregulating LDL-R activity and therefore apoB particle clearance from the bloodstream, that T3 and rT3 lab measurements may not reveal a clear story. If you rely on lab measurements, it’s best to take a series of measurements at the same time of day and monitor changes over time, compared to looking at absolute levels.
Thanks!
And some more stuff on rT3;
I found this comment by Dr. John C. Lowe on rT3 and related ‘syndromes’ in an interview with Dr. John C. Lowe here; http://toopoopedtoparticipate.com/blog/dr-john-c-lowe-speaks/
“In my opinion, the reverse T3 has served us best in diagnosing a condition that has a variety of names: “euthyroid sick syndrome,” “low T3 syndrome,” and “non-thyroidal illness syndrome.” The word “euthyroid,” of course, means that the person has in-range TSH, T4, and T3 levels. In this condition, the hypothalamus secretes less TRH, the pituitary secretes less TSH, and less thyroid hormone is transported into cells. Also, the enzyme called “5-prime deiodinase,” which converts T4 to T3, becomes far less active. Another enzyme, “5 deiodinase” (no “prime” as a modifier) becomes more active and converts more T4 to reverse T3.
The words “sick syndrome” is somewhat misleading. That term is used presumably because the condition was first identified in sick people, such as anorexics and hospitalized patients in critical condition. Studies showed that the patients had steeply raised cortisol levels. It’s their high cortisol levels that inhibit the enzyme (5-prime deiodinase) that converts T4 to T3.
I’ve found no evidence that this condition becomes chronic, as Dr. Dennis Wilson proposed. Instead, the research literature shows that within a week or two, TSH secretion increases and 5-prime deiodinase escapes the inhibition by cortisol. This happens even though the person’s cortisol levels remain high. For example, if the person undergoes prolonged treatment with prednisone, within a week or two, the TSH level returns to its previous level and 5-prime deiodinase becomes normally active again.
Old studies show that on average, most people convert more than 50% of their T4 to reverse T3; correspondingly, they convert less than 50% of T4 to the metabolically active hormone T3. And the levels of reverse T3 fluctuate up and down through the day. Because of this, I’m never confident of coming to a conclusion that someone has a problem with high reverse T3, not unless the person has had multiple measures of the reverse T3 over a 24-hour period. Like the TSH, free T4, free T3, reverse T3 levels vary dramatically every 30 minutes or so. Depending on when a person’s blood is drawn or saliva taken. Sometimes the levels will vary enough so that a clinician will give the patient a different diagnosis from the one that he or she would have given 30-minutes before or after the blood or saliva sample was taken.
So blood levels vary rapidly. Because of this, I don’t believe the reverse T3 or the other lab tests in general are very useful. However, I do believe the reverse T3 is useful under one circumstance: when we have enough measures to get averages over time, and when the levels are regularly way out of range. So, in my view, the reverse T3 can be useful, but I think its usefulness is limited, which is true of the TSH and other thyroid hormone levels”
‘Your comment is awaiting moderation’…
Not sure if you get alerted to comments ‘awaiting moderation’ or not…
So i thought i’d just let you know i posted an earlier comment at around 10.55pm.
http://perfecthealthdiet.com/2011/09/high-ldl-on-paleo-revisited-low-carb-the-thyroid/comment-page-3/#comment-80953
that is currently ‘stuck’ awaiting moderation….
thx
Hey all…
I’m new to the site and Paul’s work. Will buy book Paul’s book soon for insight into my problems. I haven’t gone through all of the comments but high LDL could be the body screaming to make more testosterone. Have you all tested for low sex hormones?
Life Extension Magazine has a great article about hyper-cholesterolemia relative to men and its implications about low steroidal sex hormones. Bottom line is fix your hormones and cholesterol will fix itself.
My own experience with supplemental pregnenolone and DHEA relative to a “pregnenolone steal” vastly improved my lipid profile in six weeks. Testo is still low due a chronic sleep disorder, but if you all search Life extension I think you will find the article very interseting. (Sorry for not providing the link)
Lastly, My high Rt3 was demolished by SRt3 of 50mcg per day, but it didn’t improve sex hormones or lipids like pregnenolone and DHEA did. Will begin to add progesterone into the mix and re-test in six weeks.
Looking foward to reading more research on this site. Very useful stuff!
Dennis,
Thanks for this! I am in a similar boat — low sex hormones, high LDL, high rT3 — but have yet to take the step of supplementing pregnenolone or DHEA. I have never been comfortable with exogenous hormones, but at this point I am running out of options.
if I may ask, what form and dosage of pregnenolone and DHEA are you using?
@MM…
Here is the article I referenced earlier. http://www.lef.org/magazine/mag2006/jul2006_atd_01.htm?source=search&key=familial%20hypercholesterolemia
Right now I’m taking 100 mg pregnenolone and 50 mg regular DHEA five days on and two off. Want to add 40mg of progesterone cream as a DHT blocker, estradiol and prolactin inhibitor. Will also add Chrysin to inhibit estradiol even more. 24 hour diurnal saliva levels are low-normal
After six weeks, labcorp values went from 200 DHEA-S to 520 and free testo from 4.8 to 10.0. Not great but better. My LDL has never been high, but went from 110 to 90 and HDL from 35 to 65 and triglycerides down to 41.
I don’t supplement with fish oil, but my omega 6 to omega 3 is 2.3 to 1, so I’m assuming the fish diet helped lipids and hormones as well.
Good luck
FACTS:
Male, white, 52
5-7
170lbs
approx. 130lbs fat-free mass
Bodyfat: approx. 19%
GOAL: <10% bf using a LC PaIeo diet combined with Intermittent Fasting which means I must lose at least 17lbs of bf, both subcutaneous and visceral.
Resistance train 4xs/week
Cardio interval train 2-3xs/week
I was dx'd via ultrasound with non-alcoholic fatty liver disease (NAFLD) two years ago. It is indeterminate how long I've had it. Liver enzymes continue to remain within normal range and I notice no symptoms
I am hypothyroid and have been taking 75mcg of sustained-release T3. My latest thyroid numbers are posted in the link below [p2, 3, 10].
TSH has improvement over last labs. Both T4 and T3 show depressed, however, I was fasting for nearly 20 hours on the first day. rT3 is less this time, which is a good thing.
Have been on LC Paleo diet for last three months and doing between a Lean Gains [ http://www.leangains.com/2010/04/leangains-guide.html ] 16/8 IF protocol to as much as 20/4 IF protocol. I do mini-carb refeeds (about 50-60g) on my workout days only. If I increase carbs more than this, my post-prandial BG will exceed 125.
What's freaking me out are my latest lipid tests. I had the top three done in a matter of two consecutive days [p2, 5, 11-14].
LATEST LABS: http://s57.photobucket.com/albums/g207/CS2006/LABCORP%2006-19-12%20and%2006-20-12%20LABS/
If we’re clearing lipids from the liver, then this is a good thing, but HOW CAN I DETERMINE THAT IT'S THIS AND NOT FROM THE DIET ITSELF?
In other words, is the increase due to CREATION or CLEARANCE (resolution of NAFLD)?
I have not changed any macros in my diet, maybe slightly more lean grass-fed animal protein, but saturated fat intake has remained constant throughout. And most of the saturated fat is drained because I steam all my meats, so how can it be CREATION?
The only other fats I eat with frequency are O3s (2-4g), coconut, flax, macadamia and olive oil.
What evidence supports this unconventional theory?
I understand that one of the key problems with fatty liver disease is that the lipids get stuck in the liver and they’re not being released into the bloodstream.
How could this be the case when taking liver support supplements like milk thistle, dessicated liver, choline, lecithin, etc.? Why wouldn't such intervention spur on the purge also?
Why wouldn't free fatty acids (FFAs) from stored subcutaneous fat be released into the bloodstream as well?
Could this explanation be the mechanism behind the clearance of FFAs: During fasting or starvation, free-fatty-acids are released during lipolysis into the liver and muscles to be burned as energy, this is called fat-oxidation. During the fed-state and especially while eating a starch-based-diet, fat-oxidation is inhibited and replaced with carbohydrate-oxidation, insulin is what mediates this shift. When carbohydrate-oxidation is taking place, fatty-acids are shuttled back and "locked away" in adipose-tissue… where they belong.
In addition to LC Paleo/IF, I also began taking 1g of choline nearly a month before the labs + 3mg methylfolate/day to help with a genetic methylation defect.
Could the above combination have created a mega-purge?
Could the answer be that the best predictor of fatty liver is obesity and insulin resistance?
Another thing:
I have been on warfarin for 3 months and must remain on it for another 3 months. This was the only thing I could find on warfarin and its effects on blood lipids:
Coumadin binds to bile acids in the intestine leading to increased excretion of bile acid in the feces leading to increased oxidation of cholesterol to bile acids resulting in increased numbers of low density lipoprotein receptors with increased hepatic uptake of LDL and lower serum cholesterol levels
source: http://www.flash-med.com/Side_Effects_Coumadin.asp
Anomalies to purge theory:
Why the decreased HDL when I was making nice progress before?
Lastly, I had been fasting for 18-20 hrs prior to my blood being drawn. My fasting insulin was only 5.2. Then why an elevation in HbA1c (5.8) and FBG (95)? Should've been in the low 80s, especially when fasting for LONGER periods AND on LC Paleo.
This even when on a broad range of BG-lowering natural agents including corosilic acid, chromium, cinammon, etc.
So, why is my insulin sensitivity is taking a nosedive during this so-called healing crisis as well [see Insulin Resistance Score – p12, 14]?
Can someone please interpret my lipid profiles, especially the NMR LipoProfile and tell me what is going on?
Hi Mark,
Your lipid profile is not at all unusual. It has the typical high trigs low HDL of many people with metabolic syndrome / cardiovascular disease. LDL is slightly high, but that’s not the major issue, the trig:HDL ratio is the big red flag.
You would benefit from eating more carbs I believe, but you say you then get diabetic blood sugars. Have you been diagnosed with diabetes?
One of the keys to curing your situation is optimizing vitamins D/A/K2. But you say you’re on warfarin, which interferes with vitamin K2. Have you had a stroke or clotting? Why are you on warfarin?
Warfarin will cause vascular injury and calcification (since vitamin K2 is needed for healthy vessels) and that might be a factor in your lower HDL.
It’s difficult for me to evaluate what’s going on, as you clearly have some health problems and are under medical care. I can’t tell whether your version of low-carb Paleo, which I think is too low carb, may be contributing to some of your problems. Have you read our book? That might give you some insight.
Best, Paul
@ Paul –
Appreciate the feedback.
Perhaps I should stick to a longer refeed window like 16/8 IF, but I feel no worse extending it. So far, I feel better and get a better workout during fasting. It may sound stressful, but no complaints with the exception of these labs. Actually, I do take a good size portion of aminos to avoid catabolism, so at least it’s something as opposed to a strict fast. Just no carbs before, only after. Training during fasting oxidizes fat more than in a fed state (no good). I have no hunger or symptoms of any kind during this time. Following training comes a sizeable refeed, largely of lean animal protein, fresh veggies, and a mini-carb refeed with less than 15g fructose and no more than 75g total carbs.
If I had leptin and insulin resistance, then why is my fasting insulin and leptin so low? That’s what doesn’t make sense.
I am not diabetic. My FBG ranges from the mid-80s-high 90s; postprandial BGs hover between 105-115 with no carbs and between 115-130 w/ smart safe carbs and in the 50-75g range in one meal. I rarely ever go above a 30 pt. rise postprandial. I can also control the level with an ounce or two of apple cider vinegar. It works!
The elevated vit A is simply from supplementation saturation (cod liver oil) and is what my doc wanted. Now, time to drop dose back. Too little A is worse for thyroid! I takes tons of zinc and mg daily and my past levels are optimal. D is optimal at nearly 60 (was as high as 100).
My O3 to O6 ratio is the opposite of everyone else’s: like 6:1 in favor of O3s which is too much O3 and not enough O6! So I am taking more O6s now to rebalance and get closer to 1:1.
I am on warfarin for a DVT (clot) I had in my left leg in March. My guess is that it was caused most likely from the MTHFR mutation I just discovered I had which can cause hyperhomocysteinemia (elevated homocysteine) which can lead to clots. I am taking a comprehensive methylation regimen of methylfolate, methylB12, P5P, R5P, NAC, TMG, DMG, SAMe, taurine, etc.
I am on the standard 6-month anticoagulant prophylaxis protocol. I have two more mos. and I’m done. Still, I wonder what effects warfarin has had, as it has definitely decreased my Vit K level on my lab which affects the protein responsible for procoagulation which affect, hello, LIPIDS:
http://atvb.ahajournals.org/content/14/11/1737.short
To what extent and how this affects lipids, I don’t know, does anyone?
I am upping my carb intake on my workout days to help offset the potential stress from chronic ketosis. BUT I STILL AM UNABLE TO SHED MORE BODYFAT! I WAS making progress (19% down from 24%, but have another 10% to go to reach my goals), and then it seems to have stopped. It would seem I am definitely NOT an efficient fat burner! If I am at 19% and have NAFLD still, I need to be IFing and doing paleo I would think!
By the way, this is not my typical lipid profile. Following are my last three lipid and glucose tests:
PRIOR TO LC PALEO & IF:
06-14-11:
TC: 163
LDL:92
HDL:42
TRIG: 147
HGBA1C: 5.6
INSULIN: 2.3
AFTER STARTING LC PALEO:
10-20-11:
TC: 214
LDL: 144
HDL: 47
TRIG: 113
HGBA1C: 5.3
INSULIN: <2.0
AFTER STARTING LC PALEO/JUST STARTED IF:
03-08-12:
TC: 197
LDL: 132
HDL: 43
TRIG: 108
HGBA1C: 5.0
INSULIN:<2.0
With all the anecdotal threads on paleo temporarily causing elevated LDL [http://paleohacks.com/questions/96588/clinical-question-about-cholesterol-and-paleo-diet#axzz1ypfg6I2f], especially when one has fatty liver, I would guess I fall into that category hands down. During a purge caused by LC Paleo/IF, free fatty acids are released into the bloodstream. But with so much going on here it is not an easy, slam-dunk answer. As I said, I haven't altered my diet, increased my IF from 16 to 20 hrs.
With all that I have tried and already done, I am leaning (and hoping) towards this anomaly being resolution of fatty liver.
Thanks again for your insight.
Hi Mark,
There are a few obvious improvements you could make to your supplement program, like taking vitamin K2 (especially important with high A and D), stopping warfarin, and reducing zinc.
But I’m not sure why you’re so concerned. Your lipids have been improving steadily. LDL of 130 is perfect, TC over 200 and HDL over 60 is optimal so both of those are low, especially HDL. Trigs are higher than optimal, but they’re improving.
I think you should read our biomarkers category for all the lipid posts, think about implementing steps to raise HDL, and improve your supplements.
I’d also implement circadian rhythm therapies: sun exposure and low-level activity early every morning and at mid-day. Avoid blue light at night. Try to finish eating around sunset.
The DVT is the only significant health problem you’ve mentioned, so I think you need to focus on vascular health.
Paul – Again, my lipids and HGBA1C have worsened from the March test and my HDL has never been 60 (I wish):
TC: 236
HDL: 36
LDL: 169
TRIG: 155
HGBA1C: 5.8
INSULIN: 5.2
That is the concern. In simple terms, I am again hoping this spike is due to resolution of fatty liver (fatty acid purge caused by LC Paleo), the other significant health problem.
I am fully aware of the drawbacks to warfarin. Fortunately, I am on it for only a short while and have two months left. But I cannot start taking K2 right now as that would inhibit the anticoagulation prophylaxis necessary to prevent another DVT or PE, either of which could be life-threatening.
Again, if the cause of the spike in LDL and TRIGS is due to the adjustment period of fasting and LC Paleo (clearance of fatty acids) as opposed to diet and/or stressors (creation), then there is light at the end of the tunnel.
That is what I need help in deciphering.
Hi Mark,
The recent changes could be due to being too low carb, or being improperly nourished in some way. I do think you should increase carbs a bit.
You’re better off taking K2 with the warfarin. There may be a slight adjustment of warfarin dose.
I don’t think it’s a transient issue.
In this link, Chris Kresser had Chris Masterjohn covered reasons why cholesterol would increase after going paleo, and why it may not be bad:
http://chriskresser.com/chris-masterjohn-on-cholesterol-and-heart-disease-part-3
Masterjohn mentioned that a transitory increased blood lipids could be a sign that fatty liver disease is being reversed.
Hi Paul,
Is it possible for dietary linoleic acid to be too low and cause unhealthy lipids?
http://www.ncbi.nlm.nih.gov/pubmed/12492626
Cholesterolaemic effect of palmitic acid in relation to other dietary fatty acids.
French MA, Sundram K, Clandinin MT.
Source
Nutrition and Metabolism Research Group, Departments of Agricultural, Food and Nutritional Science and Medicine, University of Alberta, Edmonton, Canada. tom.clandinin@ualberta.ca
Abstract
The effect of dietary intake of high palmitic acid levels in combination with other fatty acids in normal subjects was assessed. Palmitic acid (10% of energy) was fed in conjunction with decreasing levels of linoleic acid to determine if a threshold level of linoleic acid prevented palmitic acid from being hypercholesterolaemic. Healthy subjects received each of the diet treatments for 21 days, followed by washout periods of 7 days. In a second experiment, the effect of exchanging palmitic acid for trans fatty acids on plasma lipoprotein cholesterol levels and on rates for endogenous synthesis of cholesterol in normal subjects was investigated. Diet treatment lasted for 30 days. On day 30 of each diet treatment, a priming dose of deuterium was consumed, followed by a subsequent blood sample at 24 h. Blood cholesterol fractions were isolated and analysed by isotope ratio mass spectrometry to measure cholesterol fractional synthetic rates. In the first experiment, total plasma cholesterol levels increased as the percentage of linoleic acid decreased. The data indicated that high levels of palmitic acid were not hypercholesterolaemic if intake of linoleic acid was greater than 4.5% of energy. When the diet contained trans fatty acids plasma total and low-density lipoprotein-cholesterol increased and cholesterol synthesis increased with a decrease in high-density lipoprotein-cholesterol.
Thanks,
Mark
Paul –
Out of all the possibilities as to why my LDL shot up as well as FBG, this article by Chris Kresser on excessive O3 PUFAs from fish oil makes the most sense:
http://chriskresser.com/when-it-comes-to-fish-oil-more-is-not-better
Here’s another:
Fish oil has detrimental effects on hepatic cholesterol levels and lipid oxidation: http://suppversity.blogspot.com/2012/02/tta-fish-oil-fat-burning-superfats-or.html
I have been taking 3-6g daily consistently for the last 3 years. I always figured that the worst side from excess fish oil would be thinner blood. Never thought of oxidation and fish oil as part of the total PUFAs which, in excess, can wreak havoc on lipids and glucose.
Sound like a reasonable cause?
What’s you thought on Kessler’s recommendation to consume fermented cod liver oil as a replacement for fish oil?
Hi Mark,
Yes, 1 g/day from fresh fish only is optimal, 3-6 g/day is too much. It’s plausible that that’s a problem.
I don’t agree on the fermented cod liver oil, I favor fresh or frozen fish.
Have you seen excess fish oil having any effect on HDL?
Also, do you see excess FO consumption as a more plausible cause of my elevated LDL and FBG than the free fatty acid liver purge/clearance/cholesterol increase as reported by those on low-carb Paleo?
I would think that FO would lower LDL by increasing LDL-receptors. A huge excess might disregulate lipids, but your dose though high is equal to quite a small helping of salmon. Studies of FO toxicity tend to use FO as 30% of calories.
Conventional wisdom is that FO can do nor harm and only good. Read the Kresser link I posted above. There is a study that shows that 3g of FO daily LONG TERM increases LDL. Also, I believe it’s the oxidation to the oil used in supplemental form that can be detrimental to lipids unlike what is in food.
Even too much FO from fish itself is no good according to Masterjohn:
“Excessive doses of EPA from fatty fish, fish oil and cod liver oil may contribute to all of these symptoms in susceptible individuals.”
I pretty much agree with that. However, Kresser says
he can’t read the full text in Portugese. It may be that by 3g is meant 3g of EPA plus DHA, which would be 10g fish oil in standard caps. Whereas about 0.5-1g EPA plus DHA seems optimal from fish oil or CLO.
I’m a bit sceptical about rancidity as animals including humans have a long history of eating rancid fats, including some long-lived inuit, whose diet included rancid seal blubber. I’m not sure oxidised fsts are fully digested.
Here is the actual study:
http://www.ncbi.nlm.nih.gov/pubmed/20694407
That’s not a excuse, with google translator you can read pretty much anything these days… But, I don’t need any translator to read portuguese. And, you’re right, George: in that study each of the subjects took 10 fish oil capsules, totalizing 1.8g of EPA and 1.2g of DHA.
That’s what I thought.
Here’s how I think it works:
as you take PUFAs they are incorporated into cell membranes
the cells need more cholesterol to keep stable (PUFA makes them softer)
so make more LDL-receptors, which pull LDL out of the bloodstream
so the liver makes MORE cholesterol
after a few years the cells of the body contain significantly MORE cholesterol than if you’d never taken PUFA.
And any change can release that LDL back into the blood. For example, if the cells become saturated and start to burn the PUFA, the cholesterol is not needed.
If you stop supplementing PUFA, or eat more SFA, the cholesterol is not needed.
I cannot find ANY papers on the health effects of CONSUMING rancid or oxidised fats. A strange oversight; can anyone find one?
http://en.wikipedia.org/wiki/Rancidification
This hypothesis would then apply to all PUFAs including FO.
FO has stronger immediate effects, but over time it should apply to all.
MUFA in high ratios may also increase cholesterol pool.
Standard fish oil is high in shorter PUFA; CLO has some arachadonic acid, 10% EPA, 10% DHA.
The hypothesis isn’t just mine. There is evidence on PubMed
“Although unsaturated fatty acids increase cholesterol synthesis, they also increase hepatic LDL receptor number and LDL turnover in vivo.”
” increases in LDL-C due to SFAs (particularly 12:0+14:0) appear to reflect LDL overproduction associated with a shift in cholesterol from tissues to the plasma cholesteryl ester (CE) pool (both LDL-C and HDL-C) without altering whole-body cholesterol balance.”
http://jn.nutrition.org/content/135/9/2075.full
Masterjohn says ” the consumption of excess PUFAs increases oxidative stress even when the oils are fresh and properly cared for”
Possibly, especially so, as then they penetrate further into the organs before being disposed of..
Hi Paul,
I originally posted on this blog entry when it first came out. I had very high LDL and subsequent testing showed t3 at the low end of the range and rt3 at the high end.
Since then I have followed your recommended supplements and significantly upped my carbs with white rice, tapioca and dextrose.
I just had my cholesterol retested and my doctor was amazed. In the original postings I had converted the units, but I’ll just leave these as per my report:
Units: mmol/L
Test on 29 Sept 2011:
Cholesterol 10.5
Trigs 2.0
HDL Chol 1.5
Chol/HDL 7.0
LDL Chol 8.1
Test on 17 Jul 2012:
Cholesterol 4.4
Trigs 0.8
HDL Chol 1.3
Chol/HDL 3.4
LDL Chol 2.7
Obviously good news on the decrease. I’d be interested in your thoughts about the numbers overall.
Thanks so much for all your great work.
Cheers,
Adam.