A few “Peat-atarians” – followers of the iconoclastic health writer Ray Peat – have accused us of being too skeptical of fructose. They think we should promote sugar consumption.
Here’s Travis Culp:
I think fructose is only conditionally problematic and that the consumption of it alongside glucose at a time of low liver glycogen is highly advantageous. In fact, I would go so far as to say that (somewhat slowly) drinking a can of soda upon waking (as disgusting as that is) would not result in any real glycation, insulin resistance, elevated TGs etc…. I think it’s beneficial to eat something really sugary upon waking …
Here’s Danny Roddy:
Peat has stated that … fructose … “powerfully” refills glycogen …
I would consider the ability to refill glycogen (minimizing adrenaline & cortisol release) to be an important factor in health …
It’s true that the ability to refill glycogen is essential for health; some genetic glycogen storage disorders are fatal in early childhood. But everyone who lacks a glycogen storage disorder has the ability to refill glycogen from multiple sources. In addition to fructose, glucose sugars and starches refill glycogen, as does milk sugar (a compound of glucose and galactose).
So the question is which combination of dietary sugars (a) is best at refilling glycogen and (b) makes the healthiest diet, all things considered?
Sugar Composition of the Diets
Both Danny and Travis framed their arguments as criticisms of our diet. They are really arguing that a Peat-style sugary diet is healthier than a PHD-style moderate-starch diet.
So before going further, let’s look at the sugar content of the diets we’re comparing.
First, note that PHD is not a zero-fructose diet. As an examination of the PHD Food Plate shows, PHD includes many fructose-containing plant foods – fruits, berries, and vegetables such as beets, onions, carrots, and squashes – plus “pleasure foods” like chocolate.
Also, PHD is not a zero-dairy diet, so for many practitioners it will include some milk sugars which are half galactose and half glucose.
In my diet personally, probably about 55% of carb calories come from starches, 30% from fruits, berries, and sugary vegetables, and 15% from dairy products such as yogurt. In terms of simple sugars, this translates to about 77% glucose, 15% fructose, and 8% galactose.
Not every Perfect Health Dieter will have the same sugar proportions; there is no obligation to consume dairy, and the relative proportions of starchy and sugary plants will vary according to taste. But let’s take mine as characteristic PHD proportions.
In a Peat-style diet, in contrast, the breakdown of sugars is near 50% glucose and 50% fructose.
So we aren’t comparing fructose against glucose, but a 77% glucose 15% fructose diet against a 50% glucose 50% fructose diet.
Why the Focus on Refilling Glycogen?
Why do the defenders of sugar focus on its ability to refill glycogen?
The reason is that fructose is treated by the body as a poison. Dietary fructose is shunted to the liver for disposal by conversion to glycogen, fat, lactate, or pyruvate.
Fructose is treated like a poison because it is dangerous. High doses of fructose have observable harmful effects even in short-term studies. Fructose does no good to the liver while it’s there, in fact fructose combined with polyunsaturated fats very effectively creates liver disease. Fructose in any other organ does harm; for instance, fructose promotes cancer growth.
Given fructose’s rapid disposal, any benefits from fructose have to be attributable to the glycogen or other products it is turned into. If fat, lactate, or pyruvate (a glucose product) provided benefits, dietary fats or starches would do the same, without the risk of fructose toxicity or fats getting stuck in the liver due to choline and methionine deficiency. So if fructose is to have benefits, it has to be via glycogen.
Here, then, is the challenge Peat-atarians face. Fructose has many proven harms. It has only one possible benefit: its ability to help re-fill liver glycogen. Peat-atarians have to show two things:
- That a diet with Peat-like sugar proportions – roughly 50% fructose, 50% glucose –is better than a diet with PHD-like sugar proportions – 15% fructose, 8% galactose, 77% glucose – at refilling liver glycogen.
- That better re-filling of liver glycogen improves the healthfulness of the diet.
How Do Sugars Perform at Refilling Glycogen?
Danny provides no citations for his claim that fructose “powerfully” refills glycogen. But Danny’s commenters help him out.
Daz, drawing upon a New York Times report, offers two studies [1] [2]. Cliff offers several more [3] [4]. Let’s see what these tell us.
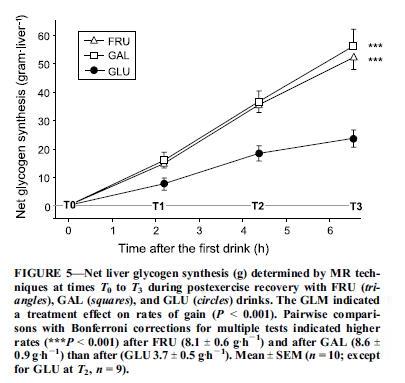
The first study, “Fructose and galactose enhance postexercise human liver glycogen synthesis” [1], looks at athletes depleted of liver glycogen by intense cycling, and assessed the effectiveness of three sugar drinks at replenishing liver glycogen. The three drinks were:
- 2/3 maltodextrin, 1/3 fructose;
- 2/3 maltodextrin, 1/3 glucose;
- 2/3 maltodextrin, 1/3 galactose.
Maltodextrin digests to glucose, so all three drinks are majority glucose. The athletes drink 275 calories of these drinks per hour for 6.5 hours after exercise. Galactose is non-toxic, but like fructose tends to be taken up by the liver.
Liver glycogen was measured every two hours with carbon-13 magnetic resonance imaging. Here were the results:
So 67% glucose / 33% galactose did the best, 67% glucose 33% fructose was close behind, and 100% glucose lagged.
Why does the 100% glucose drink underperform? One reason is that fructose and galactose, but not glucose, are preferentially targeted to the liver:
A factor of potentially larger magnitude in enhancing liver glycogen synthesis is the differential postabsorptive fates of fructose and glucose. Glucose is a relatively poor direct substrate for liver glycogen synthesis (24,27). Much of it is released from the liver into the systemic circulation to be stored as muscle glycogen (3,7). In contrast, fructose is primarily taken up by the liver … [1]
The second paper, “Superior endurance performance with ingestion of multiple transportable carbohydrates” [2], did not measure liver glycogen replenishment; instead, it gave its cyclists sugary drinks every 15 minutes throughout an intense 2-hr cycling test, and compared performance. Three different drinks were used: a 67% glucose 33% fructose drink, a 100% glucose drink, and a water-only control group. Performance was best with the 67% glucose 33% fructose drink, intermediate with the glucose drink, and worst with the water drink. The results suggest that the 67% glucose 33% fructose drink was better for liver glycogen replenishment, and that liver glycogen replenishment aided the cyclists’ performance.
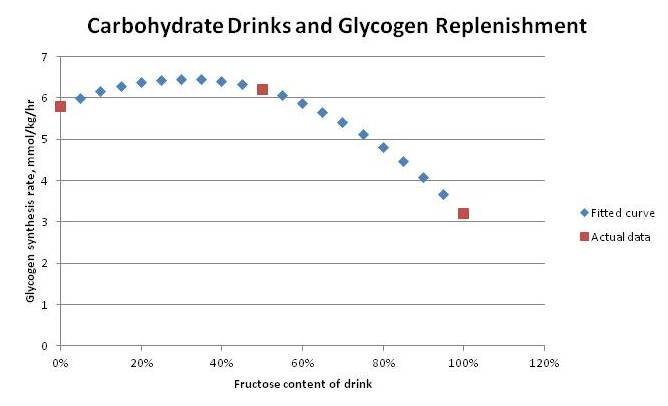
The third paper, “Effect of different post-exercise sugar diets on the rate of muscle glycogen synthesis” [3], isn’t available to me electronically, so we’ll have to work from the abstract. It looked at muscle glycogen, measured using biopsies (ouch!), rather than liver glycogen.
It first assessed the effect of different amounts of glucose. It found that 0.7 g/kg body weight of glucose given every 2 hours would maximize the rate of muscle glycogen synthesis. For an 80 kg man, that works out to 56 g or 224 calories of glucose per two-hour period, or 112 calories per hour. Above this amount, the rate of muscle glycogen synthesis is unchanged.
It then compared three formulations at this same 0.7 g/kg body weight dose: 100% glucose, 100% sucrose (50% glucose, 50% fructose), and 100% fructose. Muscle glycogen synthesis rates were:
- 5.8 mmol/kg/hr with 100% glucose
- 6.2 mmol/kg/hr with 50% glucose, 50% fructose
- 3.2 mmol/kg/hr with 100% fructose
If we fit a quadratic curve to these points, it predicts a peak rate of glycogen synthesis with 70% glucose, 30% fructose:
Athletes Agree: More Glucose Than Fructose
Of course, endurance athletes know that it’s beneficial to replenish glycogen during endurance events like marathons and triathlons.
Some authorities, including Tim Noakes, an exercise physiologist who has run over 70 marathons, believe that liver glycogen rather than muscle glycogen is the gating factor in marathon performance. From “The Science of Carbohydrate Loading” by David Peterson:
Remember also that muscle glycogen is committed to be used by muscle and cannot assist in maintaining blood sugar levels. Therefore should no additional carbohydrate be ingested during prolonged exercise, the task of maintaining blood glucose levels rests firmly on the liver’s glycogen stores and gluconeogenesis (the manufacturing of glucose from plasma amino acids). Oxidation of blood glucose at 70-80% VO2 max is about 1.0 g/min or about 60 g/hour. Therefore it can be predicted that even with full glycogen stores, a less conditioned athlete’s liver will be depleted of its carbohydrate within an hour and three quarters of continuous moderate intensity exercise. (Interestingly, the daily carbohydrate requirements of the brain and nervous system alone are enough to deplete the liver glycogen stores within 24 hours.) Once liver glycogen levels begin to drop and exercise continues the body becomes increasingly hypoglycemic (low blood sugar) mainly because blood glucose is depleted faster than it is replaced by gluconeogenesis. Professor Tim Noakes considers liver glycogen depletion and subsequent hypoglycemia to be the primary factors affecting fatigue and performance during extended duration races and especially in instances where muscle glycogen levels are low as well.
So marathoners and other endurance athletes will want to replenish liver glycogen as rapidly as possible during a race. What mix of sugars do they use?
The popular product is carbohydrate gels that can be swallowed at the same time water is taken. Here are the top carbohydrate gels sold on Amazon:
- Carb BOOM! Energy Gels – 24-Pack
consist of “a special blend of 22-25g of complex carbohydrates and just 2-4g of simple sugars to maximize energy delivery to working muscles.” The complex carbs are probably derived from starch and are 100% glucose, while the sugars probably contain some fructose. If the ratio is 2 g fructose in 25 g gel, then the composition will be 8% fructose 92% glucose.
- PowerBar Energy Gel, Double Caffeine, Tangerine, 1.44-Ounce Packets (Pack of 24)
consists of a 2:1 glucose to fructose blend, or 67% glucose 33% fructose.
- Clif Bar Shot gel, razz – 1.1oz (24/box)
list their primary ingredient as organic brown rice syrup, which is nearly 100% glucose.
So the sugar mix ranges from 67% glucose to 100% glucose. No product uses 50% fructose.
Presumably, athletes have done a great deal of personal experimentation and know that these ratios do, indeed, optimize the speed of glycogen replenishment.
When athletes have no need for speed, as when they are carb loading before a marathon, then they eat starches like pasta and bread, not sugar. So to maximize total glycogen status, regardless of speed of filling, a carb mix close to 100% glucose works just fine.
Glycemic Control
The fourth paper, “Acute fructose administration decreases the glycemic response to an oral glucose tolerance test in normal adults” [4], is about how a bit of fructose affects the glycemic response to an oral glucose tolerance test.
It showed that a 9% fructose 91% glucose test (7.5 g fructose, 75 g glucose) produced a lower glucose area under the curve and higher insulin response than a 100% glucose test. Here’s the glucose response:
In general higher insulin and lower glucose is healthier than the reverse, so this is considered an improvement.
Summary of the Data
What these papers show is:
- Glycogen replenishment proceeds the fastest with a mix of sugars consisting of about 70% glucose and 30% fructose or galactose.
- Although this wasn’t tested, we can guess that a mix of fructose and galactose would be more effective than fructose alone, since it seems that utilizing multiple carbohydrate pathways is what drives the speedier glycogen replenishment. So the fastest glycogen replenishment might occur with something like 70% glucose 15% fructose 15% galactose.
- Muscle glycogen replenishment is maximized with a carbohydrate intake of 100 calories per hour.
- Athletes agree with the research, using carb gel packs that contain typically 30-40 g carbs with a composition of 67% to 100% glucose, 0% to 33% fructose.
- Glycemic response to a large dose of carbohydrate may be improved by eating a 9% fructose 91% glucose mix.
From these data, I infer that for glycogen replenishment in liver or muscle, a PHD-style carb mix of 77% glucose, 15% fructose, 8% galactose is probably equal or superior to a Peat-style carb mix of 50% glucose, 50% fructose.
Conclusion
For athletes in the midst of a race, or in need of rapid recovery for a second race on the same day, speedy glycogen replenishment may be the endpoint to optimize. If so, they should eat a sugar drink composed of roughly 70% glucose and 30% fructose and galactose.
This is closer to PHD diet ratios than to Danny Roddy’s recommendation of orange juice or Travis Culp’s recommendation of soda!
But for others, speed of glycogen replenishment is hardly likely to be the parameter to optimize. There are unlikely to be significant benefits for non-athletes from replenishing glycogen 6.5% faster, as was found in the muscle glycogen study [3].
Speedier glycogen replenishment is almost the only known benefit to fructose consumption. It’s possible that low fructose doses, about 9% of carb calories (perhaps 2-3% of total calories), may improve glycemic control. This is a lower fructose fraction than is found in PHD, and far below the fructose fraction recommended by Danny and Travis.
Given the known risks of fructose consumption, especially with chronic intake at high doses or in conjunction with polyunsaturated fats, it seems prudent to err on the low side. It seems to me that the Peat-atarians have failed to provide any evidence at all in favor of a higher fructose intake than is provided by the fruits, berries, and sugary vegetables recommended by the Perfect Health Diet, save for athletes in the midst of a race or post-race recovery.
References
[1] Décombaz J et al. Fructose and galactose enhance postexercise human liver glycogen synthesis. Med Sci Sports Exerc. 2011 Oct;43(10):1964-71. http://pmid.us/21407126.
[2] Currell K, Jeukendrup AE. Superior endurance performance with ingestion of multiple transportable carbohydrates. Med Sci Sports Exerc. 2008 Feb;40(2):275-81. http://pmid.us/18202575.
[3] Blom PC et al. Effect of different post-exercise sugar diets on the rate of muscle glycogen synthesis. Med Sci Sports Exerc. 1987 Oct;19(5):491-6. http://pmid.us/3316904.
[4] Moore MC et al. Acute fructose administration decreases the glycemic response to an oral glucose tolerance test in normal adults. J Clin Endocrinol Metab. 2000 Dec;85(12):4515-9. http://pmid.us/11134101.












Good post, I learned a lot from it. But just how relevant is what athletes happen to do to what is actually best to do? Unless these sports products were made based on available evidence then they don’t do much to make a point. I don’t trust athletes any more than I trust doctors, I don’t trust anyone. People are highly fallible, and health science is the worst I have ever seen.
But the central point seems to be valid. Although some fructose is clearly desirable for an endurance athlete, that doesn’t warrant the recommendation for the bulk of carb calories to be sucrose.
Cheers!
Hi Paul,
I’ve read that you’re recommending rice syrup or dextrose for people with bowel dissorders as a substitue for safe starches. If I were to use only rice syrup for a while, how much would you recommend that I consume? My fear is that it’s going to spike my blood sugar too much if I use 100 grams of it a day, which is what’s needed to achieve 400 carb calories. I’m guessing guessing mixing it with protein and fat will help, but still it seems like alot.
just a comment/query/thought on “Fructose and galactose enhance postexercise human liver glycogen synthesis”;
Is their anything else that could have had an impact on the volume change of the liver in this study.
Can we be certain than the change in liver volume is 100% due to the change to liver glycogen? or are there other things in the liver that may also be a factor in the change in volume.
(ie. is water a factor….does the liver/liver cells contain water)
Hi Stabby,
I was moved to look up what athletes actually do by the fact that the journal articles rather sparsely sampled the various possible carb ratios.
Sometimes athletes are more advanced than the exercise scientists.
Since the two agree, I would consider them supporting evidence for each other.
Hi Eirik,
Bowel disorders are tough because you have to make compromises, both in what types of carbs you eat and how much you eat.
200 calories carbs + 400 calories protein I regard as the minimum intake consistent with health, so I would start by trying to get at least 200 carb calories. If rice syrup is the best tolerated, then that can be a major source. Add it to other foods like ice cream, drinks, etc so you can get it in small doses. If you can, raise carbs past 200 toward 400 and diversify food sources.
Hi Darrin,
The volume growth was not very consistent, but it did correlate with glycogen levels, and shrinkage with the exercise that depletes glycogen.
There is about 2.6 g water associated with each additional 1 g of glycogen.
Yeah but Ray Peat is kind of cool, so I’m not entirely convinced he could be wrong about something.
On a different topic, I thought you might be interested in this vid that I just saw posted on Facebook – about a guy whose alzheimers is improving through use of coconut oil.
http://www.cbn.com/media/player/index.aspx?s=/mp4/LJO190v1_WS
An excellent summary of the data, Paul. I’ve always found that particular Peatism to be bizarre — and I’m extremely physically active by modern standards.
Given the following:
* Most people don’t exercise very much
* Exercise burns less calories than most people think
The problem for the overwhelming majority is “how do I dispose of excess sugars, simple or complex,” not “how do I replenish depleted liver glycogen?”
As you point out, glycogen replenishment during intense endurance exercise is about the only time when fructose is beneficial. In all other situations, fructose is more like “well, perhaps it’s not actively harmful if consumed in moderation.”
JS
Hi Todd,
Heh, yes Ray is very interesting, I kind of root for him to be right. But as JS says, his stand on fructose is rather hard to support.
Thanks for the Mary Newport video. It’s nice to see he’s still doing well.
Hi JS,
I agree. Thanks.
I think much of this needs to be put in greater context. The data listed above is only loosely associated with the reasons Peat recommends fruits to begin with. He recommends sucrose as a supplement when fresh fruits are unavailabl as well. Add to that fruits are great sources of salicylates and inisitol, two favorable nutrients for inflammation and insulin sensitivity. Peat on the whole suggests that if there were an “ideal” macronutrient ratio it would be 33% from each source, but would vary based on the individual’s response.
Some of the reasons Peat recommends sugar from fruit is because it leaves less for gut bacteria to feed on, it replenishes glycogen best, which in Peat’s view increases the liver’s capacity to detoxify the body of PUFA and excess estrogen, suppresses adrenalin and cortisol (stress response; of course paired with adequate protein and salt in the diet), it also stimulates the production of cholesterol, which if one thinks the cholesterol-heart hypothesis is bologna, would stand to bring up the protective effects of lipoproteins and their ability to bind endotoxin. I’m not a Peat expert but the above are just a few reasons he advocates fruit. My advice, start reading his articles because I feel his ideas regarding thyroid, stress, and hormonal status marry well with your ideas.
Salicylates inhibit the krebs cycle. But you won’t hear that from ‘cherry-picker’ Ray Peat.
And then there’s his whole ‘there’s no such thing as essential fatty acids’ hypothesis, which not a single scientist or researcher agrees with.
Don’t want to defend peat to much as people can make there own conclusions and read his work for themselves but this post isn’t really a fair critique of peat. The reason(one reason) why he thinks fructose is superior to glucose is its ability to promote liver glycogen storage, in a stressed state the body has a decreased ability to store liver glycogen and has to waste energy to create it. I suggest checking out his article on Glycemia, starch, and sugar in context, a critique of that would me much better. Also Ray Peat’s approach is based on a lot of things and has many factors, focusing on one part without looking at the whole won’t get you anywhere when it comes to his work.
Some random articles-
Fructose and dietary thermogenesis.-
“Fructose ingestion induces a greater thermogenesis than does glucose. This can be explained by the hydrolysis of 3.5-4.5 mol ATP/mol fructose stored as glycogen, vs 2.5 mol ATP/mol glucose stored. Therefore the large thermogenesis of fructose corresponds essentially to an increase in obligatory thermogenesis”
http://www.ajcn.org/content/58/5/766S.short
Sucrose ingestion normalizes ADX rats-
Adrenalectomy (ADX) changes CRF and NE activity in brain, increases ACTH secretion and sympathetic outflow and reduces food intake and weight gain; all of these effects are corrected by administration of adrenal steroids. Unexpectedly, we recently found that ADX rats drinking sucrose, but not saccharin, also have normal caloric intake, metabolism, and ACTH. Here, we show that ADX (but not sham-ADX) rats prefer to consume significantly more sucrose than saccharin. Voluntary ingestion of sucrose restores CRF and dopamine-beta-hydroxylase messenger RNA expression in brain, food intake, and caloric efficiency and fat deposition, circulating triglyceride, leptin, and insulin to normal. Our results suggest that the brains of ADX rats, cued by sucrose energy (but not by nonnutritive saccharin) maintain normal activity in systems that regulate neuroendocrine (hypothalamic-pituitary-adrenal), behavioral (feeding), and metabolic functions (fat deposition).
http://www.ncbi.nlm.nih.gov/pubmed/11415998
Dietary supplementation with n-3 fatty acids may impair glucose homeostasis in patients with non-insulin-dependent diabetes mellitus.-
“The blood glucose concentration tended to increase during MaxEPA treatment, and to decrease during the placebo period, the changes under the two regimes being significantly different (P less than 0.01). In addition, the rate constant for glucose disappearance (k value) for the intravenous insulin-tolerance test, which reflected the peripheral insulin sensitivity, tended to decrease during MaxEPA treatment and increase during administration of the placebo, there being a significant difference (P less than 0.03) between the changes during the two treatments.”
http://www.ncbi.nlm.nih.gov/pubmed/2394967
O3 deteoriates glycemic response-
“Average blood glucose concentrations during the third week were significantly higher fasting (+ 15%, p < 0.01), and during the day at 1100 h (+18%, p < 0.001) and 1500 h (+ 17%, p=0.002) on PUFA than on the saturated fat diet."
http://onlinelibrary.wiley.com/doi/10.1111/j.1464-5491.1992.tb01748.x/abstract
Gabriel brings up some good points. Peat only recommends sucrose as a supplement in the context of a nutrient rich diet. Its a fruit based diet and as far as I have seen fruits have been associated with pretty much nothing but benefits in the health literature.
A couple quarts of milk and OJ with a egg yolk or 2 will provide you with just about every nutrient, add some liver or shellfish and it becomes extremely nutrient dense.
That was interesting!
Looks like chocolate milk is again the winner for liver-glycogen replenishment.
Gabriel,
from where did you get the 33% macro thing? I actually figured that myself (didn’t found anything concrete in Peat’s writings) and always wondered why Danny emphasizes sugary carbs (55% of cals) so much.
And Peat is still kinda cool! 🙂
The 33% recommendation is probably old. Ray’s current line of thinking as far as I understand is that you should eat primarily carbohydrates to minimize PUFA but certain sources(butter, coco oil. ruminant fats) are fine in moderate amounts. He usually recommends around 80-120g of protein and the rest of your cals coming from carbs with fat added for taste(some people may need more fat depending on health circumstances). Its not a fat free diet though, probably 20-30% for the average person.
>High doses of fructose have observable harmful effects even in short-term studies.
Free fructose has been demonstrated harmful, but has sucrose?
Free fructose, including high fructose-ratio foods like soda, is commonly malabsorbed, and the malabsorbtion feeds pathogens. Fructose-liver harm can be “markedly reduced” by antibiotics, and antibiotics generally will prevent fatty liver, which suggest to me that fructose may only be indirectly related to fatty liver via malabsorption + microbes, rather than some effect of fructose on the liver.
Plus, the dies lab rates eat are deficient, and it seems likely the liver needs adequate supply of certain nutrients (like choline) to properly process sucrose. What about in those contexts, i.e. fructose delivered via sucrose + a nutritious diet?
Here are two reports where mice ate 40% to 67% of their diet as sucrose, and showed no harm, when they were fed nutritious diets:
http://jn.nutrition.org/content/3/1/61.full.pdf+html
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1275514/pdf/biochemj00921-0130.pdf
http://flare8.net/health/doku.php/when_fructose_is_bad
http://flare8.net/health/doku.php/diseases#microbes3
The benefits of fructose over glucose are beyond just refiling liver glycogen:
http://flare8.net/health/doku.php/fructose#benefits
Cliff’s probably right and the upper range of 20-30% gets you close enough. Let me add that having a Peat discussion on a this blog is epic! Central to Peat’s arguments regarding physical degeneration and longevity are PUFAs and their destructive synergism with estrogen via the stress response and diet. One way to avoid any excess PUFA would be to consume more starch and sugars from fruit, potato, and rice (all recommended in certain amounts by Peat with an emphasis on fresh fruit). If you lowered fat intake and increased carbohydrate intake your body would produce some fats from the carbohydrates in the form of saturated fats. This would be protective as it would lower exposure to PUFA.
“Sugar” is just one small part of Peat’s ideas and in my opinion should be addressed properly, which I feel wasn’t done here. Of course Paul was mainly responding to Danny’s post. I feel if Paul and Ray got together for an extended discussion of their respective research it would culminate in a more unified view. They each have different strengths.
I’m with JS on this one. Given the amount of glycogen flux that an athlete’s liver experiences, I don’t think it is particularly helpful for anyone to be referencing athlete studies as a model for what might occur in your average skinny-fatty wandering around.
Just on the superiority of glycogen reloading by adding fructose in the mix. Get it right, and there might be a slight advantage. Get it wrong, and the gastrointestinal distress caused by too fructose will soon outweigh any advantage fructose gives you at the liver. Particularly with fructose – ingestion is not the same thing as absorption.
Hi Paul,
I know white rice is generally preferred over brown rice as it doesn’t have the bran which may contain toxins, however in my search for rice syrup I was unable to find a decent white rice one on Amazon. Instead, I found an organic brown rice syrup that I’ve been using. Do you think this is an ok/PHD-safe product (maybe the way it’s processed removes the toxins?) or would white rice syrup still be preferred? If so, can you recommend one (preferably on Amazon). Here’s the one I’ve been using if you could share your thoughts: http://www.lundberg.com/products/syrup/Organic_Sweet_Dreams%C2%AE_Brown_Rice_Syrup.aspx
Thanks!
I still don’t know how one would get the fat under 30% (by Calories), while drinking plenty of milk, eating cheese, eggs and beef for 120g+ of protein.
And eating real ice cream too!
The only lean portein sources are shrimps/shellfish and bone broth/gelatin.
My carb intake is about 80g (320 kcals) a day, and that is very easy just to get from a moderate amount of fruits and sugary veg like beets, carrots, zucchini, etc. In fact, i do just that – i.e get nearly all my carbs from these sources, except a small amount from dairy sugars. Is this a problem?
Like others have said, i have never seen any studies anywhere that show moderate or even high intake of fruits or high carb containing veg is detrimental to health, and some studies actually have shown the higher the proportion of carbs coming from whole fruit, the greater the weight loss. E.g. this study http://www.ncbi.nlm.nih.gov/pubmed/21621801, which Lyle discusses here http://www.bodyrecomposition.com/research-review/the-effect-of-two-energy-restricted-diets-a-low-fructose-diet-vs-a-moderate-natural-fructose-diet-research-review.html.
Of course, its important to re-iterate that fruit carbs are not pure fructose, and even the most fructose containing fruits have only 2/3rds fructose and 1/3 glucose, and most only have a 1:1 ratio of fructose :glucose. So even if you got all your carbs from fruit and sugary veg, you wont be getting huge amounts of pure fructose.
This leads me to think that fructose as part of a package in whole food like fruit and veg is not detrimental to health and adequate for non-athletes
Sorry, i forgot to add that in the study i posted, the high fruit consumption group also significantly improved some key health markers like blood sugar and blood pressure, vs the low fruit group
Franco,
The 33% macro comes from an interview with Peat (EastWestHealing I think?). Peat appears not to care about macros much; he also said in the same interview that one could go high in any macro provided they are of good quality (I.e. low PUFA, not too much muscle meat etc). He prefers carbohydrate metabolism (more CO2 produced) as Cliff states but the body burns saturated fat at rest and most people need fat to balance blood sugar and feel satisfied so 30% should be enough for that.
Peat drinks 1% milk because fullfat can be fattening when it’s considered a protein source too (simply due to calories).
As Danny posted, a Peat-a-tarian diet isn’t a gigantic sucrose snorting fest. Sugar can help in restoring oxidative metabolism but fruit is better…
Peat isn’t against starches as such; he just thinks fruit is better for a number of reasons.
I eat Peat (although Peat and PHD are very similar) but I still consider myself influenced by PHD and recommend PHD as a go to read for nutrition for anyone who asks.
All the best Paul!
James
Hi James,
thanks for clearing that up for me. Danny somehow made it sound different (milk/eggs/cheese) in his quick-start guide and I couldn’t fit his sample meal plan to his macro-ratios (20% fat only) from the very same document, except by really eating lots of sugar.
Well, I eat PHD but I still consider myself influenced by Peat. 😉
Mostly for the higher protein but I even have a tbsp. of sugar in my coffee regularly!
Oh, I forget to say that Peat also has said the ”optimal” amount of fructose to glucose ”appears to be a 1 to 3 ratio”. But also thinks you can get all your carbohydrate from fruit nicely.
Franco, looks like even Sisson is using sucrose in coffee now! ha We better not go over 150g for fear of insidious weight gain though. 🙂 I personally view sucrose as similar to coconut oil. Fuel but no vitamins or minerals; both are ok in the context of a nutrient rich diet.
I don’t like labels much but I read every post here; which is only the case for a small number of blogs!
Yes.. 1 teaspoon of sugar in his coffee… enough calories to even be worth mentioning?
*1/3 to 2/3 ratio.
/need more coffee
@jamie-
“The synthesis of liver and muscle glycogen was studied in healthy volunteers given glucose and fructose infusions. In the course of 4 hours 21 to 26 mmol sugar per kg body-weight was given. Before and after the infusion the glycogen content was determined in needle biopsy material from liver and muscle tissue. The mean increases of liver glycogen after fructose and glucose infusions were 274.6 ± 25.87 and 76.2 ± 9.92 mmol glucosyl units per kg wet weight liver tissue, respectively. In muscle tissue the increase of glycogen was of the same magnitude for both sugars, corresponding to 23.0 and 24.4 mmol glucosyl units per kg after fructose and glucose, respectively.”
http://informahealthcare.com/doi/abs/10.3109/00365517409114190
Who gets gastrointestinal stress from eating too much sucrose(50/50 gluc/fruct) based sugars? No one unless they have severe dysbiosis.
While searching google scholar I came across this gem-
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC425376/
“Evidence has mounted that under physiological conditions glucose utilization by the liver is rather limited and that it is in fact a poor precursor for glycogen and fatty acids(much inferior to gluconeogenic substrate such as fructose, lactate or glycerol)”
http://en.wikipedia.org/wiki/Glucose_paradox
“The paradox is that the large amount of glycogen (10%) in the liver cannot be explained by its relatively minimal glucose absorption.”
Making glycogen from lactate or glycerol is anti-thyroid in peats opinion.
Paul,
Great article – I’ve got a few related questions concerning athletic performance and recovery:
* In your opinion, does nutrient timing come into play for high intensity and resistance workouts as far as DOMS, recovery, and overall fitness (the canonical example being “save the starchy carbs for post-workout”)?
* Is there any advise you can offer for pre-workout nutrition? Again, assuming we’re talking about high intensity and resistance.
* Do you agree with the nutrient timing advice given in Part I of the book “The Paleo Diet for Athletes” (if you’ve read it)?
Thanks!
-Marc
Paul, I always enjoy reading you blogs, they are very eye opening. You should receive Dr. Peat’s newsletter,it also is very eye opening, and is all based on past sceince(with ref.). I would really like to read your responses to what he writes about in his newsletters.
Hi Paul,
Thanks for the blog post.
I’ve interpreted PHD fructose/fruit consumption to be optional, even though it is generally included. More of a eat fruit/fructose for variety/pleasure to a certain limit to minimize its harmful effects and none is needed to have a healthy diet … optional source of potassium/fiber to supplement veggies … supplement C, and antioxidants may not have purported benefits.
Thanks,
Mark
Despite the sugar content, sugar types and the ratios, Orange Juice (OJ) has shown very significant benefits just by ingesting a few glasses per day.
Orange juice decreases oxidative stress, diabetes and cardiovascular risks
http://conference.ifas.ufl.edu/citrus/presentations/Wednesday/PM/0335%20Cesar.pdf
Extracted from there:
Orange Juice helps to prevent pre-disease conditions:
• Insulin Resistance and Metabolic Syndrome
• Type 2 diabetes and coronary heart disease
* Orange juice improved insulin sensitivity in all individuals
studied, regardless of their sex and BMI, observed as
decreased insulin secretion and reduction of the HOMA index
* Even though OJ add calories in diet, there were no alterations
in body weight, BMI, body fat or abdominal circumference
* OJ decrease inflammation and increased antioxidant activity
1)No effect on weight, BMI, body fat or waist circumf.
2)Less Cholesterol, LDL-C in normal and overweight individuals
3)Less Insulin (no glucose) = improvement insulin sensitivity
4)Less – CRP 13% in normal and 26% in overweight
5)More – 2.5 times antioxidant capacity in both groups
6)Less – 4% Systolic BP in normal weight individuals
7)Less – 4% Diastolic BP in overweight individuals
Plus more (see the pdf)…
Also, “Sugary Drinks, Not Fruit Juice, May Be Linked To Insulin Resistance”
http://www.sciencedaily.com/releases/2007/09/070905095319.htm
My own belief is that JS and Jamie are correct, most people’s levels of exercise render any slight advantage for fructose refueling a moot point. A much more common issue for folks eating a low fat wheat centric diet, is having to constantly stop and snack because they lack energy and get light headed. That used to be me.
One of my favorite forms of exercise these days is a fast round of golf on a hilly course carrying my clubs. I am lucky to have a couple friends who share this eccentricity, and most would agree we are all in pretty good shape for 50something year old women. However, I notice that this winter, I beat them to every elevated tee and green. They are huffing, I am not. They are waiting for me to tee off even if I don’t have the honors, because they need to catch their breath. They are wearing more clothes on a 38 degree day than I. And they absolutely cannot make it through the round without their apple and orange slices, their bananas, their vitamin water and what have you. When I politely refuse their generous offers to share, they can’t believe I don’t need to eat anything. When I describe my breakfast of a couple eggs, several tablespoons of saturated fat, and a serving a safe starch, I might as well have said I am a green blooded martian. The Peatatarians can have their OJ, I’ll take my PHD rocket fuel.
2 months ago I was explaining the PHD to them and they replied to fructose being low that low fructose was odd considering we evolved from monkeys that eat so much fruit. I had no reply and this left me puzzled about fructose in context of evolution.
If we evolved from monkeys, then we started out at least eating much higher amounts of fruit and fructose, right? Do monkeys handle fructose any better than us? Does the monkey diet concept of them eating lots of bananas a myth? Or has humans just evolved for so long away from jungles that we changed to handling safe starches/glucose more and less fructose? Yet, Paul has mentioned we really started in earliest evolution with processing glucose first, so???
Hi Paul,
What I think is oft neglected when considering Peat is the hormonal reaction to foods. Though taking in ice cream and orange may not be optimal (not terrible either), I think the hormonal reduction of estrogen, glucocorticoids, and promotion of pregnenolone,etc. plays an important role in correcting a persons health. I think that people with metabolic syndrome and such have a hormonal disruption that is neglected. Maybe the optimal course for correcting health in some people is to take in foods that provide a positive hormonal reaction, while continuing to take in other highly nutritious foods to correct other disruptions–attacking the problem from multiple facets. In this manner highly nutritious foods are the major consituents of a long term correctional protocol, while sugary foods(and such) are part “supplementary” foods that provide an acute spark of supportive hormones (so that as the person becomes healthier they can probably be reduced more and more).
Just as a side note, I think it’s interesting that overeating, or eating of sugary foods,etc., are not necessarily damaging to a healthy person– i.e. when healthy people overeat or under eat they return to normal weight under subsequent ad libitum conditions. It’s probably also interesting that though a person with metabolic disorders will feel terrible most of the time, with periods of relief brought on after consumption of these sugary foods, or just overconsumption in general–signaling the possibility of beneficial hormonal (or some other) effects. In this paradigm the biggest problem seems to come from the chronic intake of toxins that separates the healthy person from the unhealthy.
Hi Paul,
How much can we extrapolate from the idea the fructose+glucose is [likely] better than glucose at repleting glycogen? First, this says little about overall health. Second, as you mention, this says little about the advantages of a 30% fructose diet vs a 10% one. Third, carbohydrate source and amount is not the only factor that affects glycogen storage/repletion.
Studies that involve rodents use diets that contain so many refined ingredients, and results are all over the place. It’s difficult to come to any confident conclusion when you’re looking at cornstarch vs sucrose, or, in the case of flare’s links above, multiple variable changes.
Peat and followers also use the idea that fructose+glucose stimulates glucose oxidation moreso than starch (and fat obviously). But, I’ve never seen direct evidence that this is a positive (in fact Lucas Tarfur makes a strong case for fatty acids and ketones being superior) besides the fact that glucose oxidation produces more CO2, which is another questionable extrapolation to overall health. Anyway, high carb/sucrose diets don’t necessarily increase CO2: there are studies that show respiration is less efficient with high carb, so that the expected increase in CO2 doesn’t happen, because there is more lactate produced.
I really enjoy Peat’s writing and ideas, but I don’t see the need to put him up on a pedestal and act like everything he says is gospel, which many of his followers do.
Oh, and although it’s not a “scientifically valid” conclusion, I think it is telling that cultures like the Kitavans favor starches over fruits, despite both being widely available (I’m not 100% sure that’s true though).
lenny,
The problem is that Peat’s recommended dietary changes don’t necessarily lead to beneficial changes in those hormones, or at least there is a lack of evidence.
Rat metabolism of fructose is a very poor model for examining human metabolism of fructose. Previous studies have shown that rats suffer much more damage from high (artificial) fructose feedings than human subjects. Alan Aragon did a whole analysis about this in a previous issue of AARR
Paul, what do you make of this rodent study comparing starch/sucrose/fat based diets?
http://jn.nutrition.org/content/136/3/582.full
How is it that LIFE-LONG feeding of a 56% refined sucrose diet did not cause these mice any ill effects compared to starch-fed mice, no obesity, no fatty liver, no elevated blood lipids, no insulin resistance, if fructose is a poison? They also had lower micronutrient intake than the starch-fed mice. I have to say studies like the above made me very skeptical that sucrose poses any particular threat at all.
The PHD is evidence-based; everything is truly backed and few things (if any) are left as simple opinions or beliefs. That is in part why it gives it way more credibility than other diets, including the standard Paleo Diet, IMHO. To that, add the many positive testimonials from PHD adopters and you have an excellent reference diet for health.
It’s unfortunate, but many Peat followers do blindly follow him, without questioning almost anything he mentions. But it is also true that those who critizice the work of Dr. Peat seem that they have never taken the time to actually read his essays, where he does provide justifications and references.
People has to understand that what he recommends is something optimal based on his knowledge, views and experimentation for optimal health and doesn’t consider evolution as far as I know, only pure biology and biochemistry. As I undertand it, dismissing his recommendations as a “High Sugar” diet is unfair and demonstrates ignorance on his work.
Peat has on his side that he’s a Ph.D in Biology, with decades of experience and knowledge so to me it is interesting to lissten to what he has to say. He’s not looking to create a movement as I see it, the people who follow his work probably are.
The plot thickens. Many very interesting comments in this thread.
Enrique, I don’t think many of us want to start a movement, but just get better. Interesting post Paul, good to see you replying so promptly to Danny’s post.
this comment thread is gonna get awesomely insane!
i’m going to tell my story here because i experiment with a mixture of ideas – given that everyone is unhealthy in their own way, self-experimentation is key.
due to my leaky gut and dysbiosis, safe starches screw with me, fatigue, constipation, bloating. even some fruit does this: bananas i’m talkin’ to you!
it has been a struggle to gain a surplus of energy without resorting to caffeine. upon experimenting with brown rice syrup, i improved a bit, but not enough for my tastes.
exploring peat-eating, i increased simple sugars. i find that i can tolerate well fruits, fructose and sugar, sucrose TO A POINT. after that point i can feel my liver become swollen and then i am overfull with fructose.
i can ingest lots of dextrose and it suits me better than brown rice syrup, so a mixture of more dextrose and less fruits is a good combo for me, but i have to monitor the liver swollen-ness thing. it’s easy to overeat sweets, even fruits.
as for blood sugar and crashing, i ingest my sugar right before a high protein meal. i do not “crash” any more or less than i did before on a lower-carb diet, presumably because now i am eating a high protein diet and 16:8 Intermittent fasting each day.
here’s where other things diverge as well. i eat very high protein, somewhere along the lines of 2-2.5g protein per kg of bodyweight. this helps with satiety, and i do not want my protein being used as blood sugar so i try to get at least 200g or more of carbs a day. i feel better on more carbs. this is key. but i also eat limited PUFA and since increasing the carbs and protein i eat LESS healthy fat in general.
the rest of my calories come from fat. i eat big in that 8 hour window and have some yerba mate to help digest.
i do also take lots of supplements to heal my leaky gut, as well as many of phd recommended supplements. as you can see, this is a mixture of phd, lalonde-paleo, kresser-paleo, harris-paleo, and peat. i am intolerant to casein, so no dairy except for grass fed ghee, and i eat very little vegetables. even peat’s recommendation of raw carrots for gut health causes my small intestine to rumble uncomfortably.
i think there may be something specific about me, perhaps my past and genetics does not allow my liver to function optimally, therefore having some fructose malabsorbtion issues, whereas other people process fructose well. there may be many other factors at play – perhaps having a super liver that is challenged everyday by that amount of fructose has some other knock-on health benefits. perhaps the dairy inclusion is helping, or perhaps other positive hormonal thresholds must be met which help the entire system offset any possible damage done by the bolus of fructose.
someone please correct me but … for dieters, liver glycogen is much more important. I’ve read a bunch of times how liver glycogen is one of the things that determines how hungry one is.
Why is anyone arguing for better muscle glycogen replenishment, when most non-athletes do very little exercise that’s in the intensity ranges that require muscle glycogen.
> as for blood sugar and crashing, i ingest my
> sugar right before a high protein meal.
> i do not “crash” any more
That’s interesting … I remember reading a paper where sugar plus cottage cheese caused twice the insulin spike as just sugar.
So for you anyway, it may not be (insulin ->force -> low blood glucose) that causes your “sugar crashes”
sam, since i don’t have any sugar crashes i don’t know what causes them… i’m just sayin’.
OK, thanks … read that part of your post too quickly.
@sam-maybe you should read the comments, specifically mine.
hi Cliff – I did read your posts, my question was why the overall discussion regularly veers off to emphasise athletes and muscle glycogen, while downplaying the area that’s probably much more important to regular dieters.
@sam- You have to ask paul about that. The studies were posted on dannys blog in response to another commenter wondering about fructose’s ability to refill muscle glycogen. If you read dannys original blog post and peats work they are much more interested in liver glycogen as it supports thyroid function, hence the emphasis on fructose. Danny’s original post(which this blog post is a reply too) doesn’t mention muscle glycogen one time, when he says refills glycogen he is referring to liver glycogen.
Thanks for the well-reasoned update on sugar. You already had me convinced a year ago when I read your book, but, as you noticed, the fructose cheerleaders have been vocal recently.
I have cut way back on my fruit consumption during the past half year, ever since I noticed that my ear canals would start itching after eating an apple or a half cup of berries. Wish I knew what that was about.
Danny Roddy made a typo…
Peat has stated that … fructose … “powerfully” refills glycogen …
SHOULD BE
Peat has stated that … fructose … “powerfully” refills LIVER glycogen …
WHICH would create a whole new argument for PJ to discuss
@KIRKC- Apples are very starchy and raw starch creates inflammation by feeding bacteria. Berries have lots of little seeds that create inflammation by feeding bacteria and the little seeds can get stuck in your colon and create diverticulitus. Ray Peat recommends Orange Juice and other tropical fruits with low serotinin and low starch content.
ALL ORGANISMS CAN USE SUGAR AS FUEL NOT THE SAME FOR STARCH
Hi Gabriel,
Thanks for summarizing Peat’s ideas, which I am not intimately familiar with. It still sounds like an excessive amount of fructose to me.
But I very much agree with his deprecation of PUFA, so we do have a lot of common ground.
Hi cliff,
I was directly addressing the role of fructose in replenishing liver glycogen. Whether there are benefits to more effective replenishment of glycogen is another topic; it seems to me difficult to make this case.
More thermogenesis from fructose is what you would expect from ingesting a toxin. The body tries to dispose of it as quickly as possible, even if that means generating waste heat.
That paper on ADX rats doesn’t even compare sucrose to other macronutrients.
Since we share Peat’s distaste for polyunsaturated fats, I’m not sure why you include your last two references.
Hi Franco,
Chocolate milk does seem like a good choice for liver glycogen!
Hi flare,
I agree that micronutrition can make a big difference. Doesn’t that make recommendations to drink low-nutrient-density sugary beverages suspect?
Some of the “benefits” of fructose you cite I see as defects.
Hi Tea,
Tapioca syrup is available at Amazon. But that brand of brown rice syrup is OK. It’s sold at our local Whole Foods.
Hi Rob,
We support natural foods. It’s the added sugar, eg orange juice or soda or other sucrose sources, that I object to.
Hi JRAC,
If the fructose to glucose ratio is 1:3, or 25% fructose, then it’s not that far apart from my 15% fructose. Hardly worth arguing over.
But Danny thought there was a difference worth critiquing. Perhaps his emphasis should have been on quantity of carbs, rather than sugar/fructose?
Hi Marc,
Yes, I think nutrient timing matters, but it depends on the type of exercise you are doing and I am not expert in this literature. For most people doing casual exercise I would recommend exercising fasted and then eating sufficient carbs post-workout.
For resistance exercise, a bit of protein pre-workout is probably helpful, but not too much – less than 10 g. The workout should be at least 3 hours since the previous meal.
I haven’t read The Paleo Diet for Athletes.
Hi Kevin,
I agree, I should subscribe to his newsletter. But I have so much that I lack time to read already!
Hi MarkES,
Lots of foods are optional individually, but since food variety is a desirable trait of a diet (one of the “Eat Paleo not Toxic” recommendations), it’s good to incorporate optional items, just not in huge doses. And pleasure is a positive goal also.
Hi Enrique,
Oranges would have worked as well as orange juice. And not a large number of oranges, either.
Epidemiological evidence is of course going to blame soda, which has increased, not fruit juice, which has decreased, for rising incidence of metabolic syndrome. That doesn’t mean fruit juice is benign.
Hi Kate,
Great story! Maybe if your scores improve too, they’ll try your diet.
Hi Jaybird,
First, the ape-monkey divergence was 24 to 29 million years ago (http://news.discovery.com/human/monkey-ape-fossil.html), so there’s been a long evolutionary time since. And bipedal grassland dwelling apes are known to have lived 20 mn and 7 mn years ago. There’s reason to believe that the common human-chimp ancestor was a grassland dwelling bipedal starch eater, not a forest-dwelling fruit eater. It may be that chimps and gorillas evolved for fruit eating, not humans for other foods.
But even if our distant ancestors ate fruit in quantity, this doesn’t make it optimal. It’s best to eat nutrients our body can incorporate in tissue. Fructose isn’t one of them.
Hi Lenny,
This seems to me a pharmaceutical approach to food: People have some pathology, characterized by faulty hormone levels, and ice cream and orange juice can treat it. I don’t believe this model. At least, it should begin by telling us exactly what the pathology is, and who has it, and show us evidence that ice cream and orange juice effectively treat it. (If the pathology is metabolic syndrome, I don’t believe they do.) If everyone has the pathology, then why did evolution give us an obligate requirement for orange juice and ice cream?
Hi John,
I agree. Stimulation of oxidation / metabolism is in most cases a negative, not a positive. Also, short term effects and long term effects may be opposite.
Hi Collden,
Rodents have trouble with high-fat diets. Sucrose is mainly a problem in combination with PUFA, but this study gave milkfats, very low in PUFA. The starchy diet had a better glycemic response to the OGTT than the sucrose diet. Overall, I don’t see anything to recommend sucrose in the study. Mice tolerate it as long as there are very low PUFA in the diet.
Hi Enrique,
Peat is certainly very interesting. His website doesn’t always link cites to statements closely, and it is hard to tell in what contexts his ideas are valid. I think there’s insight there but it is hard to chase down exactly when his insights are useful.
Hi Darius,
Thanks for sharing. Dextrose should indeed by the most tolerable carb in cases of gut dysbiosis.
Hi Kirk,
I’m afraid I don’t know what that’s about either, but congratulations to you for figuring out the cause!
Best, Paul
Ray Peat also recommends low fiber so strained Orange Juice because the fiber feeds bacteria which creates inflammation.
ALL ORGANISMS CAN USE SUGAR AS FUEL
NOT ALL ORGANISMS CAN USE STARCH AS FUEL