The gut is the front line of health. The human gut houses 100 trillion bacteria from a thousand different species [1]; they weigh several pounds and make up about half the dry weight of stool. To control these bacteria 70% to 80% of the body’s immune cells are normally found in and around the gut.
A healthy gut is protected by a mucosal layer that is designed to promote commensal (friendly) bacteria, while providing a barrier to pathogenic bacteria. Humans have evolved ways to “feed” commensal species of bacteria. For instance:
- Human mucus is made of glycoproteins, or compounds made of protein and sugar. Certain probiotic bacteria, such as Bifidobacterium bifidum, are able to digest human mucus. [2] Thus, the human intestine has evolved to produce “food” for beneficial gut bacteria, assuring that they are maintained even during long fasts.
- Mother’s milk contains special sugars, called human milk oligosaccharides, which specifically feed Bifidobacterium bifidum and assure that this species successfully colonizes the baby’s intestine and wards off infection. [3]
The absence of this protective barrier of mucus and friendly bacteria makes the intestine extremely vulnerable to infectious disease. Premature babies who are fed formula, not human breast milk, often contract a dangerous intestinal infection, necrotizing enterocolitis. [3]
In addition to pathogenic bacteria, the gut is confronted by a heavy load of toxins. Bruce Ames and Lois Gold have estimated that the average person eats 5,000 to 10,000 different plant toxins, amassing to 1500 mg per day, plus 2000 mg of burnt toxins generated during cooking. [4]
Today’s post will focus on how those 1500 mg of natural plant toxins damage the intestinal wall and its mucosal barrier, thereby bringing about infectious bowel diseases.
Cereal Grain Toxicity
Grasses became the staple foods of agriculture because of their rich yields: a single plant may generate tens of thousands of seeds annually.
Yet this prolific seed production has always made grasses attractive to herbivores, and caused seeds to evolve high levels of toxins designed to poison mammalian digestive tracts, thus enabling their seeds to pass through herbivore guts undigested. It is these toxins that make the cereal grains so dangerous to human health.
The effectiveness of grain toxins at sabotaging human digestion is illustrated by the increase in fecal mass they produce:
For every gram of wheat bran eaten, fecal weight increases by 5.7 grams. [5]
By inhibiting human digestion, wheat toxins dramatically increase the amount of undigested starch reaching the colon. This increased food supply substantially increases the bacterial population – and the presence of starch, which is ordinarily unavailable in the colon, favors the growth of pathogenic species.
Unfortunately wheat toxins do much more than inhibit digestion of food. They also damage the gut itself.
Wheat contains an ingenious cocktail of toxins:
- Gluten, a complex of proteins, inspires on immune response which inflames the intestine in at least 83% of people [6], and makes the intestine permeable, allowing gut bacteria and their toxins to enter the body. [7] Gluten triggers anti-wheat antibodies in at least 30% of the population, and auto-antibodies – that is, antibodies that attack human cells – in at least 0.4% of the population. [8] These unlucky folks suffer celiac disease, which devastates the intestine, as well as autoimmune thyroiditis. [9]
- Opioid peptides produce effects similar to morphine and heroin. Wheat opioids have been implicated as causes of schizophrenia. [10]
- Wheat germ agglutinin is a lectin, or protein that binds sugars. At extremely low doses, a few parts per billion, WGA causes gut inflammation and leakiness. At typical dietary doses, WGA causes shedding of the intestinal brush border and shrinkage in the surface area of the intestine. [11] WGA alone can induce celiac disease in rats. [12]
By unknown mechanisms, grains can induce vitamin deficiency diseases. Wheat and oats induce rickets [13] while corn induces pellagra. [14]
Since as little as 1 milligram of gluten per day can prevent recovery from bowel disease [15], it is essential that grains be eliminated entirely from the diet.
Legume Toxicity
Legumes also contain an array of toxins which suspend digestion and damage the gut. Some examples:
- Phytohaemagglutinin, a kidney bean lectin, makes the gut leaky; blocks stomach acid production, promoting bacterial overgrowth of the small intestine; overpopulates the gut with immature cells that are easily colonized by E. coli and other pathogens; disturbs the mucus and shortens villi. [16]
- Alpha-amylase inhibitors in legumes prevent starch digestion and leads to gut bloating and multiplication of pathogenic gut bacteria. [17]
- Antibodies to soy proteins have been identified in duodenitis, Crohn’s disease, ulcerative colitis, and coeliac disease, and these diseases are sometimes cured when soy is removed from the diet. [18]
It should be noted that peanut and soybean allergies are among the most common allergies. This testifies to the significant immune response legume toxins can generate.
Omega-6 Toxicity
Most people are familiar with the evidence linking the omega-6 to omega-3 ratio to cardiovascular disease. Most Americans have an omega-6 to omega-3 ratio in tissue that is ten-fold too high; cultures with a better omega-6 to omega-3 ratio, such as Greenland Inuit and Japanese, have much lower rates of heart disease.
Since the effect of an excessive omega-6 to omega-3 is to greatly increase inflammation while impairing immune function, it’s logical that an elevated ratio would worsen inflammatory bowel disease.
And it does. The EPIC (European Prospective Investigation into Cancer and Nutrition) study took food diaries from 203,193 people and followed them for four years [19]:
- Being in the upper quartile of intake of omega-6 fatty acids raised the risk of ulcerative colitis by 149%.
- Being in the upper quartile of intake of the omega-3 DHA, which is abundant in salmon and sardines, reduced the risk of ulcerative colitis by 36% – 77% after adjustment for omega-6 intake. (Apparently those who ate more omega-3s also ate more omega-6s.)
Another study found that being in the upper third of DHA intake reduced the risk of ulcerative colitis by about 50%. [20]
The upshot: anyone with inflammatory bowel diseases should strictly limit omega-6 consumption and strive to eat a pound per week of salmon or sardines.
Fructose Toxicity
Fructose is a sugar that is toxic and useless to humans – but it is a rich source of energy to bacteria. Fructose consumption strongly promotes bacterial growth in the intestine and increases levels of bacterial endotoxins in the body. [21]
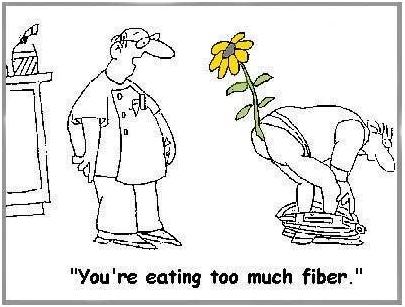
Of Fiber
Most people think that fiber is indigestible, and that it comes out in their stool. This is not true. Fiber is indigestible to humans, but not to bacteria. Fiber is bacterial food that enables gut bacteria to multiply. Bacteria, not undigested food, make up most of the dry weight of stool. [22]
Doctors often recommend fiber to bowel disease patients. While not wholly without merit, this advice usually backfires.
There are three problems: helping bacteria feed and multiply may be undesirable; fiber, such as the brans of cereal grains, often contains toxic proteins; and, finally, whole grain fibers and other “roughage” scrape and injure the intestinal wall. Dr. Paul L. McNeil explains that:
When you eat high-fiber foods, they bang up against the cells lining the gastrointestinal tract, rupturing their outer covering. [23]
That can’t be a good thing.
And it isn’t. In the Diet and Reinfarction Trial (DART), published in 1989, 2,033 British men were divided into a high-fiber group and a control group. The high-fiber group ate whole grains and doubled their grain fiber intake from 9 to 17 grams per day. The result? Deaths in the high fiber group were 22% higher over the course of the study – 9.9% of the control group died versus 12.1% of the high-fiber group. [24]
Softer soluble fibers from fruits and some vegetables are much more likely to help than wheat bran, but even they may be a good thing only in moderation, or only in a healthy bowel. Fiber feeds pathogenic bacteria as well as probiotic bacteria, and increases the populations of both. When the gut is damaged and leaky, more bacteria mean more bacterial toxins and more pathogens infiltrating the body. A low-fiber diet, leading to reduced bacterial populations in the gut, may be desirable for bowel disease patients.
Yes, it is possible to get too much fiber!
(via Peter at Hyperlipid)
Other Toxic Foods
Nightshade plants and seeds of all species can also contain toxins and may also need to be restricted in people with damaged intestines.
Dairy proteins, especially pasteurized cow casein, are also often problematic for people with damaged intestines.
In general, any foods that commonly produce allergies are likely to give trouble to people with damaged intestines.
All plant proteins are risky, as are dairy and egg proteins. It is possible to minimize risk by:
- Eating clarified butter, but refraining from protein-rich dairy foods.
- Eating cooked egg yolks, but avoiding the protein-rich egg whites.
Summary of Toxic Foods to Eliminate or Avoid
In short, bowel disease patients should eliminate toxic foods from their diet:
- Eliminate all grains except rice. Wheat, oats, and corn, and their products such as wheat flour, cornstarch, bread, and pasta, must be eliminated.
- Eliminate all legumes, especially soy, beans, and peanuts.
- Eliminate omega-6 rich oils, such as soybean oil, safflower oil, corn oil, peanut oil, and canola oil.
- Eliminate fructose sugars, except from fruits and berries. Drink no sugar-containing beverages.
- Minimize fiber to keep down gut bacterial populations and avoid mechanical injuries to the intestinal wall.
- Minimize other potentially toxic protein sources. In general, protein should be obtained from animal and fish meats, not eggs, dairy, or plants. However, fats from dairy and eggs are highly desirable.
When gut health is restored, dairy and fiber may be restored to the diet. However, the major toxic foods – grains, legumes, omega-6-rich oils, and most fructose – should be eliminated for life.
Filling the Gaps in the Diet
For most people, eliminating grains will leave a large gap in the diet. Foods that should be used to fill that gap include:
- Healthful plant foods are the safe starches, such as white rice, taro, sweet potatoes and yams, and fruits and berries.
- Saturated-fat rich oils and fats, like beef tallow, clarified butter, coconut oil, palm oil, cocoa butter (yes, chocolate desserts are healthy!), along with modest quantities of olive oil and lard. Make homemade salad dressings with these oils, rather than buying supermarket dressings made with soybean or canola oil.
- Further balance the omega-6 to omega-3 ratio by eating low-omega-6 meats, such as the red meats (beef and lamb) and seafood, and eating 1 lb per week salmon or sardines for fresh omega-3 fats.
When the small intestine is damaged, fatty foods may be difficult to tolerate, since the enzymes that digest dietary fats and proteins may also digest human cells. In such cases the diet must focus on starchy foods like rice until bowel health is restored. Be sure to supplement with vitamins and minerals in such cases.
Conclusion
Eliminating food toxins may cure bowel diseases and always improves prognosis. Pedro Bastos of The Paleo Diet Update writes:
From the feedback we have received over the years, IBS patients respond dramatically and rapidly to the Paleo Diet. Their experience indicates that milk, grains and legumes seem to be the main culprits in this condition via a number of mechanisms. [The Paleo Diet Update v.4, #18]
Auto-antibodies generated by wheat against the thyroid, pancreas, and gut typically disappear within 3 to 6 months after removal of wheat from the diet. [25, 26] This is probably a reasonable estimate for the time frame in which bowel disease patients can expect significant improvements from the elimination of dietary food toxins.
Related Posts
Other posts in this series:
- Bowel Disorders, Part I: About Gut Disease July 14, 2010
- Bowel Disease, Part III: Healing Through Nutrition July 22, 2010
- Bowel Disease, Part IV: Restoring Healthful Gut Flora July 27, 2010
References
[1] Fujimura KE et al. Role of the gut microbiota in defining human health. Expert Rev Anti Infect Ther. 2010 Apr;8(4):435-54. http://pmid.us/20377338.
[2] Ruas-Madiedo P et al. Mucin degradation by Bifidobacterium strains isolated from the human intestinal microbiota. Appl Environ Microbiol. 2008 Mar;74(6):1936-40. http://pmid.us/18223105.
[3] Bode L. Human milk oligosaccharides: prebiotics and beyond. Nutr Rev. 2009 Nov;67 Suppl 2:S183-91. http://pmid.us/19906222. Hat tip Dr. Art Ayers.
[4] Ames BN, Gold LS. Paracelsus to parascience: the environmental cancer distraction. Mutation Research 2000 Jan 17; 447(1):3-13. http://pmid.us/10686303
[5] Cummings JH. The effect of dietary fibre on fecal weight and composition. Pp 547–73 in: Spiller GA, ed. Handbook of dietary fibre in human nutrition. 2nd ed. Boca Raton, FL: CRC Press, 1993.
[6] Bernardo D et al. Is gliadin really safe for non-coeliac individuals? Production of interleukin 15 in biopsy culture from non-coeliac individuals challenged with gliadin peptides. Gut 2007 Jun;56(6):889-90. http://pmid.us/17519496.
[7] Drago S et al. Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scand J Gastroenterol. 2006 Apr;41(4):408-19. http://pmid.us/16635908.
[8] Not T et al. Celiac disease risk in the USA: high prevalence of antiendomysium antibodies in healthy blood donors. Scand J Gastroenterol. 1998 May;33(5):494-8. http://pmid.us/9648988.
[9] Sollid LM, Jabri B. Is celiac disease an autoimmune disorder? Curr Opin Immunol. 2005 Dec;17(6):595-600. http://pmid.us/16214317.
[10] Singh MM et al Wheat gluten as a pathogenic factor in schizophrenia. Science. 1976 Jan 30;191(4225):401-2. http://pmid.us/1246624. Dohan FC et al 1984 Is schizophrenia rare if grain is rare? Biol Psychiatry. 1984 Mar;19(3):385-99. http://pmid.us/6609726.
[11] Lorenzsonn V, Olsen WA. In vivo responses of rat intestinal epithelium to intraluminal dietary lectins. Gastroenterology. 1982 May;82(5 Pt 1):838-48. http://pmid.us/6895878.
[12] Sjölander A et al. Morphological changes of rat small intestine after short-time exposure to concanavalin A or wheat germ agglutinin. Cell Struct Funct. 1986 Sep;11(3):285-93. http://pmid.us/3768964.
[13] Mellanby E. (March 15 1919) An experimental investigation on rickets. The Lancet 193(4985):407-412.
[14] Carpenter KJ, Lewin WJ. A critical review: A reexamination of the composition of diets associated with pellagra. J Nutr 1985 May;115(5):543–552. http://pmid.us/3998856.
[15] Biagi F et al. A milligram of gluten a day keeps the mucosal recovery away: a case report. Nutr Rev. 2004 Sep;62(9):360-3. http://pmid.us/15497770.
[16] Kordás K et al. Phytohaemagglutinin inhibits gastric acid but not pepsin secretion in conscious rats. J Physiol Paris. 2001 Jan-Dec;95(1-6):309-14. http://pmid.us/11595455. Pusztai A et al. Kidney bean lectin-induced Escherichia coli overgrowth in the small intestine is blocked by GNA, a mannose-specific lectin. J Appl Bacteriol. 1993 Oct;75(4):360-8. http://pmid.us/8226393. Prykhod’ko O et al. Precocious gut maturation and immune cell expansion by single dose feeding the lectin phytohaemagglutinin to suckling rats. Br J Nutr. 2009 Mar;101(5):735-42. http://pmid.us/18644165.
[17] Pusztai A et al. Inhibition of starch digestion by alpha-amylase inhibitor reduces the efficiency of utilization of dietary proteins and lipids and retards the growth of rats. J Nutr. 1995 Jun;125(6):1554-62. http://pmid.us/7782910.
[18] Haeney MR et al. Soya protein antibodies in man: their occurrence and possible relevance in coeliac disease. J Clin Pathol. 1982 Mar; 35(3):319-22. http://pmid.us/7040491.
[19] IBD in EPIC Study Investigators. Linoleic acid, a dietary n-6 polyunsaturated fatty acid, and the aetiology of ulcerative colitis: a nested case-control study within a European prospective cohort study. Gut. 2009 Dec;58(12):1606-11. http://pmid.us/19628674.
[20] John S et al. Dietary n-3 polyunsaturated fatty acids and the aetiology of ulcerative colitis: a UK prospective cohort study. Eur J Gastroenterol Hepatol. 2010 May;22(5):602-6. http://pmid.us/20216220.
[21] Bergheim I et al. Antibiotics protect against fructose-induced hepatic lipid accumulation in mice: role of endotoxin. J Hepatol. 2008 Jun; 48(6): 983-92. http://pmid.us/18395289.
[22] Stephen AM et al. Effect of changing transit time on colonic microbial metabolism in man. Gut. 1987 May;28(5):601-9. http://pmid.us/3596341.
[23] Quoted in Science Daily, http://www.sciencedaily.com/releases/2006/08/060823093156.htm. Hat tip Dr. Michael Eades.
[24] Burr ML et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989 Sep 30;2(8666):757-61. http://pmid.us/2571009. Hat tip Stephan Guyenet.
[25] Berti I et al. Usefulness of screening program for celiac disease in autoimmune thyroiditis. Dig Dis Sci. 2000 Feb;45(2):403-6. http://pmid.us/10711459.
[26] Mainardi E et al. Thyroid-related autoantibodies and celiac disease: a role for a gluten-free diet? J Clin Gastroenterol. 2002 Sep;35(3):245-8. http://pmid.us/12192201.











Heya i’m for the first time here. I found this board and I in finding
It truly useful & it helped me out much. I am hoping to give one
thing back and help others such as you helped me.
Also visit my page – irritable bowel syndrome symptoms diagnosis
Thank you for all of this information. I was diagnosed with pancolitis last year (hospitalized… not a good time) but have been in remission for quite a while now thanks to meds. Being on meds indefinitely and feeling fine – is there still a need to make a diet change? I was a vegetarian for 18 years before I got sick, and started eating meat again after because of protein deficiency. Would returning to vegetarianism be a bad idea given your info on legumes?
I would like to mention that a1 casein in Holstein cow’s milk is a major problem for myself; far worse than the gluten in wheat in terms of intestinal problems, damage, and autoimmune problems (including frequent colds and flus). However, I do seem to be able to tolerate a2 casein (sheep and goats milk) in moderation.
This website has been helpful in determining the level of dairy intolerance. When it comes to Holstein cow’s milk dairy products, I am at Level 5 (Serious Intolerance) which restricts this type of dairy to grass fed butter only. I can also handle goats milk butter without problems as well.
http://failsafediet.wordpress.com/the-rpah-elimination-diet-failsafe/gluten-and-casein-responders/
What about Quinoa?
Your use of the quote re: fibre “banging up against”/tearing the walls of the GI tract is extremely misleading; that quote is part of an article about a recent study looking at the POSITIVE effects of grain fibre on the GI tract. The conclusion this study reaches is that the physical ‘ micro-damage’ done by grain roughage causes extra mucosal excretion from the cells in the gut wall- which is, according to the study, unequivocally a *good* thing. Just like the micro damage caused by weight lifting can have an overall positive effect, is an analogy, as far as i see it.
But since you have the link up, you must have read it. ??
I am not trolling here- I have GI issues, looking for information. This sort of stuff is a shame- you may have a great message, but to a science orientated person in particular, that sort of “sly” referencing just screams ” run away”. Sorry- but it really does :S
Hi Alex,
Yes, of course I’ve read it. There’s no known mechanism by which injuring the gut leads to improved gut health or an improved gut microbiome. That was pure speculation on his part trying to preserve a presumption – that wheat bran is beneficial – in the face of contrary evidence that it injures the gut. But the DART trial indicates that the presumption that wheat bran is healthful is false.
Best, Paul
http://www.drperlmutter.com/wp-content/uploads/2013/10/Physiol-Rev-2011-Fasano-151-75.pdf
Hi Paul,
Thanks for the reply.
I don’t mean to be a pain; you may well be right that grains are harmful. But “pure speculation on his part trying to preserve a presumption” seems a bit rough ( excuse the pun). There was actually repeatable data in the study, and there is reasonable backup for the idea that mucosal excretion is supportive of gut motility and ( I think??) of good microbes. I’m winging it a bit there- I think I read that in a study somehwere..too tired to fact check it just now…But the gist is, all that is definitely not a completely wild and unfounded claim on their part. UNless I missed something, I don’t believe wheat bran was ever mentioned.
And it was still a sly reference- you can’t use the man’s words to strengthen and give credence to your argument like that, failing to mention the context and intention behind them. You know 90% of people never check references.
Lastly, that damage is *always* bad is unclear. The muscle tearing example is a good one; not quite analogous, but similar, is the damage to skin in making Vitamin D. All sun exposure slightly damages skin, but we must have Vitamin D.
The damage to cells that is discussed in the paper is microdamage- it’s “scuffing” if you like. The language used casually by Dr. McNeil to create an image for a layperson ( which is clear if you read the article itself in detail) becomes extreme and dangerous sounding out of context. Which I think you *must* be aware of. That was a bit cheeky!
Alex Gray
hi Alex,
does it mention in the study how long it takes the gut wall to fully repair from the micro damage
Hi Paul,
I have severe SIBO, leaky gut, and slow-transit constipation. Since other treatments haven’t provided sustained benefit, I am about to try an elemental diet for at least 1-2 months. This will consist of only hydrolyzed whey protein, hydrolyzed collagen, dextrose powder, MCT oil, multivitamin and electrolytes.
Do have any thoughts on using an elemental diet to heal the gut? Would you recommend the same macronutrient ratios as the PHD, even though all food is absorbed rapidly and will cause a large spike in blood glucose? Any ideas for how I can minimize the harmful effects of spiking insulin, since I don’t usually tolerate high-GI carbs well?
Thank you for your help.
Hi Greg,
I don’t recommend it because that will starve gut flora of fiber and is also deficient in key nutrients besides the vitamins and minerals.
I would start with vitamin A/D/C, circadian rhythm entrainment, extra choline and inositol / egg yolks, and intermittent fasting; and then work on fiber and fermented foods.
Thank you very much for your reply. I should have mentioned that part of the reason I am following this diet is because I intend to temporarily eliminate fiber in order to treat SIBO. My worst symptoms are brain-fog, fatigue, and hormonal dysfunction, and these seem to correlate with the degree of my GI problems. I was on several different high-dose antibiotics for a few months to treat Lyme disease, so this probably made my GI problems worse. When I tried rifaximin to treat SIBO, this temporarily improved my energy and brain-fog, but the effects didn’t last. Fiber makes my fatigue and constipation much worse, and I always feel much more fatigued after meals, so I figured that a fiber-free elemental diet might allow my gut to heal.
Do you think if I added small amounts of potato starch to the elemental diet, that I could prevent starving the healthy gut flora, while still starving the SIBO? Potato starch has made me feel worse when I tried adding it to my diet, but maybe this won’t be the case if I’m following an elemental diet. Probiotics and fermented foods also usually make my symptoms worse, but I could consider adding them to the elemental diet if my transit time is faster and they don’t have time to ferment in the small intestine.
I have been supplementing with A/D/C/K for a while, along with raw pastured egg yolks. I tend to feel more fatigued when I eat egg yolks (or pure choline), but I include them in my diet anyway as a dense source of nutrients. I’ve been working on circadian rhythm entrainment, although intermittent fasting exacerbates my adrenal and thyroid symptoms.
If I include:
-vitamin D3 (I take 10,000IU daily)
-vitamin C w/ bioflavonoids
-a blend of polyphenol extracts from berries and fruits (Xymogen Oraxinol)
-pastured beef liver 1x/week for vitamin A and other nutrients
-pastured raw egg yolks for additional nutrients
Do you think this will be sufficient to prevent harmful effects from an elemental diet while healing my gut?
I completely agree that a balanced whole-food diet is optimal for most people, but I’m only considering an elemental diet of processed isolated nutrients because my health problems have persisted for so long. I am in my early 20’s, and I
was previously very healthy and high-functioning before I got sick. My medical problems have taken over my life, so I am looking for the fastest treatment possible.
Thanks again for your help.
Did you consider a possible heavy metal poisoning? Gut issues can be hard to fix for good if it is an underlying cause. If you have reasons to suspect metal toxicity, for example if your disease started after dental work, you should see a doctor knowledgeable about this. Cutler’s work is also a very useful reference guide, even if you do not have amalgams
Hi Greg, did you cure your Sibo?
Hello Paul and thank you for your work
I am 55 year old male living in UK.I have strictly followed the diet for the last six months with circadian rhythm and all supplements other than Lithium and Silicon.I I/F eating in 8 hour window.
I have never had weight issues but have atherosclerosis,and have B12 injections every 8 weeks as I have very low intrinsic factor.I have been very careful on increasing my Iodine supplement as my Thyroid TSH was 0.91 and T4 15.20 in 2011.I have only taken 300 mcg a day and not doubled up each month as you advise.I had my TSH checked two months ago and it is 1.92 and T4 16.3I am guilty of probably training too much and when I
I weight train two days a week I have terrible difficulty in sleeping.(which has since I started heavy exercise been a constant problem).Other than this I have for the last two months had a swelling on both sides of my throat under my jaw bone similar to when your glands swell up when you get a throat infection ( not lower down the neck like where online goitre pictures are shown).
My lipids are near perfect as per your book.I am worried I have either Hyperthyroid (my best guess),Hypothyroid or burnt out adrenals or high cortisol.In the book you mention slowly increasing Iodine until side effects subside.Are my symptoms typical.? My body temp on home digital thermometer average daily is 36 cent or 96.8 fahr.
Any advise do I stop exercise and supplements for a month to see how the sleep and swelling in neck body temp and TSH improve or do I up my Iodine to get it up to 1 mg.I have read elsewhere that Iodine supplements can cause Hyperthyroid ?You also mention in the book that Lithium can relieve hyperthyroid.Should I try that.?
If you advise I see my GP what should I ask to get checked.Sorry to run on.You are no doubt very busy.
Thankyou My health other than the minor things above has improved tremendously. Marcus
Hi Marcus,
It does sound like hyperthyroidism. It also sounds like you are working off the earlier version of our book. I would get the new UK edition if you can, or borrow it from your library.
We don’t recommend going above 225 mcg iodine any more. In hyperthyroidism you can’t even take that much. Try stopping it but eating a leaf of nori seaweed daily.
Iodine needs to be balanced by selenium. This is no problem in the US because our beef and vegetables are selenium rich. However, in Europe it can be an issue. Try supplementing selenium 200 mcg at least once a week, maybe 2-3 times.
Work on your sleep and on balancing nutrition. Try getting collagen from bones, joints, and tendons cooked in soups and stews, plus extra vitamin C. Make sure you are not anemic and that you have appropriate zinc and copper.
Get appropriate amounts of vitamin A from liver, spinach, carrots, sweet potatoes. If you don’t eat liver, supplement A from cod liver oil and choline.
Yes, I think you should see your GP and get checked out. Often hyperthyroidism is followed by a later hypothyroidism that benefits from replacement thyroid hormone; it also can induce adrenal dysfunction. Ask your doctor if the swelling is due to lymph nodes or goiter. The doctor can also do general blood tests to look for issues that may be contributing to your symptoms.
Best, Paul
“We don’t recommend going above 225 mcg iodine any more”
Hi Paul,
Seeing your comment above, it may be worth you modifying/updating your supplements page,
there is a bullet point under your daily supplements that currently reads,
“_Iodine at least 225 mcg, recommend 1 mg”
thankyou for taking the time to help me
Hello. I own an older edition of the book (2012). What are the reasons for you not to recommend going above 225 mcg iodine any more? Doing a quick search on iodine, I cannot find a recent article or discussion explaining it on the website. Best regards, Frans
Hi Frans, the concern is that if selenium intake is off, high doses of iodine can be dangerous; and selenium is hard to control since food levels are so variable.
Hi Dr. Jaminet,
I was wondering what is your opinion of nuts consumption for those with digestive problems or weaknesses?
And if tolerable, would raw or roasted nuts be better?
Thanks
HEy paul,
I have a question regarding small intestinal transit. Would something that digests faster such as white rice also process through the small intestines and colon (and thus be excreted) faster then something like oatmeal (soluble fibers would delay gastric emptying and small intestinal transit would it not)? I tend to have a weaker digestive system, so I want to try and stick to foods that naturally process through a bit quicker and arent tougher to digest!
Hi John,
Not necessarily, it depends on what you eat them with. Make sure your choline status is good by eating lots of egg yolks and liver, that will improve intestinal transit.
i started eating wholemeal bread and my hair started growing back, maybe becaus of all the nutrients in wholemeal bread when i eat rice my hair falls off
avoid bread with vinegar in it
so everyone is different
spicy and acidic fruits like pinaple apple foods and lemon and garlic will wreck the stomach inflaming it, thus your body will not receive any nutrients once stomach is inflames,
white bread has no nutrients only high carbs like white rice
you see many asians eating spicy and fried foods and rice and “white” bread, eventualy most all have bald sooner or later they turn bald
and you say rice is good?
its totaly false what you say about fibre causing scrape of intestinal lining or villi
its mostly all irritating foods like garlic acidic fruits chilli and spicy foods ans fried foods and strong bitter foods which will corupt your intestinal lining
also sugar will inflame the intestinal villi or lining, once your stomach or bowels is inflamed it will make you go to toilet often because the intestine cannot fill up any more faeces because of the inflamation
Hi Paul
I am glad I came across your page as it by far one of the most informative and thoroughly backed up by science I’ve found after suffering through hundreds of pseudo medical advice on this really discouraging condition.
I am 40 years old and have been suffering ( taking a deep breath) : diarrhea,constipation,bloating after meals,acute pain in my sternum,as well as ( May or May not be related) chronic water retention in hands, legs, feet,abdomen face and eyelids,dental issues( ulcers, infections), frequent sore throats, skin rashes resembling eczema mostly on my fingers,dull skin,fogginess, for roughly 10 years.
I was diagnosed bipolar at age 33 and medicated ever since (Wellbutrin and topamax).All the above symptoms have gradually worsened.
For the record my mother had anal cancer and my brother recently had a large piece of his small intestine removed.
I tend to crave starchy and sugary foods and alternate between episodes of really healthy eating and not so healthy eating.
I consulted a naturopath about 6 years ago who suspected that I had severe food intolerance ( to gluten for one and possibly dairy, as a result of eating gluten)and urged me to change my diet and supplement myself on vitamins and minerals.Did I take his advice? Obviously not, hence I am writing now.
For the past 6 months my condition got so unmanageable that I decided to really do something about it. Two weeks ago I took an abdominal ultrasound that revealed that I have a 1.2 cm gallstone and my doctor diagnosed my with IBS.
I am scheduled to see a gastroenterologist .
I have gone to great lengths to educate myself about digestive illness and food intolerance.
I do believe that the appropriate diet will highly contribute to remission.Yes I have gotten bad enough that I am determined to finally eat like a grown up.
Now….I was contemplating going on the SCD diet but find it alarmingly restrictive.
What about the GAPS.? Would you recommend it?
Or what other guidelines do you suggest I begin with?
Thank you for any advice you may give.
Hi Paul
I am writing again to apologize for asking about other diets and protocols.
Forgive me, I had just come across your page and did not realize that it is entirely dedicated to A diet in itself, my bad! Here’ s what happens when one frantically searches for an answer and does not take the time to read through the many pages of very valuable information that is available here. Ah! That must be all the residue of gluten in my system making me act like an idiot 😳 Anyways….I have done my homework and started reading your book ( I probably should have started there!) and even began to implement 99% of your dietary guidelines! I say 99 because I’ m probably not doing it perfectly right yet , I’m sure I’ m still eating foods I should not without knowing ( wrong kind of sugar maybe?) and as I will keep on educating myself I should get it right .
But I’d like to report that I resumed taking a multivitamin with all the recommended supplements a few days ago, and starting eating as you recommend and all the symptoms described in my previous post so far have greatly reduced!
Thank you! And again forgive me for barging in the first time .
Hi Delphine,
Congratulations on the improvements you’ve already experienced! One of the best things about PHD is that even though you don’t eat sugar and wheat, what you do eat tastes fabulous. It doesn’t even feel like a diet. I don’t know what version of the book you got, but I don’t think multivitamins are recommended anymore. The supplement guidelines have many recommendations, some weekly, some daily, with the goal being getting just the right amount—not too much, not too little—which is difficult to do with any multivitamins I’ve ever seen. You might want to look into low-dose lithium, as well. Maybe it could help with the bipolar issues.
Hi Joseph
Right now I am just sticking to the basic supplementation on vitamins B , K, D, C, Magnesium,Iodine and the multivitamin I take happens to have just the recommended amount showing on the chart displayed on this website.Of course if there is a better way to supplement myself , by all means do feel free to add your two cents as I have not yet reached that specific section of the books.
I am not too psyched about lithium though…I have seen my father turn into a vegetable on it, even at low doses, and isn’t it the main component of batteries?I’ m being cute , I know lithium is a less than desirable substance to have in your system, as is Wellbutrin and topamax , Granted! I hope to come off all drugs in the near future with proper brain food!
I am definitely eating more fatty fish, broth made from bones and joints, egg yolks and I have started eating white rice and potatoes again.I have eliminated EVERYTHING on the NO list but I found out today that honey is not an acceptable sweetener .what are your thoughts on Stevia? Do you suggest rice syrup as the only sweetener?
Again thank you for all the input.
Delphine, I’m certainly not trying to push lithium on anyone. The high doses some people take are forced to take have pretty serious side effects, though it does also provide them some benefits. I only mentioned lithium because Paul talks about it briefly in the PHD book as an optional supplement at a very low dose. I don’t take it because it can exacerbate hypothyroidism and I’m trying to bring down my TSH, but the shop supplements section on the website recommends as little as 1.25 mg/day, which is like a 1/4 tablet of the Doctor’s Best brand.
As for sweeteners, opinions vary widely. I am a huge fan of stevia, myself. I ordered a bag of what I call green stevia, which is just the ground up leaves of the plant, and I also have a bottle of white stevia extract, which has no other additives. You’ve got to read labels because they sneak in all sorts of “dextrins” and I like just the stevia. By itself, it has a funny after taste, so you always want to use it with some other kind of sweetener or strongly flavored food. If you add a tiny sprinkle to mashed banana and sweet potato, it really brings up the sweetness without any funny after taste and no extra fructose. Or you can use it to reduce other sweeteners. For instance, if you are sweetening a cup of tea, try sprinkling tiny amounts of stevia into the cup, just enough so you can taste it, then add a little honey to sweetness. You won’t taste the stevia anymore after you add the honey, and you’ll use a fraction of the amount of honey you otherwise would. So, to sum up: by itself, not so good, but very useful in reducing calories or fructose.
Hi !
I seem to be the only one who does not get through to Paul 🙁
I posted two different comments and emailed him personally and ….Nothing
Paul doesn’t answer all my questions either. It’s not just you. He’s probably busy with the retreat coming up. But it can be disheartening if no one answers. PHD is simple, but it’s not easy! And health progress seems to go in spurts, or sometimes with a step back before healing resumes. Stick with it!
Delphine,
Paul has mentioned that the most up to date recommendations for any of the PHD supplements is always to be found on the website. The book contains explanations on the importance (or not) of various supplements, but some of the recommendations have changed in the past several years because of more recent research results. Obviously it’s impossible to keep the books updated.
Click on the tab ‘Shop’ at the top of the page and then on ‘shop supplements’ to see the latest recommendations.
Hi Hillary
Thank you for this complement of information, I am still new to this blog and trying to get my bearings…Thank Goodness for helpful people like you and Joseph!
Paul, I have major issues with fatigue and adhd that turns around 100% while in veto. Is there anything you would suggest to make veto more healthy without the add crabs?? Frutose makes ny liver hurt and everything I add potatoes or rice the extreme fatigue returns. I own your book and recommend it often, just need some advice on keto.. Have you read keto clarity and if so what do you think?
Sorry, I can see I made many spelling errors in my post, stupid predict text. I ment my systomps totally fade while in ketosis and re appear once add crabs. Fructose really makes my liver hurt the next day. Just looking for healthy advice on safe ketosis, I have 4 kids, just want to be around and healthy for my family and self.
I seemed to be the only one who can not get through to Paul 🙁
I posted two questions, emailed him directly but never heard back from him..,
Any advice on how to get advice from him?
Thanks!
Perhaps a paid consultation 😉
No! it’s not you. Imagine if you were him, trying to concentrate on so many people’s different questions AND maintain his regular work—along with the many conversations he keeps up with colleagues (so that he can continually be honing the wonderful ideas we need him write about)—and also just have a life. I’m always amazed if he answers anyone at all. I’ve been UNanswered many many times! and that’s ok. Look back in all the comments to articles, you’ll see how many unanswered questions have been posted.
@St August : Very good point! Glad to know I’m not going about it the wrong way.
One thing that slightly confuses me about the elimination of ALL cereal grains is that in the articles referenced, they only really villianize wheat because it contains wheat gluten, peptides and WGA. If I were to consume sprouted, gluten free grains, wouldn’t this issue be minimized, if not eliminated? There’s also the small CLA content-that has been proven to be beneficial in small doses- in a lot of grains, but we’re talking grams per cup of grain, is it really that influential? I found the book to be a solid read, but that was one of the areas of the book that I found a little lacking.
A response would be much appreciated!
I want to say “thank you” for this post! It has helped me so much. I was diagnosed with Ulcerative Colitis over a year ago and tried several different diets to treat my disease (despite my gastroenterologist telling me food played no role). Although these diets pointed me in a better direction, ultimately they proved unsuccessful. And then I found you guys! Following the suggestions outlined in this post has given me my life back. My family and I are forever grateful! We happen to live in Boston as well :).
That’s great Lauren! Thank you for sharing. If you have time, consider leaving an Amazon review!
Best, Paul
Absolutely, I would be happy to!
Hi Paul,
I love your series on bowel disease it has helped me a lot so far. I started with an SCD leaky gut protocol but it didn’t end up working because of the high fiber in the diet.
I do find I am sensitive to fats and have removed them from my diet for the last few days. This feels wrong, I’m concerned with deficiencies and eating to many starches to make up for the calorie loss. When is okay to add fats back in if your sensitive? Are there fats that are easier to digest than others? What would you consider optimal low fiber choices for someone with Leaky gut, SIBO and IBS? Also, I would like to do Bulletproof intermittent fasting to get through 16-18 hour fasts but I’m concerned to do this because of the fats. Is this okay, or not?
I hope this question can answer mine and help other people on this subject!
Your response is appreciated.
Hi Paul, you say:
“…the presence of starch, which is ordinarily unavailable in the colon, favors the growth of pathogenic species.”
But doesn’t this contradict the idea that Resistant Starch actually favors the growth of beneficial species?
MatthewGrace,
You might try posting this question on the Perfect Health Diet official Facebook group. You can tag Paul there and he may see it and reply. But there are numerous very well-informed people in the group and several have the qualifications to reply to such questions. You’ll need to join Facebook first. 🙂
> Fructose Toxicity
As I read through the article, I’m crossing foods off my shopping list.
But in the Fructose section, you only say it’s bad, but don’t mention any particular foods. Confirmation would be appreciated if you’re saying that fruit should be eliminated for healing bowel disease.
No, fruit should not be eliminated. The problem is excess fructose from added sugar. Our book discusses the optimal amount of fructose in detail.
> protein should not be obtained from eggs. However, fats from eggs are highly desirable.
What are we supposed to make of that??
Hi Neil, all you need to do is separate the egg yolks from the egg whites and consume only the yolks. That way you don’t get the less desirable proteins that eggs provide but all the benefits of nutrient dense yolks.
OK; I commented too soon. Regarding frutose, you’re OK with fruits and berries. Good.
You wrote:
> 3 to 6 months after removal of wheat from the diet. This is probably a reasonable estimate for the time frame in which bowel disease patients can expect significant improvements from the elimination of dietary food toxins.
That’s good too. It’s the first time I saw a suggestion that I can get over this problem, instead of it lasting for the rest of my life.
Wanna buy a warehouse of oatmeal?
Hi, you stated:
“When the small intestine is damaged, fatty foods may be difficult to tolerate, since the enzymes that digest dietary fats and proteins may also digest human cells. In such cases the diet must focus on starchy foods like rice until bowel health is restored. Be sure to supplement with vitamins and minerals in such cases.”
I currently have a fistula where my belly button used to be and where prior incision from bowel resections (3) is. It is having problems healing as I did introduce buckwheat, moong dal beans, red lentils. I have a hard time going to animal proteins as it seems to open things up more and causing more problems. How long should I stay on the rice type diet before I get to the animal proteins? Also are white potatoes, plantains, sweet potatoes, still ok? What vitamins/minerals should I consume and can I get extra protein from another source?
Hi Paul,
I have leaky gut, candida overgrowth, celiac disease, migraines (etc, etc, the list goes on). Should I follow the tips in this post? … and to what extent? Should I avoid nightshades and cheese/yogurt/milk for example? Egg whites? But eat the yokes and butter/ghee?
I’m a bit overwhelmed by my health issues as it is, so I want to follow a simple protocol that doesn’t exhausted me too much and that isn’t too complicated to handle.
I can’t afford to buy any supplements, so how the get the necessary vitamins and so on via diet?
Is coffee still okay to drink? (I suffer from gastritis, but somehow I feel that the coffee helps my low stomach acid, I don’t know why).
There are so many opinions out there, I’m utterly confused at this point as what to do. Would be ever so grateful for your guidance.
So, I’m wondering. If we’re not to eat poultry, dairy, whole grains, legumes, and seeds. And now with the Neu5gc concern, no mammal meats either. How is one to get enough protein. Is fish the only protein left?
So the entire diet is fish, white rice and sweet potatoes (no one eats yams or taro), non-nightshade veggies, berries and coconut oil (which I’m allergic too).
I want to be healthy, but this seems too restrictive to be healthy. 🙁 I’m not going to get enough protein or fat on this diet. No wonder people lose weight.
Hi Stephen,
Are you referring to our diet? We support eating poultry, dairy, and legumes with proper preparation. And mammal meats of course – it is only in certain autoimmune conditions that Neu5gc may be problematic.
Best, Paul
Caroline,
I’ve had visual migraines (auras lasting about 15 minutes, but no pain) for more than 30 years, with increasing frequency (a few times a year, increasing over time to say 3 or 4 in 3 days) until about a year ago when they stopped. I started the diet in 2010 and became increasingly compliant over the years.
I eat a lot of white potato, steamed and cooled, but have eliminated peppers and tomatoes and dairy (I was eating sour cream and whipping cream and cheese but I’m increasingly convinced dairy makes my acne much worse). I drink 40 ounces of coffee every day. I get at least 2-3 TBSP of coconut oil, but often almost twice that. I am throwing the egg whites away and eating 3 pasture raised yolks every day. I try to eat a few canned oysters every day or most days for the incredible zink and copper content. I try to eat liver (say 1/4 lb of calf liver or a pound of chicken liver with bacon and onions) as a kind of natural food multivitamin.
My diet has been pretty close to the core of PHD (divide a plate into quarters, into which I put roughly equal volumes of 1)safe starch, 2)meat or fish, 3) sweet veg (steamed beets or carrots or berries), and 4 low cal veg (broccoli, spinach, lettuces, aspargaus, radish, etc. trying to eat more diversity than any one plant). I increase and decrease the amounts to whatever allows me to fast 16 hours with ease. I’m fanatical about calculating the nutrition of my meals with Cronometer but have discovered that Paul has really made it very simple with the 4 quadrant approach. My experience is just do that and you will be in the ballpark. Maybe a little more starch than meat, generally, and if I ever get hungry for more of something I eat it.
I haven’t had a cold or the flu since starting the diet, although I do have mood issues that have not yet been made better (maybe a brain infection, oh joy;-) and my triglycerides are 70-80 and my HDL around the same, which suggests that the diet has moved my in an excellent direction, I think.
I know what you mean about so many opinions, how to decide. I’ve been reading nutrition books my whole life, and most pale in comparison to PHD. My sense is that the independent lines of reasoning all converge to suggest PHD is pretty close to right for most people.
I encourage you to give it a try. Eliminate as much as possible all manufactured “foods” and make the vast majority of what you eat real food. I do eat rice noodles occasionally but that’s pretty much the extent of my processed foods. Canned oysters, canned salmon, sardines, tuna fish–I consider those close enough to unprocessed so long as you don’t buy any with bad oils. Each week I like to get say 12 ounces of salmon for the omega 3, and I am ruthless about minimizing omega 6.